Analysis of Stigma in Relation to Behaviour and Attitudes towards Mental Health as Influenced by Social Desirability in Nursing Students
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design, Population and Setting
2.2. Instruments
2.2.1. Mental Illness: Clinicians’ Attitudes Scale (MICA)
2.2.2. The Spanish Scale for Measuring Attitudes to the Mentally Ill among Future Health Workers—Escala de Medición de Actitudes Hacia los Enfermos Mentales en Futuros Técnicos de Salud (Spanish Acronym EMAEMFTS)
2.2.3. Reported and Intended Behaviour Scale (RIBS)
2.2.4. Social Desirability Scale (SDS)
2.3. Ethical Considerations
2.4. Procedure
2.5. Statistical Analysis
3. Results
3.1. Participants Characteristics
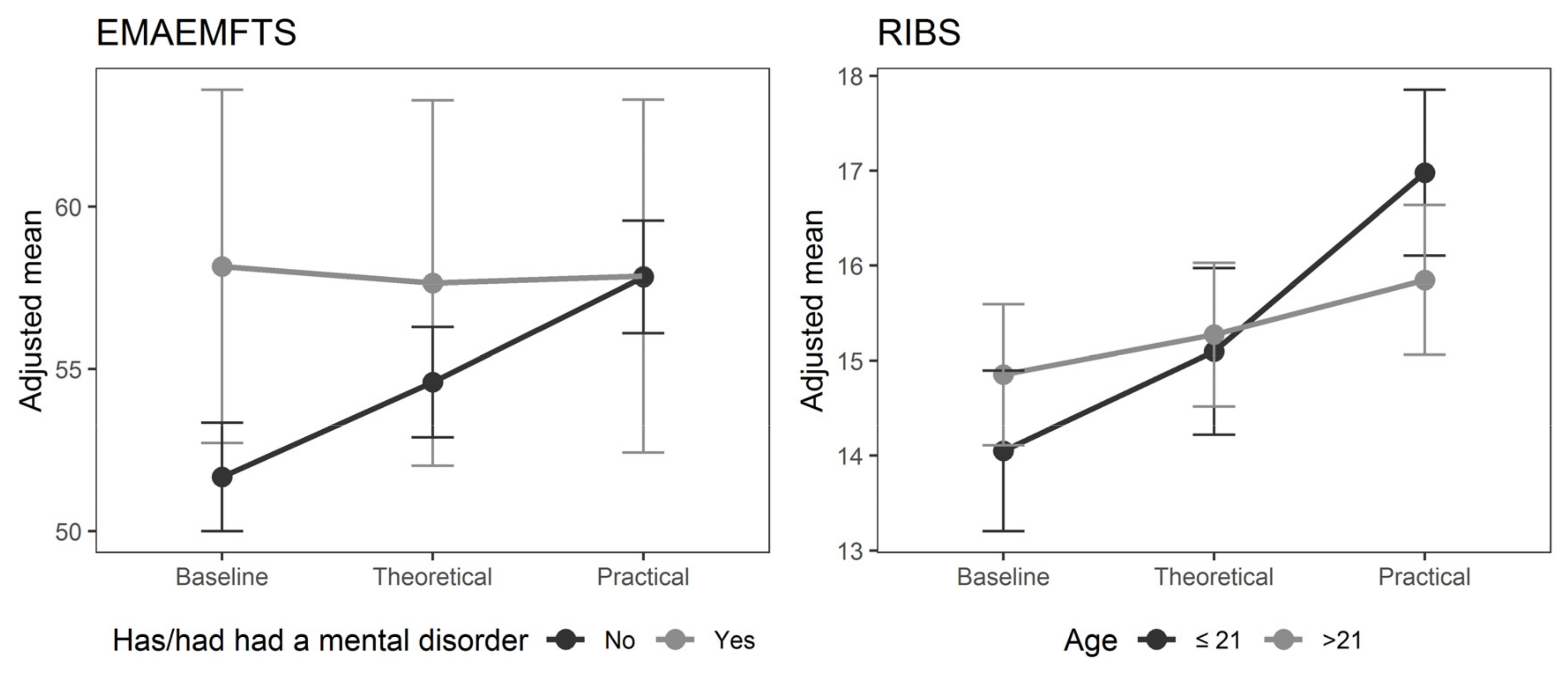
3.2. Evolution of Scores in Attitudes Based on Participants Characteristics and Mental Health Training
3.3. Associations between Participants Characteristics
4. Discussion
Limitations of the Study
5. Conclusions
Relevance to Clinical Practice
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rossler, W. The stigma of mental disorders. A millennia-long history of social exclusion and prejudices. Sci. Soc. 2016, 17, 1250–1253. [Google Scholar] [CrossRef]
- Stier, A.; Hinshaw, S.P. Explicit and implicit stigma against individuals with mental illness. Aust. Psychol. 2007, 42, 106–117. [Google Scholar] [CrossRef]
- Goffman, E. Stigma: Notes on the Management of Spoiled Identity; Prentice-Hall: New York, NY, USA, 1963; pp. 1–168. [Google Scholar]
- Thornicroft, G.; Mehta, N.; Clement, S.; Evans-lacko, S.; Doherty, M.; Rose, D.; Koschorke, M.; Shidhaye, R.; Reilly, C.O. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet 2016, 387, 1123–1132. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Mental Health Action Plan 2013–2020; WHO: Geneva, Switzerland, 2013; Volume 86, pp. 1–50. [Google Scholar]
- Thornicroft, G.; Rose, D.; Mehta, N. Discrimination against people with mental illness: What can psychiatrists do? Adv. Psychiatr. Treat. 2010, 16, 53–59. [Google Scholar] [CrossRef]
- Tapia, F.M.; Castro, W.L.; Poblete, C.M.; Soza, C.M. Estigma hacia los trastornos mentales: Características e intervenciones. Salud Ment. 2015, 38, 53–58. [Google Scholar] [CrossRef]
- Stuart, G.W. Principles and Practice of Psychiatric Nursing, 10th ed.; Elservier: Amsterdam, The Netherlands, 2013; pp. 1–832. ISBN 9780323091145. [Google Scholar]
- Bertram, G.; Stickley, T. Mental health nurses, promoters of inclusion or perpetuators of exclusion? J. Psychiatr. Ment. Health Nurs. 2005, 12, 387–395. [Google Scholar] [CrossRef]
- Jack-Ide, I.O.; Uys, L.R.; Middleton, L.E. Mental health care policy environment in Rivers State: Experiences of mental health nurses providing mental health care services in neuro-psychiatric hospital, Port Harcourt, Nigeria. Int. J. Ment. Health Syst. 2013, 7, 8. [Google Scholar] [CrossRef]
