Evolution of Select Epidemiological Modeling and the Rise of Population Sentiment Analysis: A Literature Review and COVID-19 Sentiment Illustration
Abstract
:1. Introduction
Brief Background
2. Materials and Methods
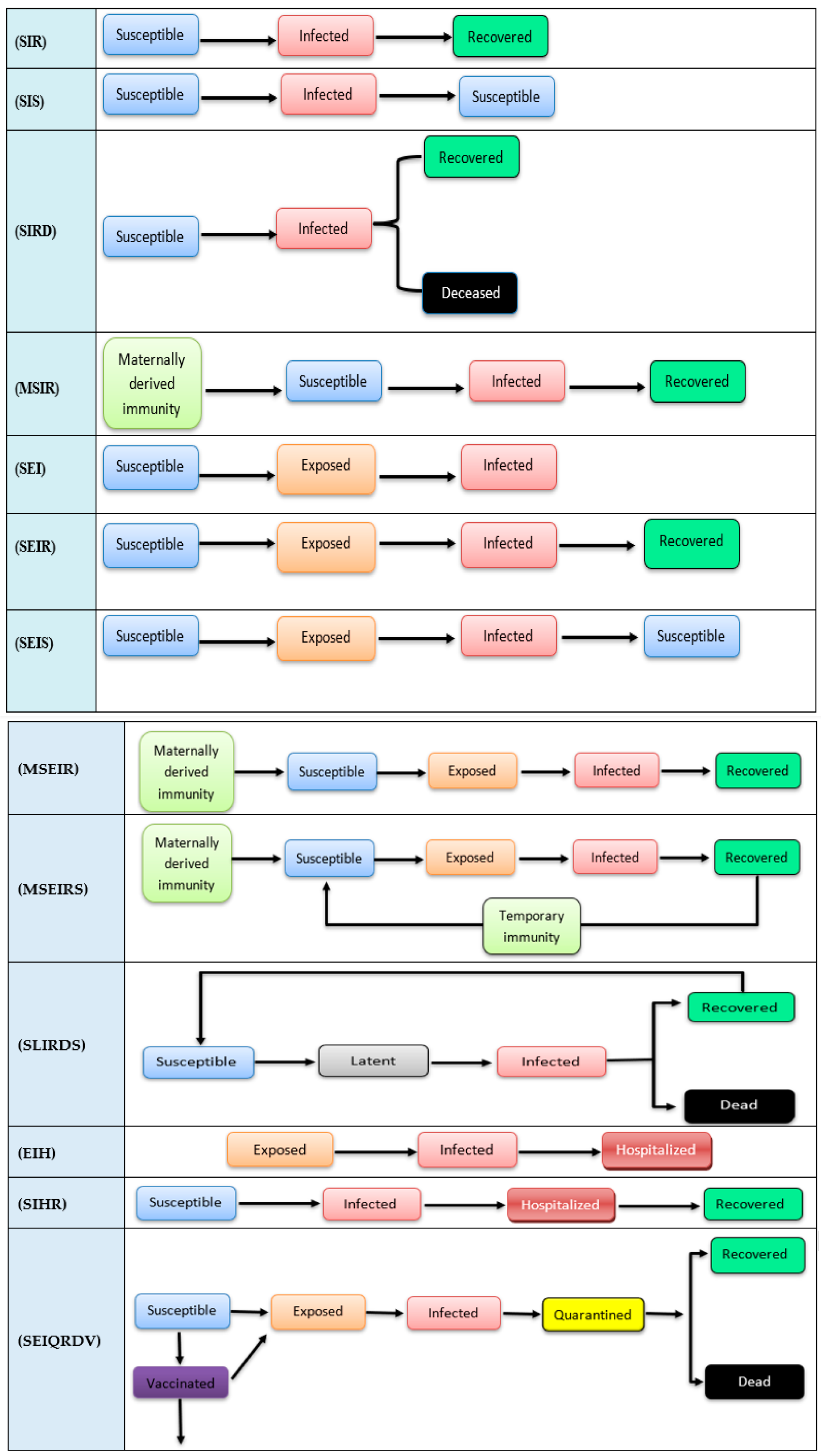
2.1. Epidemiological State Model Foundations
2.2. Epidemiological Statistical Forecast Models
2.3. Theoretical Intervention Approaches and Models
2.4. Agent-Based and Multiagent Systems Modeling
2.5. Artificial Intelligence and Hybrid Models
3. Social Media and Epidemiological Modeling
3.1. Epidemiology State Models and Social Media
3.2. Statistical Prediction Models and Social Media
3.3. Theoretical Interventions Models and Social Media
3.4. Agent-Based and Social Media and Social Networks
3.4.1. Frias-Martinez (FM) Model
3.4.2. University of Texas at Austin’s (UT COVID-19-Social Distancing) Model
3.5. Hybrid Models and Social Media
Twitter and Vaccination Prediction Model
4. Illustration of Twitter Sentiment Data
5. Discussion and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviation
| SIR | Susceptible, Infected, Recovered |
| SIS | Susceptible, Infected, Susceptible |
| SIRD | Susceptible, Infected, Recovered, Deceased |
| MSIR | Maternally derived immunity, Susceptible, Infected, Recovered |
| SEI | Susceptible, Exposed, Infected |
| SEIR | Susceptible, Exposed, Infected, Recovered |
| SEIS | Susceptible, Exposed, Infected, Susceptible |
| MSEIR | Maternally derived immunity, Susceptible, Exposed, Infected, Recovered |
| MSEIRS | Maternally derived immunity, Susceptible, Exposed, Infected, Recovered, Susceptible |
| SLIRDS | Susceptible-Latent-Infected-Recovered-Dead-Susceptible |
| EIH | Exposed, Infected, Hospitalized |
| SIHR | Susceptible, Infected, Hospitalized, Recovered |
Appendix A
| References | How Was SM or SN Used? | Platform/ Application? | Calibrated with SM or SN? | Goal/Predict no of? | Type | Model |
| [96] | ----- | ----- | No | Susceptible cases Infected cases Recovered cases | Epidemiological State models | Susceptible, Infected, Recovered (SIR) |
| [97] | ----- | ----- | No | Susceptible cases infected cases | Epidemiological State models | Susceptible, Infected, Susceptible (SIS) |
| [98] | ----- | ----- | No | Susceptible cases infected cases Recovered cases Deaths cases | Epidemiological State models | Susceptible, Infected, Recovered, Deceased (SIRD) |
| [99] | ----- | ----- | No | Susceptible cases infected cases Recovered cases | Epidemiological State models | Maternally derived immunity, Susceptible, Infected, Recovered (MSIR) |
| [82] | Use media to modify public behavior | Media awareness programs | Yes/SM | Exposed cases Infected cases Recovered cases | Epidemiological State models | Susceptible, Exposed, Infected (SEI) |
| [100] | ----- | ----- | No | Susceptible cases Exposed cases infected cases Recovered cases | Epidemiological State models | Susceptible, Exposed, Infected, Recovered (SEIR) |
| [101] | ----- | ----- | No | Susceptible cases Exposed cases infected cases | Epidemiological State models | Susceptible, Exposed, Infected, Susceptible (SEIS) |
| [102] | ----- | ----- | No | Susceptible cases Exposed cases infected cases Recovered cases | Epidemiological State models | Maternally derived immunity, Susceptible, Exposed, Infected, Recovered (MSEIR) |
| [103] | ----- | ----- | No | Susceptible cases Exposed cases infected cases Recovered cases | Epidemiological State models | Maternally derived immunity, Susceptible, Exposed, Infected, Recovered, Susceptible (MSEIRS) |
| [104] | ----- | ----- | No | Susceptible cases Latent cases Infected cases Recovered cases Deaths cases | Epidemiological State models | Susceptible-Latent-Infected-Recovered-Dead-Susceptible (SLIRDS) |
| [105] | Use media to modify public behavior | Media awareness programs | Yes/SM | Exposed cases Infected cases Hospitalized cases | Epidemiological State models | Exposed, Infected, Hospitalized (EIH) |
