Development of Critical Reflection Competency Scale for Clinical Nurses
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Methods
2.2.1. Scale Development
- Concept Definition and Preliminary Item Composition: The concept of critical reflection and the components of the scale were identified through a literature review related to critical reflection and the results of previous research [3] of the content analysis on critical reflection by this research team. The results of the literature review and previous research showed that critical reflection competency is a process of restructuring through connection with prior experiences by contemplating the meaning of experiences in clinical situations. It was found that the factor that promotes critical reflection is the improvement of confidence through open mindedness and positive feedback. Based on the concepts and characteristics derived in this way, a total of 64 preliminary items were constructed to measure critical reflection competency.
- Content Validity: The adequacy of vocabulary and expressions for the 64 preliminary items was checked with the advice of an expert from the National Institute of Korean Language. Content validity was conducted on the 64 items by an eight-member panel of experts, comprising of two nursing professors, and six clinical nurses with experience in critical reflection training. Its validity was evaluated using the content validity index (CVI) according to the criteria that a CVI of 0.78 or higher is appropriate in the case of 6 to 10 experts [28].
- Selection of a Response Format: The Likert scale was used as a response scale for the preliminary items. A scale with less than four categories is too small, and one with more than six is difficult to distinguish [29]. Therefore, in this study, a five-point Likert scale was used, ranging from one point (“not at all”) to five points (“strongly agree”).
2.2.2. Scale Validation
- Sample: The participants of this study were clinical nurses with more than one year of experience working in a medical institution, and the sample was extracted by the convenience sampling method. If the sample size required for factor analysis for construct validity verification is 200 or more, it is evaluated as stable [30]. Based on the evidence that a sample size 3 to 20 times the number of items is appropriate [31], 301 participants were required for the study, considering the dropout rate of 15% based on 256, which is a quadruple of 64 questions. A total of 298 participants responded to the survey, of which the data of 296 were used for the final analysis, as one respondent did not want to participate in the study, and another had less than one year of clinical experience.
- Measures: A preliminary scale derived through this study, a scale for critical thinking disposition [32], and a scale for clinical reasoning competence [33] were used. Critical thinking disposition is the motivation, desire, or attitude to think critically and value critical thinking [32]. The scale for critical thinking disposition is intended to measure the affective domain of critical thinking. Each subfactor had five questions on “intellectual eagerness/curiosity”, four questions on “prudence”, four items on “self-confidence”, three items on “systematicity”, four items on “intellectual fairness”, four items on “healthy skepticism”, and three items on “objectivity”, consisting of a total of 27 items, seven factors, and a five-point Likert scale. At the time of development, the Cronbach’s α was 0.84 [32], and it was 0.77 in this study. For the Korean version of the nurse clinical reasoning competence scale, the Nurse Clinical Reasoning Competence (NCRC) scale, which was developed by Liou et al. [34] and translated into Korean by Joung and Han [33], was used to verify validity and reliability. It consisted of a total of 15 items of one factor on a five-point Likert scale. The Cronbach’s α was 0.93 in the study of Joung and Han [33] and 0.81 in this study.
- Data Collection: An online survey was conducted from 13 September to 1 November 2021. The purpose and method of the study were explained to the nursing department of the institution that provided critical reflection education, and the recruitment document for participants was posted after permission was obtained to collect data. In addition, data were collected by posting recruitment documents on the online community for nurses. Recruitment documents included the purpose and method of the study, the period and procedure for participation, compensation for loss of hours during participation, and the URL of the online questionnaire. The duration of the survey was between 10 and 15 min.
