Pelvic Floor Muscle Strength in the First Trimester of Primipara: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
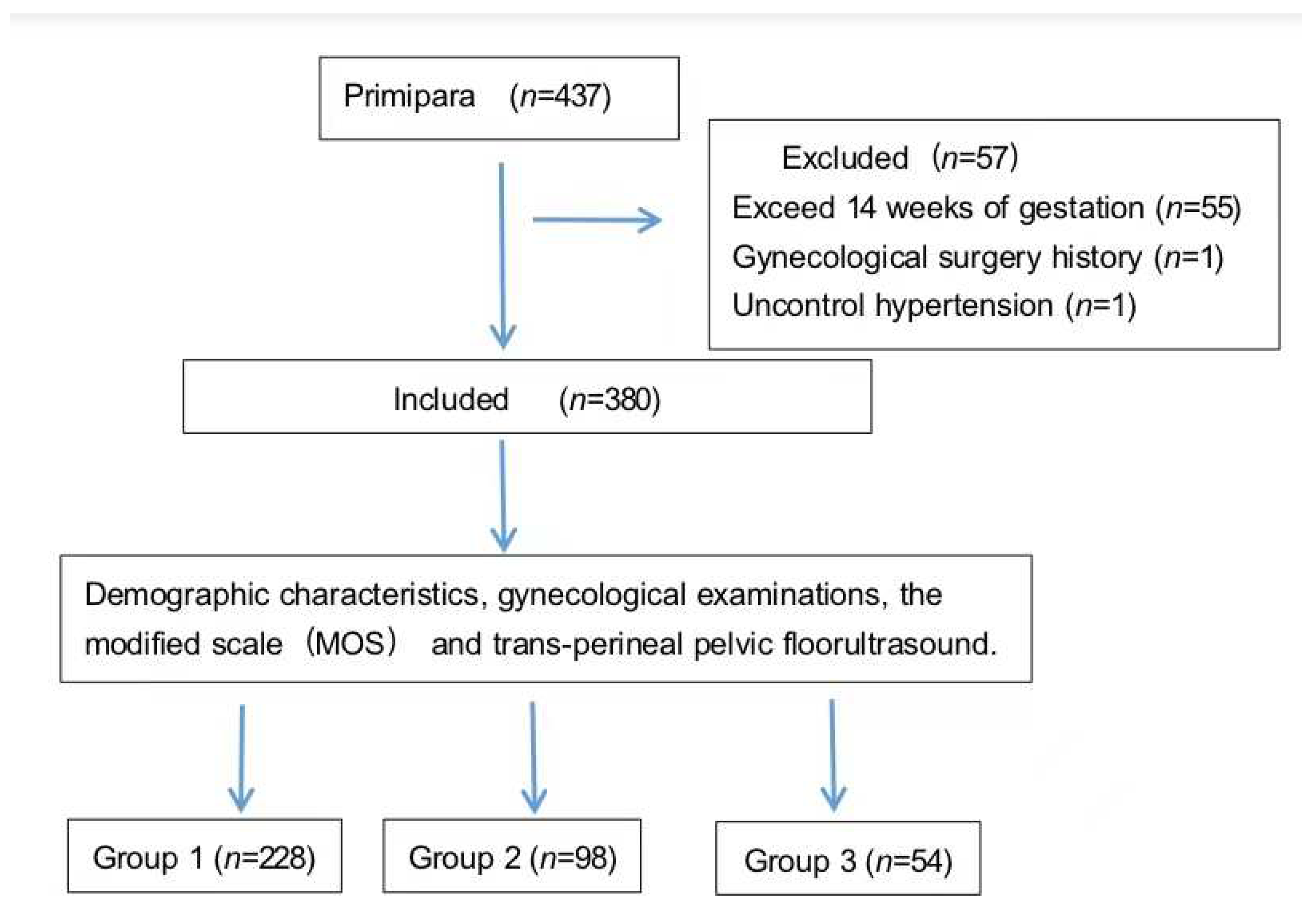
2.1. Participants
2.2. Measurement
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sangsawang, B.; Sangsawang, N. Stress urinary incontinence in pregnant women: A review of prevalence, pathophysiology, and treatment. Int. Urogynecol. J. 2013, 24, 901–912. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gümüşsoy, S.; Öztürk, R.; Kavlak, O.; Hortu, İ.; Yeniel, A.Ö. Investigating Pelvic Floor Muscle Strength in Women of Reproductive Age and Factors Affecting It. Clin. Nurs. Res. 2021, 30, 1047–1058. [Google Scholar] [CrossRef] [PubMed]
- Capobianco, G.; Madonia, M.; Morelli, S.; Dessole, F.; De Vita, D.; Cherchi, P.L.; Dessole, S. Management of female stress urinary incontinence: A care pathway and update. Maturitas 2018, 109, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Davenport, M.H.; Nagpal, T.S.; Mottola, M.F.; Skow, R.J.; Riske, L.; Poitras, V.J.; Garcia, A.J.; Gray, C.; Barrowman, N.; Meah, V.L.; et al. Prenatal exercise (including but not limited to pelvic floor muscle training) and urinary incontinence during and following pregnancy: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 1397–1404. [Google Scholar] [CrossRef] [PubMed]
- Blomquist, J.L.; Carroll, M.; Muñoz, A.; Handa, V.L. Pelvic floor muscle strength and the incidence of pelvic floor disorders after vaginal and cesarean delivery. Am. J. Obstet. Gynecol. 2020, 222, 62.e1–62.e8. [Google Scholar] [CrossRef] [Green Version]
- Mørkved, S.; Salvesen, K.A.; Bø, K.; Eik-Nes, S. Pelvic floor muscle strength and thickness in continent and incontinent nulliparous pregnant women. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2004, 15, 384–390; discussion 390. [Google Scholar] [CrossRef]
- Rathore, A.; Suri, J.; Agarwal, S.; Mittal, P. Antenatal and postnatal assessment of pelvic floor muscles in continent and incontinent primigravida women. Int. Urogynecol. J. 2021, 32, 1875–1882. [Google Scholar] [CrossRef]
- Nallasamy, S.; Yoshida, K.; Akins, M.; Myers, K.; Iozzo, R.; Mahendroo, M. Steroid Hormones are Key Modulators of Tissue Mechanical Function via Regulation of Collagen and Elastic Fibers. Endocrinology 2017, 158, 950–962. [Google Scholar] [CrossRef] [Green Version]
- Valkovic, A.L.; Bathgate, R.A.; Samuel, C.S.; Kocan, M. Understanding relaxin signalling at the cellular level. Mol. Cell. Endocrinol. 2019, 487, 24–33. [Google Scholar] [CrossRef]
- Palmezoni, V.P.; Santos, M.D.; Pereira, J.M.; Bernardes, B.T.; Pereira-Baldon, V.S.; Resende, A.P.M. Pelvic floor muscle strength in primigravidae and non-pregnant nulliparous women: A comparative study. Int. Urogynecol. J. 2017, 28, 131–137. [Google Scholar] [CrossRef]
- Woodley, S.J.; Boyle, R.; Cody, J.D.; Mørkved, S.; Hay-Smith, E.J.C. Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst. Rev. 2017, 12, Cd007471. [Google Scholar] [CrossRef] [PubMed]
- Reilly, E.T.; Freeman, R.M.; Waterfield, M.R.; Steggles, P.; Pedlar, F. Prevention of postpartum stress incontinence in primigravidae with increased bladder neck mobility: A randomised controlled trial of antenatal pelvic floor exercises. BJOG 2014, 121 (Suppl. 7), 58–66. [Google Scholar] [CrossRef] [PubMed]
