The Effect of Task-Oriented Training on Upper-Limb Function, Visual Perception, and Activities of Daily Living in Acute Stroke Patients: A Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval
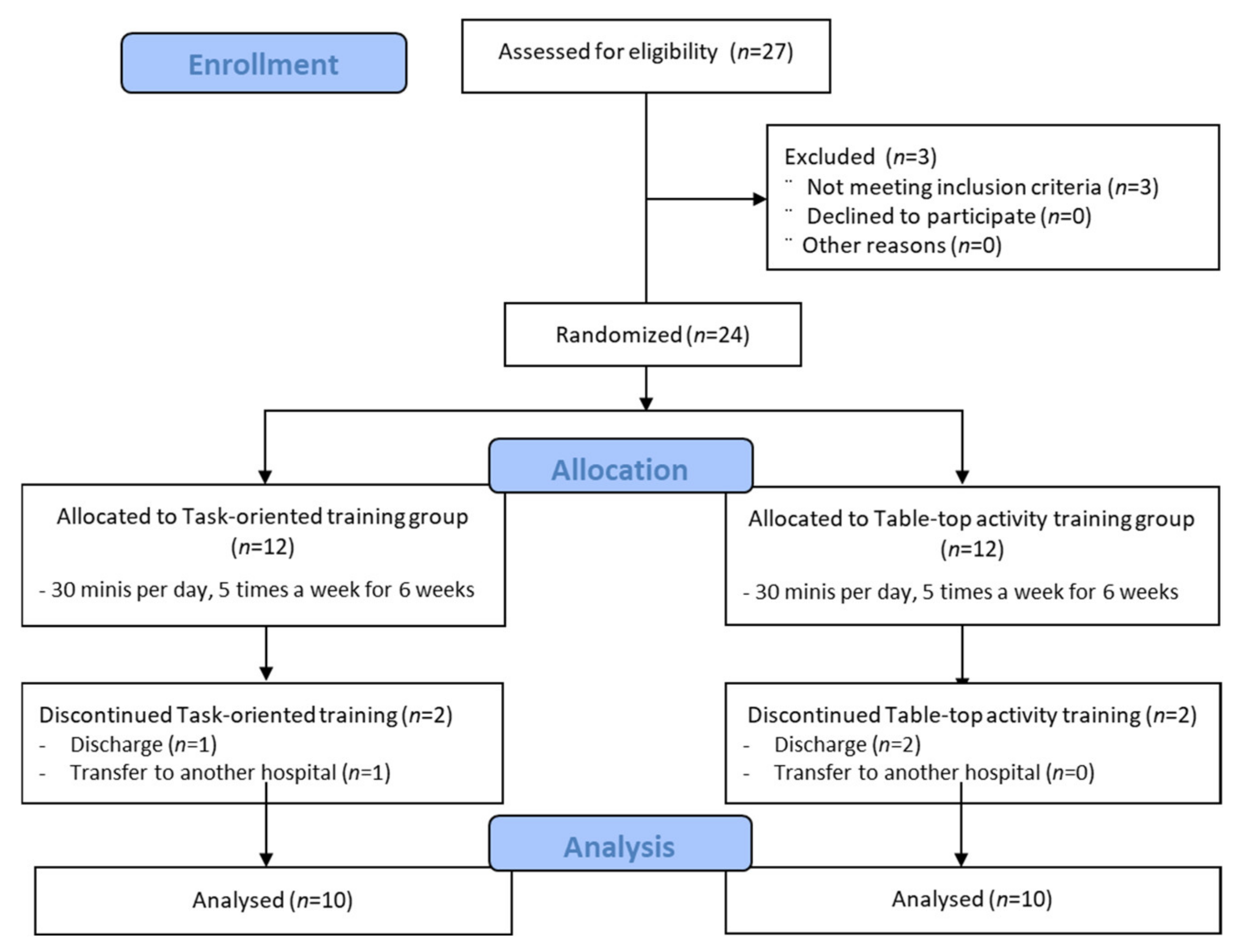
2.2. Subjects
2.3. Procedure
2.4. Outcome Measurements
2.4.1. Manual Function Test
2.4.2. Motor-Free Visual Perception Test—Vertical
2.4.3. Korean-Modified Barthel Index
2.5. Intervention
2.5.1. Task-Oriented Training Program
2.5.2. Table-Top Activity Training Program
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Korea, V.S.D.S.; Shin, H.-Y.; Kim, J.; Lee, S.; Park, M.S.; Park, S.; Huh, S. Cause-of-death statistics in 2018 in the Republic of Korea. J. Korean Med. Assoc. 2020, 63, 286–297. [Google Scholar] [CrossRef]
- Kim, J.Y.; Kang, K.; Kang, J.; Koo, J.; Kim, D.-H.; Kim, B.J.; Kim, W.-J.; Kim, E.-G.; Kim, J.G.; Kim, J.-M.; et al. Executive Summary of Stroke Statistics in Korea 2018: A Report from the Epidemiology Research Council of the Korean Stroke Society. J. Stroke 2019, 21, 42–59. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.J.; Tung, W.L.; Wu, W.L.; Su, F.C. Effect of bilateral reaching on affected arm motor control in stroke--with and without loading on unaffected arm. Disabil. Rehabil. 2006, 28, 1507–1516. [Google Scholar] [CrossRef]
- Srinayanti, Y.; Widianti, W.; Andriani, D.; Firdaus, F.A.; Setiawan, H.J.I.J.o.N.; Services, H. Range of Motion Exercise to Improve Muscle Strength among Stroke Patients: A Literature Review. Int. J. Nurs. Health Serv. 2021, 4, 332–343. [Google Scholar] [CrossRef]
- Yoo, D.H.; Kim, S.Y. Effects of upper limb robot-assisted therapy in the rehabilitation of stroke patients. J. Phys. Ther. Sci. 2015, 27, 677–679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shimojo, S.; Paradiso, M.; Fujita, I. What visual perception tells us about mind and brain. Proc. Natl. Acad. Sci. USA 2001, 98, 12340–12341. [Google Scholar] [CrossRef] [Green Version]
- Berryhill, M.E.; Fendrich, R.; Olson, I.R. Impaired distance perception and size constancy following bilateral occipitoparietal damage. Exp. Brain Res. 2009, 194, 381–393. [Google Scholar] [CrossRef] [Green Version]
- Tatler, B.W.; Land, M.F. Vision and the representation of the surroundings in spatial memory. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2011, 366, 596–610. [Google Scholar] [CrossRef] [Green Version]
- Michaelsen, S.M.; Dannenbaum, R.; Levin, M.F.J.S. Task-specific training with trunk restraint on arm recovery in stroke: Randomized control trial. Stroke 2006, 37, 186–192. [Google Scholar] [CrossRef] [Green Version]
- Webster, M.A. Visual Adaptation. Annu. Rev. Vis. Sci. 2015, 1, 547–567. [Google Scholar] [CrossRef] [Green Version]
