COVID-19 Vaccine Hesitancy: The Role of Information Sources and Beliefs in Dutch Adults
Abstract
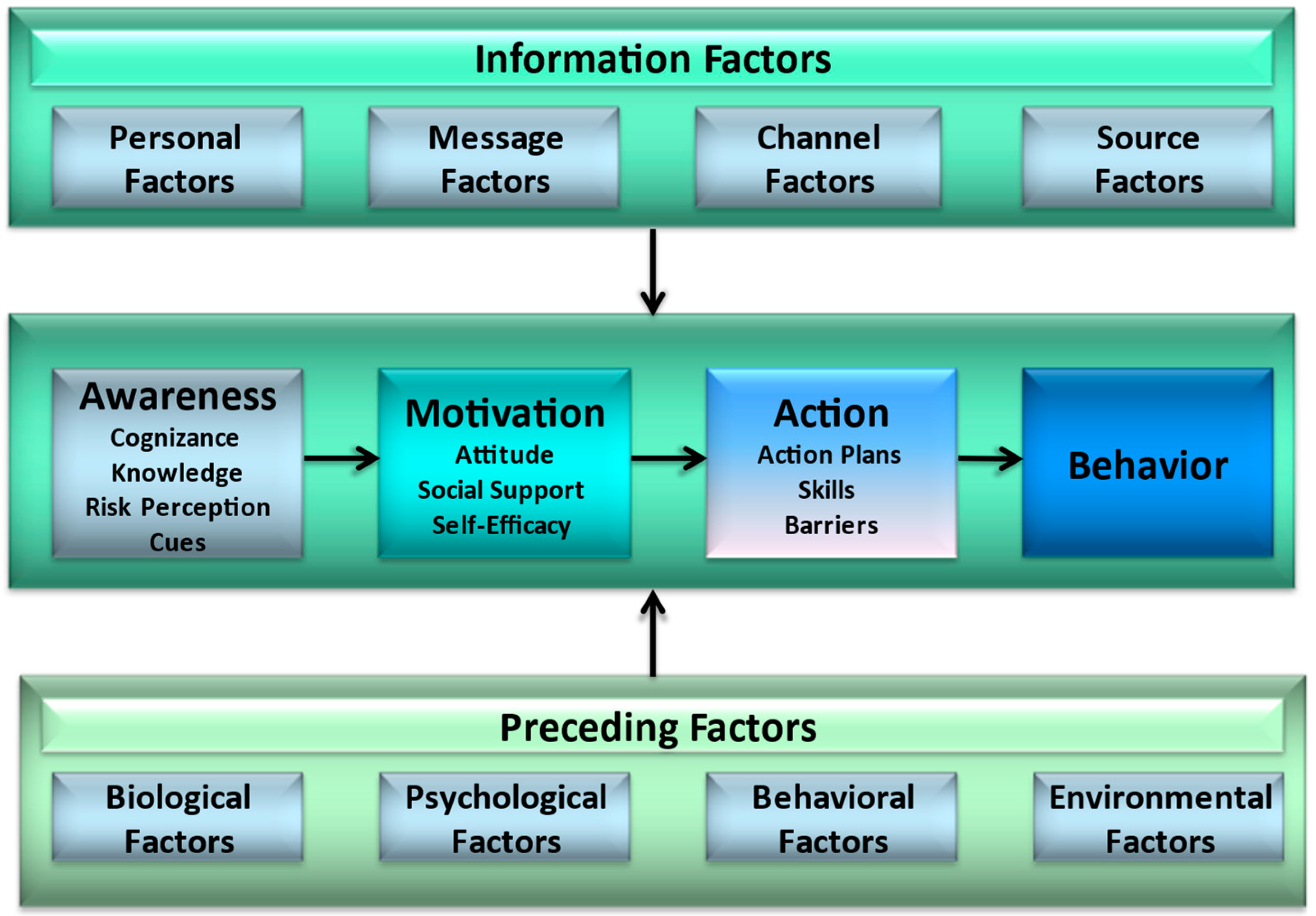
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Study Population
2.3. Questionnaire
2.3.1. Vaccine Hesitancy
2.3.2. Socio-Demographic Factors
2.3.3. Information Seeking Behaviour and Quality Checking Intentions
2.3.4. Awareness Factors
2.3.5. Motivational Factors
2.4. Data Analysis
3. Results
3.1. Respondent Characteristics
3.2. Differences in Socio-Demographic Factors
3.3. Differences in Information Seeking Behaviour
3.4. Differences in Awareness
| Mean (SD) | F | p | Post-Hoc | ||||
|---|---|---|---|---|---|---|---|
| Total (n = 240) | Hesitant (n = 58) | Somewhat Hesitant (n = 69) | Non-Hesitant (n = 113) | ||||
| COVID vaccines can infect you with COVID (false) | 0.84 (0.37) | 0.71 (0.46) | 0.91 (0.28) | 0.87 (0.34) | 5.75 | 0.00 | H < S, N |
| Pregnant women are not advised to get vaccinated 1 (true) | 0.55 (0.50) | 0.62 (0.49) | 0.61 (0.49) | 0.47 (0.50) | 2.57 | 0.08 | n/a |
| COVID vaccines often have severe side-effects (false) | 0.94 (0.24) | 0.81 (0.40) | 0.97 (0.17) | 0.99 (0.10) | 13.37 | 0.00 | H < S, N |
| If enough people get vaccinated, the virus will spread less easily (true) | 0.91 (0.28) | 0.76 (0.43) | 1.00 (0.00) | 0.94 (0.24) | 13.62 | 0.00 | H < S, N |
| Getting vaccinated against COVID is more dangerous than getting infected with COVID (false) | 0.97 (0.18) | 0.86 (0.35) | 1.00 (0.00) | 1.00 (0.00) | 14.38 | 0.00 | H < S, N |
| COVID vaccines have been tested extensively (true) | 0.81 (0.39) | 0.47 (0.50) | 0.88 (0.32) | 0.95 (0.23) | 40.88 | 0.00 | H < S, N |
| COVID vaccines are deemed safe to use (true) | 0.87 (0.34) | 0.55 (0.50) | 0.94 (0.24) | 0.98 (0.13) | 45.19 | 0.00 | H < S, N |
| How high do you estimate your chance of getting COVID? | −0.17 (1.07) | −0.34 (1.10) | 0.10 (1.03) | −0.25 (1.04) | 3.41 | 0.04 | n/a |
| How high do you estimate your chance of getting seriously sick of a COVID-infection? | −0.70 (1.27) | −0.76 (1.29) | −0.39 (1.29) | −0.86 (1.22) | 3.06 | 0.05 | S > N |
| How high do you estimate your chance of getting permanent damage from a COVID-infection? | −0.55 (1.24) | −0.55 (1.23) | −0.26 (1.21) | −0.73 (1.24) | 3.06 | 0.05 | S > N |
| How high do you estimate your chance of dying from a COVID-infection? | −1.66 (1.30) | −1.50 (1.22) | −1.72 (1.28) | −1.71 (1.35) | 0.60 | 0.55 | n/a |
| How bad would you mind getting COVID? | 0.59 (1.26) | 0.36 (1.28) | 0.71 (1.26) | 0.63 (1.23) | 1.33 | 0.27 | n/a |
| How bad would you mind getting seriously sick of a COVID-infection? | 1.80 (1.00) | 1.31 (1.27) | 2.04 (0.74) | 1.91 (0.90) | 10.43 | 0.00 | H < S, N |
| How bad would you mind getting permanent damage from a COVID-infection? | 2.40 (0.75) | 2.21 (0.93) | 2.51 (0.59) | 2.42 (0.72) | 2.75 | 0.07 | n/a |
| How bad would you mind dying from a COVID-infection? | 2.61 (0.97) | 2.33 (1.21) | 2.75 (0.70) | 2.67 (0.97) | 3.49 | 0.03 | H < S |
| I know people that got seriously sick of COVID | 0.70 (0.46) | 0.60 (0.49) | 0.72 (0.45) | 0.73 (0.45) | 1.54 | 0.22 | n/a |
| I got infected with COVID myself | 0.17 (0.37) | 0.26 (0.44) | 0.14 (0.36) | 0.13 (0.34) | 2.37 | 0.10 | n/a |
| I read a lot of news about the severity of COVID recently | 0.73 (0.45) | 0.60 (0.49) | 0.77 (0.43) | 0.77 (0.42) | 3.10 | 0.05 | n/a |