- Petricelli, C.D.; Resende, A.P.M.; Júnior, J.E.; Júnior, E.A.; Alexandre, S.M.; Zanetti, M.R.D.; Nakamura, M.U. Distensibility and strength of the pelvic floor muscles of women in the third trimester of pregnancy. Biomed. Res. Int. 2014, 2014, 437867. [Google Scholar] [CrossRef] [PubMed]
- Mørkved, S.; Bø, K. Effect of pelvic floor muscle training during pregnancy and after childbirth on prevention and treatment of urinary incontinence: A systematic review. Br. J. Sports Med. 2014, 48, 299–310. [Google Scholar] [CrossRef] [Green Version]
- Santos, M.D.; Palmezoni, V.P.; Torelli, L.; Pereira-Baldon, V.S.; Sartori, M.G.F.; Resende, A.P.M. Evaluation of pelvic floor muscle strength and its correlation with sexual function in primigravid and non-pregnant women: A cross-sectional study. Neurourol. Urodyn. 2018, 37, 807–814. [Google Scholar] [CrossRef]
- Soave, I.; Scarani, S.; Mallozzi, M.; Nobili, F.; Marci, R.; Caserta, D. Pelvic floor muscle training for prevention and treatment of urinary incontinence during pregnancy and after childbirth and its effect on urinary system and supportive structures assessed by objective measurement techniques. Arch. Gynecol. Obstet. 2019, 299, 609–623. [Google Scholar] [CrossRef]
- Gao, L.; Zhang, D.; Wang, S.; Jia, Y.; Wang, H.; Sun, X.; Wang, J. Effect of the App-Based Video Guidance on Prenatal Pelvic Floor Muscle Training Combined with Global Postural Re-education for Stress Urinary Incontinence Prevention: A Protocol for a Multicenter, Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 12929. [Google Scholar] [CrossRef]
- Siccardi, M.A.; Bordoni, B. Anatomy, Abdomen and Pelvis, Perineal Body. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2021. [Google Scholar]
- Friedman, S.; Blomquist, J.L.; Nugent, J.M.; McDermott, K.C.; Muñoz, A.; Handa, V.L. Pelvic muscle strength after childbirth. Obstet. Gynecol. 2012, 120, 1021–1028. [Google Scholar] [CrossRef]
- Bump, R.C.; Norton, P.A. Epidemiology and natural history of pelvic floor dysfunction. Obstet. Gynecol. Clin. N. Am. 1998, 25, 723–746. [Google Scholar] [CrossRef]
- Sartori, D.V.B.; Kawano, P.R.; Yamamoto, H.A.; Guerra, R.; Pajolli, P.R.; Amaro, J.L. Pelvic floor muscle strength is correlated with sexual function. Investig. Clin. Urol. 2021, 62, 79–84. [Google Scholar] [CrossRef]
- Martinez, C.S.; Ferreira, F.V.; Castro, A.A.; Gomide, L.B. Women with greater pelvic floor muscle strength have better sexual function. Acta Obstet. Gynecol. Scand. 2014, 93, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Kurt, S.; Canda, M.T.; Bal, M.; Taşyurt, A. Are there any preventable risk factors for women who had surgery for Pelvic Organ Prolapse and stress Urinary Incontinence? Pak. J. Med. Sci. 2018, 34, 874–878. [Google Scholar] [CrossRef]
- Li, H.; Wu, R.; Qi, F.; Xiao, A.; Ma, Z.; Hu, Y.; Zhang, W.; Li, W.; Wang, Z. Postpartum pelvic floor function performance after two different modes of delivery. Genet. Mol. Res. 2015, 14, 2994–3001. [Google Scholar] [CrossRef]
- Özdemır, Ö.Ç.; Bakar, Y.; Özengın, N.; Duran, B. The effect of parity on pelvic floor muscle strength and quality of life in women with urinary incontinence: A cross sectional study. J. Phys. Ther. Sci. 2015, 27, 2133–2137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sigurdardottir, T.; Steingrimsdottir, T.; Geirsson, R.T.; Halldorsson, T.I.; Aspelund, T.; Bø, K. Can postpartum pelvic floor muscle training reduce urinary and anal incontinence? An assessor-blinded randomized controlled trial. Am. J. Obstet. Gynecol. 2020, 222, 247.e1–247.e8. [Google Scholar] [CrossRef] [PubMed]
