Political Populism, Institutional Distrust and Vaccination Uptake: A Mediation Analysis
Abstract
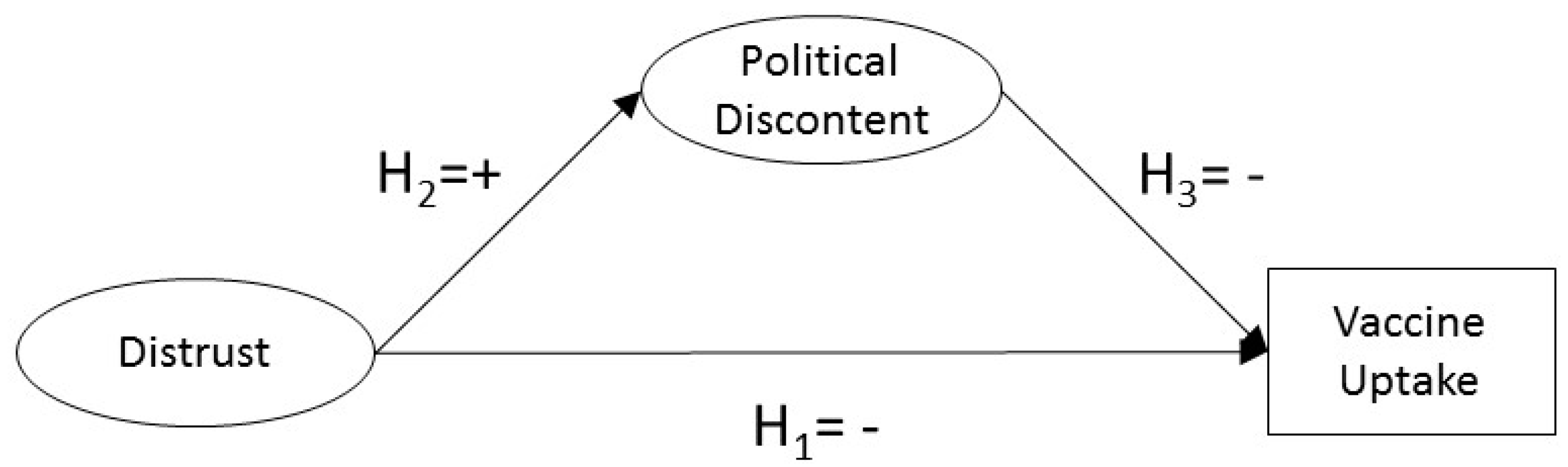
:1. Introduction
2. Conceptual Background
2.1. Trust and Vaccine Uptake
2.2. Political Dissatisfaction, Populism, Vaccine Hesitancy, and Vaccine Uptake
3. Materials and Methods
3.1. Sample
3.2. Measures
3.2.1. Model Measurement Constructs (Distrust)
3.2.2. Mediator Variable (Populism)
3.2.3. Outcome Variable (Vaccine Uptake)
3.2.4. Confounders
3.3. Statistical Analysis
4. Results
| Variable | Categories | Probit | p | Logit | elogit |
|---|---|---|---|---|---|
| Age | 15–24 years | Ref. | Ref. | Ref. | Ref. |
| 25–39 years | −0.082 | 0.000 | −0.148 | 0.862 | |
| 40–54 years | −0.099 | 0.000 | −0.179 | 0.836 | |
| 55 years and older | −0.082 | 0.000 | −0.148 | 0.862 | |
| Occupation | Self-employed | Ref. | Ref. | Ref. | Ref. |
| Managers | 0.038 | 0.001 | 0.069 | 1.071 | |
| Other white collars | 0.006 | 0.637 | 0.011 | 1.011 | |
| Manual workers | −0.001 | 0.962 | −0.002 | 0.998 | |
| House persons | −0.013 | 0.180 | −0.024 | 0.977 | |
| Unemployed | −0.034 | 0.000 | −0.062 | 0.940 | |
| Retired | 0.035 | 0.036 | 0.063 | 1.065 | |
| Students | 0.044 | 0.001 | 0.080 | 1.083 | |
| Education | No full-time education | Ref. | Ref. | Ref. | Ref. |
| Up to 15 years | 0.039 | 0.000 | 0.071 | 1.073 | |
| 16–19 | −0.018 | 0.045 | −0.033 | 0.968 | |
| 20 years and older | −0.094 | 0.000 | −0.170 | 0.844 | |
| Still studying | −0.006 | 0.511 | −0.011 | 0.989 | |
| Childs Living at Home | None | Ref. | Ref. | Ref. | Ref. |
| One | 0.022 | 0.007 | 0.040 | 1.041 | |
| Two | 0.018 | 0.037 | 0.033 | 1.033 | |
| Three | 0.011 | 0.172 | 0.020 | 1.020 | |
| Four or more | −0.004 | 0.631 | −0.007 | 0.993 | |
| Problems Paying Bills | Most of the time | −0.069 | 0.000 | −0.125 | 0.883 |
| From time to time | −0.106 | 0.000 | −0.192 | 0.825 | |
| Almost never/never | Ref. | Ref. | Ref. | Ref. | |
| Social Class | The working class | Ref. | Ref. | Ref. | Ref. |