- Data Analysis: Data were analyzed using SPSS/WIN Statistics 27.0, and frequency and percentage, mean and standard deviation were calculated by performing frequency analysis and descriptive statistics for the general characteristics of participants. Item analysis and exploratory factor analysis were performed to verify the construct validity of the scale. For item analysis, the corrected item-to-total correlation coefficient and the change in Cronbach’s α value when an item was deleted were analyzed. A correlation coefficient of less than 0.40 meant that the item had a low degree of discrimination [35]. Further, the sample fit of Kaiser-Meyer-Oklin (KMO) was checked and Bartlett’s sphericity test performed [36] to determine its suitability for factor analysis. As a factor estimation method, an exploratory factor analysis was performed using the principal component analysis method by varimax rotation, which is an orthogonal rotation. According to Kaiser’s rule, the eigenvalue of the sample correlation matrix was set to be 1.0 or more, and the criterion for each factor was 0.40 or more factor loading and 0.30 or more in communality [37]. Furthermore, for the criterion-related validity test of the scale, the correlation between the scale and critical thinking disposition scale and the scale and clinical reasoning competence scale were analyzed using the Pearson correlation coefficient. Critical thinking is an essential element for clinical reasoning, and the two scales can be seen as measuring attributes similar to the critical reflection competency. When the correlation coefficient between tools is calculated as r = 0.40–0.80, it can be considered that the criterion validity of the tool is secured [38]. The testing reliability of the scale and sub-factor scale was confirmed using Cronbach’s α for internal consistency reliability. In addition, reliability was calculated when items were removed, and the extent to which each item represents the concept to be measured was analyzed.
2.3. Ethical Considerations
3. Results
3.1. General Characteristics
3.2. Validity
3.2.1. Content Validity
3.2.2. Construct Validity
- 1.
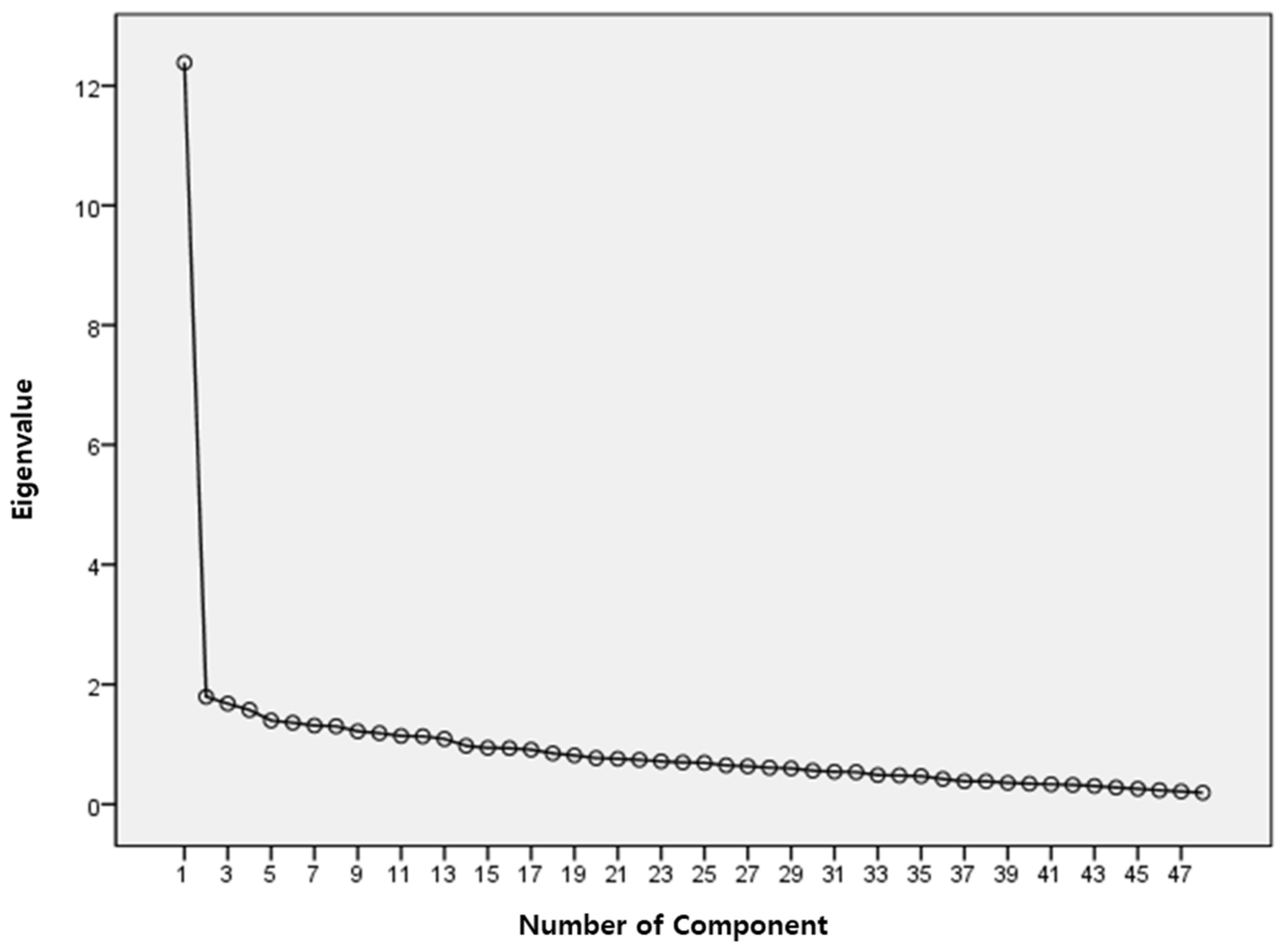
- Exploratory Factor Analysis: Based on the item analysis, the corrected item-to-total correlation coefficient was r = 0.292–0.650. A total of 16 items with a correlation coefficient of less than 0.40 between the items and the total score were deleted, and an exploratory factor analysis was performed on 48 items. KMO and Bartlett’s sphericity test were performed to determine its suitability for factor analysis. In this study, the KMO value was 0.888, which was higher than the standard 0.50 [36]. As per the result of Bartlett’s sphericity test = 5002.958, df = 1128 (<0.001), the null hypothesis was rejected, confirming that the data were suitable for factor analysis. As a result of the first exploratory factor analysis using the principal component analysis method by varimax rotation, the number of factors with eigenvalues greater than or equal to 1.0 was found to be 13. However, as a result of referring to the Scree plot, the slope was found to have changed gently based on factor five. As such, it was judged that five factors would be derived, and the analysis was carried out by fixing the number of factors to five (Figure 1).
