Positive Effects on Emotional Stress and Sleep Quality of Forest Healing Program for Exhausted Medical Workers during the COVID-19 Outbreak
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Study Design
2.2. Design of the Forest Therapy Program
2.3. Evaluation of Sleep and Emotional Status, Laboratory Measurements
2.4. Statistical Analysis
3. Results
3.1. General Characteristics of Participants
3.2. Changes of the Psychological Variables of the Participants
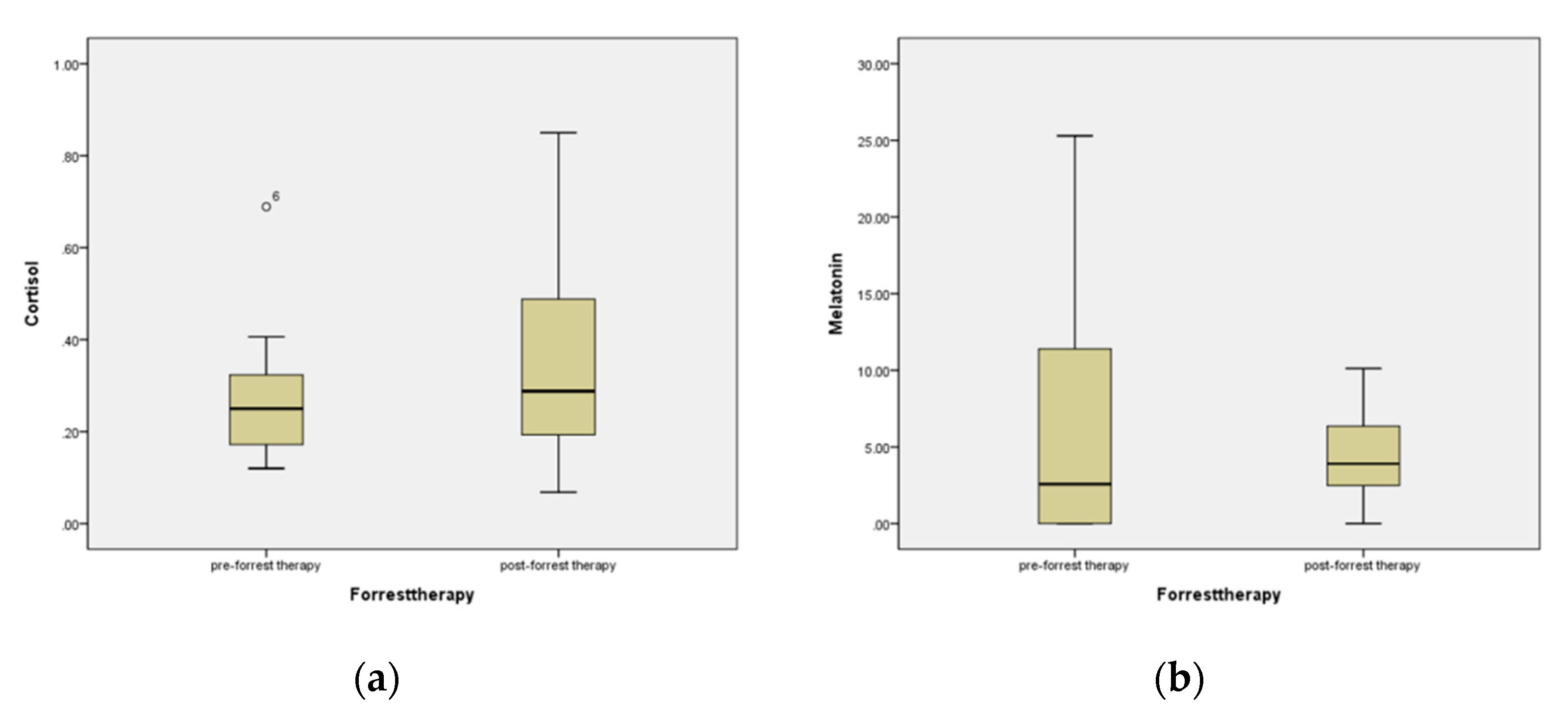
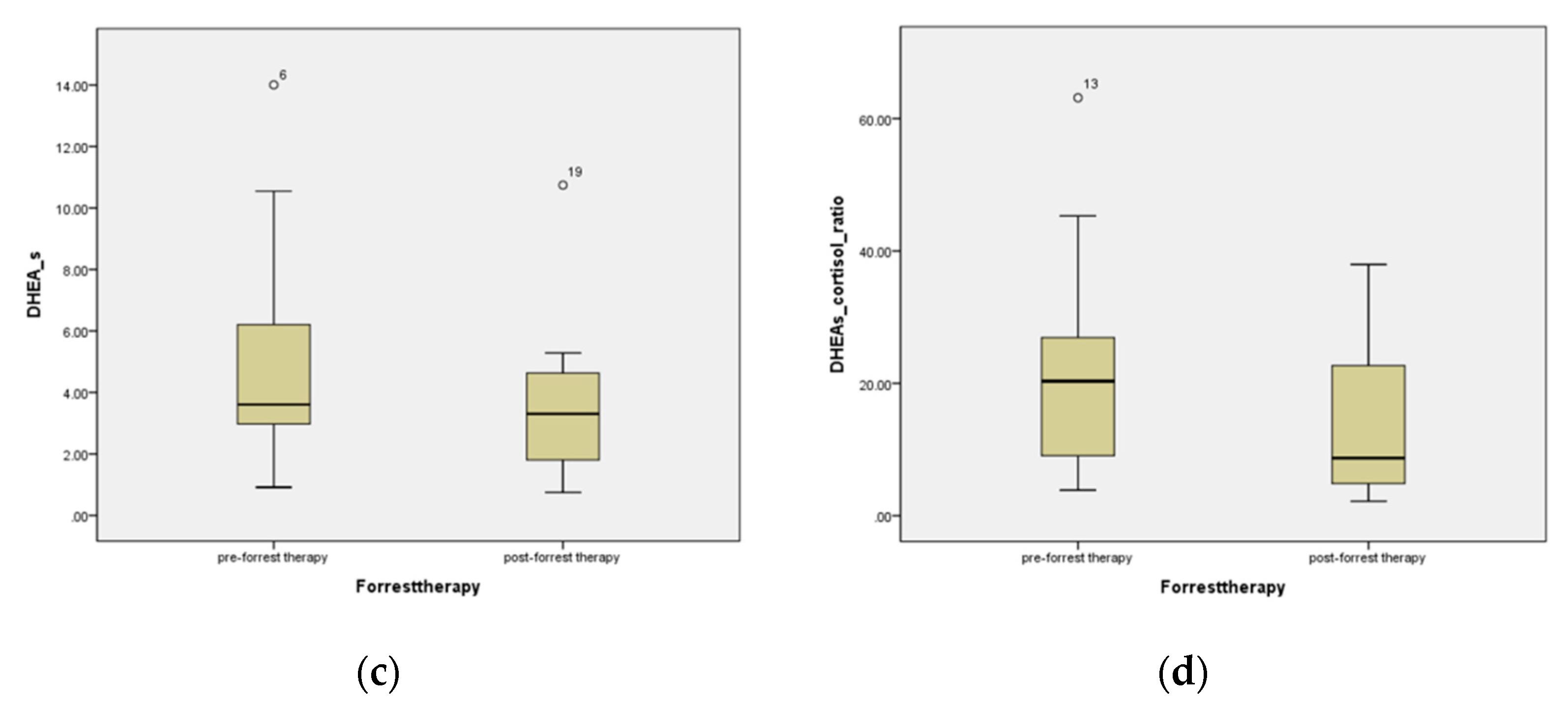
3.3. Changes of the Physiological Variables of the Participants
3.4. Satisfaction Survey
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Reicher, S.; Drury, J. Pandemic fatigue? How adherence to COVID-19 regulations has been misrepresented and why it matters. BMJ 2021, 372, n137. [Google Scholar] [CrossRef]
- Gao, J.; Zheng, P.; Jia, Y.; Chen, H.; Mao, Y.; Chen, S.; Wang, Y.; Fu, H.; Dai, J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 2020, 15, e0231924. [Google Scholar]
- Yoshioka, N.; Nomura, K.; Asayama, K.; Takenoshita, S.; Nagasawa, T.; Nakata, Y.; Hiraike, H.; Sasamori, Y.; Tsuchiya, A.; Ohkubo, T.; et al. Association between Job stress and number of physical symptoms among female nurses of medical-university-affiliated hospitals. Nihon eiseigaku zasshi. Jpn. J. Hyg. 2018, 73, 388–394. [Google Scholar] [CrossRef][Green Version]
- Oh, B.; Lee, K.J.; Zaslawski, C.; Yeung, A.; Rosenthal, D.; Larkey, L.; Back, M. Health and well-being benefits of spending time in forests: Systematic review. Environ. Health Prev. Med. 2017, 22, 71. [Google Scholar] [CrossRef]
- Song, C.; Ikei, H.; Miyazaki, Y. Physiological effects of nature therapy: A review of the research in Japan. Int. J. Environ. Res. Public Health 2016, 13, 781. [Google Scholar] [CrossRef]
- Li, Q. Effect of forest bathing trips on human immune function. Environ. Health Prev. Med. 2010, 15, 9–17. [Google Scholar] [CrossRef]
- Twohig-Bennett, C.; Jones, A. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environ. Res. 2018, 166, 628–637. [Google Scholar] [CrossRef]
