Effects of Mindfulness Meditation on Doctors’ Mindfulness, Patient Safety Culture, Patient Safety Competency and Adverse Event
Abstract
:1. Introduction
1.1. Patient Safety
1.2. Patient Safety Competency
1.3. Mindfulness
2. Methods
2.1. Participants
2.2. Instruments
2.3. Mindfulness Meditation Intervention
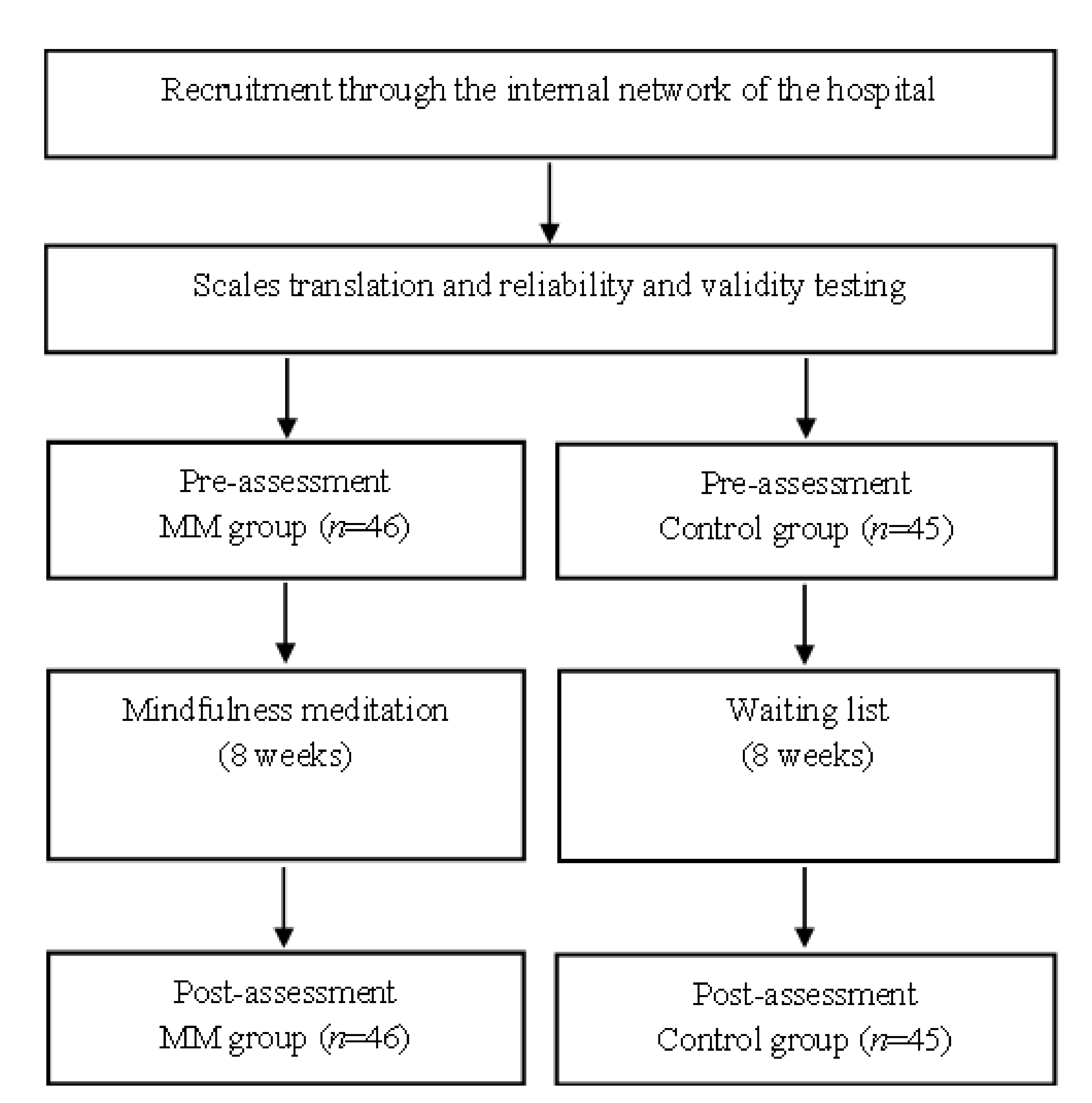
2.4. Procedure and Design
2.5. Data Analysis
3. Results
4. Discussion
4.1. Mindfulness and Safety Culture
4.2. Mindfulness and Safety Competencies
4.3. Mindfulness and Adverse Events
4.4. Research Limitations and Future Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bates, D.W.; Singh, H. Two decades since to err is human: An assessment of progress and emerging priorities in patient safety. Health Aff. 2018, 37, 1736–1743. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Global Patient Safety Action Plan 2021–2030: Towards Eliminating Avoidable Harm in Health Care; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Astier-Peña, M.P.; Martínez-Bianchi, V.; Torijano-Casalengua, M.L.; Ares-Blanco, S.; Bueno-Ortiz, J.-M.; Férnandez-García, M. The Global Patient Safety Action Plan 2021–2030: Identifying actions for safer primary health care. Aten. Primaria 2021, 53, 102224. [Google Scholar] [CrossRef] [PubMed]
- Schwendimann, R.; Blatter, C.; Dhaini, S.; Simon, M.; Ausserhofer, D. The occurrence, types, consequences and preventability of in-hospital adverse events—A scoping review. BMC Health Serv. Res. 2018, 18, 521. [Google Scholar] [CrossRef] [PubMed]
- Wong, B.M.; Baum, K.D.; Headrick, L.A.; Holmboe, E.S.; Moss, F.; Ogrinc, G.; Shojania, K.G.; Vaux, E.; Warm, E.J.; Frank, J.R. Building the bridge to quality: An urgent call to integrate quality improvement and patient safety education with clinical care. Acad. Med. 2020, 95, 59–68. [Google Scholar] [CrossRef] [Green Version]
- Goolsarran, N.; Hamo, C.E.; Lane, S.; Frawley, S.; Lu, W.-H. Effectiveness of an interprofessional patient safety team-based learning simulation experience on healthcare professional trainees. BMC Med. Educ. 2018, 18, 192. [Google Scholar] [CrossRef] [Green Version]
- Auraaen, A.; Slawomirski, L.; Klazinga, N. The Economics of Patient Safety in Primary and Ambulatory Care: Flying Blind; OECD Health Working Papers, No. 106; OECD Publishing: Paris, France, 2018. [Google Scholar]
- Gartland, R.M.; Bloom, J.P.; Fong, Z.V.; DeRoo, C.; Dwyer, K.; Quinn, G.; Lillemoe, K.; Mort, E. What have we learned from malpractice claims involving the surgical management of benign biliary disease?: A 128 million dollar question. Ann. Surg. 2019, 269, 785–791. [Google Scholar] [CrossRef]
- Spence Laschinger, H.K.; Wong, C.; Read, E.; Cummings, G.; Leiter, M.; Macphee, M.; Regan, S.; Rhéaume-Brüning, A.; Ritchie, J.; Burkoski, V. Predictors of new graduate nurses’ health over the first 4 years of practice. Nurs. Open 2019, 6, 245–259. [Google Scholar] [CrossRef]
