The Role of 3D Printing in Planning Complex Medical Procedures and Training of Medical Professionals—Cross-Sectional Multispecialty Review
Abstract
:1. Introduction
1.1. Three-Dimensional Printing Technique Overview
1.2. Application of 3D Printing in Medicine
2. Discipline Specific Applications
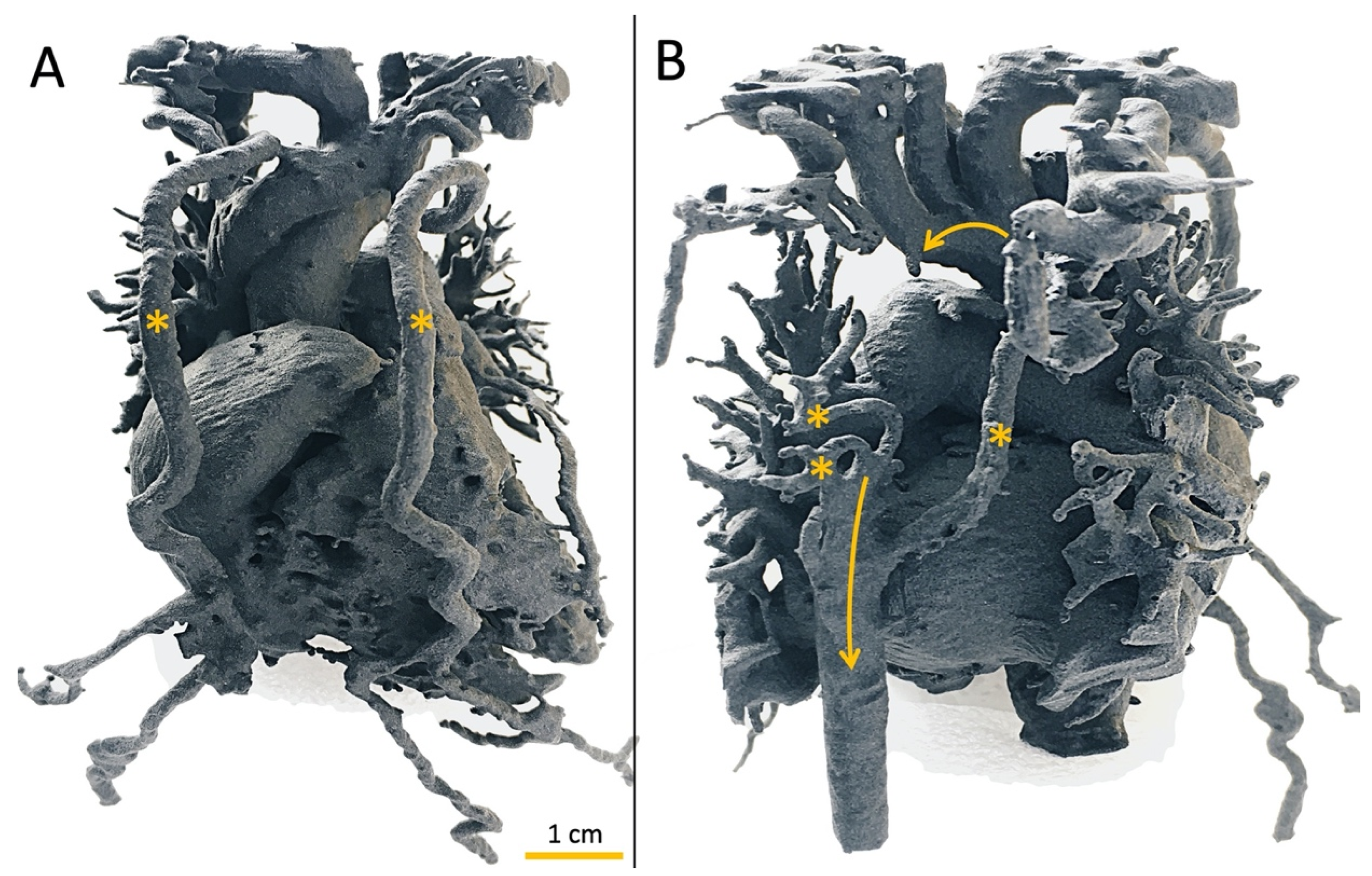
2.1. Pediatric Cardiac Surgery
2.2. Pediatric Interventional Cardiology
2.3. Cardiac Structural Interventions
2.4. Pediatric Surgery
2.5. General Surgery
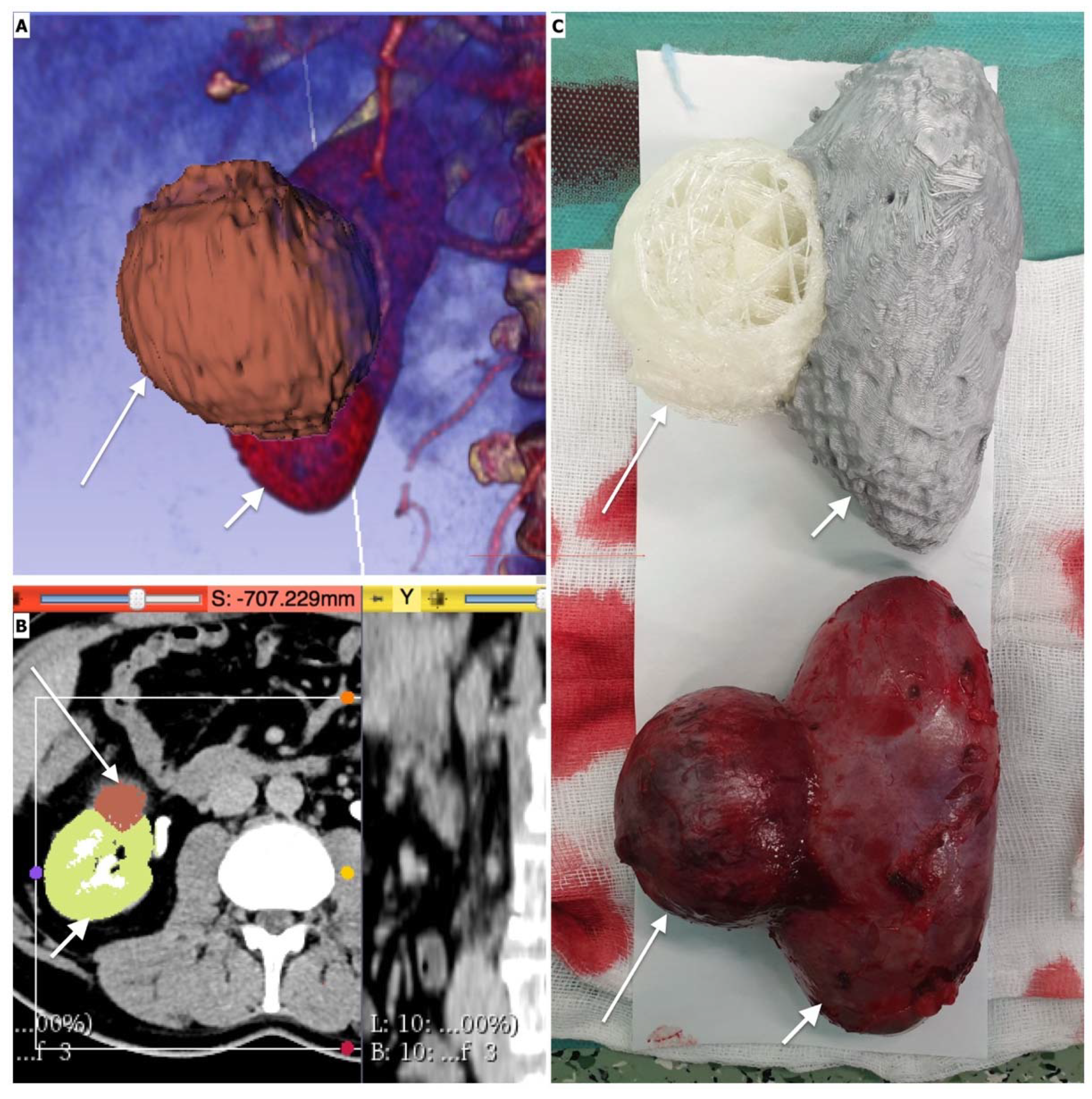
2.6. Orthopedic Surgery
2.7. Otorhinolaryngology (Ear, Nose and Throat Surgery)
2.8. Head and Neck Surgery
2.9. Neurosurgery
2.10. Gynecology and Obstetrics
2.11. Urology
2.12. Emergency Medicine and Anesthesiology
2.13. Radiotherapy
3. Discussion
3.1. Investment and Operational Costs
3.2. Print Fidelity
3.3. Radiation Exposure
3.4. Mimicking Tissues’ Mechanical Properties
3.5. Bioprinting
3.6. Drug Delivery
3.7. Ethical and Legal Considerations
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Antreas, K.; Piromalis, D. Employing a Low-Cost Desktop 3D Printer: Challenges, and How to Overcome Them by Tuning Key Process Parameters. Int. J. Mech. Appl. 2021, 10, 11–19. [Google Scholar] [CrossRef]
- Luo, H.; Meyer-Szary, J.; Wang, Z.; Sabiniewicz, R.; Liu, Y. Three-Dimensional Printing in Cardiology: Current Applications and Future Challenges. Cardiol. J. 2017, 24, 436–444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garg, R.; Zahn, E.M. Utility of Three-Dimensional (3D) Modeling for Planning Structural Heart Interventions (with an Emphasis on Valvular Heart Disease). Curr. Cardiol. Rep. 2020, 22, 125. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Szary, J.; Woźniak-Mielczarek, L.; Sabiniewicz, D.; Sabiniewicz, R. Feasibility of In-House Rapid Prototyping of Cardiovascular Three-Dimensional Models for Planning and Training Non-Standard Interventional Procedures. Cardiol. J. 2020, 26, 790–792. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scanlan, A.B.; Nguyen, A.V.; Ilina, A.; Lasso, A.; Cripe, L.; Jegatheeswaran, A.; Silvestro, E.; McGowan, F.X.; Mascio, C.E.; Fuller, S.; et al. Comparison of 3D Echocardiogram-Derived 3D Printed Valve Models to Molded Models for Simulated Repair of Pediatric Atrioventricular Valves. Pediatr. Cardiol. 2018, 39, 538–547. [Google Scholar] [CrossRef] [PubMed]
- Valverde, I.; Gomez-Ciriza, G.; Hussain, T.; Suarez-Mejias, C.; Velasco-Forte, M.N.; Byrne, N.; Ordoñez, A.; Gonzalez-Calle, A.; Anderson, D.; Hazekamp, M.G.; et al. Three-Dimensional Printed Models for Surgical Planning of Complex Congenital Heart Defects: An International Multicentre Study. Eur. J. Cardiothorac. Surg. 2017, 52, 1139–1148. [Google Scholar] [CrossRef] [PubMed]
- Deng, X.; He, S.; Huang, P.; Luo, J.; Yang, G.; Zhou, B.; Xiao, Y. A Three-Dimensional Printed Model in Preoperative Consent for Ventricular Septal Defect Repair. J. Cardiothorac. Surg. 2021, 16, 229. [Google Scholar] [CrossRef] [PubMed]
- Costello, J.P.; Olivieri, L.J.; Su, L.; Krieger, A.; Alfares, F.; Thabit, O.; Marshall, M.B.; Yoo, S.J.; Kim, P.C.; Jonas, R.A.; et al. Incorporating Three-Dimensional Printing into a Simulation-Based Congenital Heart Disease and Critical Care Training Curriculum for Resident Physicians. Congenit. Heart Dis. 2015, 10, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, N.; Ramamurthy, H.R.; Kumar, V.; Kumar, A.; Dhanalakshmi, B.; Kumar, G. The Role of Three-Dimensional Printed Cardiac Models in the Management of Complex Congenital Heart Diseases. Med. J. Armed Forces India 2021, 77, 322–330. [Google Scholar] [CrossRef]
- Valverde, I.; Gomez, G.; Coserria, J.F.; Suarez-Mejias, C.; Uribe, S.; Sotelo, J.; Velasco, M.N.; Santos De Soto, J.; Hosseinpour, A.R.; Gomez-Cia, T. 3D Printed Models for Planning Endovascular Stenting in Transverse Aortic Arch Hypoplasia. Catheter. Cardiovasc. Interv. 2015, 85, 1006–1012. [Google Scholar] [CrossRef]
- Phillips, A.B.M.; Nevin, P.; Shah, A.; Olshove, V.; Garg, R.; Zahn, E.M. Development of a Novel Hybrid Strategy for Transcatheter Pulmonary Valve Placement in Patients Following Transannular Patch Repair of Tetralogy of Fallot. Catheter. Cardiovasc. Interv. 2016, 87, 403–410. [Google Scholar] [CrossRef] [PubMed]
- Jalal, Z.; Seguela, P.-E.; Iriart, X.; Roubertie, F.; Quessard, A.; Kreitmann, B.; Thambo, J.-B. Hybrid Melody Valve Implantation in Mitral Position in a Child: Usefulness of a 3-Dimensional Printed Model for Preprocedural Planning. Can. J. Cardiol. 2018, 34, 812.e5–812.e7. [Google Scholar] [CrossRef] [PubMed]
- Bhatla, P.; Tretter, J.T.; Chikkabyrappa, S.; Chakravarti, S.; Mosca, R.S. Surgical Planning for a Complex Double-Outlet Right Ventricle Using 3D Printing. Echocardiography 2017, 34, 802–804. [Google Scholar] [CrossRef] [PubMed]
- Sabiniewicz, R.; Meyer-Szary, J.; Potaż, P.; Jagielak, D.; Moszura, T. Melody Valve Implantation Pre-Procedural Planning Using Custom-Made 3D Printed Model of the Region of Interest. Adv. Interv. Cardiol. 2018, 14, 210–211. [Google Scholar] [CrossRef] [PubMed]
- Biernacka, E.K.; Rużyłło, W.; Demkow, M. Percutaneous Pulmonary Valve Implantation–State of the Art and Polish Experience. Adv. Interv. Cardiol. 2017, 1, 3–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schievano, S.; Migliavacca, F.; Coats, L.; Khambadkone, S.; Carminati, M.; Wilson, N.; Deanfield, J.E.; Bonhoeffer, P.; Taylor, A.M. Percutaneous Pulmonary Valve Implantation Based on Rapid Prototyping of Right Ventricular Outflow Tract and Pulmonary Trunk from MR Data. Radiology 2007, 242, 490–497. [Google Scholar] [CrossRef] [PubMed]
- Ripley, B.; Kelil, T.; Cheezum, M.K.; Goncalves, A.; Di Carli, M.F.; Rybicki, F.J.; Steigner, M.; Mitsouras, D.; Blankstein, R. 3D Printing Based on Cardiac CT Assists Anatomic Visualization Prior to Transcatheter Aortic Valve Replacement. J. Cardiovasc. Comput. Tomogr. 2016, 10, 28–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zelis, J.M.; Meiburg, R.; Roijen, J.J.D.; Janssens, K.L.P.M.; van ’t Veer, M.; Pijls, N.H.J.; Johnson, N.P.; van de Vosse, F.N.; Tonino, P.A.L.; Rutten, M.C. 3D-Printed Stenotic Aortic Valve Model to Simulate Physiology before, during, and after Transcatheter Aortic Valve Implantation. Int. J. Cardiol. 2020, 313, 32–34. [Google Scholar] [CrossRef] [PubMed]
- Qian, Z.; Wang, K.; Liu, S.; Zhou, X.; Rajagopal, V.; Meduri, C.; Kauten, J.R.; Chang, Y.-H.; Wu, C.; Zhang, C.; et al. Quantitative Prediction of Paravalvular Leak in Transcatheter Aortic Valve Replacement Based on Tissue-Mimicking 3D Printing. JACC Cardiovasc. Imaging 2017, 10, 719–731. [Google Scholar] [CrossRef]
- Levin, D.; Mackensen, G.B.; Reisman, M.; McCabe, J.M.; Dvir, D.; Ripley, B. 3D Printing Applications for Transcatheter Aortic Valve Replacement. Curr. Cardiol. Rep. 2020, 22, 23. [Google Scholar] [CrossRef] [PubMed]