- Lee, I.; Choi, H.; Bang, K.S.; Kim, S.; Song, M.; Lee, B. Effects of forest therapy on depressive symptoms among adults: A systematic review. Int. J. Environ. Res. Public Health 2017, 14, 321. [Google Scholar] [CrossRef]
- Furuyashiki, A.; Tabuchi, K.; Norikoshi, K.; Kobayashi, T.; Oriyama, S. A comparative study of the physiological and psychological effects of forest bathing (Shinrin-yoku) on working age people with and without depressive tendencies. Environ. Health Prev. Med. 2019, 24, 46. [Google Scholar] [CrossRef]
- Wang, H.; Huang, D.; Huang, H.; Zhang, J.; Guo, L.; Liu, Y.; Ma, H.; Geng, Q. The psychological impact of COVID-19 pandemic on medical staff in Guangdong, China: A cross-sectional study. Psychol. Med. 2020, 1–9. [Google Scholar] [CrossRef]
- Chen, Q.; Liang, M.; Li, Y.; Guo, J.; Fei, D.; Wang, L.; He, L.I.; Sheng, C.; Cai, Y.; Li, X.; et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e15–e16. [Google Scholar] [CrossRef]
- Azoulay, E.; De Waele, J.; Ferrer, R.; Staudinger, T.; Borkowska, M.; Povoa, P.; Iliopoulou, K.; Artigas, A.; Schaller, S.J.; Hari, M.S.; et al. Symptoms of exhaustion in intensive care unit specialists facing the COVID-19 outbreak. Ann. Intensive Care 2020, 10, 110. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Song, W.; Xia, Z.; He, Y.; Tang, L.; Hou, J.; Lei, S. Sleep disturbance and psychological profiles of medical staff and non-medical staff during the early outbreak of COVID-19 in Hubei Province, China. Front. Psychiatry 2020, 11, 733. [Google Scholar] [CrossRef] [PubMed]
- Hellhammer, D.H.; Wüst, S.; Kudielka, B.M. Salivary cortisol as a biomarker in stress research. Psychoneuroendocrinology 2009, 34, 163–171. [Google Scholar] [CrossRef]
- Dawson, D.; Encel, N. Melatonin and sleep in humans. J. Pineal Res. 1993, 15, 1–12. [Google Scholar] [CrossRef]
- Lennartsson, A.-K.; Kushnir, M.M.; Bergquist, J.; Jonsdottir, I.H. DHEA and DHEA-S response to acute psychosocial stress in healthy men and women. Biol. Psychol. 2012, 90, 143–149. [Google Scholar] [CrossRef]
- Johns, M.W. Reliability and Factor Analysis of the Epworth Sleepiness Scale. Sleep 1992, 15, 376–381. [Google Scholar] [CrossRef]
- Hoddes, E.; Zarcone, V.; Dement, W. Enzyklopädie der Schlafmedizin; Springer: Berlin/Heidelberg, Germany, 2007. [Google Scholar]
