Approaches to Health Efficiency across the European Space through the Lens of the Health Budget Effort
Abstract
:1. Introduction
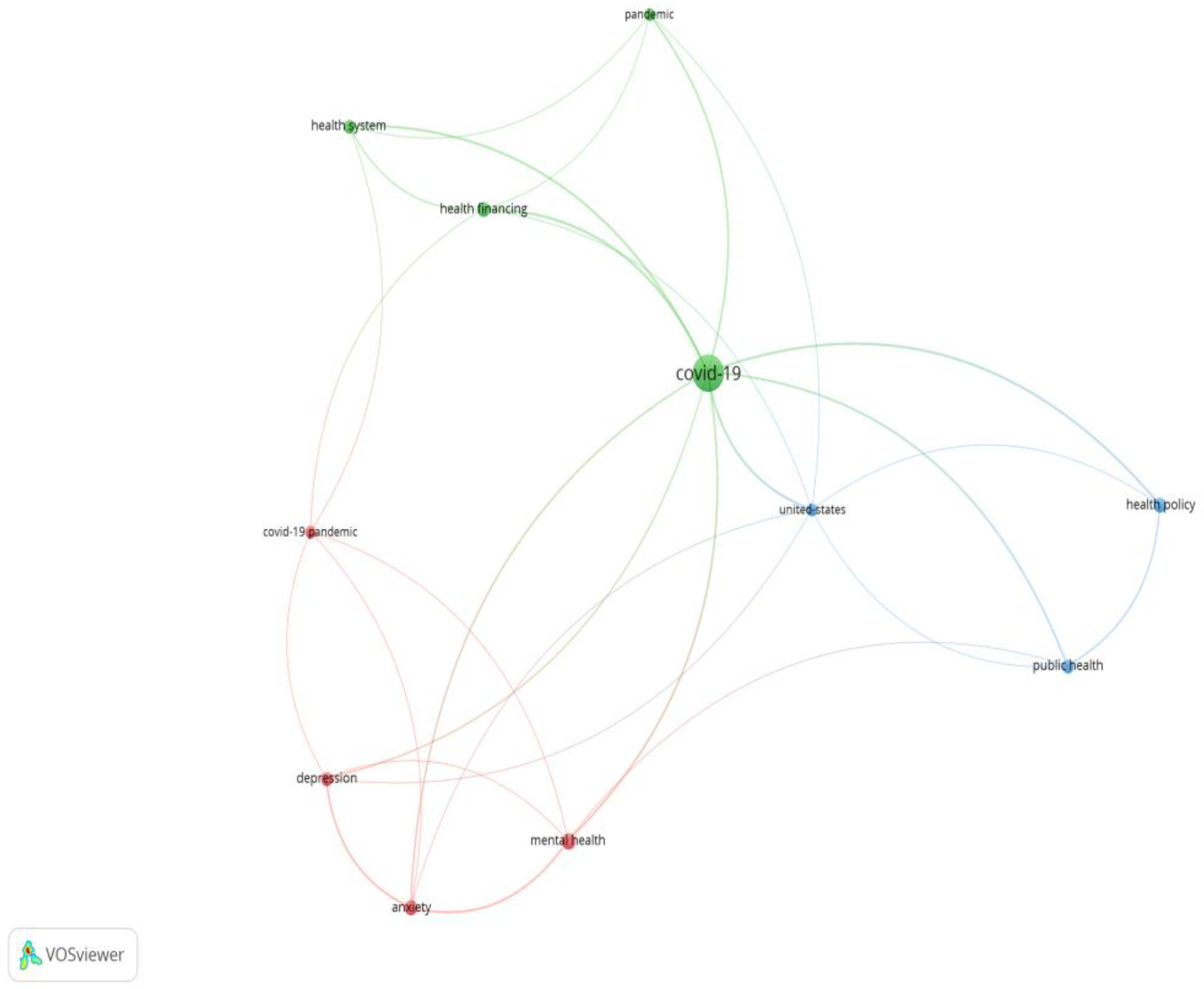
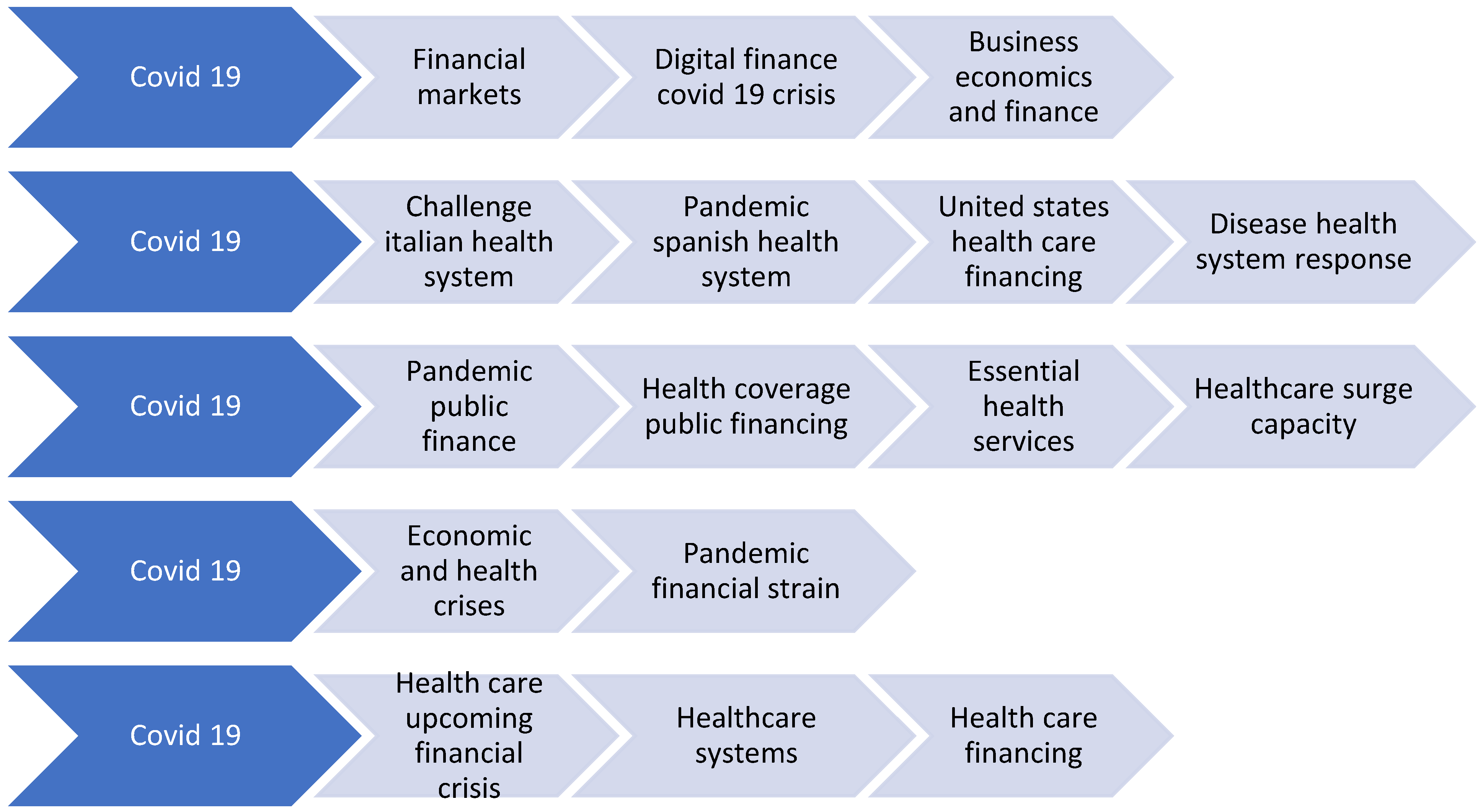
2. Literature Review
3. Methodology
4. Results and Discussion
- -
- There is a direct correlation between the health expenditure in the budget year (HLTH_SHA11_HC (year)) and the social protection expenditure (SPR_REC_SUMT_ESC). This has been the case since 2010, when European policy underwent a paradigm shift from a conservative to a forward-looking orientation, focusing on disease prevention rather than treatment. This validates hypothesis H2: In the case of financial policy stability for health, the main deflator of the allocation efficiency is the social protection expenditure as a percentage of GDP (see Table 4). The approach is congruent with other papers [4,5,34].