| I saw a lot of news about advantages of COVID vaccines recently | 0.75 (0.43) | 0.60 (0.49) | 0.72 (0.45) | 0.85 (0.36) | 6.77 | 0.00 | H < N |
| I saw a lot of news about dangers of COVID vaccines recently | 0.64 (0.48) | 0.69 (0.47) | 0.67 (0.48) | 0.60 (0.49) | 0.77 | 0.46 | n/a |
3.5. Motivational Factors
| Mean (SD) | F | p | η2 | Post-Hoc | ||||
|---|---|---|---|---|---|---|---|---|
| Total (n = 240) | Hesitant (n = 58) | Somewhat Hesitant (n = 69) | Non-Hesitant (n = 113) | |||||
| Attitude Pro Rational; If I get vaccinated against COVID-19 1: | ||||||||
| It will protect people around me from getting COVID | 1.57 (1.61) | 0.78 (1.84) | 1.81 (1.22) | 1.83 (1.58) | 10.05 | 0.00 | 0.08 | H < S, N |
| It will protect me from getting COVID | 1.74 (1.44) | 1.03 (1.65) | 2.07 (1.09) | 1.90 (1.40) | 10.25 | 0.00 | 0.08 | H < S, N |
| It will help to hinder the further spread of COVID | 1.88 (1.42) | 0.98 (1.72) | 2.12 (1.13) | 2.20 (1.21) | 17.58 | 0.00 | 0.13 | H < S, N |
| Normal life will return sooner | 1.87 (1.47) | 0.79 (1.86) | 2.12 (1.08) | 2.27 (1.15) | 24.87 | 0.00 | 0.17 | H < S, N |
| I can go on a holiday again soon | 1.26 (1.46) | 0.57 (1.68) | 1.30 (1.33) | 1.58 (1.30) | 10.00 | 0.00 | 0.08 | H < S, N |
| It will contribute against the evolution of new virus variants | 0.81 (1.79) | −0.12 (1.93) | 0.90 (1.67) | 1.24 (1.61) | 12.27 | 0.00 | 0.09 | H < S, N |
| The economy will be able to recover sooner | 1.69 (1.30) | 0.91 (1.74) | 1.74 (1.00) | 2.06 (1.01) | 16.97 | 0.00 | 0.13 | H < S, N |
| Attitude Pro Emotional; If I get vaccinated against COVID-19: | ||||||||
| I will feel safe | 1.26 (1.45) | 0.12 (1.84) | 1.45 (1.09) | 1.73 (1.05) | 30.47 | 0.00 | 0.21 | H < S, N |
| I will feel free again | 1.17 (1.44) | 0.16 (1.73) | 1.43 (1.16) | 1.52 (1.19) | 22.24 | 0.00 | 0.16 | H < S, N |
| I will feel protected | 1.37 (1.37) | 0.21 (1.68) | 1.62 (0.89) | 1.81 (1.07) | 36.36 | 0.00 | 0.24 | H < S, N |
| I will feel less alone | −0.14 (1.74) | −0.91 (1.81) | −0.19 (1.65) | 0.28 (1.62) | 9.84 | 0.00 | 0.08 | H < S, N |
| I will be less worried about COVID | 0.86 (1.55) | 0.05 (1.80) | 1.01 (1.41) | 1.18 (1.34) | 11.59 | 0.00 | 0.09 | H < S, N |
| I will feel less guilty about breaking COVID regulations | −0.07 (1.88) | −0.55 (2.05) | −0.03 (1.78) | 0.16 (1.82) | 2.80 | 0.06 | 0.02 | n/a |
| Attitude Con Rational; If I get vaccinated against COVID-19: | ||||||||
| It will not be effective | −1.78 (1.58) | −0.52 (1.96) | −2.04 (1.10) | −2.27 (1.24) | 31.23 | 0.00 | 0.21 | H > S, N |
| It will cost me too much time | −2.40 (0.82) | −1.81 (1.15) | −2.54 (0.58) | −2.62 (0.59) | 23.31 | 0.00 | 0.16 | H > S, N |
| I put myself at risk of getting COVID | −2.03 (1.29) | −1.10 (1.71) | −2.29 (0.77) | −2.35 (1.05) | 23.71 | 0.00 | 0.17 | H > S, N |
| I put myself at risk of getting severe side-effects | −1.02 (1.57) | 0.14 (1.59) | −0.99 (1.44) | −1.64 (1.27) | 30.74 | 0.00 | 0.21 | H > S > N |
| I will predominantly support the pharmaceutical industry with it | −1.36 (1.65) | 0.05 (2.03) | −1.70 (1.19) | −1.88 (1.22) | 36.54 | 0.00 | 0.24 | H > S, N |
| I do not know if that will end the pandemic | −0.42 (1.81) | 0.74 (1.68) | −0.59 (1.67) | −0.92 (1.71) | 19.04 | 0.00 | 0.14 | H > S, N |
| Attitude Con Emotional; If I get vaccinated against COVID-19: | ||||||||
| It will feel unsafe | −1.60 (1.61) | −0.29 (1.96) | −1.65 (1.43) | 2.24 (1.02) | 36.33 | 0.00 | 0.24 | H > S > N |
| It will feel scary | −1.43 (1.72) | −0.03 (2.11) | −1.45 (1.46) | −2.13 (1.11) | 37.18 | 0.00 | 0.24 | H > S > N |