- Sohn, S.I.; Kim, D.H.; Lee, M.Y.; Cho, Y.W. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath 2012, 16, 803–812. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. Perceived stress scale. Measuring stress: A guide for health and social scientists. J. Health Soc. Behav. 1994, 10, 386–396. [Google Scholar]
- Kim, J.Y.; Seo, Y.K.; Lee, J.Y.; Kang, W.; Chee, I.S.; Choi, K.Y.; Jung, I.C. Efficacy and safety of oral SOCG in treatment of major depressive disorder: A protocol for a phase II, randomized, double-blind, placebo controlled, parallel-groups, dose finding exploratory study. Medicine 2019, 98, e16854. [Google Scholar] [CrossRef]
- Park, B.J.; Shin, C.S.; Shin, W.S.; Chung, C.Y.; Lee, S.H.; Kim, D.J.; Kim, Y.H.; Park, C.E. Effects of Forest Therapy on Health Promotion among Middle-Aged Women: Focusing on Physiological Indicators. Int. J. Environ. Res. Public Health 2020, 17, 4348. [Google Scholar] [CrossRef]
- Kim, H.; Kim, J.; Ju, H.J.; Jang, B.J.; Wang, T.K.; Kim, Y.I. Effect of Forest Therapy for Menopausal Women with Insomnia. Int. J. Environ. Res. Public Health 2020, 17, 6548. [Google Scholar] [CrossRef]
- Reiter, R.J.; Rosales-Corral, S.; Sharma, R. Circadian disruption, melatonin rhythm perturbations and their contributions to chaotic physiology. Adv. Med. Sci. 2020, 65, 394–402. [Google Scholar] [CrossRef]
- Xie, Z.; Chen, F.; Li, W.A.; Geng, X.; Li, C.; Meng, X.; Feng, Y.; Liu, W.; Yu, F. A review of sleep disorders and melatonin. Neurol. Res. 2017, 39, 559–565. [Google Scholar] [CrossRef]
- Bauducco, S.; Richardson, C.; Gradisar, M. Chronotype, circadian rhythms and mood. Curr. Opin. Psychol. 2020, 34, 77–83. [Google Scholar] [CrossRef]
- De Crescenzo, F.; Lennox, A.; Gibson, J.C.; Cordey, J.H.; Stockton, S.; Cowen, P.J.; Quested, D.J. Melatonin as a treatment for mood disorders: A systematic review. Acta Psychiatr. Scand. 2017, 136, 549–558. [Google Scholar] [CrossRef]
- Lennartsson, A.K.; Theorell, T.; Kushnir, M.M.; Bergquist, J.; Jonsdottir, I.H. Perceived stress at work is associated with attenuated DHEA-S response during acute psychosocial stress. Psychoneuroendocrinology 2013, 38, 1650–1657. [Google Scholar] [CrossRef]