- -
- There is a direct correlation between the expenditure allocated to health in the budget year (HLTH_SHA11_HC (year) and the social protection scheme approved at government level through national strategies and at European level through Community strategies (SPR_REC_SUMT_GOV (year)). This validates hypothesis H1: The health status of the population varies in direct proportion to the health budget allocations, and changes in the government policies are likely to have a direct proportional influence on the medium and long-term health balance (see Table 4). The same approach was used by [26,34].
- -
- There is a direct correlation between the expenditure allocated to health in the budget year (HLTH_SHA11_HC (year)) and the strategy to protect the health of the population in the long term (HLTH_SHA11_LT (year)), i.e., to populate health units with specialists and technical equipment to ensure the sustainability of the health services and the continuous increase in the level of health of the population.
- -
- The fluctuating dynamics of the Pearson correlation of the dependent variable in relation to social protection and health security expenditure suggests that the trend is polynomial, with the forecast line being affected (with an inflection point) during the pandemic period.
- -
- The dynamics of the social protection expenditure represented by administrative costs has a polynomial evolution on the Pearson correlation coefficients with the dependent variable defined by the equation:y = −0.0771x + 1.3205
5. Conclusions
- -
- Rebalancing financial allocations for health in relation to strategic objectives at national and European levels;
- -
- Refocusing health police on prevention and health screening;
- -
- Linking short-term and long-term health policies;
- -
- Ensuring sustainability of the health sector through the sustainability of the resources used.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ANMCS | National Authority of Quality Management in Health |
| ANOVA | Analysis of variance is a collection of statistical models and their associated estimation procedures used to analyze the differences among means |
| COVID-19 | Coronavirus disease 2019 |
| DEA-BCC model | Data Envelopment Analysis-Banker, Charnes and Cooper Model |
| EU | European Union |
| EUROSTAT | is the statistical office of the European Union |
| GDP | Gross Domestic Product |
| IBM SPSS | software platform offers advanced statistical analysis, a vast library of machine learning algorithms, text analysis, open source extensibility, integration with big data and seamless deployment into applications |
| ISQua | International Society for Quality in Health Care |
| PPP | Purchasing power parity |
| OECD | Organisation for Economic Co-operation and Development |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus 2 |
| VOSviewer | software tool for constructing and visualizing bibliometric networks |
Appendix A
| Publication Type | Authors | Article Title | Source Title | ISSN | eISSN | ISBN | DOI | UT (Unique WOS ID) |
|---|---|---|---|---|---|---|---|---|
| J | Abor, P.A.; Abor, J.Y. | Implications of COVID-19 Pandemic for Health Financing System in Ghana | JOURNAL OF HEALTH MANAGEMENT | 0972-0634 | 0973-0729 | 10.1177/0972063420983096 | WOS:000618494100001 | |
| J | Beland, D.; Marchildon, G.P.; Medrano, A.; Rocco, P. | COVID-19, Federalism, and Health Care Financing in Canada, the United States, and Mexico | JOURNAL OF COMPARATIVE POLICY ANALYSIS | 1387-6988 | 1572-5448 | 10.1080/13876988.2020.1848353 | WOS:000605381000001 | |
| J | Liu, X.; Guo, S.Q. | Inclusive Finance, Environmental Regulation, and Public Health in China: Lessons for the COVID-19 Pandemic | FRONTIERS IN PUBLIC HEALTH | 2296-2565 | 10.3389/fpubh.2021.662166 | WOS:000643687100001 | ||
| J | da Silva, R.M.; Caetano, R.; Silva, A.B.; Guedes, A.C.C.M.; Ribeiro, G.D.; Santos, D.L.; Nepomuceno, C.C. | Profile and funding of health research triggered by the COVID-19 pandemic in Brazil | VIGILANCIA SANITARIA EM DEBATE-SOCIEDADE CIENCIA & TECNOLOGIA | 2317-269X | 10.22239/2317-269x.01579 | WOS:000537730600004 | ||
| J | Oliveira, P.F. | CHALLENGES OF INTERNATIONAL HEALTH LAW DURING THE COVID-19 PANDEMIC: NORMATIVE POWER, WITHDRAWAL AND FINANCING OF THE WORLD HEALTH ORGANIZATION | REVISTA ESTUDOS INSTITUCIONAIS-JOURNAL OF INSTITUTIONAL STUDIES | 2447-5467 | 10.21783/rei.v7i1.605 | WOS:000647193300006 | ||
| J | Cuervo, R.H.; Lopez, M.V. | Health public expenditure for CoVid 19 pandemic in Mexico | REVISTA MEXICANA DE ANALISIS POLITICO Y ADMINISTRACION PUBLICA | 2007-4425 | 2007-4638 | WOS:000629147400005 | ||
| J | Tandon, A.; Ivatts, S.; Cowley, P.; Roubal, T.; Dodd, R.; Pepperall, J.; Mikkelsen-Lopez, I.; Irava, W.J.; Palu, T. | Economic Contraction from COVID-19 in the Pacific: Implications for Health Financing | HEALTH SYSTEMS & REFORM | 2328-8604 | 2328-8620 | 10.1080/23288604.2020.1847991 | WOS:000599988900001 | |
| J | Werner, R.M.; Glied, S.A. | Covid-Induced Changes in Health Care Delivery - Can They Last? | NEW ENGLAND JOURNAL OF MEDICINE | 0028-4793 | 1533-4406 | 10.1056/NEJMp2110679 | WOS:000691647500001 | |
| J | Iizuka, T. | Comment on Sustainable Health Financing for COVID-19 Preparedness and Response in Asia and the Pacific | ASIAN ECONOMIC POLICY REVIEW | 1832-8105 | 1748-3131 | 10.1111/aepr.12373 | WOS:000700797200001 | |
| J | Ellis, R.P. | Comment on Sustainable Health Financing for COVID-19 Preparedness and Response in Asia and the Pacific | ASIAN ECONOMIC POLICY REVIEW | 1832-8105 | 1748-3131 | 10.1111/aepr.12366 | WOS:000687869700001 | |
| J | Mikolajczyk, B.; Draganich, C.; Philippus, A.; Goldstein, R.; Andrews, E.; Pilarski, C.; Wudlick, R.; Morse, L.R.; Monden, K.R. | Resilience and mental health in individuals with spinal cord injury during the COVID-19 pandemic | SPINAL CORD | 1362-4393 | 1476-5624 | 10.1038/s41393-021-00708-3 | WOS:000698531700003 | |
| J | Kwon, S.; Kim, E. | Sustainable Health Financing for COVID-19 Preparedness and Response in Asia and the Pacific | ASIAN ECONOMIC POLICY REVIEW | 1832-8105 | 1748-3131 | 10.1111/aepr.12360 | WOS:000678555100001 | |
| J | Gaffney, A.; Himmelstein, D.U.; Woolhandler, S. | COVID-19 and US Health Financing: Perils and Possibilities | INTERNATIONAL JOURNAL OF HEALTH SERVICES | 0020-7314 | 1541-4469 | 10.1177/0020731420931431 | WOS:000544393600001 | |