| The lower middle class | 0.034 | 0.000 | 0.062 | 1.063 | |
| The middle class | 0.041 | 0.000 | 0.074 | 1.077 | |
| The upper middle class | 0.092 | 0.000 | 0.167 | 1.181 | |
| The higher class | 0.014 | 0.084 | 0.025 | 1.026 | |
| Political Left-Right | Left | 0.062 | 0.000 | 0.112 | 1.119 |
| Center | |||||
| Right | 0.015 | 0.059 | 0.027 | 1.028 | |
| Use Online Social Network | Every day or almost every day | Ref. | Ref. | Ref. | Ref. |
| Two or three times a week | 0.016 | 0.066 | 0.029 | 1.029 | |
| About once a week | 0.001 | 0.912 | 0.002 | 1.002 | |
| Two or three times a month | −0.005 | 0.572 | −0.009 | 0.991 | |
| Less often | −0.027 | 0.003 | −0.049 | 0.952 | |
| Never | 0.055 | 0.000 | 0.100 | 1.105 |
5. Discussion
6. Conclusions
7. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Country | Number of Interviews | Population 15+ |
|---|---|---|
| Austria | 1006 | 7,554,711 |
| Belgium | 1041 | 9,693,779 |
| Bulgaria | 1026 | 6,537,535 |
| Croatia | 1010 | 3,796,476 |
| Czech Republic | 1068 | 9,238,431 |
| Denmark | 1017 | 4,838,729 |
| Estonia | 1005 | 1,160,064 |
| Finland | 1000 | 4,747,810 |
| France | 1013 | 54,097,255 |
| Germany | 1507 | 70,160,634 |
| Greece | 1014 | 9,937,810 |
| Hungary | 1030 | 8,781,161 |
| Ireland | 1078 | 3,592,162 |
| Italy | 1021 | 52,334,536 |
| Latvia | 1012 | 1,707,082 |
| Lithuania | 1004 | 2,513,384 |
| Luxemburg | 512 | 457,127 |
| Malta | 497 | 364,171 |
| Netherlands | 1017 | 13,979,215 |
| Poland | 1011 | 33,444,171 |
| Portugal | 1013 | 8,480,126 |
| Republic of Cyprus | 505 | 741,308 |
| Romania | 1025 | 16,852,701 |
| Slovakia | 1020 | 4,586,024 |
| Slovenia | 1016 | 1,760,032 |
| Spain | 1014 | 39,445,245 |
| Sweden | 1021 | 7,998,763 |
| United Kingdom | 1021 | 52,651,777 |
| TOTAL | 27,524 | 431,452,219 |
References
- Velásquez, G. Entre la Ética, la Salud y la Economía. Available online: https://mondiplo.com/entre-la-etica-la-salud-y-la-economia (accessed on 14 September 2021).