- Izawa, S.; Saito, K.; Shirotsuki, K.; Sugaya, N.; Nomura, S. Effects of prolonged stress on salivary cortisol and dehydroepiandrosterone: A study of a two-week teaching practice. Psychoneuroendocrinology 2012, 37, 852–858. [Google Scholar] [CrossRef]
- Şahan, E.; Tangılntız, A. State and trait anxiety among medical staff during the first month of COVID-19 pandemic: A sample from Turkey. Int. J. Psychiatry Med. 2021, 00912174211042698. [Google Scholar] [CrossRef]
- Wang, Q.Q.; Fang, Y.Y.; Huang, H.L.; Lv, W.J.; Wang, X.X.; Yang, T.T.; Yuan, J.M.; Gao, Y.; Qian, R.L.; Zhang, Y.H. Anxiety, depression and cognitive emotion regulation strategies in Chinese nurses during the COVID-19 outbreak. J. Nurs. Manag. 2021, 29, 1263–1274. [Google Scholar] [CrossRef] [PubMed]
- Galletta, M.; Piras, I.; Finco, G.; Meloni, F.; D’Aloja, E.; Contu, P.; Campagna, M.; Portoghese, I. Worries, Preparedness, and Perceived Impact of COVID-19 Pandemic on Nurses’ Mental Health. Front. Public Health 2021, 9, 566700. [Google Scholar] [CrossRef] [PubMed]
- Heath, C.; Sommerfield, A.; von Ungern-Sternberg, B.S. Resilience strategies to manage psychological distress among healthcare workers during the COVID-19 pandemic: A narrative review. Anaesthesia 2020, 75, 1364–1371. [Google Scholar] [CrossRef]
- Hummel, S.; Oetjen, N.; Du, J.; Posenato, E.; De Almeida, R.M.R.; Losada, R.; Ribeiro, O.; Frisardi, V.; Hopper, L.; Rashid, A.; et al. Mental Health Among Medical Professionals During the COVID-19 Pandemic in Eight European Countries: Cross-sectional Survey Study. J. Med. Internet. Res. 2021, 23, e24983. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Lee, Y.W.; Ju, H.J.; Jang, B.J.; Kim, Y.I. An Exploratory Study on the Effects of Forest Therapy on Sleep Quality in Patients with Gastrointestinal Tract Cancers. Int. J. Environ. Res. Public Health 2019, 16, 2449. [Google Scholar] [CrossRef]

| Program | Contents |
|---|---|
| Outdoor activities | Activities that awaken the five senses by immersion in elements of the forest, such as sound, scenery, and air while walking on a forest path |