| J | Durrleman, A. | Impact of COVID-19 on the health insurance in the Social Security Financing Law Project (PLFSS) for 2021 | BULLETIN DE L ACADEMIE NATIONALE DE MEDECINE | 0001-4079 | 2271-4820 | 10.1016/j.banm.2021.01.008 | WOS:000635547900003 | |
| J | Sundararaman, T. | Health Systems Preparedness for COVID-19 Pandemic | INDIAN JOURNAL OF PUBLIC HEALTH | 0019-557X | 2229-7693 | 10.4103/ijph.IJPH_507_20 | WOS:000617766700005 | |
| J | Goldman, M.L.; Druss, B.G.; Horvitz-Lennon, M.; Norquist, G.S.; Ptakowski, K.K.; Brinkley, A.; Greiner, M.; Hayes, H.; Hepburn, B.; Jorgensen, S.; Swartz, M.S.; Dixon, L.B. | Mental Health Policy in the Era of COVID-19 | PSYCHIATRIC SERVICES | 1075-2730 | 1557-9700 | 10.1176/appi.ps.202000219 | WOS:000584395500011 | |
| J | Allen, H.L.; Sommers, B.D. | Medicaid and COVID-19 At the Center of Both Health and Economic Crises | JAMA-JOURNAL OF THE AMERICAN MEDICAL ASSOCIATION | 0098-7484 | 1538-3598 | 10.1001/jama.2020.10553 | WOS:000553161000010 | |
| J | Aregbeshola, B.S.; Folayan, M.O. | Nigeria’s financing of health care during the COVID-19 pandemic: Challenges and recommendations | WORLD MEDICAL & HEALTH POLICY | 1948-4682 | 10.1002/wmh3.484 | WOS:000714985500001 | ||
| J | Halliburton, A.E.; Hill, M.B.; Dawson, B.L.; Hightower, J.M.; Rueden, H. | Increased Stress, Declining Mental Health: Emerging Adults’ Experiences in College During COVID-19 | EMERGING ADULTHOOD | 2167-6968 | 2167-6984 | 10.1177/21676968211025348 | WOS:000667899400001 | |
| J | Gloster, A.T.; Lamnisos, D.; Lubenko, J.; Presti, G.; Squatrito, V.; Constantinou, M.; Nicolaou, C.; Papacostas, S.; Aydin, G.; Chong, Y.Y.; Chien, W.T.; Cheng, H.Y.; Ruiz, F.J.; Garcia-Martin, M.B.; Obando-Posada, D.P.; Segura-Vargas, M.A.; Vasiliou, V.S.; McHugh, L.; Hofer, S.; Baban, A.; Neto, D.D.; da Silva, A.N.; Monestes, J.L.; Alvarez-Galvez, J.; Paez-Blarrina, M.; Montesinos, F.; Valdivia-Salas, S.; Ori, D.; Kleszcz, B.; Lappalainen, R.; Ivanovic, I.; Gosar, D.; Dionne, F.; Merwin, R.M.; Kassianos, A.P.; Karekla, M. | Impact of COVID-19 pandemic on mental health: An international study | PLOS ONE | 1932-6203 | 10.1371/journal.pone.0244809 | WOS:000605651900147 | ||
| J | Bustreo, F.; Merialdi, M.; Hinton, R.; Gadde, R. | Why COVID-19 strengthens the case for a dedicated financing mechanism to scale up innovation in women’s, children’s, and adolescents’ health | LANCET GLOBAL HEALTH | 2214-109X | 10.1016/S2214-109X(20)30507-6 | WOS:000621377000012 | ||
| J | Vasileiou, E.; Samitas, A.; Karagiannaki, M.; Dandu, J. | Health risk and the efficient market hypothesis in the time of COVID-19 | INTERNATIONAL REVIEW OF APPLIED ECONOMICS | 0269-2171 | 1465-3486 | 10.1080/02692171.2020.1864299 | WOS:000603782700001 | |
| J | Hasan, H.F. | Legal and Health Response to COVID-19 in the Arab Countries | RISK MANAGEMENT AND HEALTHCARE POLICY | 1179-1594 | 10.2147/RMHP.S297565 | WOS:000632266900001 | ||
| J | Lal, A.; Erondu, N.A.; Heymann, D.L.; Gitahi, G.; Yates, R. | Fragmented health systems in COVID-19: rectifying the misalignment between global health security and universal health coverage | LANCET | 0140-6736 | 1474-547X | 10.1016/S0140-6736(20)32228-5 | WOS:000607268300027 | |
| J | Behzadifar, M.; Ghanbari, M.K.; Bakhtiari, A.; Behzadifar, M.; Bragazzi, N.L. | Ensuring adequate health financing to prevent and control the COVID-19 in Iran | INTERNATIONAL JOURNAL FOR EQUITY IN HEALTH | 1475-9276 | 10.1186/s12939-020-01181-9 | WOS:000533409000001 | ||
| C | Cibik, L.; Melus, M. | FUNDING OF PUBLIC HEALTH CARE IN EU COUNTRIES IN 2010-2018: PREPARATION FOR THE COVID 19 PANDEMIC? | PUBLIC ADMINISTRATION 2020: THREE DECADES OF CHALLENGES, REFORMS, AND UNCERTAIN RESULTS | 978-80-7560-338-8 | WOS:000632733100001 | |||
| J | Friedman, E.A.; Gostin, L.O.; Maleche, A.; Nilo, A.; Foguito, F.; Rugege, U.; Stevenson, S.; Gitahi, G.; Ruano, A.L.; Barry, M.; Hossain, S.; Lucien, F.; Rusike, I.; Hevia, M.; Alwan, A.; Cameron, E.; Farmer, P.; Flores, W.; Hassim, A.; Mburu, R.; Mukherjee, J.; Mulumba, M.; Puras, D.; Periago, M.R. | Global Health in the Age of COVID-19: Responsive Health Systems Through a Right to Health Fund | HEALTH AND HUMAN RIGHTS | 1079-0969 | 2150-4113 | WOS:000543379300018 | ||
| J | Haldane, V.; Foo, C.D.; Abdalla, S.M.; Jung, A.S.; Tan, M.; Wu, S.S.; Chua, A.; Verma, M.; Shrestha, P.; Singh, S.; Perez, T.; Tan, S.M.; Bartos, M.; Mabuchi, S.; Bonk, M.; McNab, C.; Werner, G.K.; Panjabi, R.; Nordstrom, A.; Legido-Quigley, H. | Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries | NATURE MEDICINE | 1078-8956 | 1546-170X | 10.1038/s41591-021-01381-y | WOS:000651469300001 | |
| J | Rokhmah, D.; Ridzkyanto, R.P.; Khoiron | Analysis of Government Budgeting for Health: Case Study of COVID-19 in East Java Province, Indonesia | KESMAS-NATIONAL PUBLIC HEALTH JOURNAL | 1907-7505 | 2460-0601 | 10.21109/kesmas.v15i2.3986 | WOS:000557024200011 | |
| J | Waitzberg, R.; Quentin, W.; Webb, E.; Glied, S. | The Structure and Financing of Health Care Systems Affected How Providers Coped With COVID-19 | MILBANK QUARTERLY | 0887-378X | 1468-0009 | 10.1111/1468-0009.12530 | WOS:000664665000001 | |
| J | Fernandes, G.A.D.L.; Pereira, B.L.S. | The challenges of funding the Brazilian health system in fighting the COVID-19 pandemic in the context of the federative pact | REVISTA DE ADMINISTRACAO PUBLICA | 0034-7612 | 1982-3134 | 10.1590/0034-761220200290x | WOS:000565842100008 | |
| J | Peiro, A.I. | The Spanish Government informative activity during the health emergency induced by coronaviruses, COVID-19 | REVISTA ESPANOLA DE COMUNICACION EN SALUD | 1989-9882 | 10.20318/recs.2020.5441 | WOS:000551629600025 | ||
| J | Prado, N.M.D.L.; Rossi, T.R.A.; Chaves, S.C.L.; de Barros, S.G.; Magno, L.; dos Santos, H.L.P.C.; dos Santos, A.M. | The international response of primary health care to COVID-19: document analysis in selected countries | CADERNOS DE SAUDE PUBLICA | 0102-311X | 1678-4464 | 10.1590/0102-311 × 00183820 | WOS:000595534800001 | |
| J | Chua, A.Q.; Tan, M.M.J.; Verma, M.; Han, E.K.L.; Hsu, L.Y.; Cook, A.R.; Teo, Y.Y.; Lee, V.J.; Legido-Quigley, H. | Health system resilience in managing the COVID-19 pandemic: lessons from Singapore | BMJ GLOBAL HEALTH | 2059-7908 | 10.1136/bmjgh-2020-003317 | WOS:000573870700004 | ||