- Little, S.H.; Vukicevic, M.; Avenatti, E.; Ramchandani, M.; Barker, C.M. 3D Printed Modeling for Patient-Specific Mitral Valve Intervention: Repair with a Clip and a Plug. JACC Cardiovasc. Interv. 2016, 9, 973–975. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.D.; Eng, M.; Greenbaum, A.; Myers, E.; Forbes, M.; Pantelic, M.; Song, T.; Nelson, C.; Divine, G.; Taylor, A.; et al. Predicting LVOT Obstruction After TMVR. JACC Cardiovasc. Imaging 2016, 9, 1349–1352. [Google Scholar] [CrossRef] [PubMed]
- Izzo, R.L.; O’Hara, R.P.; Iyer, V.; Hansen, R.; Meess, K.M.; Nagesh, S.V.S.; Rudin, S.; Siddiqui, A.H.; Springer, M.; Ionita, C.N. 3D Printed Cardiac Phantom for Procedural Planning of a Transcatheter Native Mitral Valve Replacement. Proc. SPIE Int. Soc. Opt. Eng. 2016, 9789, 978908. [Google Scholar] [PubMed] [Green Version]
- Holmes, D.R.; Lakkireddy, D.R.; Whitlock, R.P.; Waksman, R.; Mack, M.J. Left Atrial Appendage Occlusion. J. Am. Coll. Cardiol. 2014, 63, 291–298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- January, C.T.; Wann, L.S.; Calkins, H.; Chen, L.Y.; Cigarroa, J.E.; Cleveland, J.C.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; Furie, K.L.; et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients with Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration with the Society of Thoracic Surgeons. Circulation 2019, 140. [Google Scholar] [CrossRef]
- Wang, D.D.; Eng, M.; Kupsky, D.; Myers, E.; Forbes, M.; Rahman, M.; Zaidan, M.; Parikh, S.; Wyman, J.; Pantelic, M.; et al. Application of 3-Dimensional Computed Tomographic Image Guidance to WATCHMAN Implantation and Impact on Early Operator Learning Curve. JACC Cardiovasc. Interv. 2016, 9, 2329–2340. [Google Scholar] [CrossRef] [PubMed]
- Pellegrino, P.L.; Fassini, G.; Di Biase, M.; Tondo, C. Left Atrial Appendage Closure Guided by 3D Printed Cardiac Reconstruction: Emerging Directions and Future Trends: Emerging Directions and Future Trends. J. Cardiovasc. Electrophysiol. 2016, 27, 768–771. [Google Scholar] [CrossRef] [PubMed]
- Otton, J.M.; Spina, R.; Sulas, R.; Subbiah, R.N.; Jacobs, N.; Muller, D.W.M.; Gunalingam, B. Left Atrial Appendage Closure Guided by Personalized 3D-Printed Cardiac Reconstruction. JACC Cardiovasc. Interv. 2015, 8, 1004–1006. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hell, M.; Achenbach, S.; Yoo, I.; Franke, J.; Blachutzik, F.; Roether, J.; Graf, V.; Raaz-Schrauder, D.; Marwan, M.; Schlundt, C. 3D Printing for Sizing Left Atrial Appendage Closure Device: Head-to-Head Comparison with Computed Tomography and Transoesophageal Echocardiography. EuroIntervention 2017, 13, 1234–1241. [Google Scholar] [CrossRef]
- Li, H.; Yao, Q.; Shen, B.; Shu, M.; Zhong, L.; Wang, X.; Song, Z. Application of 3D Printing Technology to Left Atrial Appendage Occlusion. Int. J. Cardiol. 2017, 231, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Sabiniewicz, R.; Meyer-Szary, J.; Woźniak-Mielczarek, L.; Sabiniewicz, D. Follow-up on Results of Three-Dimensional Printed Model Aided Unusual Intervention on Aneurysm of Aortic Arch Lesser Curvature. Cardiol. J. 2020, 27, 447–448. [Google Scholar] [CrossRef] [PubMed]
- Cruz-González, I.; Barreiro-Pérez, M.; Valverde, I. 3D-Printing in Preprocedural Planning of Paravalvular Leak Closure: Feasibility/Proof-of-Concept. Rev. Espanola Cardiol. Engl. Ed. 2019, 72, 342. [Google Scholar] [CrossRef]
- ElGuindy, A.; Osman, A.; Elborae, A.; Nagy, M. The Utility of 3D Printed Models in Complex Percutaneous Paravalvular Leak Interventions. Glob. Cardiol. Sci. Pract. 2020, 2020, e202027. [Google Scholar] [CrossRef] [PubMed]
- Bellia-Munzon, G.; Martinez, J.; Toselli, L.; Nazar Peirano, M.; Sanjurjo, D.; Vallee, M.; Martinez-Ferro, M. From Bench to Bedside: 3D Reconstruction and Printing as a Valuable Tool for the Chest Wall Surgeon. J. Pediatr. Surg. 2020, 55, 2703–2709. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.J.; Lin, K.H.; Chen, Y.Y.; Wu, T.H.; Huang, H.K.; Chang, H.; Lee, S.C.; Chen, J.E.; Huang, T.W. Feasibility and Clinical Effectiveness of Three-Dimensional Printed Model-Assisted Nuss Procedure. Ann. Thorac. Surg. 2019, 107, 1089–1096. [Google Scholar] [CrossRef] [PubMed]
- Deng, X.; Huang, P.; Luo, J.; Wang, J.; Yi, L.; Yang, G.; He, S.; Li, X.; Xiang, S. A Novel Three-Dimensional Printed Vacuum Bell for Pectus Excavatum Treatment: A Preliminary Study. J. Cardiothorac. Surg. 2020, 15, 240. [Google Scholar] [CrossRef] [PubMed]
- Villarreal, J.A.; Yoeli, D.; Masand, P.M.; Galvan, N.T.N.; Olutoye, O.O.; Goss, J.A. Hepatic Separation of Conjoined Twins: Operative Technique and Review of Three-Dimensional Model Utilization. J. Pediatr. Surg. 2020, 55, 2828–2835. [Google Scholar] [CrossRef] [PubMed]
- Prayer, F.; Metzelder, M.; Krois, W.; Brugger, P.C.; Gruber, G.M.; Weber, M.; Scharrer, A.; Rokitansky, A.; Langs, G.; Prayer, D.; et al. Three-Dimensional Reconstruction of Defects in Congenital Diaphragmatic Hernia: A Fetal MRI Study. Ultrasound Obstet. Gynecol. 2019, 53, 816–826. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Sánchez, Á.; Girón-Vallejo, Ó.; Ruiz-Pruneda, R.; Fernandez-Ibieta, M.; García-Calderon, D.; Villamil, V.; Giménez-Aleixandre, M.; Montoya-Rangel, C.; Hernández Bermejo, J. Three-Dimensional Printed Model and Virtual Reconstruction: An Extra Tool for Pediatric Solid Tumors Surgery. Eur. J. Pediatr. Surg. Rep. 2018, 06, e70–e76. [Google Scholar] [CrossRef] [Green Version]
- Beltrami, G.; Ristori, G.; Nucci, A.M.; Galeotti, A.; Tamburini, A.; Scoccianti, G.; Campanacci, D.; Innocenti, M.; Capanna, R. Custom-Made 3d-Printed Implants as Novel Approach to Reconstructive Surgery after Oncologic Resection in Pediatric Patients. J. Clin. Med. 2021, 10, 1056. [Google Scholar] [CrossRef]
- Vanesa, V.; Irene, M.P.; Marta, A.S.; Francisco José, P.F.; Miguel, B.S.; Mireia, R.M.; Josep, R.P. Accuracy of Virtually Planned Mandibular Distraction in a Pediatric Case Series. J. Cranio-Maxillofac. Surg. 2021, 49, 154–165. [Google Scholar] [CrossRef]
- Morrison, R.J.; Hollister, S.J.; Niedner, M.F.; Mahani, M.G.; Park, A.H.; Mehta, D.K.; Ohye, R.G.; Green, G.E. Erratum: Mitigation of Tracheobronchomalacia with 3D-Printed Personalized Medical Devices in Pediatric Patients (Science Translational Medicine (2015) 7 (287er4)). Sci. Transl. Med. 2015, 7, 287er4. [Google Scholar] [CrossRef] [Green Version]
- Pietrabissa, A.; Marconi, S.; Negrello, E.; Mauri, V.; Peri, A.; Pugliese, L.; Marone, E.M.; Auricchio, F. An Overview on 3D Printing for Abdominal Surgery. Surg. Endosc. 2020, 34, 1–13. [Google Scholar] [CrossRef]
- Chandak, P.; Byrne, N.; Coleman, A.; Karunanithy, N.; Carmichael, J.; Marks, S.D.; Stojanovic, J.; Kessaris, N.; Mamode, N. Patient-Specific 3D Printing: A Novel Technique for Complex Pediatric Renal Transplantation. Ann. Surg. 2019, 269, e18–e23. [Google Scholar] [CrossRef]