| [78] | Use media to modify public behavior | Media awareness programs | Yes/SM | Susceptible cases Infected cases Hospitalized cases Recovered cases | Epidemiological State models | Susceptible, Infected, Hospitalized, Recovered (SIHR) |
| [106] | ----- | ----- | No | Infected cases Hospitalized cases Deaths cases | Epidemiological Statistical Forecast Models | Differential Equations Leads to Predictions of Hospitalizations and Infections (DELPHI); |
| [83] | Data source | Google and Twitter | Yes/SM | Infected cases | Epidemiological Statistical Forecast Models | Auto regressive integrated moving average (ARIMA) |
| [61] | ----- | ----- | No | Infected cases Death cases Predict time of pandemic peak | Epidemiological Statistical Forecast Models | Los Alamos National Laboratory COVID-19 forecasting using Fast Evaluation and Estimation (LANL COFFEF) |
| [107] | ----- | ----- | No | “Forecast how likely a patient’s disease is to worsen while being treated in a hospital and at what point in their care that might happen” | Epidemiological Statistical Forecast Models | John Hopkins model COVID-19 prediction (JHU COVID-19 prediction) |
| [20] | ----- | ----- | No | Susceptible cases Exposed cases Infected cases Quarantined cases Recovered cases Vaccinated cases | Epidemiological Statistical Forecast Models | Susceptible, Exposed, Infected, Quarantined, Recovered, Dead, Vaccinated forecasting (SEIQRDV.F). |
| [26] | Data source | Yes/SM | Promote population to follow healthy behavior Predict changes in health behaviors of individuals | Theoretical Interventions model | Health Belief Model (HBM) | |
| [27] | ----- | ----- | No | Predict the human behavior | Theoretical Interventions model | The Theory of Planned Behavior (TPB) |
| [28] | ----- | ----- | No | Explains how individuals are motivated to act to protect themselves | Theoretical Interventions model | Protection Motivation Theory (PMT) |
| [51] | ----- | ----- | No | Modeling disease dynamics and fear as two interacting contagion processes | Agent-based model | The Coupled Contagion Dynamics of Fear and Disease (CCDFD) model |
| [52] | ----- | ----- | No | Testing effects of different levels of social distancing policies on the diseases spread | Agent-based model | The Social Distancing (SD) model |
| [53] | ----- | ----- | No | Project epidemic trends Explore intervention scenarios Estimate resource needs. | Agent-based model | COVID-19 Agent-based Simulator (COVASIM) model |
| [54] | ----- | ----- | No | Simulate the epidemiological and economic impacts of social distancing policies | Agent-based model | COVID-19 agent-based simulation (COVID-ABS) model |
| [55] | ----- | ----- | No | “Effectiveness of a nationwide vaccine campaign in response to different vaccine efficacies, the willingness of the population to be vaccinated, and the daily vaccine capacity under two different federal plans”. Studying the interactions between nonpharmaceutical interventions and vaccines | Agent-based model | COVID-19 Agent-based Simulator (COVASIM) and Vaccination model |
| [50] | ----- | ----- | No | Susceptible cases Infected cases Recovered cases Quarantine impact Transport restrictions impact Effectiveness of the interventions on the disease spread | Multiagent system model | DMAS-SIR model |
| [57] | Data source | Mobile phones-Calls | Yes/SN | Trace users’ phones and their mobility through network to study effects of government’ interventions on virus spread | Agent-based model | Frias-Martinez model (FM) |
| [56] | Data source | Mobile phones-GPS traces | Yes/SN | Trace users’ phones and their mobility through GPS to study effects of government’ interventions on virus spread | Agent-based model | University of Texas at Austin’s (UT COVID-19-Social distancing) model |
| [59] | ----- | ----- | No | Infected cases Deaths cases | Artificial Intelligence and Hybrid models | Y Youyang Gu COVID-19 (YYG) model |
