Implementing School-Based Mental Health Services: A Scoping Review of the Literature Summarizing the Factors That Affect Implementation
Abstract
:1. Background
2. Mental Health Services Provided in Schools
3. Aim of the Review
4. Method
4.1. Study Design
4.2. Identify Relevant Studies
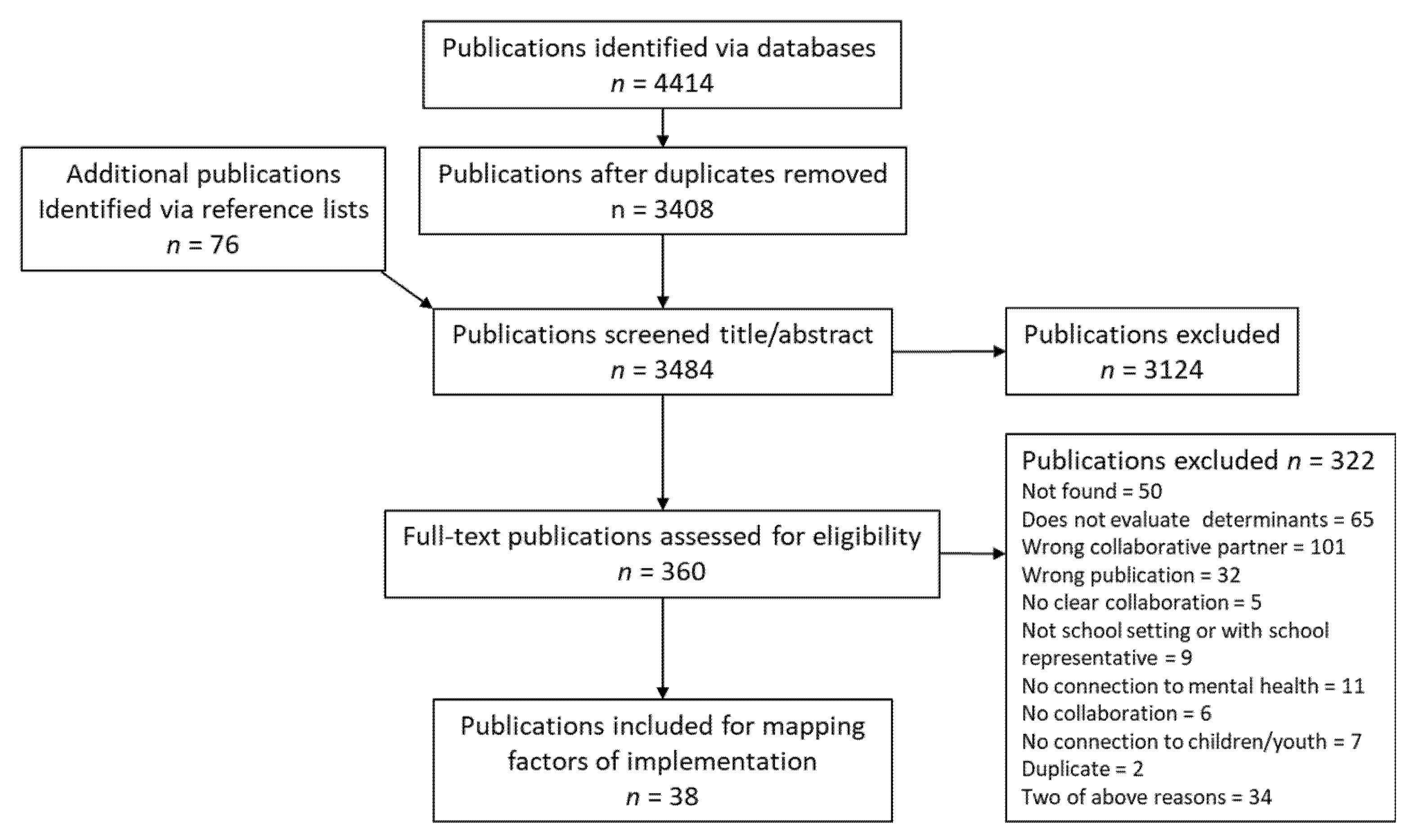
4.3. Select Studies
4.4. Chart Data
5. Results
5.1. Included Studies
5.2. Study Characteristics
5.3. Implementation Factors
6. Discussion
6.1. Adapting of the Interventions
6.2. Internal Collaboration and between Actors
6.3. Implications for Implementing SBMHS
7. Limitations
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Search Strategy
Appendix A.1. Medline
| Interface: Ovid MEDLINE(R) and Epub Ahead of Print, In-Process and Other Non-Indexed Citations and Daily Date of Search: 5 May 2019 Number of hits: 1095 Comment: In Ovid, two or more words are automatically searched as phrases; i.e., no quotation marks are needed | Field labels exp/= exploded MeSH term /= non exploded MeSH term .ti,ab,kf. = title, abstract and author keywords adjx = within x words, regardless of order * = truncation of word for alternate endings |
| |
Appendix A.2. Web of Science Core Collection
| Interface: Clarivate Analytics Date of Search: 3 May 2019 Number of hits: 850 | Field labels TS/TOPIC = title, abstract, author keywords and Keywords Plus NEAR/x = within x words, regardless of order * = truncation of word for alternate endings |
| |
Appendix A.3. Psycinfo
| Interface: Ovid Date of Search: 3 May 2019 Number of hits: 1238 Comment: In Ovid, two or more words are automatically searched as phrases; i.e., no quotation marks are needed | Field labels exp/= exploded controlled term /= non exploded controlled term .ti,ab,id. = title, abstract and author keywords adjx = within x words, regardless of order * = truncation of word for alternate endings |
| |
Appendix A.4. ERIC
| Interface: ProQuest Date of Search: 3 May 2019 Number of hits: 1231 | Field labels MAINSUBJECT.EXACT.EXPLODE = exploded subject heading MAINSUBJECT.EXACT non exploded subject heading TI,AB = title, abstract N/x = within x words, regardless of order * = truncation of word for alternate endings |
| (MAINSUBJECT.EXACT(“Mental Health” OR “Mental Disorders” OR “Psychopathology” OR “Adjustment (to Environment)” OR “Affective Behavior” OR “Depression (Psychology)” OR “Anxiety” OR “Fear” OR “Eating Disorders” OR “Aggression” OR “Sleep” OR “Pain” OR “Hyperactivity” OR “Social Problems” OR “Delinquency” OR “Antisocial Behavior” OR “Quality of Life” OR “Well Being” OR “Wellness” OR “Life Satisfaction” OR “Psychological Patterns” OR “Resilience (Psychology)”) OR MAINSUBJECT.EXACT. EXPLODE(“Anxiety Disorders” OR “Self Destructive Behavior” OR “Emotional Disturbances” OR “Attention Deficit Disorders” OR “Behavior Disorders” OR “Substance Abuse” OR “Self Concept”) OR TI,AB((mental OR emotional OR psychiatric OR psychologic*) N/3 (disease* OR disorder* OR distress OR health OR illness* OR “ill health” OR illhealth OR instabilit* OR problem* OR symptom*))) AND (TI,AB((classroom* OR highschool* OR pupil* OR school* OR teacher*) N/3 (based OR environment* OR intervent* OR implement* OR setting* OR elementary or high or middle or primary or secondary)) OR (MAINSUBJECT.EXACT.EXPLODE (“Students” OR “Schools”) OR MAINSUBJECT.EXACT(“Educational Environment” OR “Classroom Environment” OR “School Health Services” OR “School Nurses” OR “Ancillary School Services”) )) AND ((MAINSUBJECT.EXACT(“Interprofessional Relationship” OR “Interdisciplinary Approach”) OR MAINSUBJECT.EXACT.EXPLODE(“Cooperation”)) OR TI,AB(collaborat* OR coordinat* OR cooperat* OR partnership* OR teamwork) OR TI,AB((“cross-disciplinar*” OR interagency* OR interdisciplinar* OR intersectoral* OR interinstitutional* OR interprofessional* OR multidisciplinar*) N/6 (care OR communicat* OR “health care” OR intervention* OR “mental health” OR program* OR relation* OR team* OR strateg*))) AND (MAINSUBJECT.EXACT(“Child Welfare” OR “Health Services” OR “Community Health Services” OR “Clinics” OR “Psychoeducational Clinics” OR “Psychiatric Services” OR “Psychological Services” OR “Social Work” OR “Primary Health Care”) OR TI,AB((emergenc* OR health OR psychiat* OR psycholog*) N/3 (care OR nursing OR practice* OR service*)) OR TI,AB(healthcare OR “mental health center*” OR “mental health clinic*” OR “mental health rehabilitation” OR “primary care” OR “psycho* rehabilitation” OR “social service*” OR “social work*” OR support* OR treat*)) AND (MAINSUBJECT.EXACT(“Program Evaluation” OR “Program Effectiveness” OR “Program Development” OR “Program Implementation” OR “Mental Health Programs”) OR TI,AB(barrier* OR determinant* OR effect* OR evaluat* OR facilitat* OR factor* OR implement* OR intervent* OR predict* OR program*)) Applied filters: Scholarly Journals OR Reports OR Dissertations and Theses | |