- Chandak, P.; Byrne, N.; Newton, V.; Coleman, A.; Stojanovic, J.; Marks, S.D.; Kessaris, N.; Mamode, N. Classification of Abdominal Vascular Anomalies and Use of 3D Printing to Support Complex Renal Transplantation in Children. Lancet 2017, 389, S32. [Google Scholar] [CrossRef]
- Marconi, S.; Pugliese, L.; Botti, M.; Peri, A.; Cavazzi, E.; Latteri, S.; Auricchio, F.; Pietrabissa, A. Value of 3D Printing for the Comprehension of Surgical Anatomy. Surg. Endosc. 2017, 31, 4102–4110. [Google Scholar] [CrossRef]
- Tang, R.; Ma, L.; Li, A.; Yu, L.; Rong, Z.; Zhang, X.; Xiang, C.; Liao, H.; Dong, J. Choledochoscopic Examination of a 3-Dimensional Printing Model Using Augmented Reality Techniques: A Preliminary Proof of Concept Study. Surg. Innov. 2018, 25, 492–498. [Google Scholar] [CrossRef]
- Atalay, H.A.; Ülker, V.; Alkan, İ.; Canat, H.L.; Özkuvancı, Ü.; Altunrende, F. Impact of Three-Dimensional Printed Pelvicaliceal System Models on Residents’ Understanding of Pelvicaliceal System Anatomy Before Percutaneous Nephrolithotripsy Surgery: A Pilot Study. J. Endourol. 2016, 30, 1132–1137. [Google Scholar] [CrossRef]
- Shibata, E.; Takao, H.; Amemiya, S.; Ohtomo, K. 3D-Printed Visceral Aneurysm Models Based on CT Data for Simulations of Endovascular Embolization: Evaluation of Size and Shape Accuracy. Am. J. Roentgenol. 2017, 209, 243–247. [Google Scholar] [CrossRef]
- Yang, Y.Y.; Huang, H.G. [Development status of three-dimensional printing technology in pancreatic surgery]. Zhonghua Wai Ke Za Zhi 2017, 55, 795–797. (In Chinese) [Google Scholar] [CrossRef]
- Marconi, S.; Pugliese, L.; Del Chiaro, M.; Pozzi Mucelli, R.; Auricchio, F.; Pietrabissa, A. An Innovative Strategy for the Identification and 3D Reconstruction of Pancreatic Cancer from CT Images. Updat. Surg. 2016, 68, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Fang, C.-H. Application of 3D Printing Technique in the Diagnosis and Treatment for Pancreatic and Periampullary Neoplasms. Hpb 2016, 18, e357. [Google Scholar] [CrossRef] [Green Version]
- Bauermeister, A.J.; Zuriarrain, A.; Newman, M.I. Three-Dimensional Printing in Plastic and Reconstructive Surgery a Systematic Review. Ann. Plast. Surg. 2016, 77, 569–576. [Google Scholar] [CrossRef] [PubMed]
- Richard, Z.; Jackson, E.; Jung, J.P.; Kanotra, S.P. Feasibility and Potential of Three-Dimensional Printing in Laryngotracheal Stenosis. J. Laryngol. Otol. 2019, 133, 530–534. [Google Scholar] [CrossRef] [PubMed]
- Erdogan, M.M.; Simsek, T.; Ugur, L.; Kazaz, H.; Seyhan, S.; Gok, U. The Effect of 3D-Printed Custom External Nasal Splint on Edema and Ecchymosis After Rhinoplasty. J. Oral Maxillofac. Surg. 2021, 79, 1549.e1–1549.e7. [Google Scholar] [CrossRef] [PubMed]
- Zhu, P.; Chen, S. Clinical Outcomes Following Ear Reconstruction with Adjuvant 3D Template Model. Acta Otolaryngol. 2016, 136, 1236–1241. [Google Scholar] [CrossRef] [PubMed]
- Zein, N.N.; Hanouneh, I.A.; Bishop, P.D.; Samaan, M.; Eghtesad, B.; Quintini, C.; Miller, C.; Yerian, L.; Klatte, R. Three-Dimensional Print of a Liver for Preoperative Planning in Living Donor Liver Transplantation. Liver Transplant. Off. Publ. Am. Assoc. Study Liver Dis. Int. Liver Transplant. Soc. 2013, 19, 1304–1310. [Google Scholar] [CrossRef]
- Burdall, O.C.; Makin, E.; Davenport, M.; Ade-Ajayi, N. 3D Printing to Simulate Laparoscopic Choledochal Surgery. J. Pediatr. Surg. 2016, 51, 828–831. [Google Scholar] [CrossRef] [Green Version]
- Witowski, J.S.; Pędziwiatr, M.; Major, P.; Budzyński, A. Cost-Effective, Personalized, 3D-Printed Liver Model for Preoperative Planning before Laparoscopic Liver Hemihepatectomy for Colorectal Cancer Metastases. Int. J. Comput. Assist. Radiol. Surg. 2017, 12, 2047–2054. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pietrabissa, A.; Marconi, S.; Peri, A.; Pugliese, L.; Cavazzi, E.; Vinci, A.; Botti, M.; Auricchio, F. From CT Scanning to 3-D Printing Technology for the Preoperative Planning in Laparoscopic Splenectomy. Surg. Endosc. 2016, 30, 366–371. [Google Scholar] [CrossRef]
- Huang, J.-H.; Liao, H.; Tan, X.-Y.; Xing, W.-R.; Zhou, Q.; Zheng, Y.-S.; Cao, H.-Y.; Zeng, C.-J. Surgical Treatment for Both-Column Acetabular Fractures Using Pre-Operative Virtual Simulation and Three-Dimensional Printing Techniques. Chin. Med. J. Engl. 2020, 133, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Kong, L.; Yang, G.; Yu, J.; Zhou, Y.; Li, S.; Zheng, Q.; Zhang, B. Surgical Treatment of Intra-Articular Distal Radius Fractures with the Assistance of Three-Dimensional Printing Technique. Medicine 2020, 99, e19259. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Cai, L.; Zheng, W.; Wang, J.; Guo, X.; Chen, H. The Efficacy of Using 3D Printing Models in the Treatment of Fractures: A Randomised Clinical Trial. BMC Musculoskelet. Disord. 2019, 20, 65. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Yu, T.; Lei, B.; Huang, W.; Huang, R. A New Individualized Three-Dimensional Printed Template for Lateral Ankle Ligament Reconstruction. Med. Sci. Monit. 2020, 26, e922925. [Google Scholar] [CrossRef] [PubMed]
- Park, J.W.; Kang, H.G.; Kim, J.H.; Kim, H.-S. The Application of 3D-Printing Technology in Pelvic Bone Tumor Surgery. J. Orthop. Sci. 2021, 26, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Gu, F.; Li, L.; Zhang, H.; Li, X.; Ling, C.; Wang, L.; Yao, Q. Three-Dimensional-Printed Guiding Template for Unicompartmental Knee Arthroplasty. BioMed Res. Int. 2020, 2020, 7019794. [Google Scholar] [CrossRef] [PubMed]
- Harrysson, O.L.A.; Cansizoglu, O.; Marcellin-Little, D.J.; Cormier, D.R.; West, H.A. Direct Metal Fabrication of Titanium Implants with Tailored Materials and Mechanical Properties Using Electron Beam Melting Technology. Mater. Sci. Eng. C 2008, 28, 366–373. [Google Scholar] [CrossRef]
- Mazzoli, A.; Germani, M.; Raffaeli, R. Direct Fabrication through Electron Beam Melting Technology of Custom Cranial Implants Designed in a PHANToM-Based Haptic Environment. Mater. Des. 2009, 30, 3186–3192. [Google Scholar] [CrossRef]
- Kantaros, A.; Piromalis, D. Fabricating Lattice Structures via 3D Printing: The Case of Porous Bio-Engineered Scaffolds. Appl. Mech. 2021, 2, 289–302. [Google Scholar] [CrossRef]
- Cheng, L.; Suresh, K.S.; He, H.; Rajput, R.S.; Feng, Q.; Ramesh, S.; Wang, Y.; Krishnan, S.; Ostrovidov, S.; Camci-Unal, G.; et al. 3D Printing of Micro- and Nanoscale Bone Substitutes: A Review on Technical and Translational Perspectives. Int. J. Nanomed. 2021, 16, 4289–4319. [Google Scholar] [CrossRef]
- Larsen, C.G.; Stapleton, E.J.; Sgaglione, J.; Sgaglione, M.; Goldstein, T.; Sgaglione, N.A.; Grande, D.A. Three-Dimensional Bioprinting in Orthopaedics. JBJS Rev. 2020, 8, e0204. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Yang, Y. Application of 3D Printing in Implantable Medical Devices. BioMed Res. Int. 2021, 2021, 6653967. [Google Scholar] [CrossRef] [PubMed]