| J | Simoes, J.; Magalhaes, J.P.M.; Biscaia, A.; Pereira, A.D.; Augusto, G.F.; Fronteira, I. | Organisation of the State, model of health system and COVID-19 health outcomes in six European countries, during the first months of the COVID-19 epidemic in 2020 | INTERNATIONAL JOURNAL OF HEALTH PLANNING AND MANAGEMENT | 0749-6753 | 1099-1751 | 10.1002/hpm.3271 | WOS:000668139700001 | |
| J | Geyman, J. | COVID-19 Has Revealed America’s Broken Health Care System: What Can We Learn? | INTERNATIONAL JOURNAL OF HEALTH SERVICES | 0020-7314 | 1541-4469 | 10.1177/0020731420985640 | WOS:000610305200001 | |
| J | Zuo, F.; Zhai, S.G. | The Influence of China’s COVID-19 Treatment Policy on the Sustainability of Its Social Health Insurance System | RISK MANAGEMENT AND HEALTHCARE POLICY | 1179-1594 | 10.2147/RMHP.S322040 | WOS:000707417600001 | ||
| J | Leach, C.R.; Kirkland, E.G.; Masters, M.; Sloan, K.; Rees-Punia, E.; Patel, A.V.; Watson, L. | Cancer survivor worries about treatment disruption and detrimental health outcomes due to the COVID-19 pandemic | JOURNAL OF PSYCHOSOCIAL ONCOLOGY | 0734-7332 | 1540-7586 | 10.1080/07347332.2021.1888184 | WOS:000621650400001 | |
| J | Hammarberg, K.; Tran, T.; Kirkman, M.; Rowe, H.; Fisher, J. | Preferred policy options to assist post-COVID-19 mental health recovery: A population study | AUSTRALIAN JOURNAL OF PUBLIC ADMINISTRATION | 0313-6647 | 1467-8500 | 10.1111/1467-8500.12507 | WOS:000687708200001 | |
| J | Pappan, N.; Austin, S.; Venkat, D.; Thakkar, P. | Identifying Social Determinants of Health and Allocating Resources During the COVID-19 Pandemic | INFECTIOUS DISEASES IN CLINICAL PRACTICE | 1056-9103 | 1536-9943 | 10.1097/IPC.0000000000001003 | WOS:000674879200006 | |
| J | Boateng, G.O.; Phipps, L.M.; Smith, L.E.; Armah, F.A. | Household Energy Insecurity and COVID-19 Have Independent and Synergistic Health Effects on Vulnerable Populations | FRONTIERS IN PUBLIC HEALTH | 2296-2565 | 10.3389/fpubh.2020.609608 | WOS:000614394700001 | ||
| J | Marshall, J.; Scott, B.; Delva, J.; Ade, C.; Hernandez, S.; Patel, J.; Moreno-Cheek, M.; Rojas, D.; Tanner, J.P.; Kirby, R.S. | An Evaluation of Florida’s Zika Response Using the WHO Health Systems Framework: Can We Apply These Lessons to COVID-19? | MATERNAL AND CHILD HEALTH JOURNAL | 1092-7875 | 1573-6628 | 10.1007/s10995-020-02969-5 | WOS:000543018000001 | |
| J | Edelman, A.; Marten, R.; Montenegro, H.; Sheikh, K.; Barkley, S.; Ghaffar, A.; Dalil, S.; Topp, S.M. | Modified scoping review of the enablers and barriers to implementing primary health care in the COVID-19 context | HEALTH POLICY AND PLANNING | 0268-1080 | 1460-2237 | 10.1093/heapoliczab075 | WOS:000693257400015 | |
| J | Shaikh, B.T. | Strengthening health system building blocks: configuring post-COVID-19 scenario in Pakistan | PRIMARY HEALTH CARE RESEARCH AND DEVELOPMENT | 1463-4236 | 1477-1128 | 10.1017/S1463423621000128 | WOS:000632233000001 | |
| J | Dawson, W.D.; Boucher, N.A.; Stone, R.; Van Houtven, C.H. | COVID-19: The Time for Collaboration Between Long-Term Services and Supports, Health Care Systems, and Public Health Is Now | MILBANK QUARTERLY | 0887-378X | 1468-0009 | 10.1111/1468-0009.12500 | WOS:000618271400001 | |
| J | Buzelli, M.L.; Boyce, T. | The Privatization of the Italian National Health System and its Impact on Health Emergency Preparedness and Response: The COVID-19 Case | INTERNATIONAL JOURNAL OF HEALTH SERVICES | 0020-7314 | 1541-4469 | 10.1177/00207314211024900 | WOS:000664270000001 | |
| J | Tiirinki, H.; Tynkkynen, L.K.; Sovala, M.; Atkins, S.; Koivusalo, M.; Rautiainen, P.; Jormanainen, V.; Keskimaki, I. | COVID-19 pandemic in Finland - Preliminary analysis on health system response and economic consequences | HEALTH POLICY AND TECHNOLOGY | 2211-8837 | 10.1016/j.hlpt.2020.08.005 | WOS:000593763800020 | ||
| J | Gignac, M.A.M.; Shahidi, F.V.; Jetha, A.; Kristman, V.; Bowring, J.; Cameron, J.I.; Tonima, S.; Ibrahim, S. | Impacts of the COVID-19 pandemic on health, financial worries, and perceived organizational support among people living with disabilities in Canada | DISABILITY AND HEALTH JOURNAL | 1936-6574 | 1876-7583 | 10.1016/j.dhjo.2021.101161 | WOS:000696982000019 | |
| J | Barasa, E.; Kazungu, J.; Orangi, S.; Kabia, E.; Ogero, M.; Kasera, K. | Indirect health effects of the COVID-19 pandemic in Kenya: A mixed methods assessment | BMC HEALTH SERVICES RESEARCH | 1472-6963 | 10.1186/s12913-021-06726-4 | WOS:000678609300002 | ||
| J | Ciciurkaite, G.; Marquez-Velarde, G.; Brown, R.L. | Stressors associated with the COVID-19 pandemic, disability, and mental health: Considerations from the Intermountain West | STRESS AND HEALTH | 1532-3005 | 1532-2998 | 10.1002/smi.3091 | WOS:000685707200001 | |
| J | Shaikh, B.T.; Ali, N. | COVID-19 and fiscal space for health system in Pakistan: It is time for a policy decision | INTERNATIONAL JOURNAL OF HEALTH PLANNING AND MANAGEMENT | 0749-6753 | 1099-1751 | 10.1002/hpm.2986 | WOS:000536494100001 | |
| J | Pettinicchio, D.; Maroto, M.; Chai, L.; Lukk, M. | Findings from an online survey on the mental health effects of COVID-19 on Canadians with disabilities and chronic health conditions | DISABILITY AND HEALTH JOURNAL | 1936-6574 | 1876-7583 | 10.1016/j.dhjo.2021.101085 | WOS:000679288800017 | |
| J | Hrevtsova, R.Y. | INSTITUTIONAL AND LEGAL ASPECTS OF HEALTH CARE IN TIMES OF COVID-19: LEARNING FROM THE UKRAINIAN EXPERIENCE | MEDICINE AND LAW | 0723-1393 | 2471-836X | WOS:000572461900017 | ||