- Buccino, G.; Solodkin, A.; Small, S.L.J.C. Functions of the mirror neuron system: Implications for neurorehabilitation. Cogn. Behav. Neurol. 2006, 19, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Jeon, H.E.; Park, C.H. Relationship between Visual Perception and Microstructural Change of the Superior Longitudinal Fasciculus in Patients with Brain Injury in the Right Hemisphere: A Preliminary Diffusion Tensor Tractography Study. Diagnostics 2020, 10, 641. [Google Scholar] [CrossRef] [PubMed]
- Rowe, F. Visual perceptual consequences of stroke. Strabismus 2009, 17, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Vossel, S.; Weiss, P.H.; Eschenbeck, P.; Fink, G.R. Anosognosia, neglect, extinction and lesion site predict impairment of daily living after right-hemispheric stroke. Cortex J. Devoted Study Nerv. Syst. Behav. 2013, 49, 1782–1789. [Google Scholar] [CrossRef] [PubMed]
- Shumway-Cook, A.; Woollacott, M.H. Motor Control: Translating Research into Clinical Practice; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2007. [Google Scholar]
- Sheng, B.; Lin, M. A longitudinal study of functional magnetic resonance imaging in upper-limb hemiplegia after stroke treated with constraint-induced movement therapy. Brain Inj. 2009, 23, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.B.; Lim, S.H.; Kim, K.H.; Kim, K.J.; Kim, Y.R.; Chang, W.N.; Yeom, J.W.; Kim, Y.D.; Hwang, B.Y. Six-month functional recovery of stroke patients: A multi-time-point study. Int. J. Rehabil. Res. 2015, 38, 173–180. [Google Scholar] [CrossRef] [Green Version]
- Dobkin, B.H. Clinical practice. Rehabilitation after stroke. N. Engl. J. Med. 2005, 352, 1677–1684. [Google Scholar] [CrossRef] [Green Version]
- Hashimoto, K.; Higuchi, K.; Nakayama, Y.; Abo, M.J.N. Ability for basic movement as an early predictor of functioning related to activities of daily living in stroke patients. Neurorehabilit. Neural Repair 2007, 21, 353–357. [Google Scholar] [CrossRef]
- Woo, H.; Chang, K.; Park, W.K. The effects of mirror therapy on the hand function recovery in chronic stroke patients. J. Korean Soc. Occup. Ther. 2011, 19, 93–103. [Google Scholar]
- Choi, J.U.; Kang, S.H. The effects of patient-centered task-oriented training on balance activities of daily living and self-efficacy following stroke. J. Phys. Ther. Sci. 2015, 27, 2985–2988. [Google Scholar] [CrossRef] [Green Version]
- Yoo, C.; Park, J. Impact of task-oriented training on hand function and activities of daily living after stroke. J. Phys. Ther. Sci. 2015, 27, 2529–2531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.; Yoo, C. Effects of task-oriented training on upper extremity function and performance of daily activities by chronic stroke patients. J. Phys. Ther. Sci. 2015, 27, 2657–2659. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guy, C.J.P. Stroke Rehabilitation. Lancet 2003, 89, 260. [Google Scholar] [CrossRef]
