Trends of Multimorbidity Patterns over 16 Years in Older Taiwanese People and Their Relationship to Mortality
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Variables
2.3. Statistical Analysis
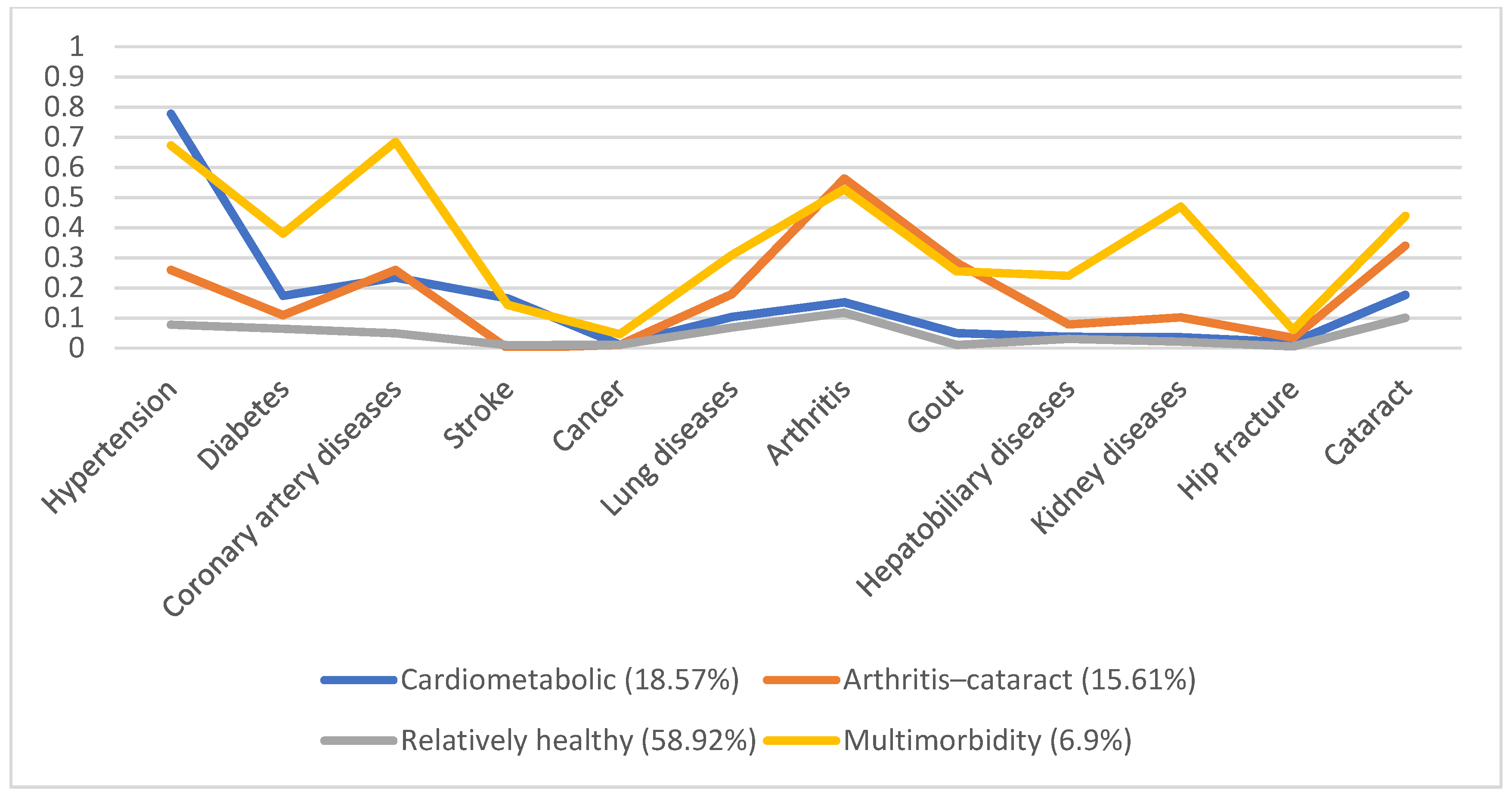
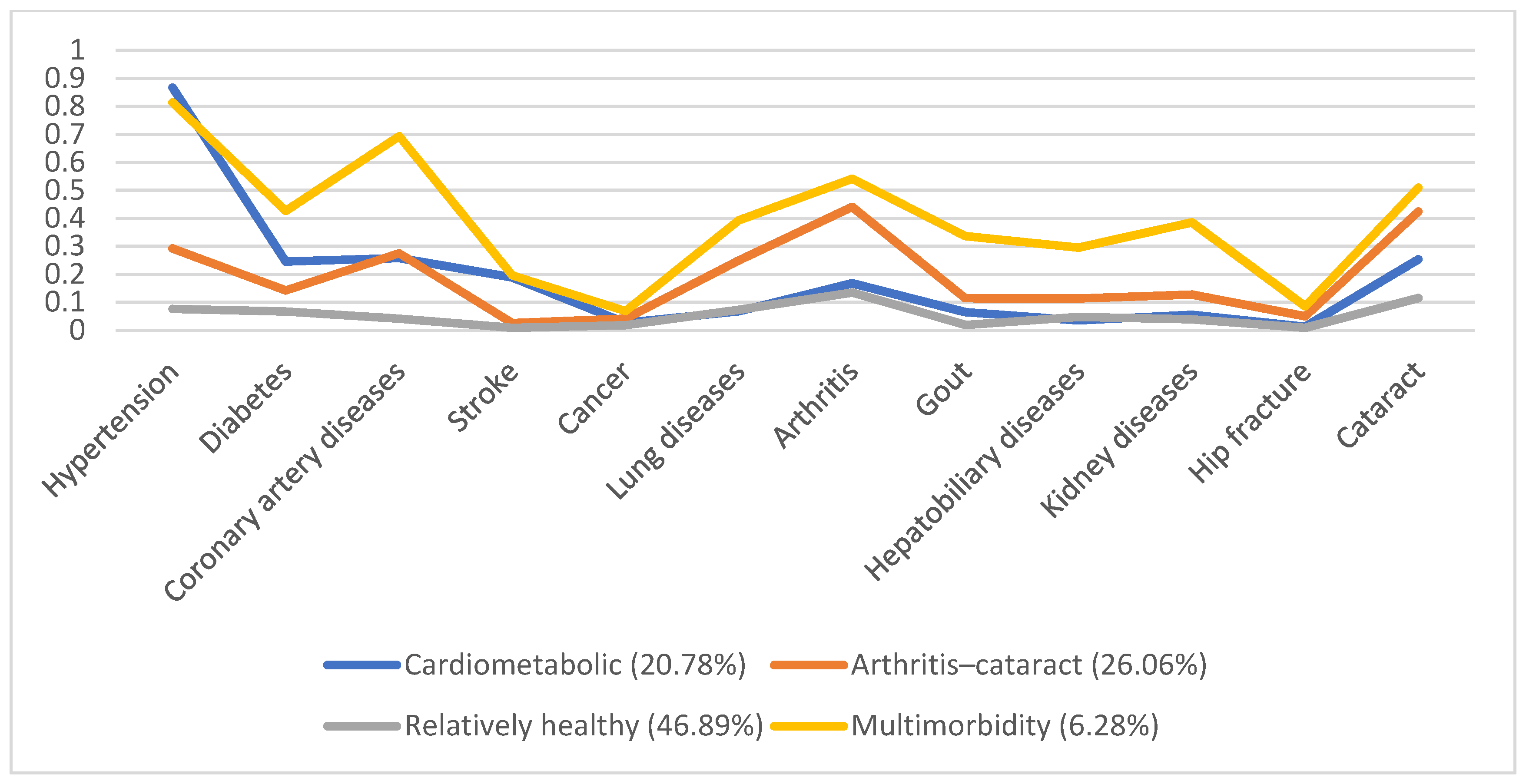
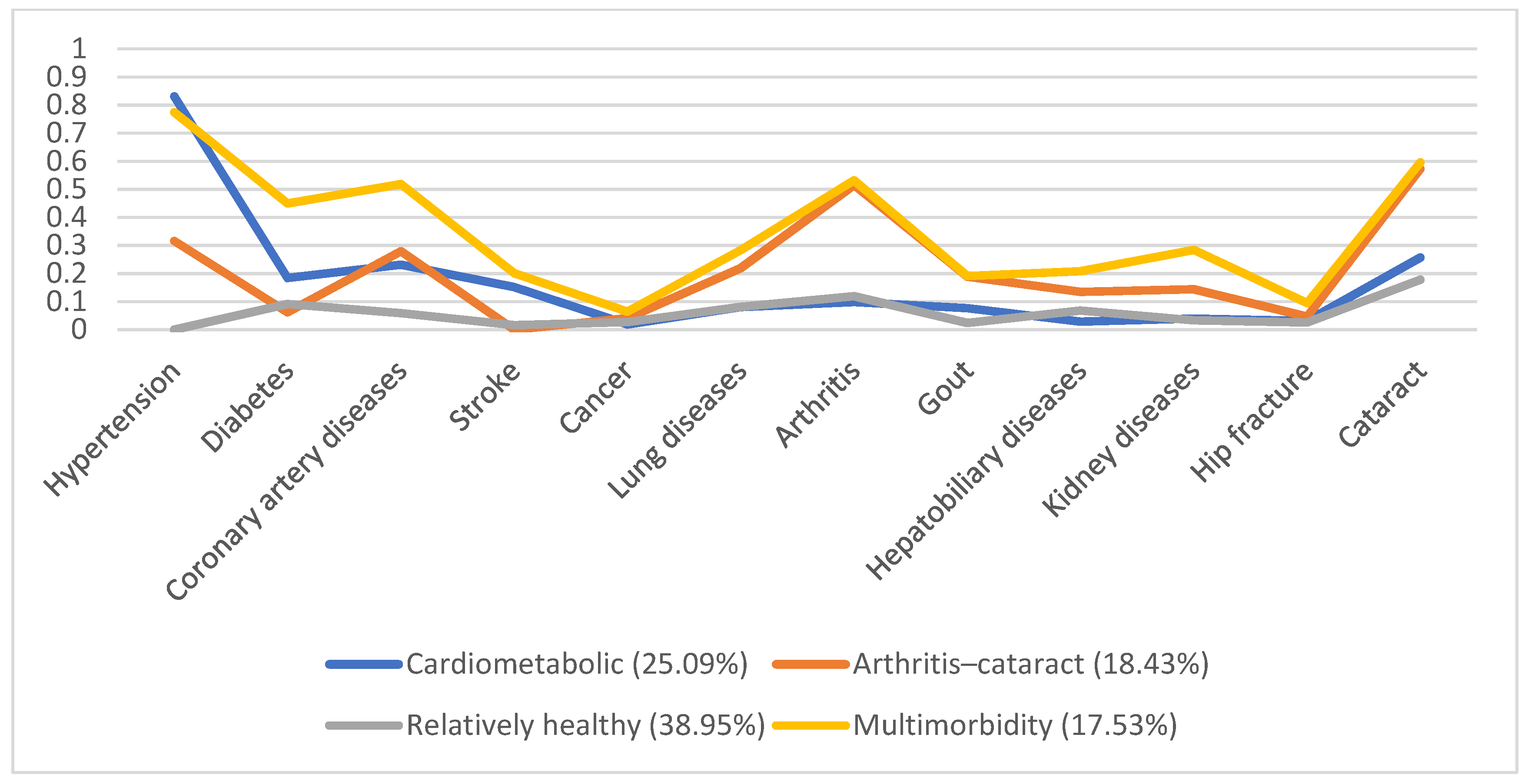