- Chae, S.; Lee, S.-S.; Choi, Y.-J.; Hong, D.H.; Gao, G.; Wang, J.H.; Cho, D.-W. 3D Cell-Printing of Biocompatible and Functional Meniscus Constructs Using Meniscus-derived Bioink. Biomaterials 2021, 267, 120466. [Google Scholar] [CrossRef] [PubMed]
- Frendø, M.; Frithioff, A.; Konge, L.; Sørensen, M.S.; Andersen, S.A.W. Cochlear Implant Surgery: Learning Curve in Virtual Reality Simulation Training and Transfer of Skills to a 3D-Printed Temporal Bone—A Prospective Trial. Cochlear Implant. Int. 2021, 22, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Frithioff, A.; Frendø, M.; Pedersen, D.B.; Sørensen, M.S.; Wuyts Andersen, S.A. 3D-Printed Models for Temporal Bone Surgical Training: A Systematic Review. Otolaryngol. Neck Surg. 2021, 165, 019459982199338. [Google Scholar] [CrossRef] [PubMed]
- Barber, S.R.; Kozin, E.D.; Dedmon, M.; Lin, B.M.; Lee, K.; Sinha, S.; Black, N.; Remenschneider, A.K.; Lee, D.J. 3D-Printed Pediatric Endoscopic Ear Surgery Simulator for Surgical Training. Int. J. Pediatr. Otorhinolaryngol. 2016, 90, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.-P.; Li, C.-Z.; Chen, G.-Q. Multimaterial and Multicolor 3D-Printed Model in Training of Transnasal Endoscopic Surgery for Pituitary Adenoma. Neurosurg. Focus 2019, 47, E21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferreira e Silva, L.; Chisté Ferreira, M.; Couceiro Seto, I.I.; Martins Umbelino, A.; Aguiar Gomes, V.C.; de Borborema Garcia, L.; Almeida Amaro, L.J. A Three-Dimensional Printed Myringotomy, Tympanostomy and Ventilation Tube Placement Simulator. J. Laryngol. Otol. 2021, 135, 420–425. [Google Scholar] [CrossRef] [PubMed]
- Gordon, A.R.; Schreiber, J.E.; Patel, A.; Tepper, O.M. 3D Printed Surgical Guides Applied in Rhinoplasty to Help Obtain Ideal Nasal Profile. Aesthetic Plast. Surg. 2021, 45, 2852–2859. [Google Scholar] [CrossRef] [PubMed]
- Tretiakow, D.; Tesch, K.; Meyer-Szary, J.; Markiet, K.; Skorek, A. Three-Dimensional Modeling and Automatic Analysis of the Human Nasal Cavity and Paranasal Sinuses Using the Computational Fluid Dynamics Method. Eur. Arch. Otorhinolaryngol. 2020, 278, 1443–1453. [Google Scholar] [CrossRef]
- Moniripiri, M.; Amjadimanesh, H.; Faramarzi, M.; Sadrizadeh, S.; Abouali, O. Numerical Simulation of Unsteady Airflow in a Nasal Cavity for Various Sizes of Maxillary Sinus Opening in a Virtual Endoscopic Surgery. Respir. Physiol. Neurobiol. 2021, 291, 103690. [Google Scholar] [CrossRef] [PubMed]
- Haemmerli, J.; Davidovic, A.; Meling, T.R.; Chavaz, L.; Schaller, K.; Bijlenga, P. Evaluation of the Precision of Operative Augmented Reality Compared to Standard Neuronavigation Using a 3D-Printed Skull. Neurosurg. Focus 2021, 50, E17. [Google Scholar] [CrossRef] [PubMed]
- Valtonen, O.; Ormiskangas, J.; Kivekäs, I.; Rantanen, V.; Dean, M.; Poe, D.; Järnstedt, J.; Lekkala, J.; Saarenrinne, P.; Rautiainen, M. Three-Dimensional Printing of the Nasal Cavities for Clinical Experiments. Sci. Rep. 2020, 10, 502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deonarain, A.R.; Harrison, R.V.; Gordon, K.A.; Looi, T.; Agur, A.M.R.; Estrada, M.; Wolter, N.E.; Propst, E.J. Synthetic Simulator for Surgical Training in Tracheostomy and Open Airway Surgery. Laryngoscope 2021, 131, E2378–E2386. [Google Scholar] [CrossRef]
- Sananès, N.; Lodi, M.; Koch, A.; Lecointre, L.; Sananès, A.; Lefebvre, N.; Debry, C. 3D-Printed Simulator for Nasopharyngeal Swab Collection for COVID-19. Eur. Arch. Otorhinolaryngol. 2021, 278, 2649–2651. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo, D.A. Fibula Free Flap: A New Method of Mandible Reconstruction. Plast. Reconstr. Surg. 1989, 84, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Mavrogenis, A.F.; Igoumenou, V.G.; Ignatiadis, I.; Mourouzis, K.; Rallis, G.; Spyridonos, S.G. Microsurgical Reconstruction of Complex Oromandibular Defects: An Update. Injury 2019, 50, S117–S122. [Google Scholar] [CrossRef]
- Pellini, R.; Mercante, G.; Spriano, G. Step-by-Step Mandibular Reconstruction with Free Fibula Flap Modelling. Acta Otorhinolaryngol. Ital. Organo Uff. Della Soc. Ital. Otorinolaringol. E Chir. Cerv.-Facc. 2012, 32, 405–409. [Google Scholar]
- Hirsch, D.L.; Garfein, E.S.; Christensen, A.M.; Weimer, K.A.; Saddeh, P.B.; Levine, J.P. Use of Computer-Aided Design and Computer-Aided Manufacturing to Produce Orthognathically Ideal Surgical Outcomes: A Paradigm Shift in Head and Neck Reconstruction. J. Oral Maxillofac. Surg. 2009, 67, 2115–2122. [Google Scholar] [CrossRef]
- Succo, G.; Berrone, M.; Battiston, B.; Tos, P.; Goia, F.; Appendino, P.; Crosetti, E. Step-by-Step Surgical Technique for Mandibular Reconstruction with Fibular Free Flap: Application of Digital Technology in Virtual Surgical Planning. Eur. Arch. Otorhinolaryngol. 2015, 272, 1491–1501. [Google Scholar] [CrossRef]
- Toto, J.M.; Chang, E.I.; Agag, R.; Devarajan, K.; Patel, S.A.; Topham, N.S. Improved Operative Efficiency of Free Fibula Flap Mandible Reconstruction with Patient-Specific, Computer-Guided Preoperative Planning: Preoperative Modeling for Free Fibula Flaps. Head Neck 2015, 37, 1660–1664. [Google Scholar] [CrossRef] [PubMed]
- Culié, D.; Dassonville, O.; Poissonnet, G.; Riss, J.-C.; Fernandez, J.; Bozec, A. Virtual Planning and Guided Surgery in Fibular Free-Flap Mandibular Reconstruction: A 29-Case Series. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2016, 133, 175–178. [Google Scholar] [CrossRef]
- Blanc, J.; Fuchsmann, C.; Nistiriuc-Muntean, V.; Jacquenot, P.; Philouze, P.; Ceruse, P. Evaluation of Virtual Surgical Planning Systems and Customized Devices in Fibula Free Flap Mandibular Reconstruction. Eur. Arch. Otorhinolaryngol. 2019, 276, 3477–3486. [Google Scholar] [CrossRef]
- Powcharoen, W.; Yang, W.; Yan Li, K.; Zhu, W.; Su, Y. Computer-Assisted versus Conventional Freehand Mandibular Reconstruction with Fibula Free Flap: A Systematic Review and Meta-Analysis. Plast. Reconstr. Surg. 2019, 144, 1417–1428. [Google Scholar] [CrossRef] [PubMed]
- Monaco, C.; Stranix, J.T.; Avraham, T.; Brecht, L.; Saadeh, P.B.; Hirsch, D.; Levine, J.P. Evolution of Surgical Techniques for Mandibular Reconstruction Using Free Fibula Flaps: The next Generation: Virtual Surgical Planning and Reconstructive Complexity. Head Neck 2016, 38, E2066–E2073. [Google Scholar] [CrossRef]
- Wu, P.; Hu, L.; Li, H.; Feng, L.; Liu, Y.; Zhang, S.; Li, X.-C.; Zhang, M.-L.; Yang, S.-Y.; Lu, R.-J. Clinical Application and Accuracy Analysis of 3D Printing Guide Plate Based on Polylactic Acid in Mandible Reconstruction with Fibula Flap. Ann. Transl. Med. 2021, 9, 460. [Google Scholar] [CrossRef] [PubMed]