- Ross, C.A.; Goldner, E.M. Stigma, negative attitudes and discrimination towards mental illness within the nursing profession: A review of the literature. J. Psychiatr. Ment. Health Nurs. 2009, 16, 558–567. [Google Scholar] [CrossRef]
- Fokuo, J.K.; Goldrick, V.; Rossetti, J.; Wahlstrom, C.; Kocurek, C.; Larson, J.; Corrigan, P. Decreasing the Stigma of Mental Illness Through a Student-Nurse Mentoring Program: A Qualitative Study. Community Ment. Health J. 2016, 53, 1–9. [Google Scholar] [CrossRef]
- Zartaloudi, A.; Madianos, M. Stigma related to help-seeking from a mental health professional. Health Sci. J. 2010, 4, 77–83. [Google Scholar]
- Heyman, I.; Webster, B.J.; Tee, S. Curriculum development through understanding the student nurse experience of suicide intervention education—A phenomenographic study. Nurse Educ. Pract. 2015, 15, 498–506. [Google Scholar] [CrossRef]
- Happell, B.; Byrne, L.; Platania-Phung, C.; Harris, S.; Bradshaw, J.; Davies, J. Lived-experience participation in nurse education: Reducing stigma and enhancing popularity. Int. J. Ment. Health Nurs. 2014, 23, 427–434. [Google Scholar] [CrossRef]
- Bates, L.; Stickley, T. Confronting Goffman: How can mental health nurses effectively challenge stigma? A critical review of the literature. J. Psychiatr. Ment. Health Nurs. 2013, 20, 569–575. [Google Scholar] [CrossRef]
- Linden, M.; Kavanagh, R. Attitudes of qualified vs. student mental health nurses towards an individual diagnosed with schizophrenia. J. Adv. Nurs. 2012, 68, 1359–1368. [Google Scholar] [CrossRef]
- Rodríguez-Almagro, J.; Hernández-Martínez, A.; Rodríguez-Almagro, D.; Quiros-García, J.M.; Solano-Ruiz, M.d.C.; Gómez-Salgado, J. Level of stigma among Spanish nursing students toward mental illness and associated factors: A mixed-methods study. Int. J. Environ. Res. Public Health 2019, 16, 4870. [Google Scholar] [CrossRef]
- Happell, B. Influencing undergraduate nursing students’ attitudes toward mental health nursing: Acknowledging the role of theory. Issues Ment. Health Nurs. 2009, 30, 39–46. [Google Scholar] [CrossRef]
- Happell, B.; Platania-Phung, C. Mental health placements in a general health setting: No substitute for the real thing! J. Clin. Nurs. 2012, 61, 2026–2033. [Google Scholar] [CrossRef]
- Henderson, S.; Happell, B.; Martin, T. Impact of theory and clinical placement on undergraduate students mental health nursing knowledge, skills, and attitudes. Int. J. Ment. Health Nurs. 2007, 16, 116–125. [Google Scholar] [CrossRef]
- Ewalds-Kvist, B.; Högberg, T.; Lützén, K. Student nurses and the general population in Sweden: Trends in attitudes towards mental illness. Nord. J. Psychiatry. 2012, 9488, 164–170. [Google Scholar] [CrossRef]