| [61] | ----- | ----- | No | Processing population’ images to detect who wear mask or who not | Artificial Intelligence and Hybrid models | Deep transfer learning (DTL) model |
| [62,63] | Data source | Mobile phones-GPS | Yes/SN | Effectiveness of the interventions on the disease spread No of required beds and at hospitals and care units Trace users’ phones and their mobility through GPS | Artificial Intelligence and Hybrid models | University of Virginia Biocomplexity Center PatchSim COVID-19 (UVA COVID-19) |
| [66] | Data source | Mobile phones-GPS | Yes/SN | Effectiveness of the interventions on the disease spread Trace users’ phones and their mobility through GPS | Artificial Intelligence and Hybrid models | Institute for Health Metrics and Evaluation COVID-19 (IHME COVID-19) |
| [67] | ----- | ----- | No | Infected cases Deaths cases No of required beds and at hospitals and care units | Artificial Intelligence and Hybrid models | Massachusetts Institute of Technology COVID-19 (MIT University COVID-19) model |
| [87] | Data source | Twitter/Users’ tweets | Yes/SM | Study and analyze Twitter users’ opinions, beliefs, and emotions about vaccination | Artificial Intelligence and Hybrid models | Twitter vaccination analysis (TWVA) model |
References
- Squazzoni, F.; Polhill, J.G.; Edmonds, B.; Ahrweiler, P.; Antosz, P.; Scholz, G.; Chappin, É.; Borit, M.; Verhagen, H.; Giardini, F.; et al. Computational models that matter during a global pandemic outbreak: A call to action. J. Artif. Soc. Soc. Simul. 2020, 23, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Correia, S.; Luck, S.; Verner, E. Fight the Pandemic, Save the Economy: Lessons from the 1918 Flu. Available online: https://libertystreeteconomics.newyorkfed.org/2020/03/fight-the-pandemic-save-the-economy-lessons-from-the-1918-flu/ (accessed on 9 December 2021).
- Holcombe, M. As Coronavirus Cases Rise, Fauci Says Public Health Measures Are the Way to Slow Spread. Available online: https://www.winknews.com/2020/10/19/as-coronavirus-cases-rise-fauci-says-public-health-measures-are-the-way-to-slow-spread/ (accessed on 9 December 2021).
- Wang, X.; Pasco, R.; Du, Z.; Petty, M.; Fox, S.; Galvani, A.; Pignone, M.; Johnston, S.C.; Meyers, L.A. Impact of Social Distancing Measures on Coronavirus Disease Healthcare Demand, Central Texas, USA. Emerg. Infect. Dis. 2020, 26, 2361–2369. [Google Scholar] [CrossRef] [PubMed]
- Cascini, F.; Hoxhaj, I.; Zaçe, D.; Ferranti, M.; Di Pietro, M.L.; Boccia, S.; Ricciardi, W. How health systems approached respiratory viral pandemics over time: A systematic review. BMJ Glob. Health 2020, 5, e003677. [Google Scholar] [CrossRef] [PubMed]
- Monmouth University Polling Institute. One in Five Still Shun Vaccine; Monmouth University Polling Institute: West Long Branch, NJ, USA, 2021; Available online: https://www.monmouth.edu/polling-institute/reports/monmouthpoll_us_041421/ (accessed on 10 December 2021).
- Kukulka, A. COVID-19 Vaccine Hesitancy among Conservatives Is Highest, But Highlighting Vaccine Benefits Could Combat That, Public Health Experts Say. Chicago Tribune, 1 May 2021. Available online: https://www.chicagotribune.com/suburbs/post-tribune/ct-ptb-vaccine-rollout-feat-st-0502-20210430-qk6cxdjc2vbm3gel6gxq5g55se-story.html(accessed on 10 December 2021).
- Neel, J. Vaccination Rates Rose In August As COVID Cases Surged Due To The Delta Variant. NPR [Online]. 1 September 2021. Available online: https://www.npr.org/2021/08/31/1032994955/vaccination-rates-rose-in-august-as-covid-cases-surge-due-to-the-delta-variant (accessed on 10 December 2021).
- Rogers, K.; Gay, S. Biden Mandates Vaccines for Workers, Saying, ‘Our Patience Is Wearing Thin’. The New York Times, 9 September 2021. Available online: https://www.nytimes.com/2021/09/09/us/politics/biden-mandates-vaccines.html(accessed on 10 December 2021).