| It will feel like I am gambling with my health | −1.39 (1.71) | 0.29 (1.88) | −1.49 (1.39) | −2.19 (1.05) | 61.77 | 0.00 | 0.34 | H > S > N |
| It will make me feel nervous | −1.27 (1.73) | 0.03 (1.88) | −1.22 (1.51) | −1.98 (1.34) | 33.08 | 0.00 | 0.22 | H > S > N |
| It will be because I feel forced to do it | −1.76 (1.75) | −0.14 (2.20) | −1.94 (1.44) | −2.48 (0.95) | 48.86 | 0.00 | 0.29 | H > S, N |
| Social norms: I should get vaccinated against COVID-19 according to my: | ||||||||
| My partner | 1.27 (1.96) | −0.07 (2.25) | 2.05 (1.30) | 1.45 (1.82) | 18.60 | 0.00 | 0.16 | H < S, N |
| My friends | 1.04 (1.73) | 0.37 (1.84) | 1.45 (1.29) | 1.12 (1.82) | 6.24 | 0.00 | 0.05 | H < S, N |
| My parents | 1.09 (1.77) | 0.10 (1.96) | 1.60 (1.41) | 1.28 (1.68) | 11.62 | 0.00 | 0.10 | H < S, N |
| My family | 1.13 (1.76) | 0.28 (1.95) | 1.54 (1.30) | 1.32 (1.76) | 9.06 | 0.00 | 0.08 | H < S, N |
| My colleagues | 0.93 (1.61) | 0.49 (1.78) | 1.51 (1.15) | 0.82 (1.67) | 5.70 | 0.00 | 0.06 | H, N < S |
| My doctor | 0.84 (1.78) | 0.29 (1.63) | 1.09 (1.53) | 0.99 (1.94) | 2.81 | 0.06 | 0.03 | n/a |
| My religious leader | −0.90 (1.59) | −1.00 (1.44) | −1.04 (1.62) | −0.72 (1.72) | 0.37 | 0.69 | 0.01 | n/a |
| Self-efficacy: I would find it hard to get vaccinated against COVID-19: | ||||||||
| If it hurts | 1.96 (1.36) | 1.74 (1.66) | 1.80 (1.38) | 2.18 (1.14) | 2.72 | 0.07 | 0.02 | n/a |
| If it makes me sick | 0.44 (1.82) | −0.48 (1.97) | 0.36 (1.72) | 0.96 (1.60) | 13.54 | 0.00 | 0.10 | H < S, N |
| If I have to get two injections | 1.65 (1.56) | 1.05 (2.00) | 1.65 (1.38) | 1.96 (1.31) | 6.88 | 0.00 | 0.06 | H < N |
| If I think it is scary | 1.48 (1.72) | 1.07 (2.02) | 1.32 (1.63) | 1.80 (1.55) | 3.97 | 0.02 | 0.03 | H < N |
| If I would have to go to the vaccination location alone | 2.19 (1.06) | 1.88 (1.37) | 2.17 (0.95) | 2.36 (0.90) | 4.13 | 0.02 | 0.03 | H < N |
| If I do not know which side effects it has | −0.08 (1.90) | −1.52 (1.50) | −0.22 (1.61) | 0.73 (1.80) | 34.77 | 0.00 | 0.23 | H < S < N |
| If I do not know for sure if it will give me full protection | 0.40 (1.86) | −0.91 (1.73) | 0.61 (1.69) | 0.96 (1.69) | 23.85 | 0.00 | 0.17 | H < S, N |
| If I do not know for how long it will protect me | 0.23 (1.85) | −1.24 (1.48) | 0.43 (1.63) | 0.85 (1.74) | 31.52 | 0.00 | 0.21 | H < S, N |
| If I hear all kinds of contradicting information about the vaccine | 0.07 (1.88) | −1.31 (1.52) | 0.12 (1.65) | 0.74 (1.80) | 28.25 | 0.00 | 0.19 | H < S < N |
| If I read or hear all kinds of fake news about the vaccine | 0.68 (1.93) | −0.52 (1.78) | 0.91 (1.78) | 1.15 (1.85) | 16.99 | 0.00 | 0.13 | H < S, N |
| If people in my environment say I should not get vaccinated | 1.42 (1.55) | 0.93 (1.62) | 1.54 (1.46) | 1.60 (1.52) | 3.98 | 0.02 | 0.03 | H < N |
| If people in my environment say that vaccinations are pointless | 1.50 (1.51) | 0.81 (1.62) | 1.62 (1.38) | 1.79 (1.42) | 8.93 | 0.00 | 0.07 | H < S, N |
| Intention: Are you willing to get vaccinated against COVID-19: | ||||||||
| In general? | 0.82 (0.47) | 0.28 (0.72) | 0.99 (0.12) | 1.00 (0.00) | 88.08 | 0.00 | 0.43 | H < S, N |
| Within a year? | 0.83 (0.45) | 0.33 (0.71) | 0.99 (0.12) | 1.00 (0.00) | 77.93 | 0.00 | 0.40 | H < S, N |
| When you receive an invitation? | 0.82 (0.48) | 0.26 (0.72) | 0.99 (0.12) | 1.00 (0.00) | 93.79 | 0.00 | 0.44 | H < S, N |