- da Fonseca, E.M.; Shadlen, K.C.; Bastos, F.I. The politics of COVID-19 vaccination in middle-income countries: Lessons from Brazil. Soc. Sci. Med. 2021, 281, 114093. [Google Scholar] [CrossRef] [PubMed]
- Greer, S.L.; Bekker, M.; De Leeuw, E.; Wismar, M.; Helderman, J.K.; Ribeiro, S.; Stuckler, D. Policy, politics and public health. Eur. J. Public Health 2017, 27, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Speed, E.; Mannion, R. Populism and health policy: Three international case studies of right-wing populist policy frames. Sociol. Health Illn. 2020, 42, 1967–1981. [Google Scholar] [CrossRef] [PubMed]
- Greer, S.L. Medicine, public health and the populist radical right. J. R. Soc. Med. 2017, 110, 305–308. [Google Scholar] [CrossRef] [PubMed]
- Algan, Y.; Guriev, S.; Papaioannou, E.; Passari, E. The European Trust Crisis and the Rise of Populism. Brook. Pap. Econ. Act. 2017, 78, 309–382. [Google Scholar] [CrossRef] [Green Version]
- Rinaldi, C.; Bekker, M.P.M. A scoping review of populist radical right parties’ influence on welfare policy and its implications for population health in Europe. Int. J. Health Policy Manag. 2021, 10, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Lasco, G.; Curato, N. Medical populism. Soc. Sci. Med. 2019, 221, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Lasco, G. Challenging world leaders amid medical populism. Lancet 2020, 396, 1802–1803. [Google Scholar] [CrossRef]
- Lasco, G. Medical populism and the COVID-19 pandemic. Glob. Public Health 2020, 15, 1417–1429. [Google Scholar] [CrossRef] [PubMed]
- Gugushvili, A.; Koltai, J.; Stuckler, D.; McKee, M. Votes, populism, and pandemics. Int. J. Public Health 2020, 65, 721–722. [Google Scholar] [CrossRef]
- Dubé, E.; Vivion, M.; MacDonald, N.E. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: Influence, impact and implications. Expert Rev. Vaccines 2015, 14, 99–117. [Google Scholar] [CrossRef] [PubMed]
- McKee, M.; Gugushvili, A.; Koltai, J.; Stuckler, D. Are Populist Leaders Creating the Conditions for the Spread of COVID-19?; Comment on “A Scoping Review of Populist Radical Right Parties’ Influence on Welfare Policy and its Implications for Population Health in Europe”. Int. J. Health Policy Manag. 2021, 10, 511–515. [Google Scholar] [CrossRef] [PubMed]
- Koltai, J.; Varchetta, F.M.; McKee, M.; Stuckler, D. Deaths of Despair and Brexit Votes: Cross-Local Authority Statistical Analysis in England and Wales. Am. J. Public Health 2020, 110, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.L.; Keown, L.-A.; Patten, S.B.; Williams, J.A.; Currie, S.R.; Beck, C.A.; Maxwell, C.J.; El-Guebaly, N.A. A population-based study on ways of dealing with daily stress: Comparisons among individuals with mental disorders, with long-term general medical conditions and healthy people. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 44, 666–674. [Google Scholar] [CrossRef] [PubMed]
- Kelland, K.; Polityuk, P. Measles and Mistrust in Ukraine Weaken World’s Defenses. Available online: https://www.reuters.com/article/us-health-measles-ukraine-insight-idUSKBN1XE15T (accessed on 26 February 2022).
- Ghinai, I.; Willott, C.; Dadari, I.; Larson, H.J. Listening to the rumours: What the northern Nigeria polio vaccine boycott can tell us ten years on. Glob. Public Health 2013, 8, 1138–1150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lasco, G.; Yu, V.G. Medical populism and the politics of dengue epidemics in the Global South. Glob. Public Health 2021, 16, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Abramowitz, S. Epidemics (Especially Ebola). Annu. Rev. Anthropol. 2017, 46, 421–445. [Google Scholar] [CrossRef]
- Giuffrida, A. Italy’s Five Star Movement Blamed for Surge in Measles Cases. Available online: https://www.theguardian.com/world/2017/mar/23/italys-five-star-movement-blamed-for-surge-in-measles-cases (accessed on 26 February 2022).