- Wadman, M. Having SARS-CoV-2 Once Confers Much Greater Immunity Than a Vaccine—But Vaccination Remains Vital. Available online: https://www.science.org/content/article/having-sars-cov-2-once-confers-much-greater-immunity-vaccine-vaccination-remains-vital (accessed on 10 December 2021).
- Erman, M.; Maddipatla, M. Heart Inflammation in Young Men Higher Than Expected after Pfizer, Moderna Vaccines-U.S. CDC. Reuters Media, 10 June 2021. Available online: https://www.reuters.com/world/us/cdc-heart-inflammation-cases-ages-16-24-higher-than-expected-after-mrna-covid-19-2021-06-10/(accessed on 10 December 2021).
- Byington, C.L.; Maldonado, Y.A.; Barnett, E.D.; Davies, H.D.; Lynfield, R.; Munoz, F.M.; Nolt, D.; Nyquist, A.C.; Rathore, M.H. Countering Vaccine Hesitancy. Pediatrics 2016, 138, e20162146. [Google Scholar] [CrossRef] [Green Version]
- National Governors Association. Protests, Policing, and COVID-19; National Governors Association: Washington, DC, USA, 2020; Available online: https://www.nga.org/center/publications/protests-policing-covid-19/ (accessed on 10 December 2021).
- Magness, P.W. Case for Mask Mandate Rests on Bad Data. The Wall Street Journal, 11 November 2020. Available online: https://www.wsj.com/articles/case-for-mask-mandate-rests-on-bad-data-11605113310(accessed on 10 December 2021).
- Brown, G.; Ozanne, M. Statistical Models for Infectious Diseases: A Useful Tool for Practical Decision-Making. Am. J. Trop. Med. Hyg. 2019, 101, 1–2. [Google Scholar] [CrossRef] [Green Version]
- Kermack, W.O.; McKendrick, A.G. Contributions to the mathematical theory of epidemics--III. Further studies of the problem of endemicity. 1933. Bull. Math. Biol. 1991, 53, 89–118. [Google Scholar] [CrossRef]
- Hethcote, H.W. Three Basic Epidemiological Models. In Applied Mathematical Ecology; Levin, S.A., Hallam, T.G., Gross, L.J., Eds.; Springer: Berlin/Heidelberg, Germany, 1989; pp. 119–144. ISBN 978-3-642-61317-3. [Google Scholar]
- Brauer, F.; van den Driessche, P.; Wu, J. (Eds.) Mathematical Epidemiology; Springer: Berlin/Heidelberg, Germany, 2008; ISBN 9783540789109. [Google Scholar]
- Johns Hopkins Coronavirus Resource Center. Understanding Vaccination Progress by Country. Available online: https://coronavirus.jhu.edu/vaccines/international (accessed on 10 December 2021).
- Ghostine, R.; Gharamti, M.; Hassrouny, S.; Hoteit, I. An Extended SEIR Model with Vaccination for Forecasting the COVID-19 Pandemic in Saudi Arabia Using an Ensemble Kalman Filter. Mathematics 2021, 9, 636. [Google Scholar] [CrossRef]
- Anderson, R.M.; Heesterbeek, H.; Klinkenberg, D.; Hollingsworth, T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet 2020, 395, 931–934. [Google Scholar] [CrossRef]
- Forrester, J.W. Industrial Dynamics: A Major Breakthrough for Decision Makers. Harv. Bus. Rev. 1958, 36, 37–66. [Google Scholar] [CrossRef]
- DeJoy, D.M. Theoretical models of health behavior and workplace self-protective behavior. J. Saf. Res. 1996, 27, 61–72. [Google Scholar] [CrossRef]
- Simpson, V. Models and theories to support health behavior intervention and program planning. Health Hum. Sci. 2015, 2, 45–47. [Google Scholar]
- Samui, P.; Mondal, J.; Khajanchi, S. A mathematical model for COVID-19 transmission dynamics with a case study of India. Chaos Solitons Fractals 2020, 140, 110173. [Google Scholar] [CrossRef] [PubMed]
- Champion, V.L.; Skinner, C.S. The health belief model. In Health Behavior and Health Education: Theory, Research, and Practice, 4th ed.; Glanz, K., Rimer, B.K., Viswanath, K., Eds.; Jossey-Bass: San Francisco, CA, USA, 2008; pp. 45–65. ISBN 9780787996147. [Google Scholar]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Okuhara, T.; Okada, H.; Kiuchi, T. Predictors of Staying at Home during the COVID-19 Pandemic and Social Lockdown based on Protection Motivation Theory: A Cross-Sectional Study in Japan. Healthcare 2020, 8, 475. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Liang, J.; Yang, J.; Ma, X.; Li, X.; Wu, J.; Yang, G.; Ren, G.; Feng, Y. Analysis of the environmental behavior of farmers for non-point source pollution control and management: An integration of the theory of planned behavior and the protection motivation theory. J. Environ. Manag. 2019, 237, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Nottmeyer, L.N.; Sera, F. Influence of temperature, and of relative and absolute humidity on COVID-19 incidence in England—A multi-city time-series study. Environ. Res. 2021, 196, 110977. [Google Scholar] [CrossRef] [PubMed]
- Thomas, C.; Nagchoudhury, S. India’s Peak Holiday Season Set to Send COVID-19 Cases Surging. Reuters Media, 15 October 2020. Available online: https://www.reuters.com/article/health-coronavirus-india-festivals-holid-idINKBN2700M9(accessed on 10 December 2021).