| With the AstraZeneca-vaccine? | 0.37 (0.72) | −0.50 (0.50) | 0.07 (0.46) | 1.00 (0.00) | 385.78 | 0.00 | 0.77 | H < S < N |
| With the Pfizer-vaccine? | 0.82 (0.45) | 0.28 (0.67) | 0.99 (0.12) | 1.00 (0.00) | 101.34 | 0.00 | 0.46 | H < S, N |
| With the Moderna-vaccine? | 0.73 (0.53) | −0.03 (0.56) | 0.91 (0.28) | 1.00 (0.00) | 224.96 | 0.00 | 0.66 | H < S, N |
| With the Johnson & Johnson-vaccine? | 0.53 (0.63) | −0.31 (0.47) | 0.46 (0.50) | 1.00 (0.00) | 265.35 | 0.00 | 0.69 | H < S < N |
3.6. Regression
| B | SE B | β | Adj. R2 | p | |
|---|---|---|---|---|---|
| Model 1: | 0.059 | ||||
| -Working | −0.198 | 0.072 | −0.178 | 0.006 | |
| -Religion other | −0.301 | 0.127 | −0.153 | 0.019 | |
| -Education | 0.060 | 0.027 | 0.143 | 0.028 | |
| Model 2: | 0.332 | ||||
| -Knowledge | 0.215 | 0.023 | 0.546 | 0.000 | |
| Model 3: | 0.577 | ||||
| -Knowledge | 0.060 | 0.023 | 0.153 | 0.009 | |
| -Attitude Con Emotional | −0.114 | 0.024 | −0.338 | 0.000 | |
| -Attitude Con Rational | −0.111 | 0.036 | −0.243 | 0.003 | |
| -Attitude Pro Emotional | 0.053 | 0.024 | 0.129 | 0.027 | |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ledford, H.; Cyranoski, D.; Van Noorden, R. The UK Has Approved a COVID Vaccine—Here’s What Scientists Now Want to Know. Nature 2020, 588, 205–206. [Google Scholar] [CrossRef] [PubMed]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine Hesitancy: The next Challenge in the Fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef] [PubMed]
- Harrison, E.A.; Wu, J.W. Vaccine Confidence in the Time of COVID-19. Eur. J. Epidemiol. 2020, 35, 325–330. [Google Scholar] [CrossRef] [Green Version]
- Lin, C.; Tu, P.; Beitsch, L.M. Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines 2021, 9, 16. [Google Scholar] [CrossRef] [PubMed]
- Cascini, F.; Pantovic, A.; Al-Ajlouni, Y.; Failla, G.; Ricciardi, W. Attitudes, Acceptance and Hesitancy among the General Population Worldwide to Receive the COVID-19 Vaccines and Their Contributing Factors: A Systematic Review. EClinicalMedicine 2021, 40, 101113. [Google Scholar] [CrossRef] [PubMed]
- Puri, N.; Coomes, E.A.; Haghbayan, H.; Gunaratne, K. Social Media and Vaccine Hesitancy: New Updates for the Era of COVID-19 and Globalized Infectious Diseases. Hum. Vaccines Immunother. 2020, 16, 2586–2593. [Google Scholar] [CrossRef]
- Chitra, U.; Musco, C. Analyzing the Impact of Filter Bubbles on Social Network Polarization|Proceedings of the 13th International Conference on Web Search and Data Mining. In Proceedings of the 13th International Conference on Web Search and Data Mining, Houston, TX, USA, 3–7 February 2020; pp. 115–123. [Google Scholar]
- Carrieri, V.; Madio, L.; Principe, F. Vaccine Hesitancy and (Fake) News: Quasi-experimental Evidence from Italy. Health Econ. 2019, 28, 1377–1382. [Google Scholar] [CrossRef]
- Tong, C.; Gill, H.; Li, J.; Valenzuela, S.; Rojas, H. “Fake News Is Anything They Say!”—Conceptualization and Weaponization of Fake News among the American Public. Mass Commun. Soc. 2020, 23, 755–778. [Google Scholar] [CrossRef]
- Klein, E.; Robison, J. Like, Post, and Distrust? How Social Media Use Affects Trust in Government. Pol. Commun. 2020, 37, 46–64. [Google Scholar] [CrossRef]
- Wang, R.; He, Y.; Xu, J.; Zhang, H. Fake News or Bad News? Toward an Emotion-Driven Cognitive Dissonance Model of Misinformation Diffusion. Asian J. Commun. 2020, 30, 317–342. [Google Scholar] [CrossRef]