- Giralt Palou, R.; Prat Vigué, G.; Tort-Nasarre, G. Attitudes and stigma toward mental health in nursing students: A systematic review. Perspect. Psychiatr. Care 2019, 55, 243–255. [Google Scholar] [CrossRef]
- Morrison, R. Nursing Students’ Attitudes toward People with Mental Illness: Do They Change after Instruction and Clinical Exposure? University of South Florida: Tampa, FL, USA, 2011. [Google Scholar]
- Romem, P.; Anson, O.; Kanat-Maymon, Y.; Moisa, R. Reshaping Students ’ Attitudes Toward Individuals with Mental Illness Through a Clinical Nursing Clerkship. J. Nurs. Educ. 2008, 47, 396–403. [Google Scholar] [CrossRef]
- Tee, S.; Sinem, Y.; Özçetin, Ü. Promoting positive perceptions and person centred care toward people with mental health problems using co-design with nursing students. Nurse Educ. Today J. 2016, 44, 116–120. [Google Scholar] [CrossRef]
- Happell, B.; Platania-Phung, C.; Scholz, B.; Bocking, J.; Horgan, A.; Manning, F.; Doody, R.; Hals, E.; Granerud, A.; Lahti, M.; et al. Changing attitudes: The impact of Expert by Experience involvement in Mental Health Nursing Education: An international survey study. Int. J. Ment. Health Nurs. 2018, 28, 480–491. [Google Scholar] [CrossRef]
- Crowne, D.; Marlowe, D. A new scale of social desirability independent of psychopathology. J. Consult. Psychol. 1960, 24, 349–354. [Google Scholar] [CrossRef]
- Nederhof, A.J. Methods of coping with social desirability bias: A review. Eur. J. Soc. Psychol. 1985, 15, 263–280. [Google Scholar] [CrossRef]
- Tourangeau, R.; Yan, T. Sensitive Questions in Surveys. Psychol. Bull. 2007, 133, 859–883. [Google Scholar] [CrossRef]
- Perinelli, E.; Gremigni, P. Use of social desirability scales in clinical psychology: A systematic review. J. Clin. Psychol. 2016, 72, 534–551. [Google Scholar] [CrossRef] [PubMed]
- Henderson, C.; Evans-Lacko, S.; Flach, C.; Thornicroft, G. Responses to mental health stigma questions: The importance of social desirability and data collection method. Can. J. Psychiatry. 2012, 57, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Gabbidon, J.; Clement, S.; van Nieuwenhuizen, A.; Kassam, A.; Brohan, E.; Norman, I.; Thornicroft, G. Mental Illness: Clinicians’ Attitudes (MICA) scale-psychometric properties of a version for healthcare students and professionals. Psychiatry Res. 2013, 206, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Hernandez Arroyo, L.; Mesa Rodas, N.; Rentero Martín, D.; Puerta Rodriguez, S.; Nieves Carnicer, M. Stigma Related to Mental Illness in Medical Students From Madrid. Eur. Psychiatry 2015, 30, 1877. [Google Scholar] [CrossRef]
- Fernandez-Rios, L.; Torres-Collazo, M.; Carballal-Balsa, M. Una Escala de medición de actitudes hacia los enfermos mentales en futuros técnicos de salud (*) A Scale for measuring attitudes to the mentally ill among future health workers. Rev. Asoc. Española Neuropsiquiatría 1988, 8, 637–651. [Google Scholar]