- Maxouris, C.; Hanna, J.; Vercammen, P.; Andone, D. Coronavirus Cases and Deaths Surge to New Highs in the United States. CP24, 10 January 2021. Available online: https://www.cp24.com/world/after-holidays-u-s-covid-19-cases-and-deaths-climb-to-all-time-highs-1.5260840?cache=yes%3FclipId%3D89578%3FclipId%3D89830(accessed on 10 December 2021).
- Bae, S.Y.; Chang, P.-J. The effect of coronavirus disease-19 (COVID-19) risk perception on behavioural intention towards ‘untact’ tourism in South Korea during the first wave of the pandemic (March 2020). Curr. Issues Tour. 2021, 24, 1017–1035. [Google Scholar] [CrossRef]
- Yastica, T.V.; Salma, S.A.; Caesaron, D.; Safrudin, Y.N.; Pramadya, A.R. Application of Theory Planned Behavior (TPB) and Health Belief Model (HBM) in COVID-19 Prevention: A Literature Review. In Proceedings of the 2020 6th International Conference on Interactive Digital Media (ICIDM), Bandung, Indonesia, 14–15 December 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 1–4, ISBN 978-1-7281-4928-8. [Google Scholar]
- Lipman, S.A.; Burt, S.A. Self-reported prevalence of pests in Dutch households and the use of the health belief model to explore householders’ intentions to engage in pest control. PLoS ONE 2017, 12, e0190399. [Google Scholar] [CrossRef] [Green Version]
- Ling, M.; Kothe, E.J.; Mullan, B.A. Predicting intention to receive a seasonal influenza vaccination using Protection Motivation Theory. Soc. Sci. Med. 2019, 233, 87–92. [Google Scholar] [CrossRef] [Green Version]
- Floyd, D.L.; Prentice-Dunn, S.; Rogers, R.W. A Meta-Analysis of Research on Protection Motivation Theory. J. Appl. Soc. Psychol. 2000, 30, 407–429. [Google Scholar] [CrossRef]
- Minnesota Department of Health. Minnesota Heart Disease and Stroke Prevention Plan 2011–2020; Minnesota Department of Health: Saint Paul, MN, USA, 2011; Available online: www.health.state.mn.us/diseases/cardiovascular/documents/cvhplan2011.pdf (accessed on 10 December 2021).
- Agents in Artificial Intelligence. Available online: https://www.geeksforgeeks.org/agents-artificial-intelligence/ (accessed on 9 December 2021).
- Bonabeau, E. Agent-based modeling: Methods and techniques for simulating human systems. Proc. Natl. Acad. Sci. USA 2002, 99 (Suppl. S3), 7280–7287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crooks, A. Agent-Based Modelling and Geographical Information Systems: A Practical Primer; SAGE Publications: Thousand Oaks, CA, USA, 2018; ISBN 9781473958654. [Google Scholar]
- Siebers, P.-O.; Aickelin, U. Introduction to Multi-Agent Simulation. In Encyclopedia of Decision Making and Decision Support Technologies; Adam, F., Humphreys, P., Eds.; IGI Global: Hershey, PA, USA, 2008; pp. 554–564. ISBN 9781599048437. [Google Scholar]
- Zohdi, T.I. An agent-based computational framework for simulation of global pandemic and social response on planet X. Comput. Mech. 2020, 66, 1195–1209. [Google Scholar] [CrossRef] [PubMed]
- Hunter, E.; Mac Namee, B.; Kelleher, J. An open-data-driven agent-based model to simulate infectious disease outbreaks. PLoS ONE 2018, 13, e0208775. [Google Scholar] [CrossRef] [PubMed]
- Hunter, E.; Mac Namee, B.; Kelleher, J.D. A Taxonomy for Agent-Based Models in Human Infectious Disease Epidemiology. J. Artif. Soc. Soc. Simul. 2017, 20, 2. [Google Scholar] [CrossRef] [Green Version]
- Parsons, S.; Wooldridge, M. Game Theory and Decision Theory in Multi-Agent Systems. Auton. Agents Multi-Agent Syst. 2002, 5, 243–254. [Google Scholar] [CrossRef]
- Alkhateeb, F.; Maghayreh, E.A.; Aljawarneh, S. A Multi Agent-Based System for Securing University Campus: Design and Architecture. In Proceedings of the 2010 International Conference on Intelligent Systems, Modelling and Simulation, Liverpool, UK, 27–29 January 2010; IEEE: Piscataway, NJ, USA, 2010; pp. 75–79, ISBN 2166-0670. [Google Scholar]
- Niazi, M.; Hussain, A. Agent-based computing from multi-agent systems to agent-based models: A visual survey. Scientometrics 2011, 89, 479–499. [Google Scholar] [CrossRef] [Green Version]
- Seddari, N.; Redjimi, M. Multi-agent modeling of a complex system. In Proceedings of the 2013 3rd International Conference on Information Technology and e-Services (ICITeS), Sousse, Tunisia, 24–26 March 2013; IEEE: Piscataway, NJ, USA, 2013; pp. 1–6. [Google Scholar]