- Bayerlein, M.; Boese, V.A.; Gates, S.; Kamin, K.; Murshed, S.M. Populism and COVID-19: How Populist Governments (Mis)Handle the Pandemic. J. Polit. Inst. Polit. Econ. 2021, 2, 389–428. [Google Scholar]
- Larson, H.J.; Clarke, R.M.; Jarrett, C.; Eckersberger, E.; Levine, Z.; Schulz, W.S.; Paterson, P. Measuring trust in vaccination: A systematic review. Hum. Vaccin. Immunother. 2018, 14, 1599–1609. [Google Scholar] [CrossRef]
- Brewer, N.T.; Chapman, G.B.; Rothman, A.J.; Leask, J.; Kempe, A. Increasing Vaccination: Putting Psychological Science Into Action. Psychol. Sci. Public Interes. 2017, 18, 149–207. [Google Scholar] [CrossRef] [Green Version]
- Larson, H.J.; Schulz, W.S.; Tucker, J.D.; Smith, D.M.D. Measuring vaccine confidence: Introducing a global vaccine confidence index. PLoS Curr. 2015, 7, 1–36. [Google Scholar] [CrossRef] [PubMed]
- Gilles, I.; Bangerter, A.; Clémence, A.; Green, E.G.T.; Krings, F.; Staerklé, C.; Wagner-Egger, P. Trust in medical organizations predicts pandemic (H1N1) 2009 vaccination behavior and perceived efficacy of protection measures in the Swiss public. Eur. J. Epidemiol. 2011, 26, 203–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Casiday, R.; Cresswell, T.; Wilson, D.; Panter-Brick, C. A survey of UK parental attitudes to the MMR vaccine and trust in medical authority. Vaccine 2006, 24, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Hill, L.; Burrell, B.; Walls, T. Factors influencing women’s decisions about having the pertussis-containing vaccine during pregnancy. J. Prim. Health Care 2018, 10, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Cooper, D.L.; Hernandez, N.D.; Rollins, L.; Akintobi, T.H.; McAllister, C. HPV vaccine awareness and the association of trust in cancer information from physicians among males. Vaccine 2017, 35, 2661–2667. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gilkey, M.B.; McRee, A.L.; Magnus, B.E.; Reiter, P.L.; Dempsey, A.F.; Brewer, N.T. Vaccination confidence and parental refusal/delay of early childhood vaccines. PLoS ONE 2016, 11, e0159087. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gilkey, M.B.; Reiter, P.L.; Magnus, B.E.; Mcree, A.-L.; Dempsey, A.F.; Brewer, N.T. Validation of the Vaccination Confidence Scale: A Brief Measure to Identify Parents at Risk for Refusing Adolescent Vaccines. Acad. Pediatr. 2016, 16, 42–49. [Google Scholar] [CrossRef] [Green Version]
- National Vaccine Advisory Committee. Assessing the State of Vaccine Confidence in the United States: Recommendations from the National Vaccine Advisory Committee: Approved by the National Vaccine Advisory Committee on 9 June 2015 [corrected]. Public Health Rep. 2015, 130, 573–595. [Google Scholar] [CrossRef] [Green Version]
- Recio-Román, A.; Recio-Menéndez, M.; Román-González, M.V. Vaccine Hesitancy and Political Populism. An Invariant Cross-European Perspective. Int. J. Environ. Res. Public Health 2021, 18, 12953. [Google Scholar] [CrossRef]
- Oduwole, E.O.; Pienaar, E.D.; Mahomed, H.; Wiysonge, C.S. Current tools available for investigating vaccine hesitancy: A scoping review protocol. BMJ Open 2019, 9, e033245. [Google Scholar] [CrossRef] [Green Version]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Lane, S.; MacDonald, N.E.; Marti, M.; Dumolard, L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015–2017. Vaccine 2018, 36, 3861–3867. [Google Scholar] [CrossRef] [PubMed]
- Van Kessel, S. Populist Parties in Europe: Agents of Discontent?/Stijn van Kessel; Palgrave Macmillan: London, UK, 2015; ISBN 9781137414106. [Google Scholar]
- Guiso, L.; Herrera, H.; Morelli, M.; Sonno, T. Demand and Supply of Populism; EIEF Working Papers Series; Einaudi Institute for Economics and Finance (EIEF): Rome, Italy, 2017. [Google Scholar]
- Nowakowski, A. Do unhappy citizens vote for populism? Eur. J. Polit. Econ. 2021, 68, 101985. [Google Scholar] [CrossRef]