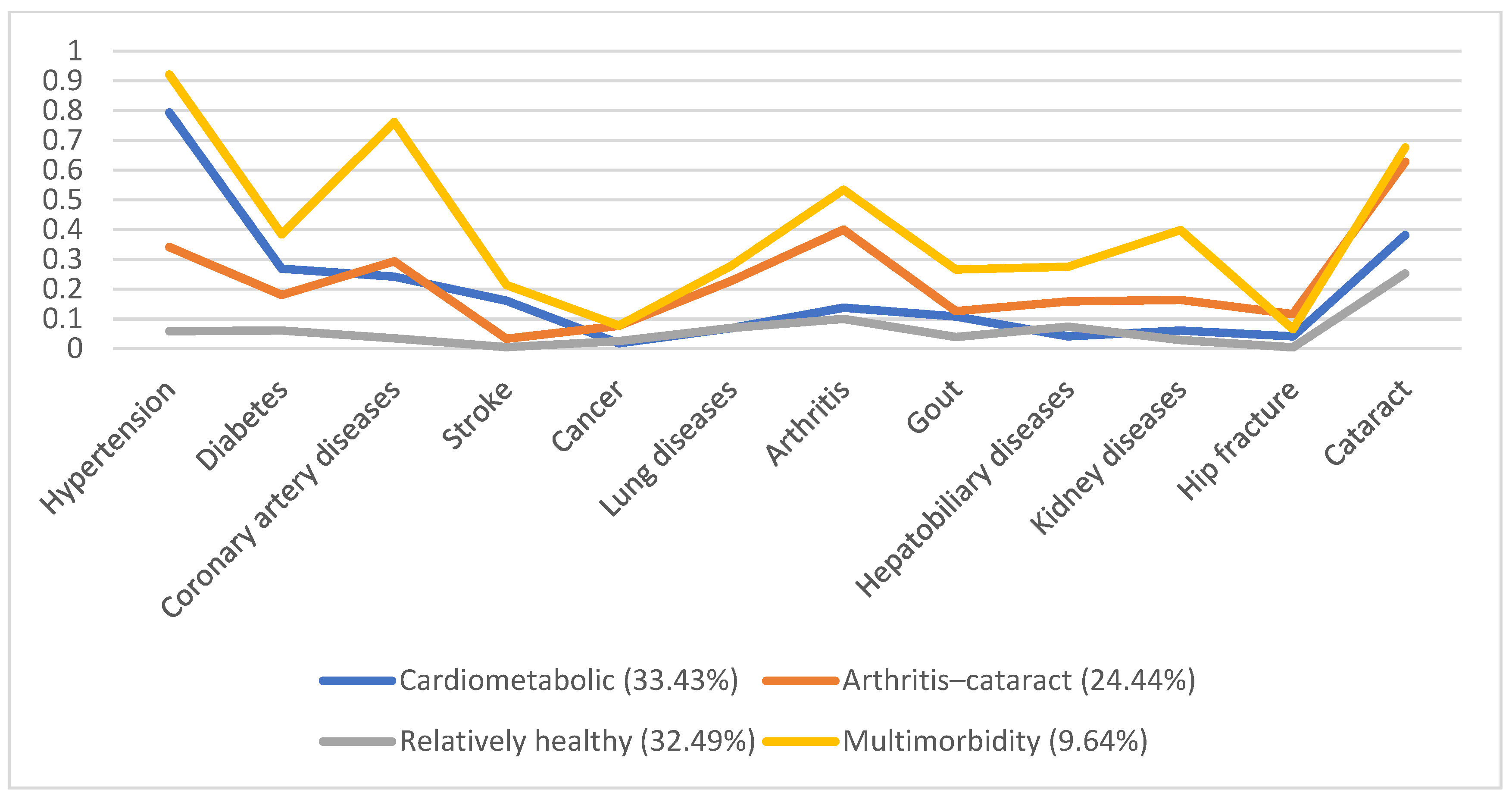
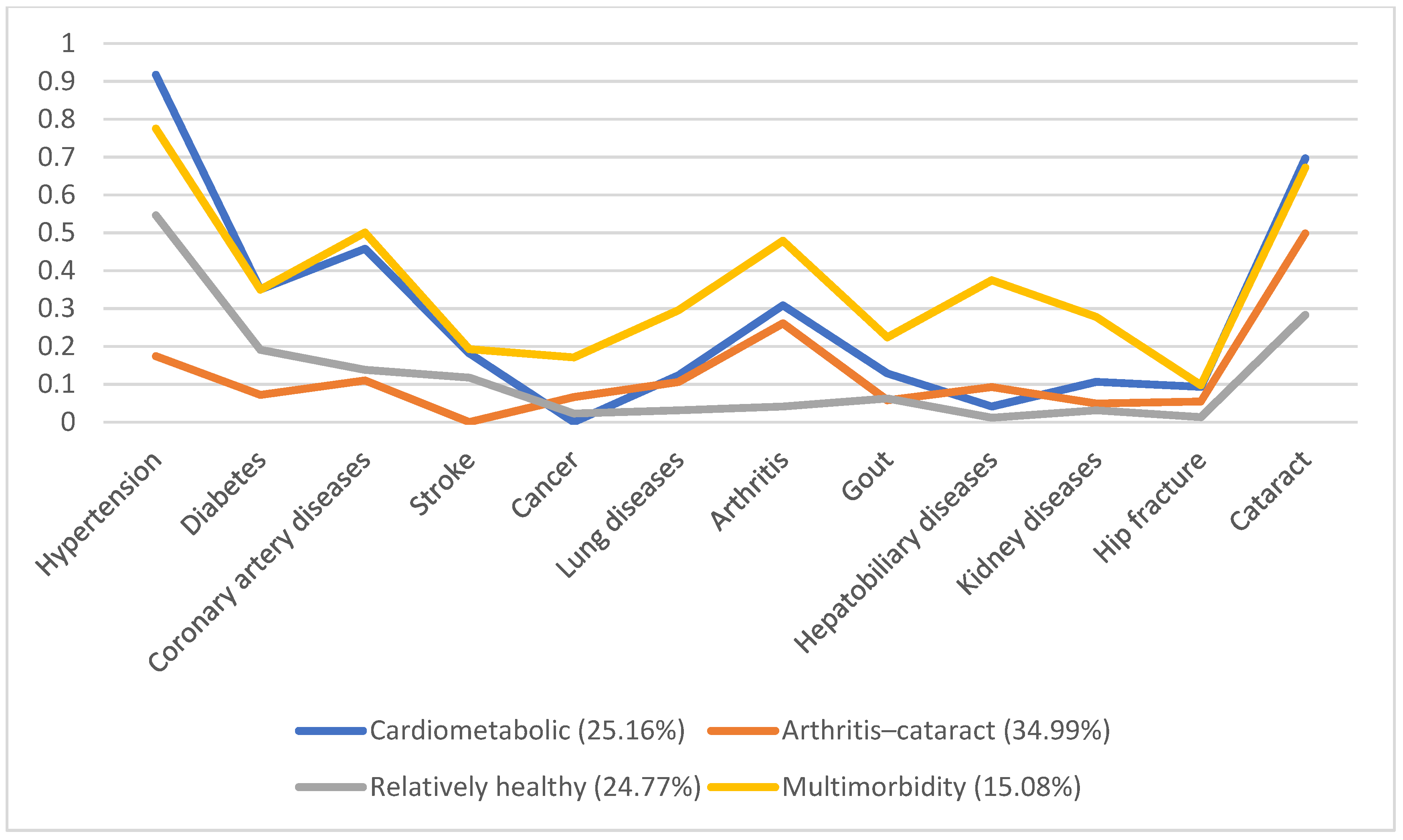
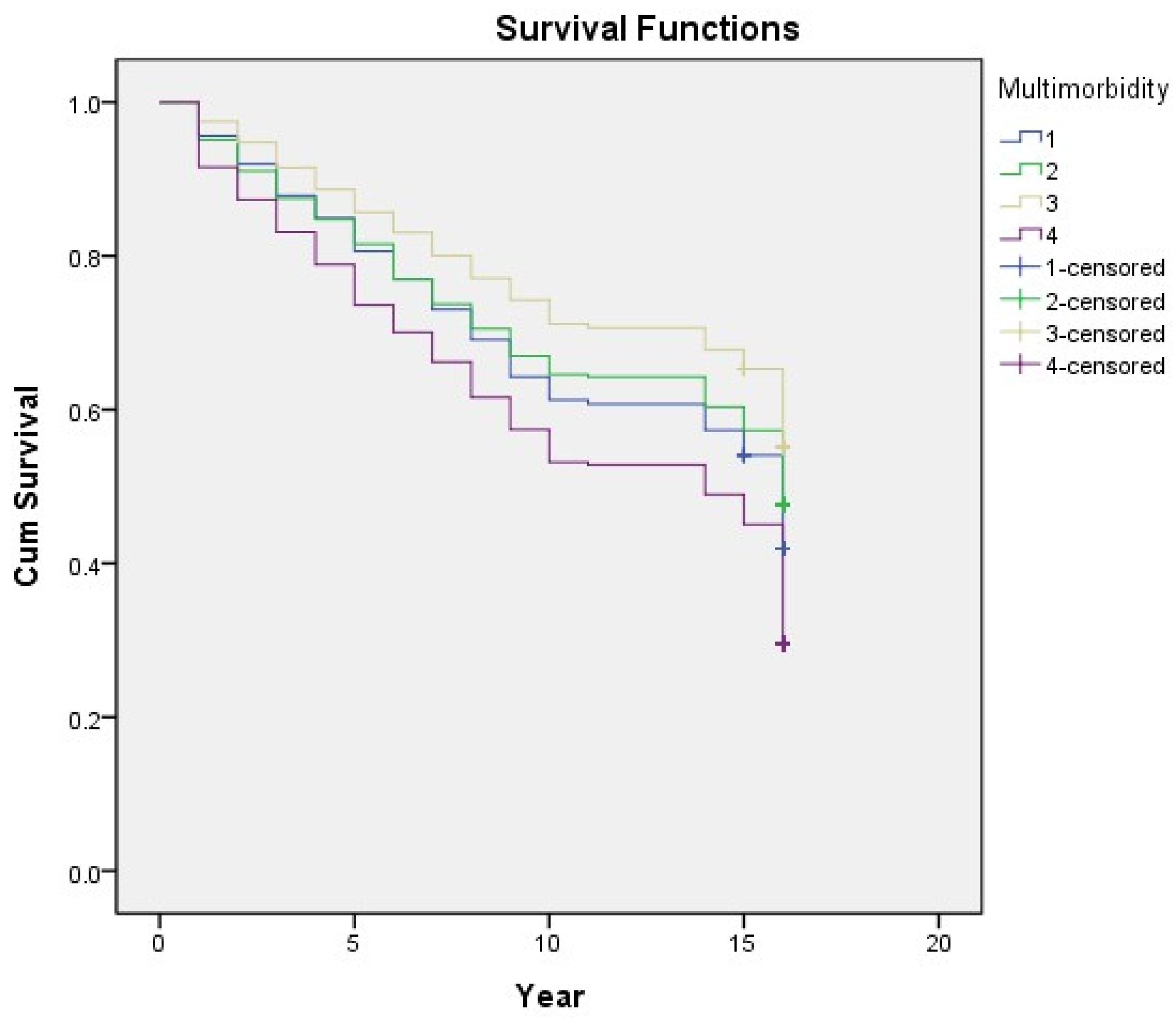
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Development Council, Taiwan. Population projections for the ROC (Taiwan): 2018–2065; National Development Council: Taipei, Taiwan, 2018.