- Vyklyuk, Y.; Manylich, M.; Škoda, M.; Radovanović, M.M.; Petrović, M.D. Modeling and analysis of different scenarios for the spread of COVID-19 by using the modified multi-agent systems—Evidence from the selected countries. Results Phys. 2021, 20, 103662. [Google Scholar] [CrossRef]
- Epstein, J.M.; Parker, J.; Cummings, D.; Hammond, R.A. Coupled Contagion Dynamics of Fear and Disease: Mathematical and Computational Explorations. PLoS ONE 2008, 3, e3955. [Google Scholar] [CrossRef] [Green Version]
- Daghriri, T.; Ozmen, O. Quantifying the Effects of Social Distancing on the Spread of COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 5566. [Google Scholar] [CrossRef]
- Kerr, C.C.; Stuart, R.M.; Mistry, D.; Abeysuriya, R.G.; Hart, G.; Rosenfeld, K.; Selvaraj, P.; Núñez, R.C.; Hagedorn, B.; George, L.; et al. Covasim: An agent-based model of COVID-19 dynamics and interventions. medRxiv 2020, arXiv:2020.05.10.20097469. [Google Scholar] [CrossRef]
- Silva, P.C.L.; Batista, P.V.C.; Lima, H.S.; Alves, M.A.; Guimarães, F.G.; Silva, R.C.P. COVID-ABS: An agent-based model of COVID-19 epidemic to simulate health and economic effects of social distancing interventions. Chaos Solitons Fractals 2020, 139, 110088. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Giabbanelli, P. Returning to a Normal Life via COVID-19 Vaccines in the United States: A Large-scale Agent-Based Simulation Study. JMIR Med. Inform. 2021, 9, e27419. [Google Scholar] [CrossRef] [PubMed]
- Woody, S.; Tec, M.; Dahan, M.; Gaither, K.; Lachmann, M.; Fox, S.J.; Meyers, L.A.; Scott, J. Projections for first-wave COVID-19 deaths across the US using social-distancing measures derived from mobile phones. medRxiv 2020, arXiv:2020.04.16.20068163. [Google Scholar] [CrossRef]
- Frias-Martinez, E.; Williamson, G.; Frias-Martinez, V. An Agent-Based Model of Epidemic Spread Using Human Mobility and Social Network Information. In Proceedings of the 2011 IEEE Third International Conference on Privacy, Security, Risk and Trust and 2011 IEEE Third International Conference on Social Computing, Boston, MA, USA, 9–11 October 2011; IEEE: Piscataway, NJ, USA, 2011; pp. 57–64. [Google Scholar]
- Coronavirus Disease (COVID-19) Cases in the U.S.: Updated on 16 July 2020; National Center for Immunization and Respiratory Diseases (U.S.), Division of Viral Diseases: Atlanta, GA, USA, 2020.
- Giattino, C. How Epidemiological Models of COVID-19 Help Us Estimate the True Number of Infections. Available online: https://ourworldindata.org/covid-models (accessed on 9 December 2021).
- Gu, Y. Six Months Later. Available online: https://youyanggu.com/blog/six-months-later (accessed on 9 December 2021).
- Loey, M.; Manogaran, G.; Taha, M.H.N.; Khalifa, N.E.M. A hybrid deep transfer learning model with machine learning methods for face mask detection in the era of the COVID-19 pandemic. Measurement 2021, 167, 108288. [Google Scholar] [CrossRef] [PubMed]
- Virginia Department of Health. UVA COVID-19 Model. Available online: https://www.vdh.virginia.gov/coronavirus/see-the-numbers/covid-19-data-insights/uva-covid-19-model/ (accessed on 10 December 2021).
- Price, C.C.; Propp, A.M. A Framework for Assessing Models of the COVID-19 Pandemic to Inform Policymaking in Virginia; RAND Corporation: Santa Monica, CA, USA, 2020; Available online: https://www.rand.org/pubs/research_reports/RRA323-1.html (accessed on 9 December 2021).
- Virginia Department of Health Home page. Available online: https://www.vdh.virginia.gov/ (accessed on 10 December 2021).
- Jewell, N.P.; Lewnard, J.A.; Jewell, B.L. Caution Warranted: Using the Institute for Health Metrics and Evaluation Model for Predicting the Course of the COVID-19 Pandemic. Ann. Intern. Med. 2020, 173, 226–227. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Institute for Health Metrics and Evaluation. COVID-19 Resources. Available online: https://www.healthdata.org/covid (accessed on 9 December 2021).
- Gallagher, M.B. Model Quantifies the Impact of Quarantine Measures on COVID-19’s Spread. Massachusetts Institute of Technology. Available online: https://news.mit.edu/2020/new-model-quantifies-impact-quarantine-measures-covid-19-spread-0416 (accessed on 10 December 2021).