- Evans-Lacko, S.; Rose, D.; Little, K.; Flach, C.; Rhydderch, D.; Henderson, C.; Thornicroft, G. Development and psychometric properties of the Reported and Intended Behaviour Scale (RIBS): A stigma-related behaviour measure. Epidemiol. Psychiatr. Sci. 2011, 20, 263–271. [Google Scholar] [CrossRef]
- Rubio-Valera, M.; Fernández, A.; Evans-Lacko, S.; Luciano, J.V.; Thornicroft, G.; Aznar-Lou, I.; Serrano-Blanco, A. Impact of the mass media OBERTAMENT campaign on the levels of stigma among the population of Catalonia, Spain. Eur. Psychiatry 2016, 31, 44–51. [Google Scholar] [CrossRef]
- Ferrando, P.J.; Chico, E. Adaptación y análisis psicométrico de la escala de deseabilidad social de Marlowe y Crowne. Psicothema 2000, 12, 383–389. [Google Scholar]
- Clement, S.; Van Nieuwenhuizen, A.; Kassam, A.; Flach, C.; Lazarus, A.; De Castro, M.; McCrone, P.; Norman, I.; Thornicroft, G. Filmed v. live social contact interventions to reduce stigma: Randomised controlled trial. Br. J. Psychiatry 2012, 201, 57–64. [Google Scholar] [CrossRef]
- Simon, N.; Verdoux, H. Impact of education program and clinical posting in psychiatry on medical students’ stigmatizing attitudes towards psychiatry and psychiatric disorders. Encephale 2018, 44, 329–336. [Google Scholar] [CrossRef]
- Eksteen, H.C.; Becker, P.J.; Lippi, G. Stigmatization towards the mentally ill: Perceptions of psychiatrists, pre-clinical and post-clinical rotation medical students. Int. J. Soc. Psychiatry 2017, 63, 782–791. [Google Scholar] [CrossRef]
- Li, J.; Li, J.; Huang, Y.; Thornicroft, G. Mental health training program for community mental health staff in Guangzhou, China: Effects on knowledge of mental illness and stigma. Int. J. Ment. Health Syst. 2014, 8, 49. [Google Scholar] [CrossRef]
- Ben Natan, M.; Drori, T.; Hochman, O. Associative Stigma Related to Psychiatric Nursing Within the Nursing Profession. Arch. Psychiatr. Nurs. 2015, 29, 388–392. [Google Scholar] [CrossRef]
- Çingöl, N.; Karakaş, M.; Zengin, S.; Çelebi, E. The effect of psychiatric nursing students’ internships on their beliefs about and attitudes toward mental health problems; a single-group experimental study. Nurse Educ. Today 2019, 19, 104243. [Google Scholar] [CrossRef]
- Granados-Gámez, G.; López Rodríguez, M.d.M.; Corral Granados, A.; Márquez-Hernández, V.V. Attitudes and Beliefs of Nursing Students Toward Mental Disorder: The Significance of Direct Experience With Patients. Perspect. Psychiatr. Care 2017, 53, 135–143. [Google Scholar] [CrossRef]
- Barry, S.; Ward, L. Undergraduate Nursing Students’ Understandings of Mental Health: A Review of the Literature. Issues Ment. Health Nurs. 2017, 38, 160–175. [Google Scholar] [CrossRef]
- Sayols-Villanueva, M.; Ballester-Ferrando, D.; Gelabert-Vilella, S.; Fuentes-Pumarola, C.; Rascón-Hernán, C. El estigma de los trastornos mentales en los estudiantes de enfermería. Rev. Enfermería Salud Ment. 2015, 2, 7–15. [Google Scholar] [CrossRef][Green Version]