- 2.
- Criterion-related Validity: A correlation analysis was conducted between the scores of the critical thinking disposition scale, the clinical reasoning competence scale, and the scale developed in this study. The result of the criterion-related validity analysis showed that the correlation coefficient between the total score of the scale and the total score of the critical reflection competency scale was 0.726, indicating a significant correlation, and the criterion-related validity of the scale was secured (Table 3). The correlation between each sub-factor was found to have a significant correlation, except for the “prudence” factor. It showed a correlation of 0.40 or higher with the factors of “intellectual eagerness/curiosity,” “intellectual fairness,” and “objectivity.” The correlation coefficient between the total score of the scale and the clinical reasoning competence scale’s total score was also significant at 0.774, thus securing the basis for the criterion-related validity of the scale (Table 3). The correlation coefficients between the sub-factors were all above 0.40.
3.3. Reliability
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Klaeson, K.; Berglund, M.; Gustavsson, S. The character of nursing students’ critical reflection at the end of their education. J. Nurs. Educ. Pract. 2017, 7, 55–61. [Google Scholar] [CrossRef]
- Lee, M.; Jang, K. The significance and application of reflective practice in nursing practice. Nurs. Health Issues 2018, 23, 1–8. [Google Scholar]
- Do, J.; Shin, S.; Lee, I.; Jung, Y.; Hong, E.; Lee, M.S. Qualitative content analysis on critical reflection of clinical nurses. J. Qual. Res. 2021, 22, 86–96. [Google Scholar] [CrossRef]
- Shin, S.; Kim, S.H. Experience of novice nurses participating in critical reflection program. J. Qual. Res. 2019, 20, 60–67. [Google Scholar] [CrossRef]
- Scheel, L.S.; Peters, M.D.; Møbjerg, A.C.M. Reflection in the training of nurses in clinical practice settings: A scoping review protocol. JBI Evid. Synth. 2017, 15, 2871–2880. [Google Scholar] [CrossRef]
- Farrington, N.; Townsend, K. Enhancing nurse-patient communication: A critical reflection. Br. J. Nurs. 2014, 23, 771–775. [Google Scholar] [CrossRef]
- Pangh, B.; Jouybari, L.; Vakili, M.A.; Sanagoo, A.; Torik, A. The effect of reflection on nurse-patient communication skills in emergency medical centers. J. Caring Sci. 2019, 8, 75–81. [Google Scholar] [CrossRef]
- Beam, R.J.; O’Brien, R.A.; Neal, M. Reflective practice enhances public health nurse implementation of nurse-family partnership. Public Health Nurs. 2010, 27, 131–139. [Google Scholar] [CrossRef]
- Gregg, S.R.; Twibell, K.R. Try-it-on: Experiential learning of holistic stress management in a graduate nursing curriculum. J. Holist. Nurs. 2016, 34, 300–308. [Google Scholar] [CrossRef]
- Bulman, C.; Lathlean, J.; Gobbi, M. The concept of reflection in nursing: Qualitative findings on student and teacher perspectives. Nurse Educ. Today 2012, 32, 8–13. [Google Scholar] [CrossRef]