- Tarsitano, A.; Battaglia, S.; Ricotta, F.; Bortolani, B.; Cercenelli, L.; Marcelli, E.; Cipriani, R.; Marchetti, C. Accuracy of CAD/CAM Mandibular Reconstruction: A Three-Dimensional, Fully Virtual Outcome Evaluation Method. J. Cranio-Maxillofac. Surg. 2018, 46, 1121–1125. [Google Scholar] [CrossRef]
- Zweifel, D.F.; Simon, C.; Hoarau, R.; Pasche, P.; Broome, M. Are Virtual Planning and Guided Surgery for Head and Neck Reconstruction Economically Viable? J. Oral Maxillofac. Surg. 2015, 73, 170–175. [Google Scholar] [CrossRef]
- Cogswell, P.M.; Rischall, M.A.; Alexander, A.E.; Dickens, H.J.; Lanzino, G.; Morris, J.M. Intracranial Vasculature 3D Printing: Review of Techniques and Manufacturing Processes to Inform Clinical Practice. 3D Print. Med. 2020, 6, 18. [Google Scholar] [CrossRef]
- Nagassa, R.G.; McMenamin, P.G.; Adams, J.W.; Quayle, M.R.; Rosenfeld, J.V. Advanced 3D Printed Model of Middle Cerebral Artery Aneurysms for Neurosurgery Simulation. 3D Print. Med. 2019, 5, 11. [Google Scholar] [CrossRef] [Green Version]
- Weinstock, P.; Prabhu, S.P.; Flynn, K.; Orbach, D.B.; Smith, E. Optimizing Cerebrovascular Surgical and Endovascular Procedures in Children via Personalized 3D Printing. J. Neurosurg. Pediatr. 2015, 16, 584–589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weinstock, P.; Rehder, R.; Prabhu, S.P.; Forbes, P.W.; Roussin, C.J.; Cohen, A.R. Creation of a Novel Simulator for Minimally Invasive Neurosurgery: Fusion of 3D Printing and Special Effects. J. Neurosurg. Pediatr. 2017, 20, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Randazzo, M.; Pisapia, J.; Singh, N.; Thawani, J. 3D Printing in Neurosurgery: A Systematic Review. Surg. Neurol. Int. 2016, 7, 801. [Google Scholar] [CrossRef] [Green Version]
- Kosterhon, M.; Neufurth, M.; Neulen, A.; Schäfer, L.; Conrad, J.; Kantelhardt, S.R.; Müller, W.E.G.; Ringel, F. Multicolor 3D Printing of Complex Intracranial Tumors in Neurosurgery. J. Vis. Exp. 2020, 60471. [Google Scholar] [CrossRef] [PubMed]
- Cecchinato, R.; Berjano, P.; Zerbi, A.; Damilano, M.; Redaelli, A.; Lamartina, C. Pedicle Screw Insertion with Patient-Specific 3D-Printed Guides Based on Low-Dose CT Scan Is More Accurate than Free-Hand Technique in Spine Deformity Patients: A Prospective, Randomized Clinical Trial. Eur. Spine J. 2019, 28, 1712–1723. [Google Scholar] [CrossRef]
- Chen, P.-C.; Chang, C.-C.; Chen, H.-T.; Lin, C.-Y.; Ho, T.-Y.; Chen, Y.-J.; Tsai, C.-H.; Tsou, H.-K.; Lin, C.-S.; Chen, Y.-W.; et al. The Accuracy of 3D Printing Assistance in the Spinal Deformity Surgery. BioMed Res. Int. 2019, 2019, 7196528. [Google Scholar] [CrossRef] [Green Version]
- Clifton, W.; Nottmeier, E.; ReFaey, K.; Damon, A.; Vlasak, A.; Tubbs, R.S.; Clifton, C.L.; Pichelmann, M. Ex Vivo Virtual and 3D Printing Methods for Evaluating an Anatomy-based Spinal Instrumentation Technique for the 12th Thoracic Vertebra. Clin. Anat. 2020, 33, 458–467. [Google Scholar] [CrossRef]
- Weiss, M.Y.; Melnyk, R.; Mix, D.; Ghazi, A.; Vates, G.E.; Stone, J.J. Design and Validation of a Cervical Laminectomy Simulator Using 3D Printing and Hydrogel Phantoms. Oper. Neurosurg. 2019, 8, opz129. [Google Scholar] [CrossRef]
- Waran, V.; Narayanan, V.; Karuppiah, R.; Thambynayagam, H.C.; Muthusamy, K.A.; Rahman, Z.A.A.; Kirollos, R.W. Neurosurgical Endoscopic Training via a Realistic 3-Dimensional Model with Pathology. Simul. Healthc. J. Soc. Simul. Healthc. 2015, 10, 43–48. [Google Scholar] [CrossRef] [Green Version]
- Miller, J.L.; Ahn, E.S.; Garcia, J.R.; Miller, G.T.; Satin, A.J.; Baschat, A.A. Ultrasound-Based Three-Dimensional Printed Medical Model for Multispecialty Team Surgical Rehearsal Prior to Fetoscopic Myelomeningocele Repair: Letter to the Editor. Ultrasound Obstet. Gynecol. 2018, 51, 836–837. [Google Scholar] [CrossRef]
- Flaxman, T.E.; Cooke, C.M.; Miguel, O.X.; Sheikh, A.M.; Singh, S.S. A Review and Guide to Creating Patient Specific 3D Printed Anatomical Models from MRI for Benign Gynecologic Surgery. 3D Print. Med. 2021, 7, 17. [Google Scholar] [CrossRef] [PubMed]
- Sandrini, C.; Lombardi, C.; Shearn, A.I.U.; Ordonez, M.V.; Caputo, M.; Presti, F.; Luciani, G.B.; Rossetti, L.; Biglino, G. Three-Dimensional Printing of Fetal Models of Congenital Heart Disease Derived from Microfocus Computed Tomography: A Case Series. Front. Pediatr. 2020, 7, 567. [Google Scholar] [CrossRef] [PubMed]
- Biglino, G.; Milano, E.G.; Capelli, C.; Wray, J.; Shearn, A.I.; Caputo, M.; Bucciarelli-Ducci, C.; Taylor, A.M.; Schievano, S. Three-Dimensional Printing in Congenital Heart Disease: Considerations on Training and Clinical Implementation from a Teaching Session. Int. J. Artif. Organs 2019, 42, 595–599. [Google Scholar] [CrossRef] [PubMed]
- Ruedinger, K.L.; Zhou, H.; Trampe, B.; Heiser, T.; Srinivasan, S.; Iruretagoyena, J.I.; Roldán-Alzate, A. Modeling Fetal Cardiac Anomalies from Prenatal Echocardiography With 3-Dimensional Printing and 4-Dimensional Flow Magnetic Resonance Imaging. Circ. Cardiovasc. Imaging 2018, 11, e007705. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, J.; Shi, H.; Chen, Q.; Hu, J.; Zhang, Y.; Song, H.; Zhou, Q. Three-Dimensional Printed Model Fabrication and Effectiveness Evaluation in Fetuses with Congenital Heart Disease or with a Normal Heart. J. Ultrasound Med. 2021, 40, 15–28. [Google Scholar] [CrossRef] [PubMed]
- Abudayyeh, I.; Gordon, B.; Ansari, M.M.; Jutzy, K.; Stoletniy, L.; Hilliard, A. A Practical Guide to Cardiovascular 3D Printing in Clinical Practice: Overview and Examples. J. Intervent. Cardiol. 2018, 31, 375–383. [Google Scholar] [CrossRef]
- Mitsouras, D.; Liacouras, P.; Imanzadeh, A.; Giannopoulos, A.A.; Cai, T.; Kumamaru, K.K.; George, E.; Wake, N.; Caterson, E.J.; Pomahac, B.; et al. Medical 3D Printing for the Radiologist. RadioGraphics 2015, 35, 1965–1988. [Google Scholar] [CrossRef] [PubMed]
- Otton, J.M.; Birbara, N.S.; Hussain, T.; Greil, G.; Foley, T.A.; Pather, N. 3D Printing from Cardiovascular CT: A Practical Guide and Review. Cardiovasc. Diagn. Ther. 2017, 7, 507–526. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mackey, A.; Ng, J.I.; Core, J.; Nguyen, L.; Cross, D.; Lim, P.; Woodfield, C.; Pugliese, R.; Ku, B. Three-Dimensional–Printed Uterine Model for Surgical Planning of a Cesarean Delivery Complicated by Multiple Myomas. Obstet. Gynecol. 2019, 133, 720–724. [Google Scholar] [CrossRef]
- Baek, M.-H.; Kim, D.-Y.; Kim, N.; Rhim, C.C.; Kim, J.-H.; Nam, J.-H. Incorporating a 3-Dimensional Printer into the Management of Early-Stage Cervical Cancer: 3D Printer in Cervical Cancer. J. Surg. Oncol. 2016, 114, 150–152. [Google Scholar] [CrossRef]
- Barsky, M.; Kelley, R.; Bhora, F.Y.; Hardart, A. Customized Pessary Fabrication Using Three-Dimensional Printing Technology. Obstet. Gynecol. 2018, 131, 493–497. [Google Scholar] [CrossRef] [PubMed]