- Happell, B.; Gaskin, C.J. The attitudes of undergraduate nursing students towards mental health nursing: A systematic review. J. Clin. Nurs. 2013, 22, 148–158. [Google Scholar] [CrossRef]
- Lim, H.J.; Moxham, L.; Patterson, C.; Perlman, D.; Lopez, V.; Goh, Y.S. Students’ mental health clinical placements, clinical confidence and stigma surrounding mental illness: A correlational study. Nurse Educ. Today 2020, 84, 104219. [Google Scholar] [CrossRef]
- Foster, K.; Withers, E.; Blanco, T.; Lupson, C.; Steele, M.; Giandinoto, J.; Furness, T. Undergraduate nursing students’ stigma and recovery attitudes during mental health clinical placement: A pre/post-test survey study. Int. J. Ment. Health Nurs. 2019, 28, 1068–1080. [Google Scholar] [CrossRef] [PubMed]
- Aznar-Lou, I.; Serrano-Blanco, A.; Fernández, A.; Luciano, J.V.; Rubio-Valera, M. Attitudes and intended behaviour to mental disorders and associated factors in catalan population, Spain: Cross-sectional population-based survey. BMC Public Health 2016, 16, 127. [Google Scholar] [CrossRef] [PubMed]
- Dalky, H.F.; Abu-Hassan, H.H.; Dalky, A.F.; Al-Delaimy, W. Assessment of Mental Health Stigma Components of Mental Health Knowledge, Attitudes and Behaviors Among Jordanian Healthcare Providers. Community Ment. Health J. 2020, 56, 524–531. [Google Scholar] [CrossRef]
- Li, J.; Li, J.; Thornicroft, G.; Huang, Y. Levels of stigma among community mental health staff in Guangzhou, China. BMC Psychiatry 2014, 14, 231. [Google Scholar] [CrossRef]
- Moreno Herrero, A.M.; Sánchez Sánchez, F.; Lópz de Lemus Sarmiento, M. Diferencias de la población general en relación a los conocimientos, actitudes y conductas hacia el estigma en salud mental. Psychol. Soc. Educ. 2014, 6, 17–26. [Google Scholar]
- Rasinski, K.A.; Baldwin, A.K.; Willis, G.B.; Jobe, J.B. Risk and loss perceptions associated with survey reporting of sensitive behaviors. In Proceedings of the Annual Meeting of the American Statistical Association, Toronto, ON, Canada, 13–18 August 1994; pp. 497–502. [Google Scholar]
- Petkari, E.; Masedo Gutiérrez, A.I.; Xavier, M.; Moreno Küstner, B. The influence of clerkship on students’ stigma towards mental illness: A meta-analysis. Med. Educ. 2018, 52, 694–704. [Google Scholar] [CrossRef]
- Happell, B.; Horgan, A.; Manning, F.; Doody, R. Experts by experiences in mental health nursing education:what have we learned from the commune project? J. Ment. Health Psychiatr. Nurs. 2020, 27, 675–677. [Google Scholar] [CrossRef]
| Characteristic | n = 162 |
|---|---|
| Age | 23.0 (SD 5.9) |
| Gender | |
| Female | 122 (75.3) |
| Male | 40 (24.7) |
| Contact with people who have or had a mental disorder | |
| No | 55 (34.0) |
| Yes | 107 (66.0) |
| Has or had had a mental disorder | |