- Dandekar, R.; Barbastathis, G. Neural Network aided quarantine control model estimation of global Covid-19 spread. arXiv 2020, arXiv:2004.02752. [Google Scholar]
- El-Sayed, A.M.; Scarborough, P.; Seemann, L.; Galea, S. Social network analysis and agent-based modeling in social epidemiology. Epidemiol. Perspect. Innov. 2012, 9, 1. [Google Scholar] [CrossRef] [Green Version]
- Pachetti, M.; Marini, B.; Giudici, F.; Benedetti, F.; Angeletti, S.; Ciccozzi, M.; Masciovecchio, C.; Ippodrino, R.; Zella, D. Impact of lockdown on Covid-19 case fatality rate and viral mutations spread in 7 countries in Europe and North America. J. Transl Med. 2020, 18, 338. [Google Scholar] [CrossRef]
- Collinson, S.; Heffernan, J.M. Modelling the effects of media during an influenza epidemic. BMC Public Health 2014, 14, 376. [Google Scholar] [CrossRef] [Green Version]
- Freberg, K.; Palenchar, M.J.; Veil, S.R. Managing and sharing H1N1 crisis information using social media bookmarking services. Public Relat. Rev. 2013, 39, 178–184. [Google Scholar] [CrossRef]
- Guidry, J.P.; Jin, Y.; Orr, C.A.; Messner, M.; Meganck, S. Ebola on Instagram and Twitter: How health organizations address the health crisis in their social media engagement. Public Relat. Rev. 2017, 43, 477–486. [Google Scholar] [CrossRef]
- Will, M.; Groeneveld, J.; Frank, K.; Müller, B. Combining social network analysis and agent-based modelling to explore dynamics of human interaction: A review. Socio-Environ. Syst. Model. 2020, 2, 16325. [Google Scholar] [CrossRef] [Green Version]
- Slovic, P. The Perception of Risk; Earthscan Publications: London, UK; Sterling, VA, USA, 2000; ISBN 9781317341116. [Google Scholar]
- Obar, J.A.; Wildman, S. Social media definition and the governance challenge: An introduction to the special issue. Telecomm. Policy 2015, 39, 745–750. [Google Scholar] [CrossRef]
- Xue, J.; Chen, J.; Hu, R.; Chen, C.; Zheng, C.; Su, Y.; Zhu, T. Twitter Discussions and Emotions About the COVID-19 Pandemic: Machine Learning Approach. J. Med. Internet Res. 2020, 22, e20550. [Google Scholar] [CrossRef] [PubMed]
- Tchuenche, J.M.; Bauch, C.T.; Xiao, Y.; Beggs, C.B.; Jose, M. Dynamics of an Infectious Disease Where Media Coverage Influences Transmission. ISRN Biomath. 2012, 2012, 581274. [Google Scholar] [CrossRef] [Green Version]
- Cui, J.; Sun, Y.; Zhu, H. The Impact of Media on the Control of Infectious Diseases. J. Dyn. Differ. Equ. 2008, 20, 31–53. [Google Scholar] [CrossRef] [PubMed]
- Sooknanan, J.; Comissiong, D.M.G. Trending on Social Media: Integrating Social Media into Infectious Disease Dynamics. Bull. Math. Biol. 2020, 82, 86. [Google Scholar] [CrossRef]
- Liu, R.; Wu, J.; Zhu, H. Media/Psychological Impact on Multiple Outbreaks of Emerging Infectious Diseases. Comput. Math. Methods Med. 2007, 8, 612372. [Google Scholar] [CrossRef] [Green Version]
- Lu, X.; Wang, S.; Liu, S.; Li, J. An SEI infection model incorporating media impact. Math. Biosci. Eng. 2017, 14, 1317–1335. [Google Scholar] [CrossRef] [Green Version]
- Samaras, L.; García-Barriocanal, E.; Sicilia, M.-A. Comparing Social media and Google to detect and predict severe epidemics. Sci. Rep. 2020, 10, 4747. [Google Scholar] [CrossRef] [Green Version]
- Raamkumar, A.S.; Tan, S.G.; Wee, H.L. Use of Health Belief Model-Based Deep Learning Classifiers for COVID-19 Social Media Content to Examine Public Perceptions of Physical Distancing: Model Development and Case Study. JMIR Pub. Health Surveill. 2020, 6, e20493. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Pacheco, G.; Duran, L.; Esteva, L.; Minzoni, A.; Lopez-Cervantes, M.; Panayotaros, P.; Ahued Ortega, A.; Villasenor Ruiz, I. Modelling of the influenza A(H1N1)v outbreak in Mexico City, April-May 2009, with control sanitary measures. Eurosurveillance 2009, 14, 19254. [Google Scholar] [CrossRef] [PubMed]
- US Dashboard. Available online: https://covid-19.tacc.utexas.edu/dashboards/us/ (accessed on 9 December 2021).
- Sattar, N.S.; Arifuzzaman, S. COVID-19 Vaccination Awareness and Aftermath: Public Sentiment Analysis on Twitter Data and Vaccinated Population Prediction in the USA. Appl. Sci. 2021, 11, 6128. [Google Scholar] [CrossRef]
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Ortiz-Ospina, E.; Hasell, J.; Macdonald, B.; Beltekian, D.; Roser, M. United States: Coronavirus Pandemic Country Profile. Available online: https://ourworldindata.org/coronavirus/country/united-states#citation (accessed on 9 December 2021).
- Rogers, E.M. Diffusion of Innovations, 4th ed.; Free Press: New York, NY, USA; London, UK, 1995; ISBN 0028740742. [Google Scholar]
- Matthews, S.D.; Proctor, M.D. Public Health Informatics, Human Factors and the End-Users. Health Serv. Res. Manag. Epidemiol. 2021, 8, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Bond, S. Just 12 People Are Behind Most Vaccine Hoaxes On Social Media, Research Shows. NPR, 14 May 2021. Available online: https://www.npr.org/2021/05/13/996570855/disinformation-dozen-test-facebooks-twitters-ability-to-curb-vaccine-hoaxes(accessed on 10 December 2021).