- Tashiro, J.; Shimpuku, Y.; Naruse, K.; Matsutani, M. Concept analysis of reflection in nursing professional development. Jpn. J. Nurs. Sci. 2013, 10, 170–179. [Google Scholar] [CrossRef]
- Jang, K.; Kim, H. A study of reflective thinking levels and conditions for reflection affecting on nursing competency in clinical nurses. J. Korean Data Anal. Soc. 2014, 16, 3393–3407. [Google Scholar]
- Bulman, C.; Lathlean, J.; Gobbi, M. The process of teaching and learning about reflection: Research insights from professional nurse education. Stud. High. Educ. 2014, 39, 1219–1236. [Google Scholar] [CrossRef]
- Oyamada, K. Experiences of a critical reflection program for mid-career nurses. Jpn. J. Nurs. Sci. 2012, 9, 9–18. [Google Scholar] [CrossRef]
- Kim, J.Y.; Lee, M. Effect of team-based learning using reflection journal on pregnancy nursing course for nursing students. Korean J. Women Health Nurs. 2018, 24, 404–413. [Google Scholar] [CrossRef]
- Pai, H.C. The effect of a self-reflection and insight program on the nursing competence of nursing students: A longitudinal study. J. Prof. Nurs. 2015, 31, 424–431. [Google Scholar] [CrossRef]
- Ahn, J.H.; Kim, M. Influence of self-reflection and insight, and academic self-efficacy on clinical reasoning competence among nursing students. J. East-West Nurs. Res. 2020, 26, 176–184. [Google Scholar] [CrossRef]
- Silvia, B.; Valerio, D.; Lorenza, G. The reflective journal: A tool for enhancing experience-based learning in nursing students in clinical practice. J. Nurs. Educ. Pract. 2013, 3, 102–111. [Google Scholar] [CrossRef]
- Jho, M.Y. Effects of writing reflective journal on meta-cognition and problem solving ability in nursing students taking a fundamental nursing skills course applying blended learning. J. Korean Acad. Fundam. Nurs. 2016, 23, 430–439. [Google Scholar] [CrossRef]
- Grant, A.M.; Franklin, J.; Langford, P. The self-reflection and insight scale: A new measure of private self-consciousness. Soc. Behav. Personal. Int. J. 2002, 30, 821–835. [Google Scholar] [CrossRef]
- Kember, D.; Leung, D.Y.; Jones, A.; Loke, A.Y.; McKay, J.; Sinclair, K.; Yeung, E. Development of a questionnaire to measure the level of reflective thinking. Assess. Eval. High. Educ. 2000, 25, 381–395. [Google Scholar] [CrossRef]
- Peltier, J.W.; Hay, A.; Drago, W. The reflective learning continuum: Reflecting on reflection. J. Mark. Educ. 2005, 27, 250–263. [Google Scholar] [CrossRef]
- Van Woerkom, M.; Croon, M. Operationalising critically reflective work behaviour. Pers. Rev. 2008, 37, 317–331. [Google Scholar] [CrossRef]
- Kuennen, J.K. Critical reflection: A transformative learning process integrating theory and evidence-based practice. Worldviews Evid.-Based Nurs. 2015, 12, 306–308. [Google Scholar] [CrossRef]
- Lundgren, H.; Poell, R.F. On critical reflection: A review of Mezirow’s theory and its operationalization. Hum. Resour. Dev. Rev. 2016, 15, 3–28. [Google Scholar] [CrossRef]
- Lee, M.; Jang, K. Reflection-related research in Korean nursing: A literature review. J. Korean Acad. Nurs. Adm. 2019, 25, 83–96. [Google Scholar] [CrossRef]
- Song, M.O.; Kim, H. Validity and reliability of the self-reflection and insight scale for Korean nursing students. J. Korean Acad. Fundam. Nurs. 2018, 25, 11–21. [Google Scholar] [CrossRef][Green Version]