- Yarnall, A.J.; Sayer, A.A.; Clegg, A.; Rockwood, K.; Parker, S.; Hindle, J.V. New horizons in multimorbidity in older adults. Age Ageing 2017, 46, 882–888. [Google Scholar] [CrossRef] [PubMed]
- Kuzuya, M. Era of geriatric medical challenges: Multimorbidity among older patients. Geriatr. Gerontol. Int. 2019, 19, 699–704. [Google Scholar] [CrossRef] [PubMed]
- Sum, G.; Hone, T.; Atun, R.; Millett, C.; Suhrcke, M.; Mahal, A.; Koh, G.C.-H.; Lee, J.T. Multimorbidity and out-of-pocket expenditure on medicines: A systematic review. BMJ Glob. Health 2018, 3, e000505. [Google Scholar] [CrossRef] [PubMed]
- Makovski, T.T.; Schmitz, S.; Zeegers, M.P.; Stranges, S.; van den Akker, M. Multimorbidity and quality of life: Systematic literature review and meta-analysis. Ageing Res. Rev. 2019, 53, 100903. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, Q.D.; Wu, C.; Odden, M.C.; Kim, D.H. Multimorbidity Patterns, Frailty, and Survival in Community-Dwelling Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2019, 74, 1265–1270. [Google Scholar] [CrossRef]
- King, D.E.; Xiang, J.; Pilkerton, C.S. Multimorbidity Trends in United States Adults, 1988–2014. J. Am. Board Fam. Med. 2018, 31, 503–513. [Google Scholar] [CrossRef]
- Hu, R.H.; Hsiao, F.Y.; Chen, L.J.; Huang, P.T.; Hsu WW, Y. Increasing age- and gender-specific burden and complexity of multimorbidity in Taiwan, 2003–2013: A cross-sectional study based on nationwide claims data. BMJ Open 2019, 9, e028333. [Google Scholar] [CrossRef]
- Poblador-Plou, B.; van den Akker, M.; Vos, R.; Calderón-Larrañaga, A.; Metsemakers, J.; Prados-Torres, A. Similar multimorbidity patterns in primary care patients from two European regions: Results of a factor analysis. PLoS ONE 2014, 9, e100375. [Google Scholar] [CrossRef][Green Version]
- Goodman, R.A.; Ling, S.M.; Briss, P.A.; Parrish, R.G.; Salive, M.E.; Finke, B.S. Multimorbidity Patterns in the United States: Implications for Research and Clinical Practice. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 215–220. [Google Scholar] [CrossRef]
- Weller, B.E.; Bowen, N.K.; Faubert, S.J. Latent class analysis: A guide to best practice. J. Black Psychol. 2020, 46, 287–311. [Google Scholar] [CrossRef]
- Zheng, D.D.; Loewenstein, D.A.; Christ, S.L.; Feaster, D.J.; Lam, B.L.; McCollister, K.E.; Curiel-Cid, R.E.; Lee, D.J. Multimorbidity patterns and their relationship to mortality in the US older adult population. PLoS ONE 2021, 16, e0245053. [Google Scholar] [CrossRef] [PubMed]
- Park, B.; Lee, H.A.; Park, H. Use of latent class analysis to identify multimorbidity patterns and associated factors in Korean adults aged 50 years and older. PLoS ONE 2019, 14, e0216259. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; O’Brien, N.; Forrest, J.I.; Salters, K.A.; Patterson, T.L.; Montaner, J.S.G.; Hogg, R.S.; Lima, V.D. Validating a shortened depression scale (10 item CES-D) among HIV-positive people in British Columbia, Canada. PLoS ONE 2012, 7, e40793. [Google Scholar] [CrossRef]
- Nguyen, H.; Wu, Y.T.; Dregan, A.; Vitoratou, S.; Chua, K.C.; Prina, A.M. Multimorbidity patterns, all-cause mortality and healthy aging in older English adults: Results from the English Longitudinal Study of Aging. Geriatr. Gerontol. Int. 2020, 20, 1126–1132. [Google Scholar] [CrossRef] [PubMed]
- Olaya, B.; Moneta, M.V.; Caballero, F.F.; Tyrovolas, S.; Bayes, I.; Ayuso-Mateos, J.L.; Haro, J.M. Latent class analysis of multimorbidity patterns and associated outcomes in Spanish older adults: A prospective cohort study. BMC Geriatr. 2017, 17, 186. [Google Scholar] [CrossRef]
- Castro, J.P.; El-Atat, F.A.; McFarlane, S.I.; Aneja, A.; Sowers, J.R. Cardiometabolic syndrome: Pathophysiology and treatment. Curr. Hypertens. Rep. 2003, 5, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Sattar, N.; Gill, J.M.R.; Alazawi, W. Improving prevention strategies for cardiometabolic disease. Nat. Med. 2020, 26, 320–325. [Google Scholar] [CrossRef]