| No | 148 (91.4) |
| Yes | 14 (8.6) |
| Previous professional experience | |
| No | 144 (88.9) |
| Yes | 18 (11.1) |
| Previous training experience | |
| No | 145 (89.5) |
| Yes | 17 (10.5) |
| L0 | L1 | L2 | p | p | |||
|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | General | L0 vs. L1 | L0 vs. L2 | L1 vs. L2 | |
| MICA | 40.6 (7.7) | 39.9 (9.2) | 37.7 (8.1) | 0.001 | 0.633 | 0.003 | 0.010 |
| EMAEMFTS | 52.3 (10.4) | 55.0 (10.4) | 58.0 (10.1) | <0.0001 | 0.002 | <0.0001 | 0.0002 |
| RIBS | 14.7 (3.6) | 15.4 (3.7) | 16.5 (3.3) | <0.0001 | 0.071 | <0.0001 | 0.0002 |
| α | |||
|---|---|---|---|
| L0 | L1 | L2 | |
| MICA | 0.617 | 0.71 | 0.644 |
| EMAEMFTS | 0.859 | 0.876 | 0.873 |
| RIBS | 0.700 | 0.762 | 0.759 |
| SDS | 0.773 | 0.799 | 0.808 |
| Unajusted | Adjusted by SDS | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| L0 | L1 | L2 | p | p | |||||||||
| Mean | SD | Mean | SD | Mean | SD | Time | Categ | Time x | Time | Categ | Time x | ||
| MICA | Categ | Categ | |||||||||||
| Gender | Male | 42.2 | 8 | 43.5 | 10.7 | 42.4 | 7.9 | ||||||
| Female | 41 | 8.1 | 39.1 | 9.1 | 37.3 | 7.5 | 0.000 | 0.110 | 0.255 | 0.000 | 0.050 | 0.239 | |
| Age | ≤21 | 39.5 | 7.1 | 38.9 | 8.4 | 36.4 | 8 | ||||||
| >21 | 41.4 | 8.1 | 40.1 | 9.8 | 38.8 | 8 | 0.000 | 0.077 | 0.889 | 0.000 | 0.054 | 0.878 | |
| Contact with people who have or | No | 40.4 | 7.9 | 40 | 10.9 | 37.7 | 8.3 | ||||||
| had a mental disorder | Yes | 40.6 | 7.6 | 39.8 | 8.4 | 37.7 | 7.9 | 0.000 | 0.983 | 0.916 | 0.000 | 0.619 | 0.911 |
| Has or had had a mental disorder | No | 40.5 | 7.5 | 40.3 | 9.3 | 38 | 8.2 | ||||||
| Yes | 40.7 | 9.6 | 35.2 | 8.1 | 35.3 | 5.5 | 0.000 | 0.259 | 0.198 | 0.000 | 0.144 | 0.282 | |
| Previous professional experience | No | 40.7 | 7.3 | 40 | 9 | 37.8 | 8 | ||||||
| Yes | 39 | 10.2 | 38.5 | 11 | 36.7 | 8.6 | 0.000 | 0.419 | 0.829 | 0.000 | 0.469 | 0.828 | |
| Previous training experience | No | 40.7 | 7.6 | 39.8 | 9.2 | 37.5 | 8 | ||||||
| Yes | 39.1 | 8.2 | 40.1 | 10.1 | 39.6 | 8.2 | 0.000 | 0.984 | 0.252 | 0.000 | 0.936 | 0.260 | |
| EMAEMFTS | |||||||||||||
| Gender | Male | 50.7 | 9.9 | 51.2 | 10.8 | 52.8 | 11 | ||||||
| Female | 53.4 | 11.4 | 56.3 | 10.7 | 58.5 | 10.1 | <0.0001 | 0.124 | 0.169 | <0.0001 | 0.071 | 0.156 | |
| Age | ≤21 | 52 | 9.7 | 55.5 | 9.9 | 59.4 | 9.3 | ||||||
| >21 | 52.3 | 11 | 54.5 | 10.9 | 56.8 | 10.6 | <0.0001 | 0.659 | 0.172 | <0.0001 | 0.590 | 0.166 | |
| Contact with people who have or | No | 50.5 | 10 | 54 | 11 | 57.7 | 11 | ||||||
| had a mental disorder | Yes | 53.2 | 10.5 | 55.5 | 10.3 | 58.1 | 9.7 | <0.0001 | 0.275 | 0.309 | <0.0001 | 0.140 | 0.353 |
| Has or had had a mental disorder | No | 51.8 | 9.8 | 54.6 | 10.3 | 58 | 10.1 | ||||||
| Yes | 57.5 | 15 | 59.6 | 12 | 57.2 | 10.3 | <0.0001 | 0.299 | 0.033 | <0.0001 | 0.201 | 0.033 | |