Appendix B. Eligibility Criteria
| Study Focus/Content | Inclusion Criteria | Exclusion Criteria |
| Implementationof the intervention | Studies that describe:
| Studies that describe:
|
| The Interventions |
|
|
| Collaborative partners |
|
|
| Arena of the intervention |
|
|
| Target group |
|
|
| Problem |
|
|
| Language |
| |
| Type of publication |
|
|
References
- Public Health Agency of Sweden. Skolans Betydelse för Inåtvända Psykiska Problem Bland Skolbarn; Public Health Agency of Sweden: Solna, Sweden, 2020. [Google Scholar]
- Becker, B.E.; Luthar, S.S. Social-Emotional Factors Affecting Achievement Outcomes Among Disadvantaged Students: Closing the Achievement Gap. Educ. Psychol. 2002, 37, 197–214. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Caring for Children and Adolescents with Mental Disorders: Setting WHO Directions; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- Olfson, M.; Blanco, C.; Wang, S.; Laje, G.; Correll, C.U. National trends in the mental health care of children, adolescents, and adults by office-based physicians. JAMA Psychiatry 2014, 71, 81–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rutter, M.; Moffitt, T.E.; Caspi, A. Gene-environment interplay and psychopathology: Multiple varieties but real effects. J. Child Psychol. Psychiatry Allied Discip. 2006, 47, 226–261. [Google Scholar] [CrossRef] [PubMed]
- Brooks, T.L.; Harris, S.K.; Thrall, J.S.; Woods, E.R. Association of adolescent risk behaviors with mental health symptoms in high school students. J. Adolesc. Health 2002, 31, 240–246. [Google Scholar] [CrossRef]
- Cicchetti, D.; Rogosch, F.A. A developmental psychopathology perspective on adolescence. J. Consult. Clin. Psychol. 2002, 70, 6–20. [Google Scholar] [CrossRef]
- Halfon, N.; Newacheck, P.W. Prevalence and impact of parent-reported disabling mental health conditions among U.S. children. J. Am. Acad. Child Adolesc. Psychiatry 1999, 38, 600–603. [Google Scholar] [CrossRef]
- Chisholm, D.; Sweeny, K.; Sheehan, P.; Rasmussen, B.; Smit, F.; Cuijpers, P.; Saxena, S. Scaling-up treatment of depression and anxiety: A global return on investment analysis. Lancet Psychiatry 2016, 3, 415–424. [Google Scholar] [CrossRef] [Green Version]
- Sallee, C.M.; Agemy, E.M. Costs and Benefits of Investing in Mental Health Services in Michigan; Anderson Economic Group: East Lansing, MI, USA, 2011; Volume 11, pp. 1–33. [Google Scholar]
- Lean, D.S.; Colucci, V.A. Barriers to Learning: The Case for Integrated Mental Health Services in Schools; Rowman Littlefield Education: Washington, WA, USA, 2010. [Google Scholar]
- Stallard, P. Promoting Children’s Well-Being. In Child Psychology and Psychiatry: Frameworks for Practice, 2nd ed.; Skuse, D., Bruce, H., Dowdney, L., Mrazek, D., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2011; pp. 72–77. [Google Scholar] [CrossRef]
- Kim-Cohen, J.; Caspi, A.; Moffitt, T.E.; Harrington, H.; Milne, B.J.; Poulton, R. Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Arch. Gen. Psychiatry 2003, 60, 709–717. [Google Scholar] [CrossRef]
- Kessler, R.C.; Avenevoli, S.; Costello, J.; Green, J.G.; Gruber, M.J.; McLaughlin, K.A.; Petukhova, M.; Sampson, N.A.; Zaslavsky, A.M.; Merikangas, K.R. Severity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Arch. Gen. Psychiatry 2012, 69, 381–389. [Google Scholar] [CrossRef] [Green Version]
- National Research Council. Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities; O’Connell, M.E., Boat, T., Warner, K.E., Eds.; National Research Council: Washington, WA, USA, 2009. [Google Scholar] [CrossRef]
- Dalsgaard, S.; McGrath, J.; Østergaard, S.D.; Wray, N.R.; Pedersen, C.B.; Mortensen, P.B.; Petersen, L. Association of Mental Disorder in Childhood and Adolescence with Subsequent Educational Achievement. JAMA Psychiatry 2020, 77, 797–805. [Google Scholar] [CrossRef]
- Durlak, J.; Weissberg, R.; Dymnicki, A.B.; Taylor, R.D.; Schellinger, K. The impact of enhancing students’ social and emotional learning: A meta-analysis of school-based universal interventions. Child Dev. 2011, 82, 405–432. [Google Scholar] [CrossRef]
- Weist, M.D.; Evans, S.W. Expanded School Mental Health: Challenges and Opportunities in an Emerging Field. J. Youth Adolesc. 2005, 34, 3–4. [Google Scholar] [CrossRef]
- Doll, B.; Nastasi, B.K.; Cornell, L.; Song, S.Y. School-Based Mental Health Services: Definitions and Models of Effective Practice. J. Appl. Sch. Psychol. 2017, 33, 179–194. [Google Scholar] [CrossRef]
- Rones, M.; Hoagwood, K. School-Based Mental Health Services: A Research Review. Clin. Child Fam. Psychol. Rev. 2000, 3, 223–241. [Google Scholar] [CrossRef] [PubMed]