- Padwal, R.S.; So, H.; Wood, P.W.; McAlister, F.A.; Siddiqui, M.; Norris, C.M.; Jeerakathil, T.; Stone, J.; Valaire, S.; Mann, B.; et al. Cost-effectiveness of home blood pressure telemonitoring and case management in the secondary prevention of cerebrovascular disease in Canada. J. Clin. Hypertens. 2019, 21, 159–168. [Google Scholar] [CrossRef]
- Kirchberger, I.; Hunger, M.; Stollenwerk, B.; Seidl, H.; Burkhardt, K.; Kuch, B.; Meisinger, C.; Holle, R. Effects of a 3-year nurse-based case management in aged patients with acute myocardial infarction on rehospitalisation, mortality, risk factors, physical functioning and mental health. a secondary analysis of the randomized controlled KORINNA study. PLoS ONE 2015, 10, e0116693. [Google Scholar] [CrossRef]
- Jin, W.; Yao, Q.; Liu, Z.; Cao, W.; Zhang, Y.; Che, Z.; Peng, H. Do eye diseases increase the risk of arthritis in the elderly population? Aging (Albany N. Y.) 2021, 13, 15580–15594. [Google Scholar] [CrossRef]
- Angeles-Han, S.; Yeh, S. Prevention and management of cataracts in children with juvenile idiopathic arthritis-associated uveitis. Curr. Rheumatol. Rep. 2012, 14, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Lima, F.B.; Abalem, M.F.; Ruiz, D.G.; Gomes BD, A.; de Azevedo, M.N.; Moraes, H.V., Jr.; Yeskel, A.S.; Kara-Junior, N. Prevalence of eye disease in Brazilian patients with psoriatic arthritis. Clinics 2012, 67, 249–253. [Google Scholar] [CrossRef]
- Wang, H.; Tao, Y. Relationship between the higher inflammatory cytokines level in the aqueous humor of Fuchs uveitis syndrome and the presence of cataract. BMC Ophthalmol. 2021, 21, 108. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.J.; Lundy, D.C. Ocular manifestations of autoimmune disease. Am. Fam. Phys. 2002, 66, 991–998. [Google Scholar]
- Hutnik, C.M.; Nichols, B.D. Cataracts in systemic diseases and syndromes. Curr. Opin. Ophthalmol. 1998, 9, 14–19. [Google Scholar] [CrossRef]
- Glover, K.; Mishra, D.; Singh, T.R.R. Epidemiology of Ocular Manifestations in Autoimmune Disease. Front. Immunol. 2021, 12, 744396. [Google Scholar] [CrossRef]
- Black, R.J.; Hill, C.L.; Lester, S.; Dixon, W. The Association between Systemic Glucocorticoid Use and the Risk of Cataract and Glaucoma in Patients with Rheumatoid Arthritis: A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0166468. [Google Scholar]
- Thorne, J.E.; Woreta, F.A.; Dunn, J.P.; Jabs, D.A. Risk of Cataract Development among Children with Juvenile Idiopathic Arthritis-Related Uveitis Treated with Topical Corticosteroids. Ophthalmology 2020, 127, S21–S26. [Google Scholar] [CrossRef]
- Mikuls, T.; Saag, K.; Criswell, L.; Merlino, L.; Cerhan, J.R. Health related quality of life in women with elderly onset rheumatoid arthritis. J. Rheumatol. 2003, 30, 952–957. [Google Scholar]
- Park, J.H.; Kim, D.J.; Kim, S.J. Is arthritis associated with suicidal ideation and quality of life? Psychol. Health Med. 2019, 24, 144–154. [Google Scholar] [CrossRef]
- Lee, Y.; Lee, S.-H.; Lim, S.M.; Baek, S.H.; Ha, I.-H. Mental health and quality of life of patients with osteoarthritis pain: The sixth Korea National Health and Nutrition Examination Survey (2013–2015). PLoS ONE 2020, 15, e0242077. [Google Scholar]
- Polack, S.; Kuper, H.; Mathenge, W.; Fletcher, A.; Foster, A. Cataract visual impairment and quality of life in a Kenyan population. Br. J. Ophthalmol. 2007, 91, 927–932. [Google Scholar] [CrossRef] [PubMed]
- Harutyunyan, T.; Giloyan, A.; Petrosyan, V. Factors associated with vision-related quality of life among the adult population living in Nagorno Karabagh. Public Health 2017, 153, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Xi, B.; Veeranki, S.P.; Zhao, M.; Ma, C.; Yan, Y.; Mi, J. Relationship of Alcohol Consumption to All-Cause, Cardiovascular, and Cancer-Related Mortality in U.S. Adults. J. Am. Coll. Cardiol. 2017, 70, 913–922. [Google Scholar] [CrossRef]
- Stockwell, T.; Zhao, J.; Panwar, S.; Roemer, A.; Naimi, T.; Chikritzhs, T. Do “Moderate” Drinkers Have Reduced Mortality Risk? A Systematic Review and Meta-Analysis of Alcohol Consumption and All-Cause Mortality. J. Stud. Alcohol Drugs 2016, 77, 185–198. [Google Scholar] [CrossRef]