- Tandoc, E.C. The Facts of Fake News: A Research Review. Sociol. Compass 2019, 13, e12724. [Google Scholar] [CrossRef]
- Ellis, J.; Mullan, J.; Worsley, A.; Pai, N. The Role of Health Literacy and Social Networks in Arthritis Patients’ Health Information-Seeking Behavior: A Qualitative Study. Int. J. Fam. Med. 2012, 2012, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Nania, T.; Dellafiore, F.; Graffigna, G.; Caruso, R. ‘Vaccine Hesitancy’ among University Students in Italy during the COVID-19 Pandemic. Eur. J. Epidemiol. 2020, 35, 781–783. [Google Scholar] [CrossRef] [PubMed]
- Schwarzinger, M.; Watson, V.; Arwidson, P.; Alla, F.; Luchini, S. COVID-19 Vaccine Hesitancy in a Representative Working-Age Population in France: A Survey Experiment Based on Vaccine Characteristics. Lancet Public Health 2021, 6, e210–e221. [Google Scholar] [CrossRef]
- Cordina, M.; Lauri, M.A.; Lauri, J. Attitudes towards COVID-19 Vaccination, Vaccine Hesitancy and Intention to Take the Vaccine. Pharm. Pract. 2021, 19, 2317. [Google Scholar] [CrossRef]
- Karafillakis, E.; Simas, C.; Jarrett, C.; Verger, P.; Peretti-Watel, P.; Dib, F.; De Angelis, S.; Takacs, J.; Ali, K.A.; Pastore Celentano, L.; et al. HPV Vaccination in a Context of Public Mistrust and Uncertainty: A Systematic Literature Review of Determinants of HPV Vaccine Hesitancy in Europe. Hum. Vaccin. Immunother. 2019, 15, 1615–1627. [Google Scholar] [CrossRef]
- De Vries, H. An Integrated Approach for Understanding Health Behavior; The I-Change Model as an Example. PBSIJ 2017, 2, 555–585. [Google Scholar] [CrossRef] [Green Version]
- Kasten, S.; van Osch, L.; Candel, M.; de Vries, H. The Influence of Pre-Motivational Factors on Behavior via Motivational Factors: A Test of the I-Change Model. BMC Psychol. 2019, 7, 7. [Google Scholar] [CrossRef]
- De Vries, H.; Mesters, I.; van de Steeg, H.; Honing, C. The General Public’s Information Needs and Perceptions Regarding Hereditary Cancer: An Application of the Integrated Change Model. Patient Educ. Couns. 2005, 56, 154–165. [Google Scholar] [CrossRef]
- Moreau, M.; Gagnon, M.-P.; Boudreau, F. Development of a Fully Automated, Web-Based, Tailored Intervention Promoting Regular Physical Activity among Insufficiently Active Adults with Type 2 Diabetes: Integrating the I-Change Model, Self-Determination Theory, and Motivational Interviewing Components. JMIR Res. Protoc. 2015, 4, e25. [Google Scholar] [CrossRef] [Green Version]
- Doornekamp, L.; van Leeuwen, L.; van Gorp, E.; Voeten, H.; Goeijenbier, M. Determinants of Vaccination Uptake in Risk Populations: A Comprehensive Literature Review. Vaccines 2020, 8, 480. [Google Scholar] [CrossRef] [PubMed]
- Romijnders, K.A.G.J.; van Seventer, S.L.; Scheltema, M.; van Osch, L.; de Vries, H.; Mollema, L. A Deliberate Choice? Exploring Factors Related to Informed Decision-Making about Childhood Vaccination among Acceptors, Refusers, and Partial Acceptors. Vaccine 2019, 37, 5637–5644. [Google Scholar] [CrossRef] [PubMed]
- Knops-Dullens, T.; de Vries, N.; de Vries, H. Reasons for Non-Attendance in Cervical Cancer Screening Programmes: An Application of the Integrated Model for Behavioural Change. Eur. J. Cancer Prev. 2007, 16, 436–445. [Google Scholar] [CrossRef]
- Rijksinstituut voor Volksgezondheid en Milieu Vaccinatiebereidheid. Available online: https://www.rivm.nl/gedragsonderzoek/maatregelen-welbevinden/vaccinatiebereidheid (accessed on 24 January 2022).