- Piemonte, M.; Okamoto, E.; Cardoso, C.; Tatiana de Paula Oliveira, M.; Miranda, C.J.J.N.P. A comparison between task oriented and client-centred task-oriented approaches to improve upper limb functioning in people with sub-acute stroke. J. Nov. Physiother. 2015, 5, 2. [Google Scholar]
- Maier, M.; Ballester, B.R.; Verschure, P.F.M.J. Principles of Neurorehabilitation After Stroke Based on Motor Learning and Brain Plasticity Mechanisms. Front. Syst. Neurosci. 2019, 13, 74. [Google Scholar] [CrossRef]
- Pomeroy, V.; Aglioti, S.M.; Mark, V.W.; McFarland, D.; Stinear, C.; Wolf, S.L.; Corbetta, M.; Fitzpatrick, S.M. Neurological principles and rehabilitation of action disorders: Rehabilitation interventions. Neurorehabil. Neural. Repair 2011, 25, 33S–43S. [Google Scholar] [CrossRef] [Green Version]
- Muratori, L.M.; Lamberg, E.M.; Quinn, L.; Duff, S.V. Applying principles of motor learning and control to upper extremity rehabilitation. J. Hand Ther. 2013, 26, 94–103. [Google Scholar] [CrossRef] [Green Version]
- Rensink, M.; Schuurmans, M.; Lindeman, E.; Hafsteinsdottir, T. Task-oriented training in rehabilitation after stroke: Systematic review. J. Adv. Nurs. 2009, 65, 737–754. [Google Scholar] [CrossRef]
- Dromerick, A.W.; Edwards, D.F.; Hahn, M.J.S. Does the application of constraint-induced movement therapy during acute rehabilitation reduce arm impairment after ischemic stroke? Stroke 2000, 31, 2984–2988. [Google Scholar] [CrossRef] [Green Version]
- Van Peppen, R.P.; Kwakkel, G.; Wood-Dauphinee, S.; Hendriks, H.J.; Van der Wees, P.J.; Dekker, J. The impact of physical therapy on functional outcomes after stroke: What’s the evidence? Clin. Rehabil. 2004, 18, 833–862. [Google Scholar] [CrossRef]
- Lee, G.-D. The Effect of Task Oriented Circuit Training in Upper Extremity Function and Self-Efficacy in a Chronic Stroke Patient; Gachon University: Incheon, Korea, 2017. [Google Scholar]
- Miyamoto, S.; Kondo, T.; Suzukamo, Y.; Michimata, A.; Izumi, S. Reliability and validity of the Manual Function Test in patients with stroke. Am. J. Phys. Med. Rehabil. 2009, 88, 247–255. [Google Scholar] [CrossRef]
- Mercier, L.; Hebert, R.; Colarusso, R.; Hammill, D.J.N. Motor-Free Visual Perception Test: Vertical; Academy Therapy Publication: Novato, CA, USA, 1997. [Google Scholar]
- Mercier, L.; Desrosiers, J.; Hébert, R.; Rochette, A.; Dubois, M.-F.J.P.; Geriatrics, O.T. Normative data for the motor-free visual perception test-vertical. Phys. Occup. Ther. Geriatr. 2001, 19, 39–50. [Google Scholar] [CrossRef]
- Gillen, G. Cognitive and Perceptual Rehabilitation: Optimizing Function; Elsevier Health Sciences: Amsterdam, The Netherlands, 2008. [Google Scholar]
- Shah, S.; Vanclay, F.; Cooper, B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J. Clin. Epidemiol. 1989, 42, 703–709. [Google Scholar] [CrossRef]