- Tajabadi, A.; Ahmadi, F.; Sadooghi Asl, A.; Vaismoradi, M. Unsafe nursing documentation: A qualitative content analysis. Nurs. Ethics 2020, 27, 1213–1224. [Google Scholar] [CrossRef] [Green Version]
- Carthon, J.M.B.; Davis, L.; Dierkes, A.; Hatfield, L.; Hedgeland, T.; Holland, S.; Plover, C.; Sanders, A.M.; Visco, F.; Ballinghoff, J. Association of nurse engagement and nurse staffing on patient safety. J. Nurs. Care Qual. 2019, 34, 40. [Google Scholar] [CrossRef]
- Marcomini, I.; Destrebecq, A.; Rosa, D.; Terzoni, S. Self-reported skills for ensuring patient safety and quality of care among Italian nursing students: A descriptive cross-sectional study. Int. J. Health Promot. Educ. 2021, 6, 1–12. [Google Scholar] [CrossRef]
- Hwang, J.-I.; Kim, S.W.; Chin, H.J. Patient participation in patient safety and its relationships with nurses’ patient-centered care competency, teamwork, and safety climate. Asian Nurs. Res. 2019, 13, 130–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, C.M. Origin and uses of primum non nocere—Above all, do no harm! J. Clin. Pharmacol. 2005, 45, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Jiang, K.; Tian, L.; Yan, C.; Li, Y.; Fang, H.; Peihang, S.; Li, P.; Jia, H.; Wang, Y.; Kang, Z. A cross-sectional survey on patient safety culture in secondary hospitals of Northeast China. PLoS ONE 2019, 14, e0213055. [Google Scholar]
- Huang, C.-H.; Wu, H.-H.; Lee, Y.-C. The perceptions of patient safety culture: A difference between physicians and nurses in Taiwan. Appl. Nurs. Res. 2018, 40, 39–44. [Google Scholar] [CrossRef]
- Hessels, A.; Paliwal, M.; Weaver, S.H.; Siddiqui, D.; Wurmser, T.A. Impact of patient safety culture on missed nursing care and adverse patient events. J. Nurs. Care Qual. 2019, 34, 287. [Google Scholar] [CrossRef]
- Han, Y.; Kim, J.-S.; Seo, Y. Cross-sectional study on patient safety culture, patient safety competency, and adverse events. West. J. Nurs. Res. 2020, 42, 32–40. [Google Scholar] [CrossRef]
- Lawati, M.H.A.; Dennis, S.; Short, S.D.; Abdulhadi, N.N. Patient safety and safety culture in primary health care: A systematic review. BMC Fam. Pract. 2018, 19, 104. [Google Scholar] [CrossRef] [Green Version]
- Morris, T.L.; Hancock, D.R. Institute of Medicine core competencies as a foundation for nursing program evaluation. Nurs. Educ. Perspect. 2013, 34, 29–33. [Google Scholar] [CrossRef]
- Kryzanowski, J.; Bloomquist, C.D.; Dunn-Pierce, T.; Murphy, L.; Clarke, S.; Neudorf, C. Quality improvement as a population health promotion opportunity to reorient the healthcare system. Can. J. Public Health 2019, 110, 58–61. [Google Scholar] [CrossRef]
- Kim, Y.M.; Yoon, Y.S.; Hong, H.C.; Min, A. Effects of a patient safety course using a flipped classroom approach among undergraduate nursing students: A quasi-experimental study. Nurse Educ. Today 2019, 79, 180–187. [Google Scholar] [CrossRef]
- Gong, Y. Safety culture among Chinese undergraduates: A survey at a university. Saf. Sci. 2019, 111, 17–21. [Google Scholar] [CrossRef]