- Polit, D.F.; Beck, C.T.; Owen, S.V. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res. Nurs. Health 2007, 30, 459–467. [Google Scholar] [CrossRef]
- Fayers, P.M.; Machin, D. Quality of Life: The Assessment, Analysis and Interpretation of Patient–Reported Outcomes; John Wiley & Sons: Hoboken, NJ, USA, 2013. [Google Scholar]
- Kang, H. A guide on the use of factor analysis in the assessment of construct validity. J. Korean Acad. Nurs. 2013, 43, 587–594. [Google Scholar] [CrossRef]
- Mundfrom, D.J.; Shaw, D.G.; Ke, T.L. Minimum sample size recommendations for conducting factor analyses. Int. J. Test. 2005, 5, 159–168. [Google Scholar] [CrossRef]
- Yoon, J. Development of an Instrument for the Measurement of Critical Thinking Disposition. Master’s Thesis, Catholic University, Seoul, Korea, 2004. [Google Scholar]
- Joung, J.; Han, J.W. Validity and reliability of a Korean version of nurse clinical reasoning competence scale. J. Korea Acad.-Ind. Coop. Soc. 2017, 18, 304–310. [Google Scholar] [CrossRef]
- Liou, S.R.; Liu, H.C.; Tsai, H.M.; Tsai, Y.H.; Lin, Y.C.; Chang, C.H.; Cheng, C.Y. The development and psychometric testing of a theory-based instrument to evaluate nurses’perception of clinical reasoning competence. J. Adv. Nurs. 2016, 72, 707–717. [Google Scholar] [CrossRef] [PubMed]
- Gliem, J.A.; Gliem, R.R. Calculating, interpreting, and reporting Cronbach’s alpha reliability coefficient for Likert-type scales. Midwest Res.-Pract. Conf. Adult Contin. Community Educ. 2003, 82–88. Available online: https://scholarworks.iupui.edu/handle/1805/344 (accessed on 23 January 2022).
- Kaiser, H.F. An index of factorial simplicity. Psychometrika 1974, 39, 31–36. [Google Scholar] [CrossRef]
- Hair, J.F. Multivariate Data Analysis with Readings, 4th ed.; Prentice-Hall: Hoboken, NJ, USA, 1995. [Google Scholar]
- Lee, K.; Shin, S. Validity of instrument development research in Korean nursing research. J. Korean Acad. Nurs. 2013, 43, 697–703. [Google Scholar] [CrossRef]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Zori, S. Teaching critical thinking using reflective journaling in a nursing fellowship program. J. Contin. Educ. Nurs. 2016, 47, 321–329. [Google Scholar] [CrossRef]
- Zhang, C.; Fan, H.; Xia, J.; Guo, H.; Jiang, X.; Yan, Y. The effects of reflective training on the disposition of critical thinking for nursing students in China: A controlled trial. Asian Nurs. Res. 2017, 11, 194–200. [Google Scholar] [CrossRef]
- Chen, F.F.; Chen, S.Y.; Pai, H.C. Self-reflection and critical thinking: The influence of professional qualifications on registered nurses. Contemp. Nurse 2019, 55, 59–70. [Google Scholar] [CrossRef]
- Yi, J.; Park, M. Nurses’ access & use of information resources and barriers & competency of evidence based practice. Korean J. Adult Nurs. 2011, 23, 255–266. [Google Scholar]
- Berthelsen, C.; Hølge-Hazelton, B. The Importance of context and organization culture in the understanding of nurses’ barriers against research utilization: A systematic review. Worldviews Evid.-Based Nurs. 2021, 18, 111–117. [Google Scholar] [CrossRef]
- Kim, J.; Lee, J. The experience of clinical nurses’ interpersonal conflict. J. Qual. Res. 2013, 14, 70–80. [Google Scholar]