| J | Micah, A.E.; Cogswell, I.E.; Cunningham, B.; Ezoe, S.; Harle, A.C.; Maddison, E.R.; McCracken, D.; Nomura, S.; Simpson, K.E.; Stutzman, H.N.; Tsakalos, G.; Wallace, L.E.; Zhao, Y.X.; Zende, R.R.; Abbafati, C.; Abdelmasseh, M.; Abedi, A.; Abegaz, K.H.; Abhilash, E.S.; Abolhassani, H.; Abrigo, M.R.M.; Adhikari, T.B.; Afzal, S.; Ahinkorah, B.O.; Ahmadi, S.; Ahmed, H.; Ahmed, M.B.; Rashid, T.A.; Ajami, M.; Aji, B.; Akalu, Y.; Akunna, C.J.; Al Hamad, H.; Alam, K.; Alanezi, F.M.; Alanzi, T.M.; Alemayehu, Y.; Alhassan, R.K.; Alinia, C.; Aljunid, S.M.; Almustanyir, S.A.; Alvis-Guzman, N.; Alvis-Zakzuk, N.J.; Amini, S.; Amini-Rarani, M.; Amu, H.; Ancuceanu, R.; Andrei, C.L.; Andrei, T.; Angell, B.; Anjomshoa, M.; Antonio, C.A.T.; Antony, C.M.; Aqeel, M.; Arabloo, J.; Arab-Zozani, M.; Aripov, T.; Arrigo, A.; Ashraf, T.; Atnafu, D.D.; Ausloos, M.; Avila-Burgos, L.; Awan, A.T.; Ayano, G.; Ayanore, M.A.; Azari, S.; Azhar, G.S.; Babalola, T.K.; Bahrami, M.A.; Baig, A.A.; Banach, M.; Barati, N.; Barnighausen, T.W.; Barrow, A.; Basu, S.; Baune, B.T.; Bayati, M.; Benzian, H.; Berman, A.E.; Bhagavathula, A.S.; Bhardwaj, N.; Bhardwaj, P.; Bhaskar, S.; Bibi, S.; Bijani, A.; Bodolica, V.; Bragazzi, N.L.; Braithwaite, D.; Breitborde, N.J.K.; Breusov, A.V.; Briko, N.I.; Busse, R.; Cahuana-Hurtado, L.; Callander, E.J.; Camera, L.A.; Castaneda-Orjuela, C.A.; Catala-Lopez, F.; Charan, J.; Chatterjee, S.; Chattu, S.K.; Chattu, V.K.; Chen, S.; Cicero, A.F.G.; Dadras, O.; Dahlawi, S.M.A.; Dai, X.C.; Dalal, K.; Dandona, L.; Dandona, R.; Davitoiu, D.V.; De Neve, J.W.; de Sa, A.R.; Denova-Gutierrez, E.; Dhamnetiya, D.; Dharmaratne, S.D.; Doshmangir, L.; Dube, J.; Ehsani-Chimeh, E.; Zaki, M.E.; El Tantawi, M.; Eskandarieh, S.; Farzadfar, F.; Ferede, T.Y.; Fischer, F.; Foigt, N.A.; Freitas, A.; Friedman, S.D.; Fukumoto, T.; Fullman, N.; Gaal, P.A.; Gad, M.M.; Garcia-Gordillo, M.A.; Garg, T.; Ghafourifard, M.; Ghashghaee, A.; Gholamian, A.; Gholamrezanezhad, A.; Ghozali, G.; Gilani, S.A.; Glavan, I.R.; Glushkova, E.V.; Goharinezhad, S.; Golechha, M.; Goli, S.; Guha, A.; Gupta, V.B.; Gupta, V.K.; Haakenstad, A.; Haider, M.R.; Hailu, A.; Hamidi, S.; Hanif, A.; Harapan, H.; Hartono, R.K.; Hasaballah, A.I.; Hassan, S.; Hassanein, M.H.; Hayat, K.; Hegazy, M.I.; Heidari, G.; Hendrie, D.; Heredia-Pi, I.; Herteliu, C.; Hezam, K.; Holla, R.; Hossain, S.J.; Hosseinzadeh, M.; Hostiuc, S.; Huda, T.M.; Hwang, B.F.; Iavicoli, I.; Idrisov, B.; Ilesanmi, O.S.; Irvani, S.S.N.; Islam, S.M.S.; Ismail, N.E.; Isola, G.; Jahani, M.A.; Jahanmehr, N.; Jakovljevic, M.; Janodia, M.D.; Javaheri, T.; Jayapal, S.K.; Jayawardena, R.; Jazayeri, S.B.; Jha, R.P.; Jonas, J.B.; Joo, T.; Joukar, F.; Jurisson, M.; Kaambwa, B.; Kalhor, R.; Kanchan, T.; Kandel, H.; Matin, B.K.; Karimi, S.E.; Kassahun, G.; Kayode, G.A.; Karyani, A.K.; Keikavoosi-Arani, L.; Khader, Y.S.; Khajuria, H.; Khalilov, R.; Khammarnia, M.; Khan, J.; Khubchandani, J.; Kianipour, N.; Kim, G.R.; Kim, Y.J.; Kisa, A.; Kisa, S.; Kohler, S.; Kosen, S.; Koteeswaran, R.; Laxminarayana, S.L.K.; Koyanagi, A.; Krishan, K.; Kumar, G.A.; Kusuma, D.; Lamnisos, D.; Lansingh, V.; Larsson, A.O.; Lasrado, S.; Le, L.K.D.; Lee, S.W.H.; Lee, Y.Y.; Lim, S.S.; Lobo, S.W.; Lozano, R.; Abd El Razek, H.M.; Abd El Razek, M.M.; Mahdavi, M.M.; Majeed, A.; Makki, A.; Maleki, A.; Malekzadeh, R.; Manda, A.L.; Mansour-Ghanaei, F.; Mansournia, M.A.; Arnedo, C.A.M.; Martinez-Valle, A.; Masoumi, S.Z.; Maude, R.J.; Mckee, M.; Medina-Solis, C.E.; Menezes, R.G.; Meretoja, A.; Meretoja, T.J.; Mesregah, M.K.; Mestrovic, T.; Kostova, N.M.; Miller, T.R.; Mini, G.K.; Mirica, A.; Mirrakhimov, E.M.; Mohajer, B.; Mohamed, T.A.; Mohammadi, M.; Mohammadian-Hafshejani, A.; Mohammed, S.; Moitra, M.; Mokdad, A.H.; Molokhia, M.; Moni, M.A.; Moradi, Y.; Morze, J.; Mousavi, S.M.; Mpundu-Kaambwa, C.; Muriithi, M.K.; Muthupandian, S.; Nagarajan, A.J.; Naimzada, M.D.; Nangia, V.; Naqvi, A.A.; Narayana, A.I.; Nascimento, B.R.; Naveed, M.; Nayak, B.P.; Nazari, J.; Ndejjo, R.; Negoi, I.; Kandel, S.N.; Nguyen, T.H.; Nonvignon, J.; Noubiap, J.J.; Nwatah, V.E.; Oancea, B.; Ojelabi, F.A.O.; Olagunju, A.T.; Olakunde, B.O.; Olgiati, S.; Olusanya, J.O.; Onwujekwe, O.E.; Otoiu, A.; Otstavnov, N.; Otstavnov, S.S.; Owolabi, M.O.; Padubidri, J.R.; Palladino, R.; Panda-Jonas, S.; Park, E.C.; Kan, F.P.; Pawar, S.; Toroudi, H.P.; Pereira, D.M.; Perianayagam, A.; Pesudovs, K.; Piccinelli, C.; Postma, M.J.; Prada, S.I.; Rabiee, M.; Rabiee, N.; Rahim, F.; Rahimi-Movaghar, V.; Rahman, M.H.U.; Rahman, M.; Rahmani, A.M.; Ram, U.; Ranabhat, C.L.; Ranasinghe, P.; Rao, C.R.; Rathi, P.; Rawaf, D.L.; Rawaf, S.; Rawal, L.; Rawassizadeh, R.; Reiner, R.C.; Renzaho, A.M.N.; Reshmi, B.; Riaz, M.A.; Ripon, R.K.; Saad, A.M.; Sahraian, M.A.; Sahu, M.; Salama, J.S.; Salehi, S.; Samy, A.M.; Sanabria, J.; Sanmarchi, F.; Santos, J.V.; Santric-Milicevic, M.M.; Sathian, B.; Savic, M.; Saxena, D.; Sayyah, M.; Schwendicke, F.; Senthilkumaran, S.; Sepanlou, S.G.; Seylani, A.; Shahabi, S.; Shaikh, M.A.; Sheikh, A.; Shetty, A.; Shetty, P.H.; Shibuya, K.; Shrime, M.G.; Shuja, K.H.; Singh, J.A.; Skryabin, V.Y.; Skryabina, A.A.; Soltani, S.; Soofi, M.; Spurlock, E.E.; Stefan, S.C.; Szerencses, V.; Szocska, M.; Tabares-Seisdedos, R.; Taddele, B.W.; Tefera, Y.G.; Thavamani, A.; Tobe-Gai, R.; Topor-Madry, R.; Tovani-Palone, M.R.; Tran, B.X.; Car, L.T.; Ullah, A.; Ullah, S.; Umar, N.; Undurraga, E.A.; Valdez, P.R.; Vasankari, T.J.; Villafane, J.H.; Violante, F.S.; Vlassov, V.; Vo, B.; Vollmer, S.; Vos, T.; Vu, G.T.; Vu, L.G.; Wamai, R.G.; Werdecker, A.; Woldekidan, M.A.; Wubishet, B.L.; Xu, G.L.; Yaya, S.; Yazdi-Feyzabadi, V.; Yigit, V.; Yip, P.; Yirdaw, B.W.; Yonemoto, N.; Younis, M.Z.; Yu, C.H.; Yunusa, I.; Moghadam, T.Z.; Zandian, H.; Zastrozhin, M.S.; Zastrozhina, A.; Zhang, Z.J.; Ziapour, A.; Zuniga, Y.M.H.; Hay, S.I.; Murray, C.J.L.; Dieleman, J.L. | Tracking development assistance for health and for COVID-19: A review of development assistance, government, out-of-pocket, and other private spending on health for 204 countries and territories, 1990-2050 | LANCET | 0140-6736 | 1474-547X | 10.1016/S0140-6736(21)01258-7 | WOS:000705490300019 | |
| J | Larson, A.; Skolnik, A.; Bhatti, A.; Mitrovich, R. | Addressing an urgent global public health need: Strategies to recover routine vaccination during the COVID-19 pandemic | HUMAN VACCINES & IMMUNOTHERAPEUTICS | 2164-5515 | 2164-554X | 10.1080/21645515.2021.1975453 | WOS:000709701900001 | |
| J | Wang, M.M.; Flessa, S. | Overcoming COVID-19 in China despite shortcomings of the public health system: what can we learn? | HEALTH ECONOMICS REVIEW | 2191-1991 | 10.1186/s13561-021-00319-x | WOS:000670273700003 | ||
| J | Whatley, M.; Castiello-Gutierrez, S. | Balancing finances, politics, and public health: international student enrollment and reopening plans at US higher education institutions amid the COVID-19 pandemic | HIGHER EDUCATION | 0018-1560 | 1573-174X | 10.1007/s10734-021-00768-7 | WOS:000705788300001 | |