- Punyaratabandhu, T.; Liacouras, P.C.; Pairojboriboon, S. Using 3D Models in Orthopedic Oncology: Presenting Personalized Advantages in Surgical Planning and Intraoperative Outcomes. 3D Print. Med. 2018, 4, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corona, P.S.; Vicente, M.; Tetsworth, K.; Glatt, V. Preliminary Results Using Patient-Specific 3d Printed Models to Improve Preoperative Planning for Correction of Post-Traumatic Tibial Deformities with Circular Frames. Injury 2018, 49, S51–S59. [Google Scholar] [CrossRef] [PubMed]
- Maddox, M.M.; Feibus, A.; Liu, J.; Wang, J.; Thomas, R.; Silberstein, J.L. 3D-Printed Soft-Tissue Physical Models of Renal Malignancies for Individualized Surgical Simulation: A Feasibility Study. J. Robot. Surg. 2018, 12, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Komai, Y.; Sugimoto, M.; Gotohda, N.; Matsubara, N.; Kobayashi, T.; Sakai, Y.; Shiga, Y.; Saito, N. Patient-Specific 3-Dimensional Printed Kidney Designed for “4D” Surgical Navigation: A Novel Aid to Facilitate Minimally Invasive Off-Clamp Partial Nephrectomy in Complex Tumor Cases. Urology 2016, 91, 226–233. [Google Scholar] [CrossRef] [PubMed]
- The ESUT Research Group; Porpiglia, F.; Bertolo, R.; Checcucci, E.; Amparore, D.; Autorino, R.; Dasgupta, P.; Wiklund, P.; Tewari, A.; Liatsikos, E.; et al. Development and Validation of 3D Printed Virtual Models for Robot-Assisted Radical Prostatectomy and Partial Nephrectomy: Urologists’ and Patients’ Perception. World J. Urol. 2018, 36, 201–207. [Google Scholar] [CrossRef]
- Shin, T.; Ukimura, O.; Gill, I.S. Three-Dimensional Printed Model of Prostate Anatomy and Targeted Biopsy-Proven Index Tumor to Facilitate Nerve-Sparing Prostatectomy. Eur. Urol. 2016, 69, 377–379. [Google Scholar] [CrossRef]
- Silberstein, J.L.; Maddox, M.M.; Dorsey, P.; Feibus, A.; Thomas, R.; Lee, B.R. Physical Models of Renal Malignancies Using Standard Cross-Sectional Imaging and 3-Dimensional Printers: A Pilot Study. Urology 2014, 84, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Jomoto, W.; Tanooka, M.; Doi, H.; Kikuchi, K.; Mitsuie, C.; Yamada, Y.; Suzuki, T.; Yamano, T.; Ishikura, R.; Kotoura, N.; et al. Development of a Three-Dimensional Surgical Navigation System with Magnetic Resonance Angiography and a Three-Dimensional Printer for Robot-Assisted Radical Prostatectomy. Cureus 2018, 10. [Google Scholar] [CrossRef] [Green Version]
- Li, H.; Chen, Y.; Liu, C.; Li, B.; Xu, K.; Bao, S. Construction of a Three-Dimensional Model of Renal Stones: Comprehensive Planning for Percutaneous Nephrolithotomy and Assistance in Surgery. World J. Urol. 2013, 31, 1587–1592. [Google Scholar] [CrossRef]
- von Rundstedt, F.C.; Scovell, J.M.; Agrawal, S.; Zaneveld, J.; Link, R.E. Utility of Patient-Specific Silicone Renal Models for Planning and Rehearsal of Complex Tumour Resections Prior to Robot-Assisted Laparoscopic Partial Nephrectomy. BJU Int. 2017, 119, 598–604. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Gao, X.; Yang, Q.; Wang, H.; Shi, T.; Chang, Y.; Xu, C.; Sun, Y. Three-Dimensional Printing Technique Assisted Cognitive Fusion in Targeted Prostate Biopsy. Asian J. Urol. 2015, 2, 214–219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blankstein, U.; Lantz, A.G.; Honey, R.J.D.; Pace, K.T.; Ordon, M.; Lee, J.Y. Simulation-Based Flexible Ureteroscopy Training Using a Novel Ureteroscopy Part-Task Trainer. Can. Urol. Assoc. J. 2015, 9, 331. [Google Scholar] [CrossRef] [PubMed]
- Park, C.-J.; Kim, H.-W.; Jeong, S.; Seo, S.; Park, Y.; Moon, H.S.; Lee, J.-H. Anti-Reflux Ureteral Stent with Polymeric Flap Valve Using Three-Dimensional Printing: An In Vitro Study. J. Endourol. 2015, 29, 933–938. [Google Scholar] [CrossRef]
- Canvasser, N.E.; De, S.; Koseoglu, E.; Lay, A.H.; Sorokin, I.; Fernandez, R.; Cadeddu, J.A. Three-Dimensional Printing of Surgical Clips: An In Vitro Pilot Study and Trial of Efficacy. J. Endourol. 2017, 31, 930–933. [Google Scholar] [CrossRef]
- del Junco, M.; Okhunov, Z.; Yoon, R.; Khanipour, R.; Juncal, S.; Abedi, G.; Lusch, A.; Landman, J. Development and Initial Porcine and Cadaver Experience with Three-Dimensional Printing of Endoscopic and Laparoscopic Equipment. J. Endourol. 2015, 29, 58–62. [Google Scholar] [CrossRef] [Green Version]
- Ali, M.; Pr, A.K.; Yoo, J.J.; Zahran, F.; Atala, A.; Lee, S.J. A Photo-Crosslinkable Kidney ECM-Derived Bioink Accelerates Renal Tissue Formation. Adv. Healthc. Mater. 2019, 8, 1800992. [Google Scholar] [CrossRef] [PubMed]
- de Kemp, V.; de Graaf, P.; Fledderus, J.O.; Ruud Bosch, J.L.H.; de Kort, L.M.O. Tissue Engineering for Human Urethral Reconstruction: Systematic Review of Recent Literature. PLoS ONE 2015, 10, e0118653. [Google Scholar] [CrossRef]
- Chen, M.Y.; Skewes, J.; Desselle, M.; Wong, C.; Woodruff, M.A.; Dasgupta, P.; Rukin, N.J. Current Applications of Three-dimensional Printing in Urology. BJU Int. 2020, 125, 17–27. [Google Scholar] [CrossRef] [Green Version]
- Cacciamani, G.E.; Okhunov, Z.; Meneses, A.D.; Rodriguez-Socarras, M.E.; Rivas, J.G.; Porpiglia, F.; Liatsikos, E.; Veneziano, D. Impact of Three-Dimensional Printing in Urology: State of the Art and Future Perspectives. A Systematic Review by ESUT-YAUWP Group. Eur. Urol. 2019, 76, 209–221. [Google Scholar] [CrossRef]
- Atalay, H.A.; Canat, H.L.; Ülker, V.; Alkan, İ.; Özkuvanci, Ü.; Altunrende, F. Impact of Personalized Three-Dimensional (3D) Printed Pelvicalyceal System Models on Patient Information in Percutaneous Nephrolithotripsy Surgery: A Pilot Study. Int. Braz. J. Urol. 2017, 43, 470–475. [Google Scholar] [CrossRef] [PubMed]
- Pang, G.; Futter, C.; Pincus, J.; Dhanani, J.; Laupland, K.B. Development and Testing of a Low Cost Simulation Manikin for Extracorporeal Cardiopulmonary Resuscitation (ECPR) Using 3-Dimensional Printing. Resuscitation 2020, 149, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Baribeau, Y.; Bortman, J.; Khamooshian, A.; Laham, R.; Mahmood, F.; Mahmood, F.; Sharkey, A.; Steely, A.; Matyal, R. A 3-Dimensionally Printed, High-Fidelity Ultrasound-Guided Pericardiocentesis Training Model. J. Cardiothorac. Vasc. Anesth. 2020, 34, 245–247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lord, S.; Lord, G.; Geary, S. A Novel, Low-Cost, Low-Fidelity Pericardiocentesis Teaching Model. West. J. Emerg. Med. 2021, 22, 931–936. [Google Scholar] [CrossRef]
- Tan, T.X.; Wu, Y.Y.; Riley, I.; Duanmu, Y.; Rylowicz, S.; Shimada, K. Development of a Three-Dimensionally Printed Ultrasound-Guided Peripheral Intravenous Catheter Phantom. Cureus 2021, 13, e17139. [Google Scholar] [CrossRef] [PubMed]
- Engelbrecht, R.; Patey, C.; Dubrowski, A.; Norman, P. Development and Evaluation of a 3D-Printed Adult Proximal Tibia Model for Simulation Training in Intraosseous Access. Cureus 2020, 12, e12180. [Google Scholar] [CrossRef] [PubMed]