- Kauffman, J.M. Characteristics of Emotional and Behavioral Disorders of Children and Youth, 7th ed.; Merrill/Prentice Hall: New Jersey, NJ, UAS, 2001. [Google Scholar]
- Langer, D.A.; Wood, J.J.; Wood, P.A.; Garland, A.F.; Landsverk, J.; Hough, R.L. Mental Health Service Use in Schools and Non-school-Based Outpatient Settings: Comparing Predictors of Service Use. Sch. Ment. Health 2015, 7, 161–173. [Google Scholar] [CrossRef]
- Merikangas, K.R.; He, J.; Burstein, M.; Swendsen, J.; Avenevoli, S.; Case, B.; Georgiades, K.; Heaton, L.; Swanson, S.; Olfson, M. Service utilization for lifetime mental disorders in U.S. adolescents: Results of the National Comorbidity Survey-Adolescent Supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 2011, 50, 32–45. [Google Scholar] [CrossRef] [Green Version]
- Armbruster, P.; Fallon, T. Clinical, sociodemographic, and systems risk factors for attrition in a children’s mental health clinic. Am. J. Orthopsychiatry 1994, 64, 577–585. [Google Scholar] [CrossRef]
- McKay, M.M.; Pennington, J.; Lynn, C.J.; McCadam, K. Understanding urban child mental health service use: Two studies of child, family, and environmental correlates. J. Behav. Health Serv. Res. 2001, 28, 475–483. [Google Scholar] [CrossRef]
- Committee on School Health. School-Based Mental Health Services. Pediatrics 2004, 113, 1839–1845. [Google Scholar] [CrossRef] [Green Version]
- Hoagwood, K.; Erwin, H.D. Effectiveness of School-Based Mental Health Services for Children: A 10-Year Research Review. J. Child Fam. Stud. 1997, 6, 435–451. [Google Scholar] [CrossRef]
- Bonell, C.; Allen, E.; Warren, E.; McGowan, J.; Bevilacqua, L.; Jamal, F.; Legood, R.; Wiggins, M.; Opondo, C.; Mathiot, A.; et al. Effects of the Learning Together intervention on bullying and aggression in English secondary schools (INCLUSIVE): A cluster randomised controlled trial. Lancet 2018, 392, 2452–2464. [Google Scholar] [CrossRef] [Green Version]
- Shinde, S.; Weiss, H.A.; Varghese, B.; Khandeparkar, P.; Pereira, B.; Sharma, A.; Gupta, R.; Ross, D.A.; Patton, G.; Patel, V. Promoting school climate and health outcomes with the SEHER multi-component secondary school intervention in Bihar, India: A cluster-randomised controlled trial. Lancet 2018, 392, 2465–2477. [Google Scholar] [CrossRef]
- Caldwell, D.M.; Davies, S.R.; Hetrick, S.E.; Palmer, J.C.; Caro, P.; López-López, J.A.; Gunnell, D.; Kidger, J.; Thomas, J.; French, C.; et al. School-based interventions to prevent anxiety and depression in children and young people: A systematic review and network meta-analysis. Lancet Psychiatry 2019, 6, 1011–1020. [Google Scholar] [CrossRef] [Green Version]
- Fazel, M.; Kohrt, B.A. Prevention versus intervention in school mental health. Lancet Psychiatry 2019, 6, 969–971. [Google Scholar] [CrossRef] [Green Version]
- Mohamed, N.E.; Sutan, R.; Abd Rahim, M.A.; Mokhtar, D.; Rahman, R.; Johani, F.; Abd Majid, M.S.; Mohd Fauzi, M.F.; Azme, M.; Mat Saruan, N.; et al. Systematic Review of School-Based Mental Health Intervention among Primary School Children. J. Community Med. Health Educ. 2018, 8, 1–6. [Google Scholar] [CrossRef]
- Sanchez, A.L.; Cornacchio, D.; Poznanski, B.; Golik, A.M.; Chou, T.; Comer, J.S. The Effectiveness of School-Based Mental Health Services for Elementary-Aged Children: A Meta-Analysis. J. Am. Acad. Child Adolesc. Psychiatry 2018, 57, 153–165. [Google Scholar] [CrossRef] [PubMed]
- Arenson, M.; Hudson, P.J.; Lee, N.; Lai, B. The Evidence on School-Based Health Centers: A Review. Glob. Pediatric Health 2019, 6, 2333794X19828745. [Google Scholar] [CrossRef]
- Lipsey, M.; Crosse, S.; Dunkle, J.; Pollard, J.; Stobart, G. Evaluation: The state of the art and the sorry state of the science. New Dir. Program Eval. 1985, 1985, 7–28. [Google Scholar] [CrossRef]
- Kern, L.; Mathur, S.R.; Albrecht, S.F.; Poland, S.; Rozalski, M.; Skiba, R.J. The Need for School-Based Mental Health Services and Recommendations for Implementation. Sch. Ment. Health 2017, 9, 205–217. [Google Scholar] [CrossRef]
- O’Brien, K.K.; Colquhoun, H.; Levac, D.; Baxter, L.; Tricco, A.C.; Straus, S.; Wickerson, L.; Nayar, A.; Moher, D.; O’Malley, L. Advancing scoping study methodology: A web-based survey and consultation of perceptions on terminology, definition and methodological steps. BMC Health Serv. Res. 2016, 16, 305. [Google Scholar] [CrossRef] [Green Version]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- SOU (1998:31); It Focuses on Life: Supporting and Caring for Children and Adolescents with Mental Health Problems. Final Report of the Committee on Child Psychiatry. National Public Inquiry 31. Ministry of Cities: Stockholm, Sweden, 1998.