| J | Mougharbel, F.; Sampasa-Kanyinga, H.; Heidinger, B.; Corace, K.; Hamilton, H.A.; Goldfield, G.S. | Psychological and Demographic Determinants of Substance Use and Mental Health During the COVID-19 Pandemic | FRONTIERS IN PUBLIC HEALTH | 2296-2565 | 10.3389/fpubh.2021.680028 | WOS:000671296000001 | ||
| J | Giovanis, E.; Ozdamar, O. | Who is Left Behind? Altruism of Giving, Happiness and Mental Health during the Covid-19 Period in the UK | APPLIED RESEARCH IN QUALITY OF LIFE | 1871-2584 | 1871-2576 | 10.1007/s11482-020-09900-8 | WOS:000599808000001 | |
| J | Busemeyer, M.R. | Financing the welfare state in times of extreme crisis: public support for health care spending during the Covid-19 pandemic in Germany | JOURNAL OF EUROPEAN PUBLIC POLICY | 1350-1763 | 1466-4429 | 10.1080/13501763.2021.1977375 | WOS:000698923700001 | |
| J | Akinyemi, O.O.; Popoola, O.A.; Fowotade, A.; Adekanmbi, O.; Cadmus, E.O.; Adebayo, A. | Qualitative exploration of health system response to COVID-19 pandemic applying the WHO health systems framework: Case study of a Nigerian state | SCIENTIFIC AFRICAN | 2468-2276 | 10.1016/j.sciaf.2021.e00945 | WOS:000704946300018 | ||
| J | Maulik, P.K.; Thornicroft, G.; Saxena, S. | Roadmap to strengthen global mental health systems to tackle the impact of the COVID-19 pandemic | INTERNATIONAL JOURNAL OF MENTAL HEALTH SYSTEMS | 1752-4458 | 10.1186/s13033-020-00393-4 | WOS:000557710700005 | ||
| J | Paltiel, O.; Hochner, H.; Chinitz, D.; Clarfield, A.M.; Gileles-Hillel, A.; Lahad, A.; Manor, O.; Nir-Paz, R.; Paltiel, A.; Stein-Zamir, C.; Yazhemsky, E.; Calderon-Margalit, R. | Academic activism on behalf of children during the COVID-19 pandemic in Israel; beyond public health advocacy | ISRAEL JOURNAL OF HEALTH POLICY RESEARCH | 2045-4015 | 10.1186/s13584-021-00485-7 | WOS:000686717500001 | ||
| J | Negro-Calduch, E.; Azzopardi-Muscat, N.; Nitzan, D.; Pebody, R.; Jorgensen, P.; Novillo-Ortiz, D. | Health Information Systems in the COVID-19 Pandemic: A Short Survey of Experiences and Lessons Learned From the European Region | FRONTIERS IN PUBLIC HEALTH | 2296-2565 | 10.3389/fpubh.2021.676838 | WOS:000706443200001 | ||
| J | Nemat, A.; Raufi, N.; Essar, M.Y.; Zeng, Q.C. | A Survey on the Health and Financial Status of Private Educational Institutions in Afghanistan During COVID-19 Pandemic | JOURNAL OF MULTIDISCIPLINARY HEALTHCARE | 1178-2390 | 10.2147/JMDH.S319872 | WOS:000669227400001 | ||
| J | Varma, P.; Burge, M.; Meaklim, H.; Junge, M.; Jackson, M.L. | Poor Sleep Quality and Its Relationship with Individual Characteristics, Personal Experiences and Mental Health during the COVID-19 Pandemic | INTERNATIONAL JOURNAL OF ENVIRONMENTAL RESEARCH AND PUBLIC HEALTH | 1660-4601 | 10.3390/ijerph18116030 | WOS:000659972500001 | ||
| J | Manouchehri, M.; Bhamra, S.K.; Fernandez-Alfonso, M.S.; Gil-Ortega, M. | The real impact of COVID-19 on community pharmacy professionals as part of the primary health care frontier workforce in Spain | JOURNAL OF PHARMACY & PHARMACOGNOSY RESEARCH | 0719-4250 | WOS:000678691600011 | |||
| J | Holingue, C.; Badillo-Goicoechea, E.; Riehm, K.E.; Veldhuis, C.B.; Thrul, J.; Johnson, R.M.; Fallin, M.D.; Kreuter, F.; Stuart, E.A.; Kalb, L.G. | Mental distress during the COVID-19 pandemic among US adults without a pre-existing mental health condition: Findings from American trend panel survey | PREVENTIVE MEDICINE | 0091-7435 | 1096-0260 | 10.1016/j.ypmed.2020.106231 | WOS:000571877100012 | |
| J | Chen, Y.S.; Zhou, Z.N.; Glynn, S.M.; Frey, M.K.; Balogun, O.D.; Kanis, M.; Holcomb, K.; Gorelick, C.; Thomas, C.; Christos, P.J.; Chapman-Davis, E. | Financial toxicity, mental health, and gynecologic cancer treatment: The effect of the COVID-19 pandemic among low-income women in New York City | CANCER | 0008-543X | 1097-0142 | 10.1002/cncr.33537, | WOS:000668286200007 | |
| J | Bedrunka, K.; Mach, L.; Kuczuk, A.; Bohdan, A. | Identification and Analysis of Structural Fund Support Mitigating the Effects of the COVID-19 Pandemic in the EU-A Case Study of Health Unit Funding | ENERGIES | 1996-1073 | 10.3390/en14164976 | WOS:000690572300001 | ||
| J | Szlamka, Z.; Kiss, M.; Bernath, S.; Kaman, P.; Lubani, A.; Karner, O.; Demetrovics, Z. | Mental Health Support in the Time of Crisis: Are We Prepared? Experiences With the COVID-19 Counselling Programme in Hungary | FRONTIERS IN PSYCHIATRY | 1664-0640 | 10.3389/fpsyt.2021.655211 | WOS:000661089000001 | ||
| J | Chen, Y.S.; Zhou, Z.N.; Glynn, S.M.; Frey, M.K.; Balogun, O.D.; Kanis, M.; Holcomb, K.; Gorelick, C.; Thomas, C.; Christos, P.J.; Chapman-Davis, E. | Financial toxicity, mental health, and gynecologic cancer treatment: The effect of the coronavirus disease 2019 (COVID-19) pandemic among low-income women in New York City | CANCER | 0008-543X | 1097-0142 | 10.1002/cncr.33537 | WOS:000643680600001 | |
| J | Bell, C.; Williman, J.; Beaglehole, B.; Stanley, J.; Jenkins, M.; Gendall, P.; Rapsey, C.; Every-Palmer, S. | Challenges facing essential workers: a cross-sectional survey of the subjective mental health and well-being of New Zealand healthcare and ‘other’ essential workers during the COVID-19 lockdown | BMJ OPEN | 2044-6055 | 10.1136/bmjopen-2020-048107 | WOS:000691828800014 | ||
| J | Amimo, F.; Lambert, B.; Magit, A.; Hashizume, M. | A review of prospective pathways and impacts of COVID-19 on the accessibility, safety, quality, and affordability of essential medicines and vaccines for universal health coverage in Africa | GLOBALIZATION AND HEALTH | 1744-8603 | 10.1186/s12992-021-00666-8 | WOS:000638235300002 |
References
- ISQua Accreditation International Accreditation Programme. Guidelines and Principles for the Development of Health and Social Care Standards 4th Edition Version 1.2. 2015. Available online: https://www.coursehero.com/file/33423828/guidelines-and-principles-for-the-development-of-health-and-social-care-standards-4th-edition-v12/ (accessed on 15 November 2021).
- National Authority of Quality Management in Health (ANMCS). Second Edition of the Accreditation Standards for Hospitals. 2021. Available online: https://anmcs.gov.ro/en/standards/ (accessed on 18 November 2021).
- Google Academics. Searching Academic Sources. 2021. Available online: https://scholar.google.ro/scholar?q=google+scholar&hl=ro&as_sdt=0&as_vis=1&oi=scholart (accessed on 19 November 2021).