- Kwon, S.; Ahn, H.; Kwak, M.; Yun, S. Conflicts experienced by the nurses in hospital nursing organizations. J. Korean Acad. Nurs. Adm. 2019, 25, 499–509. [Google Scholar] [CrossRef]
- Aukes, L.C.; Geertsma, J.; Cohen-Schotanus, J.; Zwierstra, R.P.; Slaets, J.P. The development of a scale to measure personal reflection in medical practice and education. Med. Teach. 2007, 29, 177–182. [Google Scholar] [CrossRef]
- Miraglia, R.; Asselin, M.E. Reflection as an educational strategy in nursing professional development: An integrative review. J. Nurses Prof. Dev. 2015, 31, 62–72. [Google Scholar] [CrossRef]
| Variable | Category | n | % | Median | M ± SD |
|---|---|---|---|---|---|
| Gender | Female | 284 | 95.9 | ||
| Male | 12 | 4.1 | |||
| Age (years) | 20–29 | 74 | 25.0 | 33.13 ± 4.92 | |
| 30–39 | 188 | 63.5 | 33 | ||
| 40≤ | 34 | 11.5 | |||
| Education | Associate | 11 | 3.7 | ||
| Bachelor | 222 | 75.0 | |||
| Master or more | 63 | 21.3 | |||
| Clinical experience (years) | <3 | 37 | 12.5 | 94.86 ± 64.95 (months) | |
| 3–5 | 70 | 23.6 | |||
| 6–9 | 111 | 37.5 | |||
| 10≤ | 78 | 26.4 | |||
| Experiences with critical reflection education | Yes | 85 | 28.7 | ||
| No | 211 | 71.3 | |||
| Experiences with using cases of critical reflection in clinical practice (n = 85) | Yes | 69 | 81.2 | ||
| No | 16 | 18.8 |
| No | Items | Communality | Factor Loading | ||||
|---|---|---|---|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | |||
| 1 | I apply what I have learned from experience to future work situations. | 0.593 | 0.722 | 0.151 | 0.016 | 0.119 | 0.188 |
| 2 | I think about the nursing care that I will be providing before I actually provide it. | 0.657 | 0.709 | 0.165 | 0.052 | 0.275 | 0.222 |
| 3 | I think about what I can do for patients in addition to my assigned tasks. | 0.594 | 0.612 | 0.324 | 0.172 | 0.241 | 0.161 |
| 4 | I respect other people’s opinions that are different from mine. | 0.593 | 0.587 | −0.062 | 0.484 | −0.097 | −0.035 |
| 5 | I think deeply about what I find important about my work. | 0.573 | −0.038 | 0.734 | 0.093 | 0.085 | 0.128 |
| 6 | I implement nursing care while keeping its purpose in mind. | 0.523 | 0.154 | 0.683 | 0.052 | 0.166 | 0.054 |
| 7 | I look at the bigger picture when dealing with patients, rather than focusing on individual tasks. | 0.409 | 0.161 | 0.543 | 0.241 | 0.173 | −0.007 |
| 8 | I look back on the tasks I have carried out and identify things I did well and things I did badly. | 0.469 | 0.252 | 0.494 | 0.186 | −0.105 | 0.340 |
| 9 | I ask questions about things I do not know, and endeavor to solve them myself. | 0.369 | 0.367 | 0.455 | 0.004 | 0.090 | 0.136 |
| 10 | I give meaning to nursing work and feel rewarded for it. | 0.564 | 0.131 | 0.264 | 0.684 | 0.075 | 0.060 |
| 11 | I understand my strengths and weaknesses as a nurse. | 0.567 | −0.076 | 0.106 | 0.667 | 0.273 | 0.174 |
| 12 | When a problem occurs, I identify the cause. | 0.426 | 0.358 | 0.135 | 0.490 | 0.104 | 0.172 |
| 13 | I make efforts to apply the work-related knowledge that I have learned to my nursing practice. | 0.500 | 0.108 | 0.143 | 0.052 | 0.670 | 0.127 |