| Dry foot bath | Activities that use a dry cypress foot bath to warm the feet to relieve foot fatigue and enhance blood circulation |
| Drinking tea conversation | Activities focusing on the enjoyment of the color, smell, and taste of tea while drinking tea, and talking with the participants in a comfortable atmosphere |
| Woodworking | Activities promoting a sense of immersion and accomplishment while using a burning machine to engrave favorite sentences, pictures, etc., onto wood carvings |
| Warm-up exercises | Activities that relieve tension by slowly relaxing the muscles of the entire body |
| Walking | Activities that give rest to the mind while taking a walk in the forest |
| Singing bowl meditation | Activities used to empty the head and calm the mind and body while meditating using a singing bowl |
| N (%)/Mean ± SD | Min | Max | |
|---|---|---|---|
| Age (year) | 42.23 ± 10.99 | 23.00 | 58.00 |
| Sex (female/male) | 11/2 (84.6/15.4) | ||
| Height (cm) | 160.5 ± 5.3 | 152.0 | 171.0 |
| Weight (kg) | 56.8 ± 6.1 | 50.0 | 70.5 |
| BMI (cm/kg2) | 22.1 ± 2.2 | 19.7 | 26.0 |
| Pre | Post | Diff (Post-Pre) | Z | p | |
|---|---|---|---|---|---|
| Sleep onset time (min) | 33.46 ± 19.94 | 42.69 ± 38.00 | 9.23 ± 26.05 | 1.06 | 0.291 |
| Sleep duration (min) | 332.31 ± 56.74 | 373.85 ± 61.99 | 41.54 ± 46.70 | −2.54 | 0.011 |
| PSQI-K | 8.00 ± 2.38 | 6.85 ± 2.61 | −1.15 ± 2.15 | −1.72 | 0.086 |
| ISI | 8.62 ± 3.01 | 8.54 ± 4.72 | −0.08 ± 3.73 | −0.102 | 0.918 |
| SSS | 2.62 ± 1.50 | 2.08 ± 0.49 | −0.54 ± 1.27 | −1.51 | 0.131 |
| ESS | 7.38 ± 3.48 | 8.46 ± 3.57 | 1.08 ± 3.01 | −0.99 | 0.324 |
| HADS | 12.08 ± 6.01 | 9.69 ± 6.56 | −2.38 ± 4.19 | −1.84 | 0.066 |
| PSS | 30.92 ± 4.19 | 28.23 ± 5.00 | −2.69 ± 3.73 | −2.25 | 0.025 |
| Somatization symptoms (KSCL95) | 14.23 ± 7.67 | 13.15 ± 9.06 | −1.08 ± 6.45 | −0.60 | 0.552 |
| Pre | Post | Diff (Post-Pre) | Z | p | |
|---|---|---|---|---|---|
| Cortisol | 0.28 ± 0.15 | 0.37 ± 0.25 | 0.09 ± 0.27 | 0.87 | 0.279 |
| Melatonin | 7.74 ± 9.86 | 4.55 ± 3.03 | −3.32 ± 10.53 | −0.63 | 0.530 |
| DHEA-s | 5.09 ± 3.92 | 3.67 ± 2.59 | −1.42 ± 2.07 | −2.06 | 0.039 |
| Ratio of DHEA-s/Cortisol | 20.92 ± 17.55 | 14.91 ± 12.72 | −6.01 ± 20.06 | −1.08 | 0.279 |