- Racoare Apetroi, F.C.; Mihalache, I.-C.; Todosia, M. Economic Models of Financing Health Services in the European Union. Eur. Financ. Regul. EUFIRE 2018, 211–224. [Google Scholar]
- Bernd, R. Funding for public health in Europe in decline? Health Policy 2019, 123, 21–26. [Google Scholar] [CrossRef]
- Cacace, M. Case study C: Transforming healthcare financing in Central and Eastern European countries. In Handbook on Social Protection Systems; Edward Elgar Publishing: Cheltenham, UK, 2021. [Google Scholar]
- Racoare Apetroi, F.C.; Mihalache, I.-C.; Todosia, M. The Organization of Health Sector Financing in the Member States of the European Union and Health Policies. InTraders Int. Trade Acad. J. 2019, 2, 185–204. [Google Scholar]
- Wielechowski, M.; Grzęda, Ł. Health Care Financing in the European Union Countries—Structure and Changes. Acta Sci. Polonorum. Oeconomia 2020, 19, 71–80. [Google Scholar] [CrossRef]
- Tinica, G.; Bostan, I.; Grosu, V. Correlations regarding the economic growth and the direct and indirect costs incurred by chronic diseases. Rom. J. Bioeth. 2010, 8, 116–124. [Google Scholar]
- Tinica, G.; Bostan, I.; Grosu, V. The dynamics of public expenses in healthcare and demographic evolution in Italy and Romania. Rom. J. Bioeth. 2008, 6, 56–63. [Google Scholar]
- Abor, P.A.; Abor, J.Y. Implications of COVID-19 Pandemic for Health Financing System in Ghana. J. Health Manag. 2020, 22, 559–569. [Google Scholar] [CrossRef]
- Béland, D.; Marchildon, G.P.; Medrano, A.; Rocco, P. COVID-19, Federalism, and Health Care Financing in Canada, the United States, and Mexico. J. Comp. Policy Anal. Res. Pract. 2021, 23, 143–156. [Google Scholar] [CrossRef]
- Liu, X.; Guo, S. Inclusive Finance, Environmental Regulation, and Public Health in China: Lessons for the COVID-19 Pandemic. Front. Public Health 2021, 9, 204. [Google Scholar] [CrossRef]
- Da Silva, R.M.; Caetano, R.; Silva, A.B.; Guedes, A.C.C.M.; da Ribeiro, G.R.; Santos, D.L.; de Paiva, C.C.N. Profile and funding of health research triggered by the COVID-19 pandemic in Brazil. Health Surveill. Debate Soc. Sci. Technol. 2020, 8, 28–38. [Google Scholar] [CrossRef]
- Iizuka, T. Comment on “Sustainable Health Financing for COVID-19 Preparedness and Response in Asia and the Pacific”. Asian Econ. Policy Rev. 2022, 17, 159–160. [Google Scholar] [CrossRef]
- Kwon, S.; Kim, E. Sustainable Health Financing for COVID-19 Preparedness and Response in Asia and the Pacific. Asian Econ. Policy Rev. 2022, 17, 140–156. [Google Scholar] [CrossRef]
- Gaffney, A.; Himmelstein, D.U.; Woolhandler, S. COVID-19 and US Health Financing: Perils and Possibilities. Int. J. Health Serv. 2020, 50, 396–407. [Google Scholar] [CrossRef] [PubMed]
- Durrleman, A. Incidence de la COVID-19 sur l’Assurance maladie dans le projet de loi de financement de la Sécurité sociale (PLFSS) pour 2021. Bull. L’académie Natl. Méd. 2021, 205, 207–208. [Google Scholar] [CrossRef]
- Sundararaman, T. Health systems preparedness for COVID-19 pandemic. Indian J. Public Health 2020, 64, S91–S93. [Google Scholar] [CrossRef]
- Aregbeshola, B.S.; Folayan, M.O. Nigeria’s financing of health care during the COVID-19 pandemic: Challenges and recommendations. World Med. Health Policy 2021, 1–10. [Google Scholar] [CrossRef]
- Vasileiou, E.; Samitas, A.; Karagiannaki, M.; Dandu, J. Health risk and the efficient market hypothesis in the time of COVID-19. Int. Rev. Appl. Econ. 2021, 35, 210–223. [Google Scholar] [CrossRef]
- Hasan, H. Legal and Health Response to COVID-19 in the Arab Countries. Risk Manag. Healthc. Policy 2021, 14, 1141–1154. [Google Scholar] [CrossRef]
- Cíbik, L.; Meluš, M. Funding of Public Health Care in EU Countries in 2010–2018: Preparation for the COVID 19 Pandemic? In Proceedings of the 13th International Scientific Conference, Osijek, Croatia, 7–8 September 2020. [Google Scholar]
- Waitzberg, R.; Quentin, W.; Webb, E.; Glied, S. The Structure and Financing of Health Care Systems Affected How Providers Coped with COVID-19. Milbank Q. 2021, 99, 542–564. [Google Scholar] [CrossRef]
- Prado, N.; Aranha Rossi, T.; Chaves, S.C.; Barros, S.; Magno, L.; Santos, H.; Santos, A. The international response of primary health care to COVID-19: Document analysis in selected countries. Cad. Saúde Pública 2020, 36. [Google Scholar] [CrossRef]
- Bulatnikov, V.; Constantin, C.P. Systematic Analysis of Literature on the Marketing of Healthcare Systems. Challenges for Russian and Romanian Healthcare Systems. Healthcare 2021, 9, 656. [Google Scholar] [CrossRef] [PubMed]
- Rokicki, T.; Perkowska, A.; Ratajczak, M. Differentiation in Healthcare Financing in EU Countries. Sustainability 2021, 13, 251. [Google Scholar] [CrossRef]
- Spasova, S.; Terry, W. Social Protection Expenditure and its Financing in Europe. A study of National Policies 2019; European Social Policy Network (ESPN): Brussels, Belgium, 2019. [Google Scholar] [CrossRef]
- Mance, D.; Vretenar, N.; Gojković, J. Comparison of European Union Public Health Systems. Sel. Pap. 2019, 65–77. [Google Scholar] [CrossRef]
- Stepovic, M.; Rancic, N.; Vekic, B.; Dragojevic-Simic, V.; Vekic, S.; Ratkovic, N.; Jakovljevic, M. Gross Domestic Product and Health Expenditure Growth in Balkan and East European Countries-Three-Decade Horizon. Front. Public Health 2020, 8, 492. [Google Scholar] [CrossRef] [PubMed]
- Balçik, P.; Demirci, Ş.; Konca, M. Comparison of European countries’ health indicators and health expenditures by clustering analysis. Ömer Halisdemir Üniversitesi İktisadi İdari Bilimler Fakültesi Derg. 2021, 14, 365–377. [Google Scholar] [CrossRef]
- Giammanco, M.D.; Gitto, L. Health expenditure and FDI in Europe. Econ. Anal. Policy 2019, 62, 255–267. [Google Scholar] [CrossRef]
- Caunic, R.; Asandului, L. A data envelopment analysis of the response of healthcare facilities to coronavirus pandemic: Evidence from Romania. In Assessing the EU’s Actorness in the Eastern Neighbourhood-Eurint; Centre for European Studies, UAIC: Iasi, Romania, 2021; pp. 23–40. Available online: www.cse.uaic.ro (accessed on 18 November 2021).
- OECD. Romania: Country Health Profile 2019, State of Health in the EU; European Observatory on Health Systems and Policies, Ed.; State of H; OECD Publishing: Brussels, Belgium, 2019. [Google Scholar]
- Forman, R.; Shah, S.; Jeurissen, P.; Jit, M.; Mossialos, E. COVID-19 vaccine challenges: What have we learned so far and what remains to be done? Health Policy 2021, 125, 553–567. [Google Scholar] [CrossRef]
- Shaikh, B.T. Strengthening health system building blocks: Configuring post-COVID-19 scenario in Pakistan. Prim. Health Care Res. Dev. 2021, 22, e9. [Google Scholar] [CrossRef]
- EUROSTAT, DATABASE. Available online: https://ec.europa.eu/eurostat/data/database (accessed on 15 November 2021).