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 2009, 4, 50. [Google Scholar] [CrossRef] [Green Version]
- Anderson-Butcher, D.; Iachini, A.L.; Ball, A.; Barke, S.; Martin, L.D. A University-School Partnership to Examine the Adoption and Implementation of the Ohio Community Collaboration Model in One Urban School District: A Mixed-Method Case Study. J. Educ. Stud. Placed Risk JESPAR 2016, 21, 190–204. [Google Scholar] [CrossRef]
- Atkins, M.S.; Frazier, S.L.; Leathers, S.J.; Graczyk, P.A.; Talbott, E.; Jakobsons, L.; Adil, J.A.; Marinez-Lora, A.; Demirtas, H.; Gibbons, R.B.; et al. Teacher Key Opinion Leaders and Mental Health Consultation in Low-Income Urban Schools. J. Consult. Clin. Psychol. 2008, 76, 905–908. [Google Scholar] [CrossRef] [PubMed]
- Axberg, U.; Hansson, K.; Broberg, A.G.; Wirtberg, I. The Development of a Systemic School-Based Intervention: Marte Meo and Coordination Meetings. Fam. Process 2006, 45, 375–389. [Google Scholar] [CrossRef] [PubMed]
- Baxendale, J.; Lockton, E.; Adams, C.; Gaile, J. Parent and Teacher Perceptions of Participation and Outcomes in an Intensive Communication Intervention for Children with Pragmatic Language Impairment. Int. J. Lang. Commun. Disord. 2013, 48, 41–53. [Google Scholar] [CrossRef]
- Bellinger, S.A.; Lee, S.W.; Jamison, T.R.; Reese, R.M.; Bellinger, S.A.; Lee, S.W.; Jamison, T.R.; Reese, R.M.; Bellinger, S.A.; Lee, S.W.; et al. Conjoint Behavioral Consultation: Community-School Collaboration and Behavioral Outcomes Using Multiple Baseline Conjoint Behavioral Consultation: Community-School Baseline. J. Educ. Psychol. Consult. 2016, 26, 139–165. [Google Scholar] [CrossRef]
- Bhatara, V.S.; Vogt, H.B.; Patrick, S. Acceptability of a Web-based Attention-deficit/Hyperactivity Disorder Scale (T-SKAMP) by Teachers: A Pilot Study. J. Am. Board Fam. Med. 2006, 19, 195–200. [Google Scholar] [CrossRef] [Green Version]
- Bruns, E.J.; Walrath, C.; Glass-Siegel, M.; Weist, M.D. School-based mental health services in Baltimore: Association with school climate and special education referrals. Behav. Modif. 2004, 28, 491–512. [Google Scholar] [CrossRef]
- Capp, G. Our Community, Our Schools: A Case Study of Program Design for School-Based Mental Health Services. Child. Sch. 2015, 37, 241–248. [Google Scholar] [CrossRef]
- Clarke, M.; Coombs, C.; Walton, L. School Based Early Identi¢cation and Intervention Service for Adolescents: A Psychology and School Nurse Partnership Model. Child Adolesc. Ment. Health 2003, 8, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Fazel, M.; Doll, H.; Stein, A. A school-based mental health intervention for refugee children: An exploratory study. Clin. Child Psychol. Psychiatry 2009, 14, 297–309. [Google Scholar] [CrossRef]
- Fiester, L.; Nathanson, S. Healing Fractured Lives: How Three School-Based Projects Approach Violence Prevention and Mental Health Care. 1996. Available online: https://files.eric.ed.gov/fulltext/ED408542.pdf (accessed on 10 February 2022).
- Foy, J.M.; Earls, M.F. A Process for Developing Community Consensus Regarding the Diagnosis and Management of Attention- Deficit/Hyperactivity Disorder. Pediatrics 2005, 17, 84–97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goodwin, T.; Pacey, K.; Grace, M. Childreach: Violence Prevention in Preschool Settings. J. Child Adolesc. Psychiatr. Nurs. 2003, 16, 55–59. [Google Scholar] [CrossRef]
- Hunter, A.; Playle, J.; Sanchez, P.; Cahill, J. Introduction of a child and adolescent mental health link worker: Education and health staff focus. J. Psychiatr. Ment. Health Nurs. 2008, 15, 670–677. [Google Scholar] [CrossRef]
- Jaatinen, P.T.; Erkolahti, R.; Asikainen, P. Networking family counselling services. Developing psychosocial support for school children. J. Interprof. Care 2005, 19, 294–295. [Google Scholar] [CrossRef]
- Jennings, J.; Pearson, G.; Harris, M. Implementing and Maintaining School-Based Mental Health Services in a large, Urban School District. J. Sch. Health 2000, 70, 201–205. [Google Scholar] [CrossRef]
- Juszczak, L.; Melinkovich, P.; Kaplan, D. Use of health and mental health services by adolescents across multiple delivery sites. J. Adolesc. Health 2003, 32, 108–118. [Google Scholar] [CrossRef]
- Khan, R.J.; Bedford, K.; Williams, M. Evaluation of the MindMatters buddy support scheme in achievements and challenges. Health Educ. J. 2011, 71, 320–326. [Google Scholar] [CrossRef]
- Kutcher, S.; Wei, Y. Mental health and the school environment: Secondary schools, promotion and pathways to care. Curr. Opin. Psychiatry 2012, 25, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Li-Grining, C.P.; Raver, C.C.; Jones-Lewis, D.; Madison-Boyd, S.; Lennon, J. Targeting classrooms’ emotional climate and preschoolers’ socioemotional adjustment: Implementation of the Chicago School Readiness Project. J. Prev. Interv. Community 2014, 42, 264–281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maddern, L.; Franey, J.; Mclaughlin, V.; Cox, S.; Maddern, L.; Franey, J.; Mclaughlin, V.; Cox, S.; Maddern, L.; Franey, J.; et al. An evaluation of the impact of an inter-agency intervention programme to promote social skills in primary school children. Educ. Psychol. Pract. 2004, 20, 135–155. [Google Scholar] [CrossRef]
- Mcallister, M.; Dawkins, J.; Knight, B.A.; Hasking, P.; Withyman, C. Building resilience in regional youth: Impacts of a universal mental health promotion programme. Int. J. Ment. Health Nurs. 2018, 27, 1044–1054. [Google Scholar] [CrossRef] [PubMed]
- Mckenzie, K.; Murray, G.C.; Prior, S.; Stark, L.; Mckenzie, K.; Murray, G.C.; Prior, S.; Stark, L. An evaluation of a school counselling service with direct links to Child and Adolescent Mental Health ( CAMH ) services. Br. J. Guid. Couns. 2011, 39, 67–82. [Google Scholar] [CrossRef]
- Mellin, E.A.; Weist, M.D. Exploring School Mental Health Collaboration in an Urban Community: A Social Capital Perspective. Sch. Ment. Health 2011, 3, 81–92. [Google Scholar] [CrossRef]
- Mishna, B.F.; Muskat, B. School-Based Group Treatment for Students with Learning Disabilities: A Collaborative Approach. Child. Sch. 2004, 26, 135–150. [Google Scholar] [CrossRef]
- Moilanen, D.L.; Med, S.B. A High School Depression and Suicide Prevention Program: A Collaboration between Health Education and Psychological Services. Am. J. Health Educ. 2002, 33, 148–153. [Google Scholar] [CrossRef]
- Mufson, L.; Dorta, K.P.; Wickramaratne, P.; Nomura, Y.; Olfson, M.; Weissman, M.M. A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Arch. Gen. Psychiatry 2004, 61, 577–584. [Google Scholar] [CrossRef] [Green Version]
- Munns, A.; Forde, K.A.; Krouzecky, M.; Shields, L. Rainbows: A primary health care initiative for primary schools. Collegian 2015, 22, 153–160. [Google Scholar] [CrossRef] [Green Version]
- O’Callaghan, P.; Cunningham, E. Can a targeted, group-based CBT intervention reduce depression and anxiety and improve self- concept in primary-age children? Educ. Psychol. Pract. 2015, 31, 313–325. [Google Scholar] [CrossRef]
- Owens, J.S.; Girio, E.L.; Himawan, L.K.; Abbot, M.Y. Implementing and Evaluating Evidence- Based Treatments in Schools: Successes and Lessons Learned. Adv. Sch. Ment. Health Promot. 2008, 1, 39–51. [Google Scholar] [CrossRef]