- Kong, L.-n.; Zhu, W.-F.; He, S.; Chen, S.-Z.; Yang, L.; Qi, L.; Peng, X. Attitudes towards patient safety culture among postgraduate nursing students in China: A cross-sectional study. Nurse Educ. Pract. 2019, 38, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.E.; Quinn, B.L. Safety culture and patient safety outcomes in East Asia: A literature review. West. J. Nurs. Res. 2020, 42, 220–230. [Google Scholar] [CrossRef] [PubMed]
- Eva, K.W.; Armson, H.; Holmboe, E.; Lockyer, J.; Loney, E.; Mann, K.; Sargeant, J. Factors influencing responsiveness to feedback: On the interplay between fear, confidence, and reasoning processes. Adv. Health Sci. Educ. 2012, 17, 15–26. [Google Scholar] [CrossRef] [Green Version]
- Chan, T.M.; Mercuri, M.; Turcotte, M.; Gardiner, E.; Sherbino, J.; de Wit, K. Making decisions in the era of the clinical decision rule: How emergency physicians use clinical decision rules. Acad. Med. 2020, 95, 1230–1237. [Google Scholar] [CrossRef]
- Braun, S.E.; Kinser, P.A.; Rybarczyk, B. Can mindfulness in health care professionals improve patient care? An integrative review and proposed model. Transl. Behav. Med. 2019, 9, 187–201. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. The Liberative Potential of Mindfulness. Mindfulness 2021, 12, 1555–1563. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Meditation is not what you think. Mindfulness 2021, 12, 784–787. [Google Scholar] [CrossRef]
- Strohmaier, S.; Jones, F.W.; Cane, J.E. Effects of length of mindfulness practice on mindfulness, depression, anxiety, and stress: A randomized controlled experiment. Mindfulness 2021, 12, 198–214. [Google Scholar] [CrossRef]
- Liu, C.; Chen, H.; Liu, C.-Y.; Lin, R.-T.; Chiou, W.-K. The effect of loving-kindness meditation on flight attendants’ spirituality, mindfulness and subjective well-being. Healthcare 2020, 8, 174. [Google Scholar] [CrossRef]
- Liu, C.; Chen, H.; Liu, C.-Y.; Lin, R.-T.; Chiou, W.-K. Cooperative and individual mandala drawing have different effects on mindfulness, spirituality, and subjective well-being. Front. Psychol. 2020, 11, 2629. [Google Scholar] [CrossRef]
- Chen, H.; Liu, C.; Cao, X.; Hong, B.; Huang, D.-H.; Liu, C.-Y.; Chiou, W.-K. Effects of Loving-Kindness Meditation on Doctors’ Mindfulness, Empathy, and Communication Skills. Int. J. Environ. Res. Public Health 2021, 18, 4033. [Google Scholar] [CrossRef] [PubMed]
- Ito, T.A.; Larsen, J.T.; Smith, N.K.; Cacioppo, J.T. Negative information weighs more heavily on the brain: The negativity bias in evaluative categorizations. J. Personal. Soc. Psychol. 1998, 75, 887. [Google Scholar] [CrossRef]
- Weis, R.; Ray, S.D.; Cohen, T.A. Mindfulness as a way to cope with COVID-19-related stress and anxiety. Couns. Psychother. Res. 2021, 21, 8–18. [Google Scholar] [CrossRef]
- Braun, S.E.; Dow, A.; Loughan, A.; Mladen, S.; Crawford, M.; Rybarczyk, B.; Kinser, P. Mindfulness training for healthcare professional students: A waitlist controlled pilot study on psychological and work-relevant outcomes. Complement. Ther. Med. 2020, 51, 102405. [Google Scholar] [CrossRef] [Green Version]