- Dadaczynski, K.; Okan, O.; Messer, M.; Leung, A.Y.M.; Rosário, R.; Darlington, E.; Rathmann, K. Digital Health Literacy and Web-Based Information-Seeking Behaviors of University Students in Germany During the COVID-19 Pandemic: Cross-Sectional Survey Study. J. Med. Internet Res. 2021, 23, e24097. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.L. COVID-19 Information Seeking on Digital Media and Preventive Behaviors: The Mediation Role of Worry. Cyberpsychol. Behav. Soc. Netw. 2020, 23, 677–682. [Google Scholar] [CrossRef]
- Gunderson, J.; Mitchell, D.; Reid, K.; Jordan, M. COVID-19 Information-Seeking and Prevention Behaviors in Florida, April 2020. Prev. Chronic Dis. 2021, 18, 200575. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.C.S.; Wong, E.L.Y.; Huang, J.; Cheung, A.W.L.; Law, K.; Chong, M.K.C.; Ng, R.W.Y.; Lai, C.K.C.; Boon, S.S.; Lau, J.T.F.; et al. Acceptance of the COVID-19 Vaccine Based on the Health Belief Model: A Population-Based Survey in Hong Kong. Vaccine 2021, 39, 1148–1156. [Google Scholar] [CrossRef]
- Menard, S. Applied Logistic Regression Analysis: Sage University Series on Quantitative Applications in the Social Sciences; SAGE Publications: Thousand Oaks, CA, USA, 1995. [Google Scholar]
- Robertson, E.; Reeve, K.S.; Niedzwiedz, C.L.; Moore, J.; Blake, M.; Green, M.; Katikireddi, S.V.; Benzeval, M.J. Predictors of COVID-19 Vaccine Hesitancy in the UK Household Longitudinal Study. Brain Behav. Immun. 2021, 94, 41–50. [Google Scholar] [CrossRef]
- Allington, D.; McAndrew, S.; Moxham-Hall, V.; Duffy, B. Coronavirus Conspiracy Suspicions, General Vaccine Attitudes, Trust and Coronavirus Information Source as Predictors of Vaccine Hesitancy among UK Residents during the COVID-19 Pandemic. Psychol. Med. 2021, 12, 1–12. [Google Scholar] [CrossRef]
- Batty, G.D.; Deary, I.J.; Fawns-Ritchie, C.; Gale, C.R.; Altschul, D. Pre-Pandemic Cognitive Function and COVID-19 Vaccine Hesitancy: Cohort Study. Brain Behav. Immun. 2021, 96, 100–105. [Google Scholar] [CrossRef]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological Characteristics Associated with COVID-19 Vaccine Hesitancy and Resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef] [PubMed]
- Pelčić, G.; Karačić, S.; Mikirtichan, G.L.; Kubar, O.I.; Leavitt, F.J.; Cheng-tek Tai, M.; Morishita, N.; Vuletić, S.; Tomašević, L. Religious Exception for Vaccination or Religious Excuses for Avoiding Vaccination. Croat. Med. J. 2016, 57, 516–521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geelen, E.; van Vliet, H.; de Hoogh, P.; Horstman, K. Taming the Fear of Voice: Dilemmas in Maintaining a High Vaccination Rate in the Netherlands. Soc. Sci. Med. 2016, 153, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Wong, E.L.-Y.; Ho, K.-F.; Cheung, A.W.-L.; Yau, P.S.-Y.; Dong, D.; Wong, S.Y.-S.; Yeoh, E.-K. Change of Willingness to Accept COVID-19 Vaccine and Reasons of Vaccine Hesitancy of Working People at Different Waves of Local Epidemic in Hong Kong, China: Repeated Cross-Sectional Surveys. Vaccines 2021, 9, 62. [Google Scholar] [CrossRef] [PubMed]
- Troiano, G.; Nardi, A. Vaccine Hesitancy in the Era of COVID-19. Public Health 2021, 194, 245–251. [Google Scholar] [CrossRef]
- Litaker, J.R.; Tamez, N.; Lopez Bray, C.; Durkalski, W.; Taylor, R. Sociodemographic Factors Associated with Vaccine Hesitancy in Central Texas Immediately Prior to COVID-19 Vaccine Availability. Int. J. Environ. Res. Public Health 2021, 19, 368. [Google Scholar] [CrossRef]
- Gehrau, V.; Fujarski, S.; Lorenz, H.; Schieb, C.; Blöbaum, B. The Impact of Health Information Exposure and Source Credibility on COVID-19 Vaccination Intention in Germany. Int. J. Environ. Res. Public Health 2021, 18, 4678. [Google Scholar] [CrossRef]
- Holzmann-Littig, C.; Braunisch, M.; Kranke, P.; Popp, M.; Seeber, C.; Fichtner, F.; Littig, B.; Carbajo-Lozoya, J.; Allwang, C.; Frank, T.; et al. COVID-19 Vaccination Acceptance and Hesitancy among Healthcare Workers in Germany. Vaccines 2021, 9, 777. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Eid, H.; Al-Mahzoum, K.; Al-Haidar, A.; Taim, D.; Yaseen, A.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines 2021, 9, 42. [Google Scholar] [CrossRef]
- Dambadarjaa, D.; Altankhuyag, G.-E.; Chandaga, U.; Khuyag, S.-O.; Batkhorol, B.; Khaidav, N.; Dulamsuren, O.; Gombodorj, N.; Dorjsuren, A.; Singh, P.; et al. Factors Associated with COVID-19 Vaccine Hesitancy in Mongolia: A Web-Based Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 12903. [Google Scholar] [CrossRef]
- Zimand-Sheiner, D.; Kol, O.; Frydman, S.; Levy, S. To Be (Vaccinated) or Not to Be: The Effect of Media Exposure, Institutional Trust, and Incentives on Attitudes toward COVID-19 Vaccination. Int. J. Environ. Res. Public Health 2021, 18, 12894. [Google Scholar] [CrossRef] [PubMed]