- Keyes, K.M.; Calvo, E.; Ornstein, K.A.; Rutherford, C.; Fox, M.P.; Staudinger, U.M.; Fried, L.P. Alcohol Consumption in Later Life and Mortality in the United States: Results from 9 Waves of the Health and Retirement Study. Alcohol. Clin. Exp. Res 2019, 43, 1734–1746. [Google Scholar] [CrossRef]
| Multimorbidity Patterns | |||||||
|---|---|---|---|---|---|---|---|
| Characteristics | Total | Cardiometabolic | Arthritis–Cataract | Relatively Healthy | Multimorbidity | p Value | |
| n = 5130 | n = 1111 | n = 594 | n = 3138 | n = 287 | |||
| Age | 66.7 (9.37) | 68.12 (8.84) | 68.9 (8.76) | 65.51 (9.58) | 69.73 (7.9) | <0.0001 | |
| Sex | <0.0001 | ||||||
| Male | 2760 (53.8%) | 577 (51.94%) | 258 (43.43%) | 1794 (57.17%) | 131 (45.64%) | ||
| Female | 2370 (46.2%) | 534 (48.06%) | 336 (56.57%) | 1344 (42.83%) | 156 (54.36%) | ||
| Income satisfaction | <0.0001 | ||||||
| Poor | 829 (17.79%) | 166 (16.73%) | 106 (18.76%) | 478 (16.35%) | 79 (30.38%) | ||
| Fair | 2126 (44.3%) | 432 (43.55%) | 271 (47.96%) | 1310 (44.82%) | 93 (35.77%) | ||
| Good | 1805 (38.08%) | 394 (39.72%) | 188 (33.27%) | 1135 (38.83%) | 88 (33.85%) | ||
| Social participation | <0.0001 | ||||||
| Yes | 2146 (41.83%) | 509 (45.81%) | 259 (43.6%) | 1234 (39.32%) | 144 (50.17%) | ||
| No | 2984 (58.17%) | 602 (54.19%) | 335 (56.4%) | 1904 (60.68%) | 143 (49.83%) | ||
| Self-rated health | <0.0001 | ||||||
| Poor | 1401 (29.40%) | 359 (35.83%) | 261 (46.03%) | 594 (20.24%) | 187 (71.37%) | ||
| Fair | 1613 (33.84%) | 341 (34.03%) | 205 (36.16%) | 1008 (30.34%) | 59 (22.52%) | ||
| Good | 1752 (36.76%) | 302 (30.14%) | 101 (17.81%) | 1333 (45.42%) | 16 (6.11%) | ||
| Smoking | <0.0001 | ||||||
| Yes | 1380 (26.9%) | 224 (20.14%) | 123 (20.71%) | 971 (30.94%) | 62 (21.6%) | ||
| No | 3750 (73.1%) | 887 (79.84%) | 471 (79.29%) | 2167 (69.06%) | 225 (78.4%) | ||
| Alcohol | <0.0001 | ||||||
| Yes | 1083 (21.12%) | 195 (17.55%) | 98 (16.5%) | 764 (24.35%) | 26 (9.06%) | ||
| No | 4046 (78.88%) | 916 (82.45%) | 496 (83.5%) | 2373 (75.65%) | 261 (90.94%) | ||
| Betelnut | 0.0212 | ||||||
| Yes | 346 (6.75%) | 65 (5.85%) | 39 (6.57%) | 233 (7.43%) | 9 (3.14%) | ||
| No | 4783 (93.25%) | 1046 (94.15%) | 555 (93.43%) | 2904 (92.57%) | 278 (96.86%) | ||
| Admission in past one year | <0.0001 | ||||||
| Yes | 909 (17.72%) | 262 (23.58%) | 129 (21.72%) | 400 (12.75%) | 118 (41.11%) | ||
| No | 4221 (82.28%) | 849 (76.42%) | 465 (78.28%) | 2738 (87.25%) | 169 (58.89%) | ||
| Exercise | 0.0077 | ||||||
| No | 2506 (48.87%) | 488 (43.92%) | 306 (51.52%) | 1556 (49.62%) | 156 (54.36%) | ||
| ≤2 times/week | 275 (5.36%) | 54 (4.86%) | 29 (4.88%) | 174 (5.52%) | 18 (6.27%) | ||
| 3–5 times/week | 395 (7.7%) | 88 (7.92%) | 43 (7.24%) | 242 (7.72%) | 22 (7.67%) | ||
| ≥6 times/week | 1952 (38.07%) | 481 (43.29%) | 216 (36.36%) | 1164 (37.12%) | 91 (31.71%) | ||
| Disability | <0.0001 | ||||||
| Yes | 671 (13.1%) | 200 (18.03%) | 111 (18.69%) | 271 (8.64%) | 89 (31.12%) | ||
| No | 4453 (86.9%) | 909 (81.97%) | 483 (81.31%) | 2864 (91.36%) | 197 (68.88%) | ||
| Depression | <0.0001 | ||||||
| Yes | 1062 (22.42%) | 228 (22.85%) | 198 (35.17%) | 508 (17.42%) | 128 (49.61%) | ||
| No | 3674 (77.58%) | 770 (77.15%) | 365 (64.83%) | 2409 (82.58%) | 130 (50.39%) | ||
| Mortality | ||||
|---|---|---|---|---|
| OR | 95% CI | p Value | ||
| Age | 1.141 * | 1.132–1.150 | <0.0001 | |
| Sex | ||||
| Male | 1.551 * | 1.389–1.732 | <0.0001 | |
| Female | Ref | |||
| Income satisfaction | ||||
| Poor | 1.200 * | 1.018–1.415 | 0.0299 | |
| Fair | 0.986 | 0.869–1.119 | 0.8271 | |
| Good | Ref | |||
| Social participation | ||||
| Yes | Ref | |||
| No | 1.716 * | 1.534–1.919 | <0.0001 | |
| Self-rated health | ||||
| Poor | 2.533 * | 2.193–2.926 | <0.0001 | |
| Fair | 1.356 * | 1.182–1.556 | <0.0001 | |
| Good | Ref | |||
| Smoking | ||||
| Yes | 1.44 * | 1.272–1.630 | <0.0001 | |
| No | Ref | |||
| Drinking | ||||
| Yes | 0.739 | 0.646–0.846 | <0.0001 | |
| No | Ref | |||
| Betelnut | ||||
| Yes | 0.891 | 0.716–1.109 | 0.3013 | |
| No | Ref | |||
| Admission | ||||
| Yes | 2.719 * | 2.333–3.169 | <0.0001 | |
| No | Ref | |||
| Exercise habits | ||||
| No | 1.329 * | 1.073–1.646 | 0.0092 | |