- Ginsburg, L.; Castel, E.; Tregunno, D.; Norton, P.G. The H-PEPSS: An instrument to measure health professionals’ perceptions of patient safety competence at entry into practice. BMJ Qual. Saf. 2012, 21, 676–684. [Google Scholar] [CrossRef]
- Chen, L.; Huang, F.; Yuan, X.; Song, J.; Chen, L. An assessment of the reliability and factorial validity of the Chinese version of the health professional education in patient safety survey (H-PEPSS). Front. Psychol. 2019, 10, 2183. [Google Scholar] [CrossRef]
- Brown, K.W.; Ryan, R.M. The benefits of being present: Mindfulness and its role in psychological well-being. J. Personal. Soc. Psychol. 2003, 84, 822. [Google Scholar] [CrossRef] [Green Version]
- Deng, Y.-Q.; Li, S.; Tang, Y.-Y.; Zhu, L.-H.; Ryan, R.; Brown, K. Psychometric properties of the Chinese translation of the mindful attention awareness scale (MAAS). Mindfulness 2012, 3, 10–14. [Google Scholar] [CrossRef]
- Sorra, J.; Gray, L.; Streagle, S.; Famolaro, T.; Yount, N.; Behm, J. AHRQ Hospital Survey on Patient Safety Culture: User’s Guide; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2016. [Google Scholar]
- Chen, I.C.; Li, H.-H. Measuring patient safety culture in Taiwan using the Hospital Survey on Patient Safety Culture (HSOPSC). BMC Health Serv. Res. 2010, 10, 152. [Google Scholar] [CrossRef] [Green Version]
- Nie, Y.; Mao, X.; Cui, H.; He, S.; Li, J.; Zhang, M. Hospital survey on patient safety culture in China. BMC Health Serv. Res. 2013, 13, 228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teng, C.-I.; Shyu, Y.-I.L.; Chiou, W.-K.; Fan, H.-C.; Lam, S.M. Interactive effects of nurse-experienced time pressure and burnout on patient safety: A cross-sectional survey. Int. J. Nurs. Stud. 2010, 47, 1442–1450. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.Y.; Friesner, D.; Lee, I.C.; Chu, T.L.; Chen, H.L.; Wu, W.E.; Teng, C.I. Openness to experience, work experience and patient safety. J. Nurs. Manag. 2016, 24, 1098–1108. [Google Scholar] [CrossRef] [PubMed]
- Bamber, M.D.; Morpeth, E. Effects of mindfulness meditation on college student anxiety: A meta-analysis. Mindfulness 2019, 10, 203–214. [Google Scholar] [CrossRef]
- Manigault, A.W.; Slutsky, J.; Raye, J.; Creswell, J.D. Examining Practice Effects in a Randomized Controlled Trial: Daily Life Mindfulness Practice Predicts Stress Buffering Effects of Mindfulness Meditation Training. Mindfulness 2021, 12, 2487–2497. [Google Scholar] [CrossRef]
- Gao, L.; Curtiss, J.; Liu, X.; Hofmann, S.G. Differential treatment mechanisms in mindfulness meditation and progressive muscle relaxation. Mindfulness 2018, 9, 1268–1279. [Google Scholar] [CrossRef]
- Wu, R.; Liu, L.-L.; Zhu, H.; Su, W.-J.; Cao, Z.-Y.; Zhong, S.-Y.; Liu, X.-H.; Jiang, C.-L. Brief mindfulness meditation improves emotion processing. Front. Neurosci. 2019, 13, 1074. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Liu, F.; Zhang, Q.; Liu, X.; Wei, P. The effect of mindfulness training on proactive and reactive cognitive control. Front. Psychol. 2018, 9, 1002. [Google Scholar] [CrossRef] [Green Version]