- Dib, F.; Mayaud, P.; Chauvin, P.; Launay, O. Online Mis/Disinformation and Vaccine Hesitancy in the Era of COVID-19: Why We Need an EHealth Literacy Revolution. Hum. Vaccines Immunother. 2021, 12, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Jennings, W.; Stoker, G.; Willis, H.; Valgardsson, V.; Gaskell, J.; Devine, D.; McKay, L.; Mills, M.C. Lack of Trust and Social Media Echo Chambers Predict COVID-19 Vaccine Hesitancy. MedRxiv 2021. [Google Scholar] [CrossRef]
- Kim, H.K.; Ahn, J.; Atkinson, L.; Kahlor, L.A. Effects of COVID-19 Misinformation on Information Seeking, Avoidance, and Processing: A Multicountry Comparative Study. Sci. Commun. 2020, 42, 586–615. [Google Scholar] [CrossRef]
- Soroya, S.H.; Farooq, A.; Mahmood, K.; Isoaho, J.; Zara, S. From Information Seeking to Information Avoidance: Understanding the Health Information Behavior during a Global Health Crisis. Inf. Process. Manag. 2021, 58, 102440. [Google Scholar] [CrossRef]
- Garett, R.; Young, S.D. Online Misinformation and Vaccine Hesitancy. Transl. Behav. Med. 2021, 11, 2194–2199. [Google Scholar] [CrossRef]
- Sievert, E.C.D.; Kok, G.K.; De Vries, H. Exploring Factors Related to COVID-19 Fact-Checking: A Cross-Sectional Study among Adults in Europe. 2022; under review. [Google Scholar]
- Fernández-Torres, M.J.; Almansa-Martínez, A.; Chamizo-Sánchez, R. Infodemic and Fake News in Spain during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 1781. [Google Scholar] [CrossRef]
- Gregory, M.E.; MacEwan, S.R.; Gaughan, A.A.; Rush, L.J.; Powell, J.R.; Kurth, J.D.; Kenah, E.; Panchal, A.R.; Scheck McAlearney, A. Closing the Gap on COVID-19 Vaccinations in First Responders and Beyond: Increasing Trust. Int. J. Environ. Res. Public Health 2022, 19, 644. [Google Scholar] [CrossRef]
- Dratva, J.; Wagner, A.; Zysset, A.; Volken, T. To Vaccinate or Not to Vaccinate—This Is the Question among Swiss University Students. Int. J. Environ. Res. Public Health 2021, 18, 9210. [Google Scholar] [CrossRef]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding Vaccine Hesitancy around Vaccines and Vaccination from a Global Perspective: A Systematic Review of Published Literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef]
- Dubé, È.; Farrands, A.; Lemaitre, T.; Boulianne, N.; Sauvageau, C.; Boucher, F.D.; Tapiero, B.; Quach, C.; Ouakki, M.; Gosselin, V.; et al. Overview of Knowledge, Attitudes, Beliefs, Vaccine Hesitancy and Vaccine Acceptance among Mothers of Infants in Quebec, Canada. Hum. Vaccines Immunother. 2019, 15, 113–120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eggers, S.M.; Aarø, L.E.; Bos, A.E.R.; Mathews, C.; de Vries, H. Predicting Condom Use in South Africa: A Test of Two Integrative Models. AIDS Behav. 2014, 18, 135–145. [Google Scholar] [CrossRef] [PubMed]
- Huynh, G.; Nguyen, T.V.; Nguyen, D.D.; Lam, Q.M.; Pham, T.N.; Nguyen, H.T.N. Knowledge About COVID-19, Beliefs and Vaccination Acceptance Against COVID-19 Among High-Risk People in Ho Chi Minh City, Vietnam. Infect. Drug Resist. 2021, 14, 1773–1780. [Google Scholar] [CrossRef] [PubMed]
- Salali, G.D.; Uysal, M.S. COVID-19 Vaccine Hesitancy Is Associated with Beliefs on the Origin of the Novel Coronavirus in the UK and Turkey. Psychol. Med. 2020, 1–3. [Google Scholar] [CrossRef]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Fernandes, N.; Costa, D.; Costa, D.; Keating, J.; Arantes, J. Predicting COVID-19 Vaccination Intention: The Determinants of Vaccine Hesitancy. Vaccines 2021, 9, 1161. [Google Scholar] [CrossRef]
- Dubé, E.; Gagnon, D.; Ouakki, M.; Bettinger, J.A.; Guay, M.; Halperin, S.; Wilson, K.; Graham, J.; Witteman, H.O.; MacDonald, S.; et al. Understanding Vaccine Hesitancy in Canada: Results of a Consultation Study by the Canadian Immunization Research Network. PLoS ONE 2016, 11, e0156118. [Google Scholar] [CrossRef]
- Palm, R.; Bolsen, T.; Kingsland, J.T. The Effect of Frames on COVID-19 Vaccine Resistance. Front. Polit. Sci. 2021, 3, 661257. [Google Scholar] [CrossRef]
- Guidry, J.P.D.; Laestadius, L.I.; Vraga, E.K.; Miller, C.A.; Perrin, P.B.; Burton, C.W.; Ryan, M.; Fuemmeler, B.F.; Carlyle, K.E. Willingness to Get the COVID-19 Vaccine with and without Emergency Use Authorization. Am. J. Infect. Control 2021, 49, 137–142. [Google Scholar] [CrossRef]
- MacDonald, N.E. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Jemielniak, D.; Krempovych, Y. An analysis of AstraZeneca COVID-19 vaccine misinformation and fear mongering on Twitter. Public Health 2021, 200, 4–6. [Google Scholar] [CrossRef] [PubMed]
- Sønderskov, K.M.; Dinesen, P.T.; Østergaard, S.D. Sustained COVID-19 Vaccine Willingness after Safety Concerns over the Oxford-AstraZeneca Vaccine. Dan. Med. J. 2021, 68, A03210292. [Google Scholar] [PubMed]