- Panayiotopoulos, C.; Kerfoot, M. A Home and School Support Project for Children Excluded from Primary and First Year Secondary School. Child Adolesc. Ment. Health 2004, 9, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Powell, S.; Calkins, C.; Quealy-berge, D. Adolescent Day Treatment: A School and Community Based Alternative to Residential Care. J. Dev. Phys. Disabil. 1999, 11, 275–286. [Google Scholar] [CrossRef]
- Rosenblatt, A.; Francisco, S.; Attkisson, C.C. Integrating Systems of Care in California for Youth with Severe Emotional Disturbance IV: Educational Attendance and Achievement. J. Child Fam. Stud. 1997, 6, 113–129. [Google Scholar] [CrossRef]
- Stanzel, K.A. Outreach youth health service in school setting: A retrospective case study. Aust. J. Prim. Health 2016, 22, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Vander Stoep, A.; McCauley, E.; Thompson, K.A.; Herting, J.R.; Kuo, E.S.; Stewart, D.G.; Anderson, C.A.; Kushner, S. Universal Emotional Health Screening at the Middle School Transition. J. Emot. Behav. Disord. 2005, 13, 213–223. [Google Scholar] [CrossRef] [PubMed]
- White, H.; Lafleur, J.; Blake, S.M.; Houle, K.; Hyrydermith, P. Evaluation of a school-based transition program designed to facilitate school reentry following a mental health crisis or psychiatric hospitalization. Psychol. Sch. 2017, 54, 868–882. [Google Scholar] [CrossRef]
- Winther, J.; Carlsson, A.; Vance, A. A pilot study of a school-based prevention and early intervention program to reduce oppositional defiant disorder/conduct disorder. Early Interv. Psychiatry 2014, 8, 181–189. [Google Scholar] [CrossRef]
- Wolraich, M.; Bickman, L.; Schuchman, M.A. Intervening to Improve Communication between Parents, Teachers, and Primary Care. Providers of Children with ADHD or at High Risk for ADHD. J. Atten. Disord. 2005, 9, 354–368. [Google Scholar] [CrossRef]
- Blackman, K.F.; Powers, J.D.; Edwards, J.D.; Wegmann, K.M.; Lechner, E.; Swick, D.C. Closing the Gap: Principal Perspectives on an Innovative School-Based Mental Health Intervention. Urban Rev. 2016, 48, 245–263. [Google Scholar] [CrossRef]
- Einspruch, E.; Deck, D.; Grover, J.; Hahn, K. Readiness to Learn School-Linked Models for Integrated Family Services. 1999–2000 Evaluation Update. 2001; pp. 1–50. Available online: https://eric.ed.gov/?id=ED450966 (accessed on 10 February 2022).
- Carroll, C.; Patterson, M.; Wood, S.; Booth, A.; Rick, J.; Balain, S. A conceptual framework for implementation fidelity. Implement. Sci. 2007, 2, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hasson, H. Systematic evaluation of implementation fidelity of complex interventions in health and social care. Implement. Sci. IS 2010, 5, 67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Proctor, E.; Silmere, H.; Raghavan, R.; Hovmand, P.; Aarons, G.; Bunger, A.; Griffey, R.; Hensley, M. Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Adm. Policy Ment. Health Ment. Health Serv. Res. 2011, 38, 65–76. [Google Scholar] [CrossRef] [Green Version]
- Aarons, G.; Miller, E.; Green, A.; Perrott, J.; Bradway, R. Adaptation happens: A qualitative case study of implementation of The Incredible Years evidence-based parent training programme in a residential substance abuse treatment programme. J. Child. Serv. 2012, 7, 233–245. [Google Scholar] [CrossRef]
- Moore, J.E.; Bumbarger, B.K.; Cooper, B.R. Examining adaptations of evidence-based programs in natural contexts. J. Prim. Prev. 2013, 34, 147–161. [Google Scholar] [CrossRef] [PubMed]
- Stirman, S.W.; Gamarra, J.; Bartlett, B.; Calloway, A.; Gutner, C. Empirical Examinations of Modifications and Adaptations to Evi dence-Based Psychotherapies: Methodologies, Impact, and Future Directions. Clin. Psychol. 2017, 24, 396–420. [Google Scholar] [CrossRef]
- Castro, F.G.; Yasui, M. Advances in EBI Development for Diverse Populations: Towards a Science of Intervention Adaptation. Prev. Sci. 2017, 18, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Castro, F.G.; Barrera, M.; Martinez, C.R. The Cultural Adaptation of Prevention Interventions: Resolving Tensions between Fidelity and Fit. Prev. Sci. 2004, 5, 41–45. [Google Scholar] [CrossRef]
- Lee, S.J.; Altschul, I.; Mowbray, C.T. Using planned adaptation to implement evidence-based programs with new populations. Am. J. Community Psychol. 2008, 41, 290–303. [Google Scholar] [CrossRef] [Green Version]
- Pérez, D.; Van der Stuyft, P.; Zabala, M.D.C.; Castro, M.; Lefèvre, P. A modified theoretical framework to assess implementation fidelity of adaptive public health interventions. Implement. Sci. 2016, 11, 91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chambers, D.A.; Norton, W.E. The Adaptome: Advancing the Science of Intervention Adaptation. Am. J. Prev. Med. 2016, 51, S124–S131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- von Thiele Schwarz, U.; Förberg, U.; Sundell, K.; Hasson, H. Colliding ideals-an interview study of how intervention researchers address adherence and adaptations in replication studies. BMC Med. Res. Methodol. 2018, 18, 36. [Google Scholar] [CrossRef] [Green Version]
- von Thiele Schwarz, U.; Aarons, G.A.; Hasson, H. The Value Equation: Three complementary propositions for reconciling fidelity and adaptation in evidence-based practice implementation. BMC Health Serv. Res. 2019, 19, 868. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drahota, A.; Meza, R.D.; Brikho, B.; Naaf, M.; Estabillo, J.A.; Gomez, E.D.; Vejnoska, S.F.; Dufek, S.; Stahmer, A.C.; Aarons, G.A. Community-Academic Partnerships: A Systematic Review of the State of the Literature and Recommendations for Future Research. Milbank Q. 2016, 94, 163–214. [Google Scholar] [CrossRef] [Green Version]
- Cuijpers, P.; Graaf, I.D.; Bohlmeijer, E. Adapting and disseminating effective public health interventions in another country: Towards a systematic approach. Eur. J. Public Health 2005, 15, 166–169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beidas, R.S.; Kendall, P.C. Training Therapists in Evidence-Based Practice: A Critical Review of Studies From a Systems-Contextual Perspective. Clin. Psychol. 2010, 17, 1–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glisson, C.; Landsverk, J.; Schoenwald, S.; Kelleher, K.; Hoagwood, K.E.; Mayberg, S.; Green, P. Assessing the organizational social context (OSC) of mental health services: Implications for research and practice. Adm. Policy Ment. Health 2008, 35, 98–113. [Google Scholar] [CrossRef] [PubMed]
- Lyon, A.R.; Whitaker, K.; Locke, J.; Cook, C.R.; King, K.M.; Duong, M.; Davis, C.; Weist, M.D.; Ehrhart, M.G.; Aarons, G.A. The impact of inter-organizational alignment (IOA) on implementation outcomes: Evaluating unique and shared organizational influences in education sector mental health. Implement. Sci. 2018, 13, 24. [Google Scholar] [CrossRef] [Green Version]
- Organisation for Economic Cooperation and Development. Working and Learning Together; Organisation for Economic Cooperation and Development: Paris, France, 2019. [Google Scholar] [CrossRef]
- Kost, R.G.; Reider, C.; Stephens, J.; Schuff, K.G. Research subject advocacy: Program implementation and evaluation at clinical and translational science award centers. Acad. Med. J. Assoc. Am. Med. Coll. 2012, 87, 1228–1236. [Google Scholar] [CrossRef] [Green Version]