- Auxier, B.; Anderson, M. Social Media Use in 2021; Pew Research Centre: Washington, DC, USA, 2021; Available online: https://www.pewresearch.org/internet/2021/04/07/social-media-use-in-2021/ (accessed on 10 December 2021).
- Mckeever, A. Why Even Fully Vaccinated Older People Are at High Risk for Severe COVID-19. Available online: https://www.nationalgeographic.com/science/article/why-older-vaccinated-people-face-higher-risks-for-severe-covid-19 (accessed on 10 December 2021).
- Perrin, A.; Atske, S. 7% of Americans Don’t Use the Internet. Who Are They? Available online: https://www.pewresearch.org/fact-tank/2021/04/02/7-of-americans-dont-use-the-internet-who-are-they/ (accessed on 10 December 2021).
- Haslett, C. The Risks Unvaccinated Americans are Weighing. ABC News, 1 May 2021. Available online: https://abcnews.go.com/Politics/risks-unvaccinated-americans-weighing/story?id=77319410(accessed on 10 December 2021).
- Cooper, I.; Mondal, A.; Antonopoulos, C.G. A SIR model assumption for the spread of COVID-19 in different communities. Chaos Solitons Fractals 2020, 139, 110057. [Google Scholar] [CrossRef]
- Vargas-De-León, C. On the global stability of SIS, SIR and SIRS epidemic models with standard incidence. Chaos Solitons Fractals 2011, 44, 1106–1110. [Google Scholar] [CrossRef]
- Fernández-Villaverde, J.; Jones, C.I. Estimating and Simulating a SIRD Model of COVID-19 for Many Countries, States, and Cities; Working Paper Series No. 27128; National Bureau of Economic Research: Cambridge, MA, USA, 2020; Available online: http://www.nber.org/papers/w27128 (accessed on 9 December 2021).
- Seyoum Desta, B.; Koya, P.R. Modified Model and Stability Analysis of the Spread of Hepatitis B Virus Disease. Am. J. Math. 2019, 7, 13–20. [Google Scholar] [CrossRef]
- Lekone, P.E.; Finkenstädt, B.F. Statistical inference in a stochastic epidemic SEIR model with control intervention: Ebola as a case study. Biometrics 2006, 62, 1170–1177. [Google Scholar] [CrossRef] [Green Version]
- Fan, M.; Li, M.Y.; Wang, K. Global stability of an SEIS epidemic model with recruitment and a varying total population size. Math. Biosci. 2001, 170, 199–208. [Google Scholar] [CrossRef]
- Zhou, Y.; Li, Y. Application of MSEIR Model of Secondary Infection in Pest Control. Multidiscip. J. Sci. Technol. 2019, 6, 10905–10918. [Google Scholar]
- Pinter, G.; Felde, I.; Mosavi, A.; Ghamisi, P.; Gloaguen, R. COVID-19 Pandemic Prediction for Hungary; A Hybrid Machine Learning Approach. Mathematics 2020, 8, 890. [Google Scholar] [CrossRef]
- Bin, S.; Sun, G.; Chen, C.-C. Spread of Infectious Disease Modeling and Analysis of Different Factors on Spread of Infectious Disease Based on Cellular Automata. Int. J. Environ. Res. Public Health 2019, 16, 4683. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greenhalgh, D.; Rana, S.; Samanta, S.; Sardar, T.; Bhattacharya, S.; Chattopadhyay, J. Awareness programs control infectious disease—Multiple delay induced mathematical model. Appl. Math. Comput. 2015, 251, 539–563. [Google Scholar] [CrossRef] [Green Version]
- COVIDAnalytics. Available online: https://www.covidanalytics.io/projections (accessed on 9 December 2021).
- Garibaldi, B.T.; Fiksel, J.; Muschelli, J.; Robinson, M.L.; Rouhizadeh, M.; Perin, J.; Schumock, G.; Nagy, P.; Gray, J.H.; Malapati, H.; et al. Patient Trajectories Among Persons Hospitalized for COVID-19: A Cohort Study. Ann. Intern. Med. 2021, 174, 33–41. [Google Scholar] [CrossRef] [PubMed]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Daghriri, T.; Proctor, M.; Matthews, S. Evolution of Select Epidemiological Modeling and the Rise of Population Sentiment Analysis: A Literature Review and COVID-19 Sentiment Illustration. Int. J. Environ. Res. Public Health 2022, 19, 3230. https://doi.org/10.3390/ijerph19063230
Daghriri T, Proctor M, Matthews S. Evolution of Select Epidemiological Modeling and the Rise of Population Sentiment Analysis: A Literature Review and COVID-19 Sentiment Illustration. International Journal of Environmental Research and Public Health. 2022; 19(6):3230. https://doi.org/10.3390/ijerph19063230
Chicago/Turabian StyleDaghriri, Talal, Michael Proctor, and Sarah Matthews. 2022. "Evolution of Select Epidemiological Modeling and the Rise of Population Sentiment Analysis: A Literature Review and COVID-19 Sentiment Illustration" International Journal of Environmental Research and Public Health 19, no. 6: 3230. https://doi.org/10.3390/ijerph19063230
APA StyleDaghriri, T., Proctor, M., & Matthews, S. (2022). Evolution of Select Epidemiological Modeling and the Rise of Population Sentiment Analysis: A Literature Review and COVID-19 Sentiment Illustration. International Journal of Environmental Research and Public Health, 19(6), 3230. https://doi.org/10.3390/ijerph19063230