- Maier, P.; Silvestro, E.; Goldfarb, S.B.; Piccione, J.; Phinizy, P.A.; Andronikou, S. Three-Dimensional Printed Realistic Pediatric Static and Dynamic Airway Models for Bronchoscopy and Foreign Body Removal Training. Pediatr. Pulmonol. 2021, 56, 2654–2659. [Google Scholar] [CrossRef] [PubMed]
- Leong, A.; Benscoter, D.; Brewington, J.; Torres-Silva, C.; Wood, R.E. Pediatric Flexible Airway Endoscopy Training during a Pandemic and beyond: Bending the Curve. Pediatr. Pulmonol. 2021, 56, 1386–1388. [Google Scholar] [CrossRef] [PubMed]
- Ho, B.H.K.; Chen, C.J.; Tan, G.J.S.; Yeong, W.Y.; Tan, H.K.J.; Lim, A.Y.H.; Ferenczi, M.A.; Mogali, S.R. Multi-Material Three Dimensional Printed Models for Simulation of Bronchoscopy. BMC Med. Educ. 2019, 19, 236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kei, J.; Mebust, D.P.; Duggan, L.V. The REAL CRIC Trainer: Instructions for Building an Inexpensive, Realistic Cricothyrotomy Simulator With Skin and Tissue, Bleeding, and Flash of Air. J. Emerg. Med. 2019, 56, 426–430. [Google Scholar] [CrossRef]
- Dziedzic, R.; Rzyman, G.; Rzyman, W. Three-Dimensional Printed Trachea Helps Develop Tailored Treatment for Tracheobronchomalacia. Pol. Arch. Intern. Med. 2020, 130, 140–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Han, M.; Portnova, A.A.; Lester, M.; Johnson, M. A Do-It-Yourself 3D-Printed Thoracic Spine Model for Anesthesia Resident Simulation. PLoS ONE 2020, 15, e0228665. [Google Scholar] [CrossRef] [PubMed]
- Odom, M.; Gomez, J.R.; Danelson, K.A.; Sarwal, A. Development of a Homemade Spinal Model for Simulation to Teach Ultrasound Guidance for Lumbar Puncture. Neurocrit. Care 2019, 31, 550–558. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Ahn, J.; Yoon, S.U.; Choo, K.S.; Kim, H.-J.; Chung, M.; Kim, H.Y. Prediction of Endotracheal Tube Size Using a Printed Three-Dimensional Airway Model in Pediatric Patients with Congenital Heart Disease: A Prospective, Single-Center, Single-Group Study. Korean J. Anesthesiol. 2021, 74, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Shaylor, R.; Verenkin, V.; Golden, E.; Matot, I. The Use of Three-Dimensional Printing and Virtual Reality to Develop a Personalised Airway Plan in a 7.5-Year-Old Child: A Case Report. Eur. J. Anaesthesiol. 2020, 37, 512–515. [Google Scholar] [CrossRef] [PubMed]
- Olomu, P.; Galvez, J.; Silvestro, E.; Kiss, E.; Gonzalez, A.; Booth, T.; Hussain, M. Personalized 3D Printed Model for Difficult Airway Management Planning: The Future Is Here. Trends Anaesth. Crit. Care 2020, 30, e145–e146. [Google Scholar] [CrossRef]
- Han, B.; Liu, Y.; Zhang, X.; Wang, J. Three-Dimensional Printing as an Aid to Airway Evaluation after Tracheotomy in a Patient with Laryngeal Carcinoma. BMC Anesthesiol. 2016, 16, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atun, R.; Jaffray, D.A.; Barton, M.B.; Bray, F.; Baumann, M.; Vikram, B.; Hanna, T.P.; Knaul, F.M.; Lievens, Y.; Lui, T.Y.M.; et al. Expanding Global Access to Radiotherapy. Lancet Oncol. 2015, 16, 1153–1186. [Google Scholar] [CrossRef]
- Rooney, M.K.; Rosenberg, D.M.; Braunstein, S.; Cunha, A.; Damato, A.L.; Ehler, E.; Pawlicki, T.; Robar, J.; Tatebe, K.; Golden, D.W. Three-dimensional Printing in Radiation Oncology: A Systematic Review of the Literature. J. Appl. Clin. Med. Phys. 2020, 21, 15–26. [Google Scholar] [CrossRef]
- Dyer, B.A.; Campos, D.D.; Hernandez, D.D.; Wright, C.L.; Perks, J.R.; Lucero, S.A.; Bewley, A.F.; Yamamoto, T.; Zhu, X.; Rao, S.S. Characterization and Clinical Validation of Patient-Specific Three-Dimensional Printed Tissue-Equivalent Bolus for Radiotherapy of Head and Neck Malignancies Involving Skin. Phys. Med. 2020, 77, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.L.; Dietrich, M.C.; Desai, U.G.; Das, A.; Yu, S.; Xiang, H.F.; Jaffe, C.C.; Hirsch, A.E.; Bloch, B.N. A 3D-Printed Patient-Specific Phantom for External Beam Radiation Therapy of Prostate Cancer. J. Eng. Sci. Med. Diagn. Ther. 2018, 1, 041004. [Google Scholar] [CrossRef] [PubMed]
- Biltekin, F.; Yazici, G.; Ozyigit, G. Characterization of 3D-Printed Bolus Produced at Different Printing Parameters. Med. Dosim. 2021, 46, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Craft, D.F.; Kry, S.F.; Balter, P.; Salehpour, M.; Woodward, W.; Howell, R.M. Material Matters: Analysis of Density Uncertainty in 3D Printing and Its Consequences for Radiation Oncology. Med. Phys. 2018, 45, 1614–1621. [Google Scholar] [CrossRef] [PubMed]
- Hazelaar, C.; van Eijnatten, M.; Dahele, M.; Wolff, J.; Forouzanfar, T.; Slotman, B.; Verbakel, W.F.A.R. Using 3D Printing Techniques to Create an Anthropomorphic Thorax Phantom for Medical Imaging Purposes. Med. Phys. 2018, 45, 92–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biltekin, F.; Akyol, H.; Gültekin, M.; Yildiz, F. 3D Printer-Based Novel Intensity-Modulated Vaginal Brachytherapy Applicator: Feasibility Study. J. Contemp. Brachytherapy 2020, 12, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Logar, H.B.Z.; Hudej, R.; Šegedin, B. Development and Assessment of 3D-Printed Individual Applicators in Gynecological MRI-Guided Brachytherapy. J. Contemp. Brachytherapy 2019, 11, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Semeniuk, O.; Cherpak, A.; Robar, J. Design and Evaluation of 3D Printable Patient-specific Applicators for Gynecologic HDR Brachytherapy. Med. Phys. 2021, 48, 4053–4063. [Google Scholar] [CrossRef] [PubMed]
- Arenas, M.; Sabater, S.; Sintas, A.; Arguís, M.; Hernández, V.; Árquez, M.; López, I.; Rovirosa, À.; Puig, D. Individualized 3D Scanning and Printing for Non-Melanoma Skin Cancer Brachytherapy: A Financial Study for Its Integration into Clinical Workflow. J. Contemp. Brachytherapy 2017, 3, 270–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, E.; Zhang, Y.; Zhang, H.; Jia, C.; Liang, Y.; Wang, J. Dosimetry Study of Three-Dimensional Print Template for 125I Implantation Therapy. Radiat. Oncol. 2021, 16, 115. [Google Scholar] [CrossRef] [PubMed]
- Chiu, T.; Xiong, Z.; Parsons, D.; Folkert, M.R.; Medin, P.M.; Hrycushko, B. Low-Cost 3D Print–Based Phantom Fabrication to Facilitate Interstitial Prostate Brachytherapy Training Program. Brachytherapy 2020, 19, 800–811. [Google Scholar] [CrossRef]
- Doyle, A.J.; Sullivan, F.; Walsh, J.; King, D.M.; Cody, D.; Browne, J.E. Development and Preliminary Evaluation of an Anthropomorphic Trans-Rectal Ultrasound Prostate Brachytherapy Training Phantom. Ultrasound Med. Biol. 2021, 47, 833–846. [Google Scholar] [CrossRef] [PubMed]
- Campelo, S.; Subashi, E.; Meltsner, S.G.; Chang, Z.; Chino, J.; Craciunescu, O. Multimaterial Three-Dimensional Printing in Brachytherapy: Prototyping Teaching Tools for Interstitial and Intracavitary Procedures in Cervical Cancers. Brachytherapy 2020, 19, 767–776. [Google Scholar] [CrossRef] [PubMed]