- Wilkins, C.H.; Spofford, M.; Williams, N.; McKeever, C.; Allen, S.; Brown, J.; Opp, J.; Richmond, A.; Strelnick, A.H. Community representatives’ involvement in Clinical and Translational Science Awardee activities. Clin. Transl. Sci. 2013, 6, 292–296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goodman, M.S.; Sanders Thompson, V.L. The science of stakeholder engagement in research: Classification, implementation, and evaluation. Transl. Behav. Med. 2017, 7, 486–491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Domitrovich, C.E.; Bradshaw, C.P.; Poduska, J.M.; Buckley, J.A.; Olin, S.; Romanelli, L.H.; Leaf, P.J.; Greenberg, M.T.; Ialongo, N.S. Preventive interventions in schools: A conceptual framework. Adv. Sch. Ment. Health Promot. 2008, 1, 6–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Medical Research Council. A Framework for the Development and Evaluation of RCTs for Complex Interventions to Improve Health; Medical Research Council: Swindon, UK, 2000. [Google Scholar]
- Hawe, P.; Shiell, A.; Riley, T.; Gold, L. Methods for exploring implementation variation and local context within a cluster randomised community intervention trial. J. Epidemiol. Community Health 2004, 58, 788–793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Authors, Year | Country | Data Collection | Target Intervention Group | Participating Actors | Type of Issue | Intervention Name/Goal | Intervention Type |
|---|---|---|---|---|---|---|---|
| Anderson-Butcher et al. [42] | USA | Quantitative | Students in 3rd, 6th, 8th, and 12th grades | School, health-care providers, social service | Students at risk for poor academic and developmental outcomes | Ohio Community Collaboration Model for School Improvement (OCCMSI). Help schools and districts expand improvement efforts for at-risk children. | Selective |
| Atkins et al. [43] | USA | Quantitative | School teachers in urban, deprived areas | School and mental health services | ADHD | Increase the use of practices for children with ADHD. | Selective |
| Axberg et al. [44] | Sweden | Quantitative | Youth with externalizing problems | School, mental health services | Externalizing behavior | Marte Meo (MM) and Coordination Meeting (CM). Help children with externalizing problems and help their families. | Indicated |
| Baxendale et al. [45] | USA | Qualitative | Youth with communication needs | School, health care | Communication disorder | The Social Communication Intervention Project (SCIP). Enhance communication skills. | Indicated |
| Bellinger et al. [46] | USA | Quantitative | Children (ages 3–8) who experienced frequent noncompliance at home and school | School, mental health services | Behavioral and emotional problems | Conjoint Behavioral Consulting (CBC). Address student needs via evidence-based interventions, involve and engage families in their child’s education, and facilitate partnerships and build relationships between schools and families. | Indicated |
| Bhatara et al. [47] | USA | Qualitative | Teachers | School, mental health services, social services | ADHD | Swanson, Kotkin, Agler, M-Flynn and Pelham Scale-Teacher Version (T-SKAMP). Promote grading efficacy for children with ADHD. | Universal |
| Bruns et al. [48] | USA | Quantitative | All students at a public elementary school | School, mental health services | Emotional and behavioral problems | Expanded School Mental Health (ESMH). Provide school-based mental health services. | Universal |
| Capp [49] | USA | Qualitative | School students and staff and parents | School, mental health services | Diagnosable mental health disorders | Our Community, Our Schools (OCOS). Provide easy access to mental health promotion and treatment for students and their families, including access for those without insurance. | Universal |
| Clarke et al. [50] | UK | Mixed | School nurses and elementary school students, aged 10–11, in deprived areas | School, mental health services, and social services | General mental health issues | Facilitate accessible mental health support for young people, provide a problem- solving model for adolescents who have mental health issues, and support the role of school nurses by enhancing of their skills in mental health. | Universal |
| Fazel et al. [51] | UK | Quantitative | Refugee children and school staff | Schools and mental health services | Risk of emotional and behavioral problems | Provide a mental health service for refugees. | Selective |
| Fiester and Nathanson [52] | USA | Qualitative | School students | Schools and health-care providers | General mental health issues | Provide violence prevention and mental health services. | Universal |
| Foy and Earls [53] | USA | Qualitative | Community stakeholders, teachers, and parents | Schools and health-care providers | ADHD | Increase practice efficiency and improve practice standards for children with ADHD. | Indicated |
| Goodwin et al. [54] | USA | Quantitative | Children older than 5 years in child-care centers, preschools, or in a child-care provider’s home care | Schools, mental health services, and health-care providers | Emotional or behavioral problems | The Childreach program. Decrease violent and aggressive behavior in preschool-age children. | Selective |
| Hunter et al. [55] | UK | Qualitative | Students in secondary education | Schools and mental health services | General mental health issues | Enhance the effectiveness of the interface between primary care and specialist CAMHS services. | Universal |
| Jaatinen et al. [56] | Finland | No info | Children and adolescence | Schools, mental health services, health-care providers, and social services | Mental health and psychosocial problems | Provide psychosocial support for schoolchildren via networking family counselling services. | Universal |
| Jennings et al. [57] | USA | Mixed | Youth in an urban school district and their families | Schools and mental-health services | General mental health issues | Dallas (Texas) public school initiative. Provide physical health, mental health, and other support services for students and their families. | Universal |
| Juszczak et al. [58] | USA | Quantitative | All children who visited a clinic or school mental-health service | Schools and health-care providers | General mental health issues | School-Based Health Centers. Facilitate access to care. | Universal |
| Khan et al. [59] | Australia | Qualitative | Secondary- school students | Schools, mental health services, and health-care providers | General mental health | MindMatters. Improve health, well-being, and education outcomes in secondary schools in south-west Sydney. | Selective |
| Kutcher and Wei [60] | Canada | Mixed | School students | Schools, mental-health services, health-care providers, and social services | General mental health services | The School-Based Pathway to Care Model. Enhance the collaboration between schools, health-care providers, and community stakeholders to meet the need for mental-health support for adolescents. | Universal |
| Li-Grining et al. [61] | USA | Quantitative | All caregiving adults (e.g., teachers) and children from a preschool | Schools, mental-health services, and social services | General emotional and behavioral issues | Chicago School Readiness Project (CSRP). Promote low-income young children’s school readiness by creating emotionally supportive classrooms and by fostering preschoolers’ self-regulatory competence. | Universal |