| 14 | I listen to other people’s opinions. | 0.475 | 0.097 | 0.098 | 0.298 | 0.606 | −0.002 |
| 15 | I acknowledge the need for me to change in the interest of self-development. | 0.606 | 0.089 | 0.072 | −0.068 | 0.579 | 0.503 |
| 16 | When a problematic situation arises, I try to identify the behavior that caused the problem. | 0.514 | 0.403 | 0.136 | 0.174 | 0.543 | −0.089 |
| 17 | I look back on the nursing care that I provide based on my experiences. | 0.625 | 0.107 | 0.269 | 0.209 | −0.060 | 0.703 |
| 18 | I think about the reason for the importance of nursing care implemented in the line of duty based on evidence. | 0.665 | 0.194 | −0.180 | 0.397 | 0.184 | 0.635 |
| 19 | I think specifically about the outcomes of nursing care. | 0.351 | 0.198 | 0.261 | −0.046 | 0.160 | 0.465 |
| Eigenvalue | 5.29 | 1.36 | 1.19 | 1.63 | 1.07 | ||
| Explained variance (%) | 27.86 | 7.16 | 6.26 | 6.12 | 5.62 | ||
| Cumulative explained variance (%) | 53.02 | ||||||
| Critical Reflection Competency | |||||||
|---|---|---|---|---|---|---|---|
| Total | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | ||
| Critical thinking disposition | Total | 0.726 ** | 0.539 ** | 0.606 ** | 0.511 ** | 0.505 ** | 0.531 ** |
| Intellectual eagerness/ curiosity | 0.657 ** | 0.471 ** | 0.558 ** | 0.411 ** | 0.458 ** | 0.538 ** | |
| Prudence | 0.046 | 0.010 | 0.060 | 0.047 | 0.026 | 0.027 | |
| Self- confidence | 0.480 ** | 0.353 ** | 0.446 ** | 0.320 ** | 0.300 ** | 0.346 ** | |
| Systematicity | 0.330 ** | 0.255 ** | 0.270 ** | 0.241 ** | 0.245 ** | 0.211 ** | |
| Intellectual fairness | 0.664 ** | 0.537 ** | 0.509 ** | 0.523 ** | 0.481 ** | 0.411 ** | |
| Healthy skepticism | 0.416 ** | 0.305 ** | 0.356 ** | 0.256 ** | 0.283 ** | 0.339 ** | |
| Objectivity | 0.607 ** | 0.446 ** | 0.459 ** | 0.478 ** | 0.435 ** | 0.452 ** | |
| Clinical reasoning competence | Total | 0.774 ** | 0.623 ** | 0.608 ** | 0.558 ** | 0.545 ** | 0.535 ** |
| Factors | No. of Items | Cronbach’s α |
|---|---|---|
| Factor 1 | 4 | 0.738 |
| Factor 2 | 5 | 0.670 |
| Factor 3 | 3 | 0.572 |
| Factor 4 | 4 | 0.607 |
| Factor 5 | 3 | 0.515 |
| Total | 19 | 0.853 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, S.; Hong, E.; Do, J.; Lee, M.S.; Jung, Y.; Lee, I. Development of Critical Reflection Competency Scale for Clinical Nurses. Int. J. Environ. Res. Public Health 2022, 19, 3483. https://doi.org/10.3390/ijerph19063483
Shin S, Hong E, Do J, Lee MS, Jung Y, Lee I. Development of Critical Reflection Competency Scale for Clinical Nurses. International Journal of Environmental Research and Public Health. 2022; 19(6):3483. https://doi.org/10.3390/ijerph19063483
Chicago/Turabian StyleShin, Sujin, Eunmin Hong, Jiyoung Do, Mee Sun Lee, Youngsun Jung, and Inyoung Lee. 2022. "Development of Critical Reflection Competency Scale for Clinical Nurses" International Journal of Environmental Research and Public Health 19, no. 6: 3483. https://doi.org/10.3390/ijerph19063483
APA StyleShin, S., Hong, E., Do, J., Lee, M. S., Jung, Y., & Lee, I. (2022). Development of Critical Reflection Competency Scale for Clinical Nurses. International Journal of Environmental Research and Public Health, 19(6), 3483. https://doi.org/10.3390/ijerph19063483