- Kabat-Zinn, J. Mindfulness-based interventions in context: Past, present, and future. Clin. Psychol. Sci. Pract. 2003, 10, 144–156. [Google Scholar] [CrossRef]
- Grabovac, A.D.; Lau, M.A.; Willett, B.R. Mechanisms of mindfulness: A Buddhist psychological model. Mindfulness 2011, 2, 154–166. [Google Scholar] [CrossRef]
- Strong, S.D. Contemplative psychotherapy: Clinician mindfulness, Buddhist psychology, and the therapeutic common factors. J. Psychother. Integr. 2021, 31, 146–162. [Google Scholar] [CrossRef]
- Fulton, P.R.; Siegel, R.D. Buddhist and western psychology: Seeking common ground. In Mindfulness and Psychotherapy; The Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Kang, C.; Whittingham, K. Mindfulness: A dialogue between Buddhism and clinical psychology. Mindfulness 2010, 1, 161–173. [Google Scholar] [CrossRef]
- Jones, P. Mindfulness training: Can it create superheroes? Front. Psychol. 2019, 10, 613. [Google Scholar] [CrossRef] [PubMed]
- Marques, J. At the intersection of workplace spirituality and Buddhist psychology: A critical summary of literature. J. Glob. Responsib. 2021, 12, 137–157. [Google Scholar] [CrossRef]
- Miller, C.S.; Scott, S.D.; Beck, M. Second victims and mindfulness: A systematic review. J. Patient Saf. Risk Manag. 2019, 24, 108–117. [Google Scholar] [CrossRef]
- Renecle, M.; Tomás, I.; Gracia, F.J.; Peiró, J.M. Spanish validation of the mindful organizing scale: A questionnaire for the assessment of collective mindfulness. Accid. Anal. Prev. 2020, 134, 105351. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Córcoles, M.; Vogus, T.J. Mindful organizing for safety. Saf. Sci. 2020, 124, 1–5. [Google Scholar] [CrossRef]
- Parchment, J. Mindfulness: A necessary leadership competency. Nurs. Made Incred. Easy 2022, 20, 17–20. [Google Scholar] [CrossRef]
- de Bienassis, K.; Kristensen, S.; Burtscher, M.; Brownwood, I.; Klazinga, N.S. Culture as a Cure: Assessments of Patient Safety Culture in OECD Countries; OECD Health Working Papers, No. 119; OECD Publishing: Paris, France, 2020. [Google Scholar]
- Hofert, S.M.; Tackett, S.; Gould, n.; Sibinga, E. Mindfulness instruction for community-hospital physicians for burnout and patient care: A pilot study. J. Patient Saf. Risk Manag. 2020, 25, 15–21. [Google Scholar] [CrossRef]
- Ravi, D.; Tawfik, D.S.; Sexton, J.B.; Profit, J. Changing safety culture. J. Perinatol. 2021, 41, 2552–2560. [Google Scholar] [CrossRef]