- Jung, H.Y.; Park, B.K.; Shin, H.S.; Kang, Y.K.; Pyun, S.B.; Paik, N.J.; Kim, S.H.; Kim, T.H.; Han, T.R. Development of the Korean version of Modified Barthel Index (K-MBI): Multi-center study for subjects with stroke. J. Korean Acad. Rehabil. Med. 2007, 31, 283–297. [Google Scholar]
- French, B.; Thomas, L.H.; Coupe, J.; McMahon, N.E.; Connell, L.; Harrison, J.; Sutton, C.J.; Tishkovskaya, S.; Watkins, C.L. Repetitive task training for improving functional ability after stroke. Cochrane Database Syst. Rev. 2016, 11, CD006073. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Janet, H.C.; Roberta, B.S. Stroke Stroke Rehabilitation Guidelines for Exercise and Training to Optimize Motor Skill; Butierwortii-Heinemann: Oxford, UK, 2003. [Google Scholar]
- Son, J.-R. The Effect of Task Oriented Activities of Daily Living Training on Upper Extremity Function and Quality of Life in Patient with Stroke; Gachon University: Incheon, Korea, 2015. [Google Scholar]
- Sung, K.-S. The Effect of Patients-Selected Task-Oriented Training on Activities of Daily Living and Quality of Life in Stroke Patients’ Life Time Use; Gachon University: Incheon, Korea, 2016. [Google Scholar]
- Shepherd, R.B. Exercise and training to optimize functional motor performance in stroke: Driving neural reorganization? Neural Plast. 2001, 8, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Lang, C.E.; Wagner, J.M.; Bastian, A.J.; Hu, Q.; Edwards, D.F.; Sahrmann, S.A.; Dromerick, A.W. Deficits in grasp versus reach during acute hemiparesis. Exp. Brain Res. 2005, 166, 126–136. [Google Scholar] [CrossRef] [PubMed]
- Langhorne, P.; Coupar, F.; Pollock, A. Motor recovery after stroke: A systematic review. Lancet Neurol. 2009, 8, 741–754. [Google Scholar] [CrossRef]
- Kim, K.Y.; Lee, J.-S.; Park, J.-H. The effects of selective task-oriented training of stroke patients on upper extremity functions and activity of daily living. Korean Soc. Med. Ther. Sci. 2015, 7, 15–28. [Google Scholar]
- Ma, S.-R.; Jung, S.-M.; Park, J.-J. The effect of the task-oriented activities on balance and activities of daily living performance in the stroke patients. JKEIA 2015, 9, 1. [Google Scholar] [CrossRef]
- Lee, J.-H. The Effect of Task-Oriented Movement Therapy on Upper Motor Function, Patterns and Reorganization of Motor Network for Stroke Patients; Daegu University: Daegu, Korea, 2002. [Google Scholar]
- Mercier, L.; Audet, T.; Hébert, R.; Rochette, A.; Dubois, M.F. Impact of motor, cognitive, and perceptual disorders on ability to perform activities of daily living after stroke. Stroke 2001, 32, 2602–2608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Case-Smith, J.; O’Brien, J.C. Occupational Therapy for Children and Adolescents-e-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Radomski, M.V.; Latham, C.A.T. Occupational Therapy for Physical Dysfunction; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2008. [Google Scholar]