- Elchardus, M.; Spruyt, B. Populism, Persistent Republicanism and Declinism: An Empirical Analysis of Populism as a Thin Ideology. Gov. Oppos. 2016, 51, 111–133. [Google Scholar] [CrossRef] [Green Version]
- Laclau, E. On Populist Reason; Verso: New York, NY, USA, 2005; ISBN 9781859846413. [Google Scholar]
- Berman, S. Populism is a Symptom Rather than a Cause: Democratic Disconnect, the Decline of the Center-Left, and the Rise of Populism in Western Europe. Polity 2019, 51, 654–667. [Google Scholar] [CrossRef]
- Giebler, H.; Hirsch, M.; Schürmann, B.; Veit, S. Discontent with What? Linking Self-Centered and Society-Centered Discontent to Populist Party Support. Polit. Stud. 2020, 69, 900–920. [Google Scholar] [CrossRef]
- Kitschelt, H. Popular Dissatisfaction with Democracy: Populism and Party Systems BT-Democracies and the Populist Challenge; Mény, Y., Surel, Y., Eds.; Palgrave Macmillan: London, UK, 2002; pp. 179–196. ISBN 978-1-4039-2007-2. [Google Scholar]
- Voogd, R.; Dassonneville, R. Are the Supporters of Populist Parties Loyal Voters? Dissatisfaction and Stable Voting for Populist Parties. Gov. Oppos. 2020, 55, 349–370. [Google Scholar] [CrossRef] [Green Version]
- Carvalho Bivar, G.C.; Santini Cesar de Aguilar, M.E.; Cavalcanti Santos, R.V.; Guabelto Cardoso, P.R. COVID-19, the anti-vaccine movement and immunization challenges in Brazil: A review. Sci. Med. 2021, 31, 33. [Google Scholar] [CrossRef]
- Larson, H.J. Stuck. How Vaccine Rumors Start—And Why They Don’t Go Away; Oxford University Press: New York, NY, USA, 2020. [Google Scholar]
- Herwartz, H.; Theilen, B. Health Care and Ideology: A Reconsideration of Political Determinants of Public Healthcare Funding in the OECD. Health Econ. 2014, 23, 225–240. [Google Scholar] [CrossRef] [PubMed]
- Holmberg, C.; Miller, J.H.; Blume, S.; Greenough, P. (Eds.) The Politics of Vaccination. A Global History; Manchester University Press: Manchester, UK, 2017. [Google Scholar]
- Broniatowski, D.A.; Jamison, A.M.; Qi, S.; AlKulaib, L.; Chen, T.; Benton, A.; Quinn, S.C.; Dredze, M. Weaponized Health Communication: Twitter Bots and Russian Trolls Amplify the Vaccine Debate. Am. J. Public Health 2018, 108, 1378–1384. [Google Scholar] [CrossRef]
- Deml, M.J.; Jafflin, K.; Merten, S.; Huber, B.; Buhl, A.; Frau, E.; Mettraux, V.; Sonderegger, J.; Kliem, P.; Cattalani, R.; et al. Determinants of vaccine hesitancy in Switzerland: Study protocol of a mixed-methods national research programme. BMJ Open 2019, 9, e032218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klein, S.L.; Pekosz, A. Sex-based Biology and the Rational Design of Influenza Vaccination Strategies. J. Infect. Dis. 2014, 209, S114–S119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yaqub, O.; Castle-Clarke, S.; Sevdalis, N.; Chataway, J. Attitudes to vaccination: A critical review. Soc. Sci. Med. 2014, 112, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.L. Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar]
- European Commission. Eurobarometer 91.2, March 2019; Gesis Data Archive: ZA7592, Data File Version 1.0.0; Kantar Public: Brussels, Belgium, 2019. [Google Scholar]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Marsh, H.W.; Hau, K.-T.; Wen, Z. In Search of Golden Rules: Comment on Hypothesis-Testing Approaches to Setting Cutoff Values for Fit Indexes and Dangers in Overgeneralizing Hu and Bentler’s (1999) Findings. Struct. Equ. Model. A Multidiscip. J. 2004, 11, 320–341. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B.O. Regression Analysis, Exploratory Factor Analysis, Confirmatory Factor Analysis, and Structural Equation Modeling For Categorical, Censored, and Count Outcomes. Available online: http://www.statmodel.com/download/Topic2-v20[CompatibilityMode]1.pdf (accessed on 14 December 2021).