- Nowak, L.J.; Pawlowska, E. Technical Note: An Algorithm and Software for Conversion of Radiotherapy Contour-sequence Data to Ready-to-print 3D Structures. Med. Phys. 2019, 46, 1829–1832. [Google Scholar] [CrossRef] [PubMed]
- Chae, M.P.; Chung, R.D.; Smith, J.A.; Hunter-Smith, D.J.; Rozen, W.M. The Accuracy of Clinical 3D Printing in Reconstructive Surgery: Literature Review and in Vivo Validation Study. Gland Surg. 2021, 10, 2293–2303. [Google Scholar] [CrossRef] [PubMed]
- Ravi, P.; Chepelev, L.; Lawera, N.; Haque, K.M.A.; Chen, V.C.P.; Ali, A.; Rybicki, F.J. A Systematic Evaluation of Medical 3D Printing Accuracy of Multi-pathological Anatomical Models for Surgical Planning Manufactured in Elastic and Rigid Material Using Desktop Inverted Vat Photopolymerization. Med. Phys. 2021, 48, 3223–3233. [Google Scholar] [CrossRef] [PubMed]
- Willemsen, K.; Ketel, M.H.M.; Zijlstra, F.; Florkow, M.C.; Kuiper, R.J.A.; van der Wal, B.C.H.; Weinans, H.; Pouran, B.; Beekman, F.J.; Seevinck, P.R.; et al. 3D-Printed Saw Guides for Lower Arm Osteotomy, a Comparison between a Synthetic CT and CT-Based Workflow. 3D Print. Med. 2021, 7, 13. [Google Scholar] [CrossRef] [PubMed]
- Haryńska, A.; Gubanska, I.; Kucinska-Lipka, J.; Janik, H. Fabrication and Characterization of Flexible Medical-Grade TPU Filament for Fused Deposition Modeling 3DP Technology. Polymers 2018, 10, 1304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hong, N.; Yang, G.-H.; Lee, J.; Kim, G. 3D Bioprinting and Its in Vivo Applications. J. Biomed. Mater. Res. B Appl. Biomater. 2018, 106, 444–459. [Google Scholar] [CrossRef]
- Zhuang, W.; Ye, G.; Wu, J.; Wang, L.; Fang, G.; Ye, Z.; Lai, G.; Qiu, X.; Sang, H. A 3D-Printed Bioactive Polycaprolactone Scaffold Assembled with Core/Shell Microspheres as a Sustained BMP2-Releasing System for Bone Repair. Mater. Sci. Eng. C Mater. Biol. Appl. 2022, 112619. [Google Scholar] [CrossRef]
- Turnbull, G.; Clarke, J.; Picard, F.; Riches, P.; Jia, L.; Han, F.; Li, B.; Shu, W. 3D Bioactive Composite Scaffolds for Bone Tissue Engineering. Bioact. Mater. 2018, 3, 278–314. [Google Scholar] [CrossRef] [Green Version]
- Prasad, L.K.; Smyth, H. 3D Printing Technologies for Drug Delivery: A Review. Drug Dev. Ind. Pharm. 2016, 42, 1019–1031. [Google Scholar] [CrossRef] [PubMed]
- Park, S.A.; Lee, S.J.; Lim, K.S.; Bae, I.H.; Lee, J.H.; Kim, W.D.; Jeong, M.H.; Park, J.-K. In Vivo Evaluation and Characterization of a Bio-Absorbable Drug-Coated Stent Fabricated Using a 3D-Printing System. Mater. Lett. 2015, 141, 355–358. [Google Scholar] [CrossRef]
- Goyanes, A.; Buanz, A.B.M.; Basit, A.W.; Gaisford, S. Fused-Filament 3D Printing (3DP) for Fabrication of Tablets. Int. J. Pharm. 2014, 476, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Bastawrous, S.; Wu, L.; Strzelecki, B.; Levin, D.B.; Li, J.-S.; Coburn, J.; Ripley, B. Establishing Quality and Safety in Hospital-Based 3D Printing Programs: Patient-First Approach. RadioGraphics 2021, 41, 1208–1229. [Google Scholar] [CrossRef] [PubMed]
- Leng, S.; McGee, K.; Morris, J.; Alexander, A.; Kuhlmann, J.; Vrieze, T.; McCollough, C.H.; Matsumoto, J. Anatomic Modeling Using 3D Printing: Quality Assurance and Optimization. 3D Print. Med. 2017, 3, 6. [Google Scholar] [CrossRef] [PubMed]
- Neely, E.L. The Risks of Revolution: Ethical Dilemmas in 3D Printing from a US Perspective. Sci. Eng. Ethics 2016, 22, 1285–1297. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Szary, J.; Patel, A.; Luis, M.S.; Sabiniewicz, R.; Kwiatkowska, J. Teaching Medical Applications and Workflow of Three-Dimensional Printing to Medical Students: Results of a Pilot Elective Course. Cardiol. J. 2020, 27, 894–896. [Google Scholar] [CrossRef]
- Vozenilek, J.; Huff, J.S.; Reznek, M.; Gordon, J.A. See One, Do One, Teach One: Advanced Technology in Medical Education. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2004, 11, 1149–1154. [Google Scholar] [CrossRef]









| Preprocedural Planning | Procedure Simulation | Professional Education | |
|---|---|---|---|
| Pediatric Cardiac Surgery | [6,7,9] | [5,8] | |
| Pediatric Interventional Cardiology | [11,12,13] | [10,12] | |
| Cardiac Structural Interventions | [14,15,16,20,21,22,23,27,28,29,31,32,33] | [14,17,18,19,30] | [26,27,28,29] |
| Pediatric Surgery | [37,38,39,40,41] | [34,35] | |
| General Surgery | [44,45,46,50,51,52,53,56,57] | [47,49,54] | [48,58,59,60] |
| Orthopedic Surgery | [62,63,64,65,66,122,123] | [61,66,122,123] | |
| Otorhinolaryngology | [77,79,80] | [74,75,76,77,78,81,82,83,84,85] | |
| Head and Neck Surgery | [87,88,89,90,91,92,93,94,95,96,97,98] | [91,92,93,94,95,96,97,98] | [88] |
| Neurosurgery | [101,103,104,105,106,107] | [100] | [100,119,124,125,126,127,128,129,131,132,151] |
| Gynecology and Obstetrics | [110,111,112,113,114,115,120] | [119] | |
| Urology | [127,130] | [124,125,126,127,128,129,131,132] | [131,133] |
| Emergency Medicine and Anesthesiology | [151,154,155,156,157,158] | [151] | [142,143,144,145,146,147,148,149,150,152,153] |
| Radiotherapy | [160,162,163,164,166,168] | [166,168,170,171,172] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meyer-Szary, J.; Luis, M.S.; Mikulski, S.; Patel, A.; Schulz, F.; Tretiakow, D.; Fercho, J.; Jaguszewska, K.; Frankiewicz, M.; Pawłowska, E.; et al. The Role of 3D Printing in Planning Complex Medical Procedures and Training of Medical Professionals—Cross-Sectional Multispecialty Review. Int. J. Environ. Res. Public Health 2022, 19, 3331. https://doi.org/10.3390/ijerph19063331
Meyer-Szary J, Luis MS, Mikulski S, Patel A, Schulz F, Tretiakow D, Fercho J, Jaguszewska K, Frankiewicz M, Pawłowska E, et al. The Role of 3D Printing in Planning Complex Medical Procedures and Training of Medical Professionals—Cross-Sectional Multispecialty Review. International Journal of Environmental Research and Public Health. 2022; 19(6):3331. https://doi.org/10.3390/ijerph19063331
Chicago/Turabian StyleMeyer-Szary, Jarosław, Marlon Souza Luis, Szymon Mikulski, Agastya Patel, Finn Schulz, Dmitry Tretiakow, Justyna Fercho, Kinga Jaguszewska, Mikołaj Frankiewicz, Ewa Pawłowska, and et al. 2022. "The Role of 3D Printing in Planning Complex Medical Procedures and Training of Medical Professionals—Cross-Sectional Multispecialty Review" International Journal of Environmental Research and Public Health 19, no. 6: 3331. https://doi.org/10.3390/ijerph19063331
APA StyleMeyer-Szary, J., Luis, M. S., Mikulski, S., Patel, A., Schulz, F., Tretiakow, D., Fercho, J., Jaguszewska, K., Frankiewicz, M., Pawłowska, E., Targoński, R., Szarpak, Ł., Dądela, K., Sabiniewicz, R., & Kwiatkowska, J. (2022). The Role of 3D Printing in Planning Complex Medical Procedures and Training of Medical Professionals—Cross-Sectional Multispecialty Review. International Journal of Environmental Research and Public Health, 19(6), 3331. https://doi.org/10.3390/ijerph19063331