| ≤2 times/week | 0.809 | 0.591–1.181 | 0.1865 | |
| 3–5 times/week | Ref | |||
| ≥6 times/week | 1.336 * | 1.074–1.661 | 0.0092 | |
| Disability | ||||
| Yes | 5.669 * | 4.618–6.958 | <0.0001 | |
| No | Ref | |||
| Depression | ||||
| Yes | 2.203 * | 1.760–2.325 | <0.0001 | |
| No | Ref | |||
| Model 1 | Model 2 | Model 3 | Model 4 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | OR | 95% CI | p Value | OR | 95% CI | p Value | ||
| Disease patterns | |||||||||||||
| Cardio-metabolic | 1.703 * | 1.484–1.956 | <0.0001 | 1.354 * | 1.147–1.599 | 0.0003 | 1.424 * | 1.203–1.684 | <0.0001 | 1.237 * | 1.040–1.472 | 0.0162 | |
| Arthritis–cataract | 1.379 * | 1.157–1.644 | <0.0001 | 1.023 | 0.831–1.260 | 0.8292 | 1.04 | 0.844–1.282 | 0.7145 | 0.831 | 0.667–1.034 | 0.0968 | |
| Relatively healthy | Ref | Ref | Ref | Ref | |||||||||
| Multimorbidity | 2.924 * | 2.251–3.797 | <0.0001 | 2.028 * | 1.504–2.736 | <0.0001 | 2.008 * | 1.486–2.713 | <0.0001 | 1.353 | 0.982–1.863 | 0.0646 | |
| Age | 1.136 * | 1.126–1.146 | <0.0001 | 1.14 * | 1.129–1.150 | <0.0001 | 1.133 * | 1.122–1.143 | <0.0001 | ||||
| Sex | <0.0001 | <0.0001 | <0.0001 | ||||||||||
| Male | 1.907 * | 1.659–2.192 | 1.689 * | 1.437–1.985 | 1.718 * | 1.454–2.028 | |||||||
| Female | Ref | Ref | Ref | ||||||||||
| Income satisfaction | |||||||||||||
| Poor | 1.54 * | 1.269–1.870 | <0.0001 | 1.434 * | 1.177–1.747 | 0.0003 | 1.115 | 0.901–1380 | 0.3163 | ||||
| Fair | 1.137 | 0.981–1.316 | 0.0878 | 1.085 | 0.935–1.259 | 0.2826 | 1.013 | 0.869–1.181 | 0.8704 | ||||
| Good | Ref | Ref | Ref | ||||||||||
| Social participation | 0.0023 | 0.0058 | 0.1369 | ||||||||||
| Yes | Ref | Ref | Ref | ||||||||||
| No | 1.247 * | 1.082–1.437 | 1.224 * | 1.060–1.413 | 1.119 | 0.965–1.297 | |||||||
| Smoking | <0.0001 | <0.0001 | |||||||||||
| Yes | 1.708 * | 1.432–2.037 | 1.756 * | 1.468–2.1 | |||||||||
| No | Ref | Ref | |||||||||||
| Drinking | 0.0003 | 0.0197 | |||||||||||
| Yes | 0.724 * | 0.606–0.864 | 0.807 * | 0.673–0.966 | |||||||||
| No | Ref | Ref | |||||||||||
| Exercise habits | |||||||||||||
| No | 1.222 | 0.945–1.582 | 0.1267 | 1.172 | 0.901–1.525 | 0.2358 | |||||||
| ≤2 times/week | 0.888 | 0.605–1.302 | 0.5416 | 0.872 | 0.591–1.287 | 0.4903 | |||||||
| 3–5 times/week | Ref | Ref | |||||||||||
| ≥6 times/week | 0.97 | 0.748–1.259 | 0.8193 | 1.06 | 0.814–1.382 | 0.6649 | |||||||
| Self-rated health | |||||||||||||
| Poor | 1.587 * | 1.301–1.935 | <0.0001 | ||||||||||
| Fair | 1.119 | 0.947–1.323 | 0.1853 | ||||||||||
| Good | Ref | ||||||||||||
| Admission | <0.0001 | ||||||||||||
| Yes | 1.84 * | 1.516–2.232 | |||||||||||
| No | Ref | ||||||||||||
| Disability | <0.0001 | ||||||||||||
| Yes | 1.799 * | 1.390–2.2328 | |||||||||||
| No | Ref | ||||||||||||
| Depression | 0.0178 | ||||||||||||
| Yes | 1.249 * | 1.039–1.501 | |||||||||||
| No | No | ||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ho, H.-E.; Yeh, C.-J.; Wei, J.C.-C.; Chu, W.-M.; Lee, M.-C. Trends of Multimorbidity Patterns over 16 Years in Older Taiwanese People and Their Relationship to Mortality. Int. J. Environ. Res. Public Health 2022, 19, 3317. https://doi.org/10.3390/ijerph19063317
Ho H-E, Yeh C-J, Wei JC-C, Chu W-M, Lee M-C. Trends of Multimorbidity Patterns over 16 Years in Older Taiwanese People and Their Relationship to Mortality. International Journal of Environmental Research and Public Health. 2022; 19(6):3317. https://doi.org/10.3390/ijerph19063317
Chicago/Turabian StyleHo, Hsin-En, Chih-Jung Yeh, James Cheng-Chung Wei, Wei-Min Chu, and Meng-Chih Lee. 2022. "Trends of Multimorbidity Patterns over 16 Years in Older Taiwanese People and Their Relationship to Mortality" International Journal of Environmental Research and Public Health 19, no. 6: 3317. https://doi.org/10.3390/ijerph19063317
APA StyleHo, H.-E., Yeh, C.-J., Wei, J. C.-C., Chu, W.-M., & Lee, M.-C. (2022). Trends of Multimorbidity Patterns over 16 Years in Older Taiwanese People and Their Relationship to Mortality. International Journal of Environmental Research and Public Health, 19(6), 3317. https://doi.org/10.3390/ijerph19063317