- Muthén, B.O.; Muthén, L.K.; Asparouhov, T. Regression and Mediation Analysis Using Mplus/Bengt O. Muthén, Linda K. Muthén, Tohomir Asparouhov; Muthén & Muthén: Los Angeles, CA, USA, 2016; ISBN 9780982998311. [Google Scholar]
- Agresti, A. Categorical Data Analysis, 3rd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2013. [Google Scholar]
- Kennedy, J. Populist politics and vaccine hesitancy in Western Europe: An analysis of national-level data. Eur. J. Public Health 2019, 29, 512–516. [Google Scholar] [CrossRef]
- Lee, C.; Whetten, K.; Omer, S.; Pan, W.; Salmon, D. Hurdles to herd immunity: Distrust of government and vaccine refusal in the US, 2002–2003. Vaccine 2016, 34, 3972–3978. [Google Scholar] [CrossRef]
- Das, J.; Das, S. Trust, learning, and vaccination: A case study of a North Indian village. Soc. Sci. Med. 2003, 57, 97–112. [Google Scholar] [CrossRef]
- Manika, D.; Ball, J.G.; Stout, P.A. Factors associated with the persuasiveness of direct-to-consumer advertising on HPV vaccination among young women. J. Health Commun. 2014, 19, 1232–1247. [Google Scholar] [CrossRef]
- Szilagyi, P.G.; Thomas, K.; Shah, M.D.; Vizueta, N.; Cui, Y.; Vangala, S.; Fox, C.; Kapteyn, A. The role of trust in the likelihood of receiving a COVID-19 vaccine: Results from a national survey. Prev. Med. 2021, 153, 106727. [Google Scholar] [CrossRef] [PubMed]
- de Munter, A.C.; Klooster, T.M.S.-v.t.; van Lier, A.; Akkermans, R.; de Melker, H.E.; Ruijs, W.L.M. Determinants of HPV-vaccination uptake and subgroups with a lower uptake in the Netherlands. BMC Public Health 2021, 21, 1848. [Google Scholar] [CrossRef] [PubMed]
- Norris, P. Measuring Populism Worldwide; Harvard Kennedy School-Faculty Research Working Paper Series; Harvard University: Boston, MA, USA, 2020. [Google Scholar]
- Pirro, A.L.P.; Pirro, A.L.P. The Populist Radical Right in Central and Eastern Europe Ideology, Impact, and Electoral Performance Conclusions; ECPR Standing Grp Extremism & Democrac: London, UK, 2015; Volume 27, ISBN 978-1-315-73315-9. [Google Scholar]
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; et al. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ortiz, R.R.; Smith, A.; Coyne-Beasley, T. A systematic literature review to examine the potential for social media to impact HPV vaccine uptake and awareness, knowledge, and attitudes about HPV and HPV vaccination. Hum. Vaccin. Immunother. 2019, 15, 1465–1475. [Google Scholar] [CrossRef] [PubMed]
- Recio-Román, A.; Recio-Menéndez, M.; Román-González, M.V. Global Vaccine Hesitancy Segmentation: A Cross-European Approach. Vaccines 2021, 9, 617. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Social Marketing Guide for Public Health Programme Managers and Practitioners; ECDC: Stockholm, Sweden, 2014; ISBN 9789291936052.