- Smerilli, G.; Cipolletta, E.; Moscioni, E.; Francioso, F.; Risa, A.M.; Maccarrone, V.; Zompa, D.; Di Matteo, A.; Di Carlo, M.; De Angelis, R.; et al. Correspondence on ‘SARS-CoV-2 Vaccine Hesitancy among Patients with Rheumatic and Musculoskeletal Diseases: A Message for Rheumatologists’. Ann. Rheum. Dis. 2021, 80, e168. [Google Scholar] [CrossRef] [PubMed]
- Tavolacci, M.P.; Dechelotte, P.; Ladner, J. COVID-19 Vaccine Acceptance, Hesitancy, and Resistancy among University Students in France. Vaccines 2021, 9, 654. [Google Scholar] [CrossRef] [PubMed]
- Castellano-Tejedor, C.; Torres-Serrano, M.; Cencerrado, A. Unveiling Associations of COVID-19 Vaccine Acceptance, Hesitancy, and Resistance: A Cross-Sectional Community-Based Adult Survey. Int. J. Environ. Res. Public Health 2021, 18, 12348. [Google Scholar] [CrossRef]
- AlShurman, B.A.; Khan, A.F.; Mac, C.; Majeed, M.; Butt, Z.A. What Demographic, Social, and Contextual Factors Influence the Intention to Use COVID-19 Vaccines: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 9342. [Google Scholar] [CrossRef]
- Albarracin, D.; Jung, H.; Song, W.; Tan, A.; Fishman, J. Rather than Inducing Psychological Reactance, Requiring Vaccination Strengthens Intentions to Vaccinate in US Populations. Sci. Rep. 2021, 11, 20796. [Google Scholar] [CrossRef]
| Total | Vaccine Hesitancy (VH) | Statistics | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 240) | Hesitant (n = 58) | Somewhat Hesitant (n = 69) | Non-Hesitant (n = 113) | χ2/F | df | p | |||||
| Age (mean ± SD) | 44.1 ± 17.2 | 46.3 ± 15.6 | 41.0 ± 15.9 | 44.9 ± 18.6 | 1.78 | 2 | 0.17 | ||||
| Gender | % | n | % | n | % | n | % | n | 6.70 | 4 | 0.15 |
| Male | 25.8 | 62 | 21.0 | 12 | 18.8 | 13 | 59.7 | 37 | |||
| Female | 73.8 | 177 | 26.0 | 46 | 31.6 | 56 | 42.4 | 75 | |||
| Other | 0.4 | 1 | 0.0 | 0 | 0.0 | 0 | 0.9 | 1 | |||
| Education (mean ± SD) | 6.50 ± 1.21 | 5.98 ± 1.42 | 6.80 ± 0.98 | 6.58 ± 1.14 | 8.09 | 2 | 0.00 | ||||
| Religion | % | n | % | n | % | n | % | n | 8.43 | 10 | 0.08 |
| No religion | 53.8 | 129 | 17.8 | 23 | 31.0 | 40 | 51.2 | 66 | |||
| Catholic | 39.6 | 95 | 30.5 | 29 | 24.2 | 23 | 45.3 | 43 | |||
| Other | 6.6 | 16 | 37.5 | 6 | 37.5 | 6 | 25.0 | 4 | |||
| Paid work | % | n | % | n | % | n | % | n | 6.22 | 2 | 0.05 |
| Yes | 72.1 | 173 | 27.2 | 47 | 30.6 | 53 | 42.2 | 73 | |||
| No | 27.9 | 67 | 16.4 | 11 | 23.9 | 16 | 59.7 | 40 | |||
| How Often do You Use the Following News Sources for Information Regarding COVID-19 Vaccination? (Never-Very Often) | Mean (SD) | F | p | Post-Hoc | |||
|---|---|---|---|---|---|---|---|
| Total (n = 240) | Hesitant (n = 58) | Somewhat Hesitant (n = 69) | Non-Hesitant (n = 113) | ||||
| 3.18 (1.23) | 2.91 (1.22) | 3.19 (1.33) | 3.31 (1.17) | 2.00 | 0.14 | n/a |
| 2.02 (1.69) | 1.50 (1.47) | 2.13 (1.74) | 2.21 (1.72) | 3.71 | 0.03 | H < N |
| 2.56 (1.43) | 2.41 (1.46) | 2.49 (1.48) | 2.68 (1.37) | 0.79 | 0.46 | n/a |
| 0.88 (1.25) | 1.02 (1.34) | 0.97 (1.31) | 0.76 (1.15) | 1.05 | 0.35 | n/a |
| 2.51 (1.42) | 2.28 (1.50) | 2.39 (1.49) | 2.71 (1.32) | 2.15 | 0.12 | n/a |
| 3.05 (1.48) | 2.66 (1.61) | 3.10 (1.53) | 3.21 (1.35) | 2.84 | 0.06 | n/a |
| 1.16 (1.26) | 1.19 (1.34) | 1.03 (1.20) | 1.22 (1.27) | 0.52 | 0.60 | n/a |
| 1.50 (1.42) | 1.78 (1.46) | 1.39 (1.47) | 1.42 (1.37) | 1.49 | 0.23 | n/a |
| 1.45 (1.51) | 1.88 (1.58) | 1.28 (1.56) | 1.35 (1.42) | 3.12 | 0.05 | n/a |
| 0.86 (1.27) | 1.02 (1.31) | 0.86 (1.34) | 0.78 (1.20) | 0.68 | 0.51 | n/a |
| 3.03 (1.12) | 2.98 (1.21) | 3.07 (1.01) | 3.02 (1.16) | 0.10 | 0.90 | n/a |
| 1.45 (1.39) | 1.55 (1.35) | 1.58 (1.59) | 1.31 (1.28) | 1.03 | 0.36 | n/a |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Vries, H.; Verputten, W.; Preissner, C.; Kok, G. COVID-19 Vaccine Hesitancy: The Role of Information Sources and Beliefs in Dutch Adults. Int. J. Environ. Res. Public Health 2022, 19, 3205. https://doi.org/10.3390/ijerph19063205
de Vries H, Verputten W, Preissner C, Kok G. COVID-19 Vaccine Hesitancy: The Role of Information Sources and Beliefs in Dutch Adults. International Journal of Environmental Research and Public Health. 2022; 19(6):3205. https://doi.org/10.3390/ijerph19063205
Chicago/Turabian Stylede Vries, Hein, Wouter Verputten, Christian Preissner, and Gerjo Kok. 2022. "COVID-19 Vaccine Hesitancy: The Role of Information Sources and Beliefs in Dutch Adults" International Journal of Environmental Research and Public Health 19, no. 6: 3205. https://doi.org/10.3390/ijerph19063205
APA Stylede Vries, H., Verputten, W., Preissner, C., & Kok, G. (2022). COVID-19 Vaccine Hesitancy: The Role of Information Sources and Beliefs in Dutch Adults. International Journal of Environmental Research and Public Health, 19(6), 3205. https://doi.org/10.3390/ijerph19063205