| Maddern et al. [62] | UK | Mixed | Children with severe emotional and behavioral problems and their parents | Schools and mental-health services | Severe emotional and behavioral problems | Promote children’s cooperative skills and anger management. | Indicated |
| Mcallister et al. [63] | Australia | Quantitative | 13-year-old children in rural areas | Schools and mental-health services | Psychological distress | Icare-R. Promote mental health. | Universal |
| Mckenzie et al. [64] | UK | Quantitative | Students in a rural area and guidance staff | Schools and mental-health services | General mental health issues | Provide community-based school counselling services. | Universal |
| Mellin and Weist [65] | USA | Qualitative | Elementary/middle (combined in this district) and high school students | Schools and mental-health services | General mental health | Enhance collaboration between schools and mental health services. | Universal |
| Mishna and Muskat [66] | Canada | Mixed | Students with various social, emotional, and behavioral problems; their families; school peers; school personnel; and social workers | Schools, mental-health services, and social services | Learning disabilities and psychosocial problems | Improve the psychosocial functioning of high-risk students with learning disabilities and psychosocial problems and increase the understanding of their learning disability. | Selective |
| Moilanen and Med [67] | USA | Mixed | Students in grades 8 through 12, school personnel, and parents | Schools and mental-health services | Depression and suicide | Prevent depression and suicide within high schools and local communities | Universal/Indicated |
| Mufson et al. [68] | USA | Quantitative | Depressed youth | Schools, mental-health services, health-care providers, and social services | Depression | IPT-A. Reduce depressive symptoms and improve interpersonal functions. | Indicated |
| Munns et al. [69] | Australia | Qualitative | Primary school-aged children who experienced loss (such as a death in the family, parental divorce, or other painful transitions) | Schools and health-care providers | Traumatic events | The Rainbow program. Support children who have experienced traumatic events | Indicated |
| O’Callaghan and Cunningham [70] | UK | Mixed | Primary-age children, 8- to 11-year-old pupils | Schools and mental-health services | Anxiety, depression, or low self-esteem | Cool Connections. Decrease depression and the risk of suicide and improve self-perception. | Indicated |
| Owens et al. [71] | USA | Mixed | Students in kindergarten through 6th grade | Schools and mental-health services | ADHD | Youth Experiencing Success in School (YESS). Enhance the use of EBTs in schools, improve the academic and behavioral functioning of children, enhance home–school collaboration and support services for parents, and provide ongoing collaborative consultation for teachers. | Indicated |
| Panayiotopoulos and Kerfoot [72] | UK | Mixed | Pupils, their family, and school staff | Schools, mental-health services, and social services | School exclusion | A home and school support project (HASSP). Prevent school exclusions. | Indicated |
| Powell et al. [73] | USA | Quantitative | Students in grades 7 to 12 | Schools and mental health services | Emotional and behavioral disorders and educational disabilities | Help students return to public-school settings as quickly as possible. | Indicated |
| Rosenblatt et al. [74] | USA | Quantitative | Special education students/students with SED | Schools and mental-health services | Severe emotional disturbance (SED) | Provide collaborative mental health and education services. | Indicated |
| Stanzel [75] | Australia | Qualitative | High school students in rural areas | Schools and health-care providers | General mental health | Outreach youth clinic (OYC). Promote better health for young people by ensuring coordination between schools and community health and support s ervices. | Universal |
| Vander Stoep et al. [76] | USA | Quantitative | 6th-grade students, the majority in special-needs groups | Schools and mental-health services | Emotional distress | Developmental Pathways Screening Program (DPSP). Identify youth experiencing significant emotional distress who need support services. | Universal |
| White et al. [77] | USA | Quantitative | Students returning to school after a psychiatric hospitalization or other prolonged absence due to mental-health reasons and their families | Schools and mental-health services | General mental-health issues | Bridge for Resilient Youth in Transition. Support academic and clinical outcomes for high school students returning to school after a mental-health crisis. | Selective and indicated |
| Winther et al. [78] | Australia | Quantitative | All children from preparatory to grade 3 (ages 4–10 years), teachers, and parents | School, health care and mental-health services | Oppositional defiance disorder/conduct disorder (ODD/CD) | Royal Children’s Hospital, Child and Adolescent Mental Health Service and Schools’ Early Action Program. Address emerging ODD/CD. | Indicated |
| Wolraich et al. [79] | USA | Mixed | ADHD children and their caregivers, medical services, and teachers | Schools and health-care providers | ADHD | Improve communication between individuals who care for children with ADHD. | Indicated |
| CFIR Domains | All Studies n = 38 | Universal Interventions n = 17 | Selective Interventions n = 7 | Indicated Interventions n = 14 |
|---|---|---|---|---|
| 47 | 17 | 8 | 22 |
| Intervention Source | - | - | - | - |
| Evidence Strength and Quality | 3 | - | 2 | 1 |
| Relative Advantage | 2 | 1 | - | 1 |
| Adaptability | 11 | 2 | 2 | 7 |
| Trialability | 3 | 1 | - | 2 |
| Complexity | 2 | 2 | - | - |
| Design Quality and Packaging | 19 | 9 | 2 | 8 |
| Cost | 7 | 2 | 2 | 3 |
| 19 | 9 | 2 | 8 |
| Patient Needs and Resources | 1 | - | - | 1 |
| Cosmopolitanism | 6 | 3 | 1 | 2 |
| Peer Pressure | 2 | - | 1 | 1 |
| External Policy and Incentives | 10 | 6 | - | 4 |
| 62 | 30 | 12 | 20 |
| Structural Characteristics | 4 | 1 | 2 | 1 |
| Networks and Communications | 17 | 9 | 3 | 5 |
| Culture | 6 | 4 | 1 | 1 |
| Implementation Climate | - | - | - | - |
| - | - | - | - |
| 2 | 1 | - | 1 |
| 4 | 2 | 1 | 1 |
| - | - | - | - |
| 9 | 4 | 2 | 3 |
| - | - | - | - |
| Readiness for Implementation | - | - | - | - |
| 2 | 2 | - | - |
| 16 | 5 | 3 | 8 |
| 2 | 2 | - | - |
| 11 | 2 | 3 | 5 |
| Knowledge and Beliefs About the Innovation | 9 | 2 | 2 | 4 |
| Self-Efficacy | - | - | - | - |
| Individual Stage of Change | - | - | - | - |
| Individual Identification with Organization | - | - | - | - |
| Other Personal Attributes | 2 | - | 1 | 1 |
| 40 | 20 | 9 | 11 |
| Planning | 5 | 5 | - | - |
| Engaging | - | - | - | - |
| 3 | - | 2 | 1 |
| 2 | 1 | 1 | - |
| - | - | - | - |
| 1 | - | 1 | - |
| 17 | 10 | 3 | 4 |
| 9 | 3 | 2 | 4 |
| Executing | 1 | - | - | 1 |
| Reflecting and Evaluating | 2 | 1 | - | 1 |
| Reference | Process | Inner Setting | Outer Setting | Intervention Characteristics | Individuals’ Characteristics |