- Opel, D.J.; Diekema, D.S.; Lee, N.R.; Marcuse, E.K. Social marketing as a strategy to increase immunization rates. Arch. Pediatr. Adolesc. Med. 2009, 163, 432–437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nowak, G.J.; Gellin, B.G.; MacDonald, N.E.; Butler, R.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; et al. Addressing vaccine hesitancy: The potential value of commercial and social marketing principles and practices. Vaccine 2015, 33, 4204–4211. [Google Scholar] [CrossRef] [Green Version]
- Washington State Department of Health. Social Marketing Recommendations for COVID-19 Vaccine; Washington State Department of Health: Seattle, WA, USA, 2020.
- Salmon, D.A.; Teret, S.P.; MacIntyre, C.R.; Salisbury, D.; Burgess, M.A.; Halsey, N.A. Compulsory vaccination and conscientious or philosophical exemptions: Past, present, and future. Lancet 2006, 367, 436–442. [Google Scholar] [CrossRef]
- Salmon, D.A.; Dudley, M.Z.; Glanz, J.M.; Omer, S.B. Vaccine hesitancy Causes, consequences, and a call to action. Vaccine 2015, 33, D66–D71. [Google Scholar] [CrossRef]
- Colgrove, J. The ethics and politics of compulsory HPV vaccination. N. Engl. J. Med. 2006, 355, 2389–2391. [Google Scholar] [CrossRef] [Green Version]
- Brito, D.L.; Sheshinski, E.; Intriligator, M.D. Externalities and Compulsory Vaccinations. J. Public Econ. 1991, 45, 69–90. [Google Scholar] [CrossRef]
- French, J.; Deshpande, S.; Evans, W.; Obregon, R. Key guidelines in developing a pre-emptive COVID-19 vaccination uptake promotion strategy. Int. J. Environ. Res. Public Health 2020, 17, 5893. [Google Scholar] [CrossRef] [PubMed]
- Aupers, S. “Trust no one”: Modernization, paranoia and conspiracy culture. Eur. J. Commun. 2012, 27, 22–34. [Google Scholar] [CrossRef] [Green Version]
- Cata-Preta, B.D.; Wehrmeister, F.C.; Santos, T.M.; Barros, A.J.D.; Victora, C.G. Patterns in Wealth-related Inequalities in 86 Low- and Middle-Income Countries: Global Evidence on the Emergence of Vaccine Hesitancy. Am. J. Prev. Med. 2021, 60, S24–S33. [Google Scholar] [CrossRef]

| Paths | Unstandardized Path Coefficient, β Estimate (95% CI) | Standardized Path Coefficient, β Estimate (95% CI) | p |
|---|---|---|---|
| Direct Effect | |||
| D → V | −0.029 (−0.102 0.043) | −0.017 (−0.060 0.025) | 0.432 |
| Indirect Effect | |||
| D → P → V | −0.166 (-0.225 −0.107) | −0.098 (−0.133 −0.063) | <0.001 |
| Total Effect | |||
| D → V | −0.195 (−0.225 −0.165) | −0.115 (−0.133 −0.098) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Recio-Román, A.; Recio-Menéndez, M.; Román-González, M.V. Political Populism, Institutional Distrust and Vaccination Uptake: A Mediation Analysis. Int. J. Environ. Res. Public Health 2022, 19, 3265. https://doi.org/10.3390/ijerph19063265
Recio-Román A, Recio-Menéndez M, Román-González MV. Political Populism, Institutional Distrust and Vaccination Uptake: A Mediation Analysis. International Journal of Environmental Research and Public Health. 2022; 19(6):3265. https://doi.org/10.3390/ijerph19063265
Chicago/Turabian StyleRecio-Román, Almudena, Manuel Recio-Menéndez, and María Victoria Román-González. 2022. "Political Populism, Institutional Distrust and Vaccination Uptake: A Mediation Analysis" International Journal of Environmental Research and Public Health 19, no. 6: 3265. https://doi.org/10.3390/ijerph19063265
APA StyleRecio-Román, A., Recio-Menéndez, M., & Román-González, M. V. (2022). Political Populism, Institutional Distrust and Vaccination Uptake: A Mediation Analysis. International Journal of Environmental Research and Public Health, 19(6), 3265. https://doi.org/10.3390/ijerph19063265