| Previous professional experience | No | 51.9 | 10.4 | 55.0 | 10.5 | 57.8 | 10.3 | ||||||
| Yes | 55.7 | 10.5 | 55 | 10 | 59.2 | 8.5 | <0.0001 | 0.366 | 0.360 | <0.0001 | 0.398 | 0.316 | |
| Previous training experience | No | 52.2 | 10.6 | 55.2 | 10.6 | 58.2 | 10.4 | ||||||
| Yes | 53.3 | 8.6 | 52.8 | 9 | 56 | 6.7 | <0.0001 | 0.805 | 0.403 | <0.0001 | 0.767 | 0.405 | |
| RIBS | |||||||||||||
| Gender | Male | 14.9 | 3.9 | 14.2 | 4.6 | 5.2 | 4.2 | ||||||
| Female | 15.1 | 3.4 | 16.1 | 3.2 | 16.3 | 3.4 | <0.0001 | 0.211 | 0.077 | <0.0001 | 0.122 | 0.064 | |
| Age | ≤21 | 14.2 | 3.8 | 15.3 | 3.6 | 17.1 | 2.8 | ||||||
| >21 | 15.1 | 3.5 | 15.4 | 3.8 | 16 | 3.6 | <0.0001 | 0.980 | 0.004 | <0.0001 | 0.937 | 0.004 | |
| Contact with people who have or | No | 14 | 3.5 | 14.7 | 4 | 16.2 | 3.6 | ||||||
| had a mental disorder | Yes | 15.1 | 3.7 | 15.7 | 3.6 | 16.7 | 3.2 | <0.0001 | 0.086 | 0.620 | <0.0001 | 0.028 | 0.671 |
| Has or had had a mental disorder | No | 14.5 | 3.6 | 15.2 | 3.7 | 16.5 | 3.3 | ||||||
| Yes | 17 | 3.2 | 17.2 | 2.6 | 17 | 3.9 | <0.0001 | 0.078 | 0.117 | <0.0001 | 0.039 | 0.104 | |
| Previous professional experience | No | 14.6 | 3.5 | 15.5 | 3.6 | 16.6 | 3.2 | ||||||
| Yes | 15.5 | 4.5 | 14.4 | 4.2 | 15.8 | 4.5 | <0.0001 | 0.797 | 0.089 | <0.0001 | 0.729 | 0.073 | |
| Previous training experience | No | 14.7 | 3.5 | 15.6 | 3.5 | 16.6 | 3.2 | ||||||
| Yes | 14.35 | 5.1 | 13.7 | 5 | 15.4 | 4.3 | <0.0001 | 0.159 | 0.356 | <0.0001 | 0.140 | 0.351 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giralt Palou, R.; Prat Vigué, G.; Romeu-Labayen, M.; Tort-Nasarre, G. Analysis of Stigma in Relation to Behaviour and Attitudes towards Mental Health as Influenced by Social Desirability in Nursing Students. Int. J. Environ. Res. Public Health 2022, 19, 3213. https://doi.org/10.3390/ijerph19063213
Giralt Palou R, Prat Vigué G, Romeu-Labayen M, Tort-Nasarre G. Analysis of Stigma in Relation to Behaviour and Attitudes towards Mental Health as Influenced by Social Desirability in Nursing Students. International Journal of Environmental Research and Public Health. 2022; 19(6):3213. https://doi.org/10.3390/ijerph19063213
Chicago/Turabian StyleGiralt Palou, Rosa, Gemma Prat Vigué, Maria Romeu-Labayen, and Glòria Tort-Nasarre. 2022. "Analysis of Stigma in Relation to Behaviour and Attitudes towards Mental Health as Influenced by Social Desirability in Nursing Students" International Journal of Environmental Research and Public Health 19, no. 6: 3213. https://doi.org/10.3390/ijerph19063213
APA StyleGiralt Palou, R., Prat Vigué, G., Romeu-Labayen, M., & Tort-Nasarre, G. (2022). Analysis of Stigma in Relation to Behaviour and Attitudes towards Mental Health as Influenced by Social Desirability in Nursing Students. International Journal of Environmental Research and Public Health, 19(6), 3213. https://doi.org/10.3390/ijerph19063213