- Lee, H.-S.; Lee, D.-J.; Yoo, K.-T. The Effect of Task-Oriented Program on the Visual Perception, Standing Balance and Activities of Daily Living in the patients with Stroke. Off. J. Korean Acad. Kinesiol. 2011, 13, 11–20. [Google Scholar]
- Gu, Y.; Kim, B. An Impact of Action-Observation Training and Task-Oriented Training on Activities of Daily Living of Stroke Patients. J. Korean Soc. Integr. Med. 2013, 1, 19–28. [Google Scholar] [CrossRef]
- Heo, M. The Effect of Task-Oriented Upper Extremity Exercise Program on Arm Function and Activities of Daily Living for Inpatients Stroke Patients. J. Korean Entertain. Ind. 2013, 5, 152–157. [Google Scholar]
- Jung, J.-H. The Effect of Task-Oriented Movement Therapy on Upper Extremity, Upper Extremity Function and Activities of Daily Living for Stroke Patients; Daegu University: Daegu, Korea, 2009. [Google Scholar]
| Task | Task-Oriented Training Program |
|---|---|
| Taking out a drink from the refrigerator and pouring it into a cup | Open the refrigerator door, take out a liquid-containing bottle, put it on the counter next to the refrigerator, close the refrigerator door, and pour the drink into a cup. (The difficulty level was controlled by varying the size of the bottle and the volume of the drink.) |
| Washing a cup | Wash the cup using dish soap and a sponge. (The difficulty level was controlled by varying the cup or tumbler size.) |
| Cleaning with a vacuum cleaner | Clean the dust off a floor, curtain, and furniture. (The difficulty level was controlled by instructing patients to lift the vacuum cleaner while vacuuming the floor to vacuuming an item located at a higher level, such as a curtain.) |
| Folding towels and stacking them | Sit on a chair and fold towels on a table and stack them. (The difficulty level was controlled by instructing patients to fold towels using both hands or one hand and to sit or stand while performing the task.) |
| Using a pair of chopsticks | Use Edison training chopsticks to grab a block (1 × 1 cm), a bean, and a pin. (The difficulty level was controlled by progressively using Edison training chopsticks, wooden chopsticks, stainless steel chopsticks, and Chinese-style chopsticks with a thick end.) |
| Task | Occupational Therapy Program |
|---|---|
| Stacking cones | Lift a cone with one hand and stack it on top of a fixed cone. (The difficulty level was controlled by using resistance bands of varying weights or instructing patients to sit or stand while performing the task.) |
| Stacking 3 × 3 cm blocks | Pick up blocks one at a time by using one hand and stack them. (The difficulty level was controlled by using resistance bands of varying weights.) |
| Tailwind | Use both hands to push the handles of an instrument up and down to the sounds of a metronome. (The difficulty level was controlled by varying the angle.) |