- Lamothe, M.; McDuff, P.; Pastore, Y.D.; Duval, M.; Sultan, S. Developing professional caregivers’ empathy and emotional competencies through mindfulness-based stress reduction (MBSR): Results of two proof-of-concept studies. BMJ Open 2018, 8, e018421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mazur, L.M.; Marks, L.B.; McLeod, R.; Karwowski, W.; Mosaly, P.; Tracton, G.; Adams, R.D.; Hoyle, L.; Das, S.; Chera, B. Promoting safety mindfulness: Recommendations for the design and use of simulation-based training in radiation therapy. Adv. Radiat. Oncol. 2018, 3, 197–204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kerry, M.J.; Ander, D.S. Mindfulness fostering of interprofessional simulation training for collaborative practice. BMJ Simul. Technol. Enhanc. Learn. 2018, 7, 106–116. [Google Scholar] [CrossRef]
- Van Gordon, W.; Sapthiang, S.; Shonin, E.; Griffiths, M. Mindfulness for addressing key public health concerns in young people: Preventative applications and safety concerns. Educ. Health 2019, 37, 9–14. [Google Scholar]
- Struth, D.L. Dispositional Mindfulness in Senior-Level Nursing Students: Examining the Relationship to Situation Awareness and Clinical Outcomes. Ph.D. Thesis, Indiana University of Pennsylvania, Indiana, PA, USA, 2019. [Google Scholar]
- Brown, R.G.; Fernie, B.A. Metacognitions, anxiety, and distress related to motor fluctuations in Parkinson’s disease. J. Psychosom. Res. 2015, 78, 143–148. [Google Scholar] [CrossRef]
- Gawande, R.; Pine, E.; Griswold, T.; Creedon, T.; Vallejo, Z.; Rosenbaum, E.; Lozada, A.; Schuman-Olivier, Z. Insurance-reimbursable mindfulness for safety-net primary care patients: A pilot randomized controlled trial. Mindfulness 2019, 10, 1744–1759. [Google Scholar] [CrossRef]
- Altmiller, G. “Perioperative Unfolding Case Study”—A Lesson in Quality and Safety. AORN J. 2020, 112, 104–111. [Google Scholar] [CrossRef]
- Basler, J.; Lancaster, R.J.; Schmitt, C.A.; Hong, P.Y.; Malcore, M.; Docter, A.; Wallace-Leece, J. Mindfulness and Patient Safety Simulation in Third-Year Baccalaureate Students. Clin. Simul. Nurs. 2020, 42, 8–11. [Google Scholar] [CrossRef]
- Brady, S.; O’Connor, N.; Burgermeister, D.; Hanson, P. The impact of mindfulness meditation in promoting a culture of safety on an acute psychiatric unit. Perspect. Psychiatr. Care 2012, 48, 129–137. [Google Scholar] [CrossRef]
- Haynes, A.B.; Weiser, T.G.; Berry, W.R.; Lipsitz, S.R.; Breizat, A.-H.S.; Dellinger, E.P.; Dziekan, G.; Herbosa, T.; Kibatala, P.L.; Lapitan, M.C.M. Changes in safety attitude and relationship to decreased postoperative morbidity and mortality following implementation of a checklist-based surgical safety intervention. BMJ Qual. Saf. 2011, 20, 102–107. [Google Scholar] [CrossRef]
- Koppel, S.; Bugeja, L.; Hua, P.; Osborne, R.; Stephens, A.N.; Young, K.L.; Chambers, R.; Hassed, C. Do mindfulness interventions improve road safety? A systematic review. Accid. Anal. Prev. 2019, 123, 88–98. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wu, C. The influence of dispositional mindfulness on safety behaviors: A dual process perspective. Accid. Anal. Prev. 2014, 70, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Chen, H.; Xin, X.; Ji, M. The influence of mindfulness on mental state with regard to safety among civil pilots. J. Air Transp. Manag. 2020, 84, 101768. [Google Scholar] [CrossRef]