| Mean ± SD | |
|---|---|
| Satisfaction | |
| Overall | 4.23 ± 0.599 |
| Outdoor activities | 4.46 ± 0.877 |
| Dry foot bath | 4.54 ± 0.660 |
| Drinking tea-conversation | 4.46 ± 0.776 |
| Woodworking | 4.46 ± 0.519 |
| Warm-up exercise | 4.46 ± 0.519 |
| Walking | 4.46 ± 0.660 |
| Singing bowl meditation | 4.15 ± 0.801 |
| Intention to Re-Participation | |
| Outdoor activities | 4.23 ± 0.927 |
| Dry foot bath | 4.46 ± 0.660 |
| Drinking tea conversation | 4.38 ± 0.768 |
| Woodworking | 4.00 ± 0.070 |
| Warm-up exercise | 4.00 ± 0.707 |
| Walking | 4.31 ± 0.751 |
| Singing bowl meditation | 3.92 ± 0.954 |
| Intention to Recommend to Others | |
| Outdoor activities | 4.31 ± 0.947 |
| Dry foot bath | 4.38 ± 0.650 |
| Drinking tea conversation | 4.38 ± 0.650 |
| Woodworking | 4.15 ± 0.801 |
| Warm-up exercise | 4.23 ± 0.725 |
| Walking | 4.38 ± 0.768 |
| Singing bowl meditation | 4.15 ± 0.801 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.; Choi, Y.; Kim, H. Positive Effects on Emotional Stress and Sleep Quality of Forest Healing Program for Exhausted Medical Workers during the COVID-19 Outbreak. Int. J. Environ. Res. Public Health 2022, 19, 3130. https://doi.org/10.3390/ijerph19053130
Kim Y, Choi Y, Kim H. Positive Effects on Emotional Stress and Sleep Quality of Forest Healing Program for Exhausted Medical Workers during the COVID-19 Outbreak. International Journal of Environmental Research and Public Health. 2022; 19(5):3130. https://doi.org/10.3390/ijerph19053130
Chicago/Turabian StyleKim, Yunsoo, Yoonhee Choi, and Hyeyun Kim. 2022. "Positive Effects on Emotional Stress and Sleep Quality of Forest Healing Program for Exhausted Medical Workers during the COVID-19 Outbreak" International Journal of Environmental Research and Public Health 19, no. 5: 3130. https://doi.org/10.3390/ijerph19053130
APA StyleKim, Y., Choi, Y., & Kim, H. (2022). Positive Effects on Emotional Stress and Sleep Quality of Forest Healing Program for Exhausted Medical Workers during the COVID-19 Outbreak. International Journal of Environmental Research and Public Health, 19(5), 3130. https://doi.org/10.3390/ijerph19053130