| Pinch exerciser | Take a pinch pin and put it on a rod. (The difficulty level was controlled by varying the resistance of the pinch pin (5 grades) and the diameter of the rod (3 grades).) |
| O’Connor Tweezer Dexterity Test | Pick up a pin (2.5 cm long) and put it in a 15 mm hole. (The difficulty level was controlled by using different tweezers.) |
| Task-Oriented Training (n = 10) | Table-Top Activity Training (n = 10) | p | |
|---|---|---|---|
| Age (years) | 54.4 ± 12.7 | 59.8 ± 8.29 | 0.277 |
| Sex, Females, n (%) | 2 (20.0) | 3 (30.0) | 0.606 |
| Stroke type | |||
| Infarction, n (%) | 5 (50.0) | 8 (80.0) | 0.160 |
| Hemorrhage, n (%) | 5 (50.0) | 2 (20.0) | |
| Affected side, left, n (%) | 4 (40.0) | 7 (70.0) | 0.178 |
| Onset (months) | 1.2 ± 0.4 | 1.6 ± 0.5 | 0.074 |
| K-MMSE (scores) | 25.7 ± 3.5 | 27.0 ± 1.8 | 0.308 |
| NIHSS | 3.1 ± 1.1 | 2.5 ± 1.4 | 0.380 |
| MFT | 56.6 ± 12.9 | 58.4 ± 11.0 | 0.741 |
| K-MBI | 55.9 ± 14.4 | 59.2 ± 14.5 | 0.615 |
| MVPT-V | 27.8 ± 2.0 | 28.3 ± 1.3 | 0.646 |
| Task-Oriented Training (n = 10) | Table-Top Activity Training (n = 10) | Group × Time Interaction F (p) | Main Effect of Group F (p) | ||
|---|---|---|---|---|---|
| MFT | Pretest | 56.6 ± 12.9 | 58.4 ± 11.0 | 36.9 (<0.001) | 1.40 (0.251) |
| Post-test | 79.4 ± 11.6 | 65.0 ± 13.4 | |||
| d † | 1.859 * | 0.538 * | |||
| K-MBI | Pretest | 55.9 ± 14.4 | 59.2 ± 14.5 | 7.65 (0.013) | 0.20 (0.657) |
| Post-test | 80.9 ± 12.3 | 72.5 ± 12.6 | |||
| d † | 1.867 * | 0.979 * | |||
| MVPT-V | Pretest | 27.8 ± 2.0 | 28.3 ± 1.3 | 2.37 (0.141) | 0.12 (0.735) |
| Post-test | 32.7 ± 2.5 | 31.7 ± 1.9 | |||
| d † | 2.164 * | 2.089 * | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, W. The Effect of Task-Oriented Training on Upper-Limb Function, Visual Perception, and Activities of Daily Living in Acute Stroke Patients: A Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 3186. https://doi.org/10.3390/ijerph19063186
Choi W. The Effect of Task-Oriented Training on Upper-Limb Function, Visual Perception, and Activities of Daily Living in Acute Stroke Patients: A Pilot Study. International Journal of Environmental Research and Public Health. 2022; 19(6):3186. https://doi.org/10.3390/ijerph19063186
Chicago/Turabian StyleChoi, Wonho. 2022. "The Effect of Task-Oriented Training on Upper-Limb Function, Visual Perception, and Activities of Daily Living in Acute Stroke Patients: A Pilot Study" International Journal of Environmental Research and Public Health 19, no. 6: 3186. https://doi.org/10.3390/ijerph19063186
APA StyleChoi, W. (2022). The Effect of Task-Oriented Training on Upper-Limb Function, Visual Perception, and Activities of Daily Living in Acute Stroke Patients: A Pilot Study. International Journal of Environmental Research and Public Health, 19(6), 3186. https://doi.org/10.3390/ijerph19063186