- Parnas, S.; Isobel, S. Using relational mindfulness to facilitate safety in the clinical encounter. Australas. Psychiatry 2019, 27, 596–599. [Google Scholar] [CrossRef] [PubMed]
- Feldman, G.; Greeson, J.; Renna, M.; Robbins-Monteith, K. Mindfulness predicts less texting while driving among young adults: Examining attention-and emotion-regulation motives as potential mediators. Personal. Individ. Differ. 2011, 51, 856–861. [Google Scholar] [CrossRef] [Green Version]

| Characteristic | Total | MM Group | Control Group |
|---|---|---|---|
| Age (SD) | 39.71 (7.82) | 38.42 (8.13) | 41.03 (6.54) |
| Male (%) | 37 (41%) | 19 (41.3%) | 18 (40%) |
| Female (%) | 54 (59%) | 27 (58.7%) | 27 (60%) |
| Group | Measure | Mean (SD) | |
|---|---|---|---|
| Pre | Post | ||
| MM | MAAS | 2.878(0.765) | 3.560(0.748) |
| PEPSS | 3.701(0.880) | 4.318(0.908) | |
| HSOPSC | 3.154(0.838) | 3.737(0.850) | |
| MAE | 5.065(0.437) | ||
| Control | MAAS | 3.038(0.837) | 2.929(0.727) |
| PEPSS | 3.842(0.953) | 3.931(0.771) | |
| HSOPSC | 3.301(0.843) | 3.202(0.803) | |
| MAE | 4.804(0.391) | ||
| Measure | Variable | F | p | η2 |
|---|---|---|---|---|
| MAAS | Time ** | 6.753 | 0.011 | 0.071 |
| Group * | 3.976 | 0.049 | 0.043 | |
| Time × Group *** | 12.875 | <0.001 | 0.126 | |
| PEPSS | Time ** | 8.813 | 0.004 | 0.090 |
| Group | 0.761 | 0.385 | 0.008 | |
| Time × Group * | 4.928 | 0.029 | 0.052 | |
| HSOPSC | Time * | 4.063 | 0.047 | 0.044 |
| Group | 2.332 | 0.130 | 0.026 | |
| Time × Group ** | 8.017 | 0.006 | 0.083 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, C.; Chen, H.; Cao, X.; Sun, Y.; Liu, C.-Y.; Wu, K.; Liang, Y.-C.; Hsu, S.-E.; Huang, D.-H.; Chiou, W.-K. Effects of Mindfulness Meditation on Doctors’ Mindfulness, Patient Safety Culture, Patient Safety Competency and Adverse Event. Int. J. Environ. Res. Public Health 2022, 19, 3282. https://doi.org/10.3390/ijerph19063282
Liu C, Chen H, Cao X, Sun Y, Liu C-Y, Wu K, Liang Y-C, Hsu S-E, Huang D-H, Chiou W-K. Effects of Mindfulness Meditation on Doctors’ Mindfulness, Patient Safety Culture, Patient Safety Competency and Adverse Event. International Journal of Environmental Research and Public Health. 2022; 19(6):3282. https://doi.org/10.3390/ijerph19063282
Chicago/Turabian StyleLiu, Chao, Hao Chen, Xinyi Cao, Yini Sun, Chia-Yih Liu, Kan Wu, Yu-Chao Liang, Szu-Erh Hsu, Ding-Hau Huang, and Wen-Ko Chiou. 2022. "Effects of Mindfulness Meditation on Doctors’ Mindfulness, Patient Safety Culture, Patient Safety Competency and Adverse Event" International Journal of Environmental Research and Public Health 19, no. 6: 3282. https://doi.org/10.3390/ijerph19063282
APA StyleLiu, C., Chen, H., Cao, X., Sun, Y., Liu, C.-Y., Wu, K., Liang, Y.-C., Hsu, S.-E., Huang, D.-H., & Chiou, W.-K. (2022). Effects of Mindfulness Meditation on Doctors’ Mindfulness, Patient Safety Culture, Patient Safety Competency and Adverse Event. International Journal of Environmental Research and Public Health, 19(6), 3282. https://doi.org/10.3390/ijerph19063282