- Google News. Worldwide Coronavirus Statistics. 2021. Available online: https://news.google.com/covid19/map?hl=en-US&gl=US&ceid=US%3Aen&mid=%2Fm%2F06c1y (accessed on 18 November 2021).
| Indicators’ Names | Symbol | Unit of Measurement | Source |
|---|---|---|---|
| Expenditure on social protection | SPR_EXP_SUM | Percentage of GDP | [37] |
| Social benefits, in cash or in kind, to households and individuals | SPR_EXP_BNF | Percentage of GDP | [37] |
| Administration costs to the scheme for health management and administration | SPR_ADM | Percentage of GDP | [37] |
| Other expenditure by social protection schemes (payment of property income and other) | SPR_OTHER | Percentage of GDP | [37] |
| Receipts of social protection schemes (social contributions, general government contributions and other receipts) | SPR_REC_SUMT_GOV | Percentage of GDP | [37] |
| Employers’ social contributions | SPR_REC_SUMT_ESC- | Percentage of GDP | [37] |
| Total health care expenditure by EU27 average expenditure (Country average/EU27 average) | HLTH_SHA11_HC | Percentage of EU27 average expenditure | [37] |
| Long-term care (health) expenditure by EU27 average long-term expenditure (Country average/EU27 average) | HLTH_SHA11_LT | Percentage of EU27 average expenditure. | [37] |
| The rate of illness | COVID_ILL | Cases per 1 M people | [38] |
| The rate of vaccinations | COVID_VACC | % of population fully vaccinated | [38] |
| Model Year | R | R Square | Adjusted R Square | Std. Error of the Estimate | Change Statistics | Durbin-Watson | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| R Square Change | F Change | df1 | df2 | Sig. F Change | ||||||
| 2009 | 0.999 | 0.998 | 0.996 | 2.365 | 0.998 | 734.070 | 10 | 16 | 0.000 | 2.059 |
| 2010 | 0.998 | 0.996 | 0.994 | 2.928 | 0.996 | 452.810 | 10 | 16 | 0.000 | 2.061 |
| 2011 | 0.998 | 0.996 | 0.994 | 3.013 | 0.996 | 443.429 | 10 | 16 | 0.000 | 2.131 |
| 2012 | 0.999 | 0.998 | 0.996 | 2.468 | 0.998 | 645.618 | 10 | 16 | 0.000 | 2.146 |
| 2013 | 0.999 | 0.998 | 0.997 | 2.075 | 0.998 | 863.058 | 10 | 16 | 0.000 | 2.303 |
| 2014 | 0.999 | 0.998 | 0.997 | 2.049 | 0.998 | 889.853 | 10 | 16 | 0.000 | 2.028 |
| 2015 | 1.000 | 0.999 | 0.999 | 1.253 | 0.999 | 2266.115 | 10 | 16 | 0.000 | 2.339 |
| 2016 | 0.999 | 0.999 | 0.998 | 1.569 | 0.999 | 1352.670 | 10 | 16 | 0.000 | 1.452 |
| 2017 | 0.999 | 0.999 | 0.998 | 1.454 | 0.999 | 1523.163 | 10 | 16 | 0.000 | 2.453 |
| 2018 | 1.000 | 0.999 | 0.998 | 1.365 | 0.999 | 1662.286 | 10 | 16 | 0.000 | 1.495 |
| 2019 | 0.999 | 0.999 | 0.998 | 1.423 | 0.999 | 1498.636 | 10 | 16 | 0.000 | 1.959 |
| 2020 | 0.998 | 0.996 | 0.994 | 2.649 | 0.996 | 443.106 | 10 | 16 | 0.000 | 1.910 |
| Model Year | Sum of Squares Regression | Sum of Squares Residual | Sum of Squares Total | df Rg. | df Res | df Tot | Mean Square Regression | Mean Square Residual | F | Sig. |
|---|---|---|---|---|---|---|---|---|---|---|
| 2009 | 41,072.167 | 89.522 | 41,161.689 | 10 | 16 | 26 | 4107.217 | 5.595 | 734.070 | 0.000 |
| 2010 | 38,825.678 | 137.190 | 38,962.868 | 10 | 16 | 26 | 3882.568 | 8.574 | 452.810 | 0.000 |
| 2011 | 40,249.734 | 145.231 | 40,394.965 | 10 | 16 | 26 | 4024.973 | 9.077 | 443.429 | 0.000 |
| 2012 | 39,328.383 | 97.465 | 39,425.848 | 10 | 16 | 26 | 3932.838 | 6.092 | 645.618 | 0.000 |
| 2013 | 37,149.809 | 68.871 | 37,218.680 | 10 | 16 | 26 | 3714.981 | 4.304 | 863.058 | 0.000 |
| 2014 | 37,373.159 | 67.199 | 37,440.357 | 10 | 16 | 26 | 3737.316 | 4.200 | 889.853 | 0.000 |
| 2015 | 35,586.873 | 25.126 | 35,611.999 | 10 | 16 | 26 | 3558.687 | 1.570 | 2266.115 | 0.000 |
| 2016 | 33,294.597 | 39.382 | 33,333.980 | 10 | 16 | 26 | 3329.460 | 2.461 | 1352.670 | 0.000 |
| 2017 | 32,190.421 | 33.814 | 32,224.236 | 10 | 16 | 26 | 3219.042 | 2.113 | 1523.163 | 0.000 |
| 2018 | 30,952.398 | 29.793 | 30,982.191 | 10 | 16 | 26 | 3095.240 | 1.862 | 1662.286 | 0.000 |
| 2019 | 30,344.785 | 32.397 | 30,377.182 | 10 | 16 | 26 | 3034.479 | 2.025 | 1498.636 | 0.000 |
| 2020 | 31,092.351 | 112.271 | 31,204.621 | 10 | 16 | 26 | 3109.235 | 7.017 | 443.106 | 0.000 |
| Year | HLTH_SHA11_HC (Year-1) | SPR_EXP_SUM (Year) | SPR_EXP_BNF (Year) | SPR_ADM (Year) | SPR_OTHER (Year) | SPR_REC_SUMT_ESC (Year) | SPR_REC_SUMT_GOV (Year) | HLTH_SHA11_LT (Year) | HLTH_SHA11_LT (Year-1) |
|---|---|---|---|---|---|---|---|---|---|
| 2009 | 0.999 | 0.840 | −0.546 | 0.581 | 0.272 | 0.306 | 0.580 | 0.854 | 0.850 |
| 2010 | 0.828 | −0.497 | 0.572 | 0.180 | 0.308 | 0.566 | 0.998 | 0.864 | 0.868 |
| 2011 | 0.800 | −0.397 | 0.558 | 0.038 | 0.376 | 0.574 | 0.987 | 0.856 | 0.896 |
| 2012 | 0.810 | −0.405 | 0.610 | −0.001 | 0.379 | 0.593 | 0.995 | 0.897 | 0.899 |
| 2013 | 0.797 | −0.233 | 0.573 | −0.090 | 0.410 | 0.558 | 0.998 | 0.895 | 0.899 |
| 2014 | 0.785 | −0.428 | 0.578 | 0.054 | 0.403 | 0.559 | 0.998 | 0.898 | 0.903 |
| 2015 | 0.735 | −0.439 | 0.546 | 0.097 | 0.346 | 0.568 | 0.999 | 0.902 | 0.907 |
| 2016 | 0.722 | −0.461 | 0.587 | 0.100 | 0.288 | 0.582 | 0.999 | 0.900 | 0.905 |
| 2017 | 0.718 | −0.493 | 0.576 | 0.158 | 0.277 | 0.598 | 0.999 | 0.904 | 0.911 |
| 2018 | 0.710 | −0.632 | 0.576 | 0.318 | 0.334 | 0.597 | 0.999 | 0.912 | 0.917 |
| 2019 | 0.658 | −0.551 | 0.570 | 0.187 | 0.334 | 0.574 | 0.999 | 0.915 | 0.918 |
| 2020 | 0.645 | −0.527 | 0.569 | 0.149 | 0.314 | 0.560 | 0.996 | 0.919 | 0.905 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antohi, V.M.; Ionescu, R.V.; Zlati, M.L.; Mirica, C.; Cristache, N. Approaches to Health Efficiency across the European Space through the Lens of the Health Budget Effort. Int. J. Environ. Res. Public Health 2022, 19, 3063. https://doi.org/10.3390/ijerph19053063
Antohi VM, Ionescu RV, Zlati ML, Mirica C, Cristache N. Approaches to Health Efficiency across the European Space through the Lens of the Health Budget Effort. International Journal of Environmental Research and Public Health. 2022; 19(5):3063. https://doi.org/10.3390/ijerph19053063
Chicago/Turabian StyleAntohi, Valentin Marian, Romeo Victor Ionescu, Monica Laura Zlati, Cristian Mirica, and Nicoleta Cristache. 2022. "Approaches to Health Efficiency across the European Space through the Lens of the Health Budget Effort" International Journal of Environmental Research and Public Health 19, no. 5: 3063. https://doi.org/10.3390/ijerph19053063