|---|---|---|---|---|---|
| Anderson-Butcher et al. [42] | Implementation Climate—Relative Priority Implementation Climate—Goals and Feedback | Adaptability | |||
| Atkins et al. [43] | Engaging Opinion Leaders | ||||
| Axberg et al. [44] | Networks and Communications | Trialability Design Quality and Packaging Adaptability | |||
| Baxendale et al. [45] | Reflecting and Evaluating Planning Engaging Innovation Participants | Implementation Climate— Compatibility Readiness for Implementation—Available Resources | External Policy and Incentives | Design Quality and Packaging Adaptability Evidence Strength and Quality | Knowledge and Beliefs |
| Bellinger et al. [46] | Readiness for Implementation—Available Resources | External Policy and Incentives | Cost Design Quality and Packaging | ||
| Bhatara et al. [47] | Engaging Key Stakeholders | Cosmopolitanism | Design Quality and Packaging | ||
| Bruns et al. [48] | Design Quality and Packaging | ||||
| Capp [49] | Engaging Key Stakeholders Engaging Innovation Participants | Readiness for Implementation—Available Resources | Design Quality and Packaging Cost | ||
| Clarke et al. [50] | Engaging Key Stakeholders | ||||
| Fazel et al. [51] | Engaging Innovation Participants | Readiness for Implementation—Available Resources Networks and Communications | Peer Pressure | Evidence Strength and Quality | |
| Fiester and Nathanson [52] | Planning Engaging Key Stakeholders | Implementation Climate—Relative Priority Readiness for Implementation—Leadership Engagement Implementation Climate—Goals and Feedback Culture Readiness for Implementation—Available Resources | External Policy and Incentives Cosmopolitanism | Complexity | |
| Foy and Earls [53] | Engaging Key Stakeholders | External Policy and Incentives Cosmopolitanism | |||
| Goodwin et al. [54] | Cosmopolitanism | Cost | Other Personal Attributes | ||
| Hunter et al. [55] | Engaging Key Stakeholders | Implementation Climate— Compatibility Readiness for Implementation—Access to Information Readiness for Implementation—Available Resources Implementation Climate—Goals and Feedback Culture Networks and Communications | External Policy and Incentives | Relative Advantage Trialability | |
| Jaatinen et al. [56] | Engaging Key Stakeholders | Networks and Communications | |||
| Jennings et al. [57] | Engaging Innovation Participants Engaging Key Stakeholders | Networks and Communications | External Policy and Incentives | Knowledge and Beliefs | |
| Juszczak et al. [58] | External Policy and Incentives | ||||
| Khan et al. [59] | Engaging Key Stakeholders Engaging Innovation Participants Engaging External Change Agent Engaging Formally Appointed Internal Implementation Leaders | Structural Characteristics Networks and Communications Culture Readiness for Implementation—Available Resources | Design Quality and Packaging Cost | Knowledge and Beliefs | |
| Kutcher and Wei [60] | Reflecting and Evaluating Engaging Key Stakeholders | Networks and Communications Implementation Climate—Goals and Feedback | External Policy and Incentives | Adaptability Design Quality and Packaging | Knowledge and Beliefs |
| Li-Grining et al. [61] | Planning | Networks and Communications Culture | Complexity Design Quality and Packaging | ||
| Maddern et al. [62] | Engaging Innovation Participants Engaging Key Stakeholders | Implementation Climate Readiness for Implementation—Available Resources Implementation Climate—Goals and Feedback Networks and Communications Structural Characteristics | Patient Needs and Resources Peer Pressure | Adaptability Design Quality and Packaging | |
| Mcallister et al. [63] | Implementation Climate—Relative Priority Networks and Communications | Design Quality and Packaging | |||
| Mckenzie et al. [64] | Engaging Innovation Participants | Readiness for Implementation—Leadership Engagement Networks and Communications | Design Quality and Packaging | ||
| Mellin and Weist [65] | Planning Engaging Key Stakeholders | Networks and Communications Structural Characteristics Readiness for Implementation—Available Resources Culture Implementation Climate—Goals and Feedback | External Policy and Incentives | Knowledge and Beliefs | |
| Mishna and Muskat [66] | Engaging Opinion Leaders Engaging Key Stakeholders | Implementation Climate—Goals and Feedback Networks and Communications Structural Characteristics | Design Quality and Packaging Evidence Strength and Quality Adaptability | Knowledge and Beliefs | |
| Moilanen and Med [67] | Engaging Key Stakeholders | Design Quality and Packaging | |||
| Mufson et al. [68] | Engaging Innovation Participants | Readiness for Implementation—Available Resources | Adaptability Design Quality and Packaging | ||
| Munns et al. [69] | Engaging Key Stakeholders | Readiness for Implementation—Available Resources Networks and Communications | Cosmopolitanism | Design Quality and Packaging Cost Adaptability | |
| O’Callaghan and Cunningham [70] | Networks and Communications | Design Quality and Packaging | |||
| Owens et al. [71] | Planning Engaging Opinion Leaders Executing | Networks and Communications Implementation Climate—Goals and Feedback Readiness for Implementation—Available Resources | External Policy and Incentives | Trialability | Other Personal Attributes Knowledge and Beliefs |
| Panayiotopoulos and Kerfoot [72] | Engaging Key Stakeholders | Implementation Climate—Goals and Feedback | Adaptability | Knowledge and Beliefs | |
| Powell et al. [73] | Adaptability | ||||
| Rosenblatt et al. [74] | Readiness for Implementation—Available Resources Culture | Knowledge and Beliefs | |||
| Stanzel [75] | Engaging Formally Appointed Internal Implementation Leaders | Networks and Communications Readiness for Implementation—Access to Knowledge and Information | Design Quality and Packaging Adaptability | ||
| Vander Stoep et al. [76] | Readiness for Implementation—Available Resources | Cosmopolitanism | Cost | ||
| White et al. [77] | Engaging Key Stakeholders | Readiness for Implementation—Available Resources Implementation Climate—Relative Priority | |||
| Winther et al. [78] | Readiness for Implementation—Available Resources | Cost Design Quality and Packaging | |||
| Wolraich et al. [79] | Engaging Innovation Participants | Relative Advantage |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Richter, A.; Sjunnestrand, M.; Romare Strandh, M.; Hasson, H. Implementing School-Based Mental Health Services: A Scoping Review of the Literature Summarizing the Factors That Affect Implementation. Int. J. Environ. Res. Public Health 2022, 19, 3489. https://doi.org/10.3390/ijerph19063489
Richter A, Sjunnestrand M, Romare Strandh M, Hasson H. Implementing School-Based Mental Health Services: A Scoping Review of the Literature Summarizing the Factors That Affect Implementation. International Journal of Environmental Research and Public Health. 2022; 19(6):3489. https://doi.org/10.3390/ijerph19063489
Chicago/Turabian StyleRichter, Anne, My Sjunnestrand, Maria Romare Strandh, and Henna Hasson. 2022. "Implementing School-Based Mental Health Services: A Scoping Review of the Literature Summarizing the Factors That Affect Implementation" International Journal of Environmental Research and Public Health 19, no. 6: 3489. https://doi.org/10.3390/ijerph19063489