- García-Sánchez, E.; Ávila-Gandía, V.; López-Román, J.; Martínez-Rodríguez, A.; Rubio-Arias, J.Á. What Pelvic Floor Muscle Training Load is Optimal in Minimizing Urine Loss in Women with Stress Urinary Incontinence? A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 4358. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ashton-Miller, J.A.; DeLancey, J.O. Functional anatomy of the female pelvic floor. Ann. N. Y. Acad. Sci. 2007, 1101, 266–296. [Google Scholar] [CrossRef]
- Dietz, H.P.; Wong, V.; Shek, K.L. A simplified method for determining hiatal biometry. Aust. N. Z. J. Obstet. Gynaecol. 2011, 51, 540–543. [Google Scholar] [CrossRef]
- Xiao, T.; Chen, Y.; Gan, Y.; Xu, J.; Huang, W.; Zhang, X. Can Stress Urinary Incontinence be Predicted by Ultrasound? AJR Am. J. Roentgenol. 2019, 213, 1163–1169. [Google Scholar] [CrossRef]
- Brækken, H.; MSc, I.; Majida, M.; Marie, E.E.; Bø, K. Morphological changes after pelvic floor muscle training measured by 3-dimensional ultrasonography: A randomized controlled trial. Obstet. Gynecol. 2010, 115 Pt 1, 317–324. [Google Scholar] [CrossRef] [Green Version]
- Rane, A.; Iyer, J. Posture and micturition: Does it really matter how a woman sits on the toilet? Int. Urogynecol. J. 2014, 25, 1015–1021. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Fernandez, A.; Petros, P.E. A four month squatting-based pelvic exercise regime cures day/night enuresis and bowel dysfunction in children aged 7–11 years. Cent. Eur. J. Urol. 2020, 73, 307–314. [Google Scholar]
- Anderson, K.; Behm, D.G. Trunk muscle activity increases with unstable squat movements. Can. J. Appl. Physiol. 2005, 30, 33–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wretenberg, P.; Feng, Y.; Arborelius, U.P. High- and low-bar squatting techniques during weight-training. Med. Sci. Sports Exerc. 1996, 28, 218–224. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Occupational category | Occupation in this study refers to a woman’s daily job. It was categorized according to the potential impacts of the job on the PFM as the follows: Brainwork refers to office work that had least impact on PFM. Mild manual labor refers to manual work in sitting position without heavy loads. Medium manual labor refers to manual work in standing position or moving with occasional heavy loads. Heavy manual labor refers to manual work with heavy loads that needs frequent or continuous body movement and high abdomen pressure to resist gravity. |
| Working posture | Refers to woman’s body posture when she is doing a job and is categorized according to the potential impacts of the job to the PFM as the follows: Sitting refers to a situation that a job is undertaken dominantly in sitting position. Standing refers to a situation that a job is undertaken dominantly in standing position. Others refers to a situation that a job is undertaken with posture shifting among sitting, standing, squatting, and bending, etc. |
| Toilet type | Refers to the type of toilet that a woman used for most of their defecating and is categorized according to the potential impacts on the PFM as squatting toilet dominant, sitting toilet dominant, or unspecified. |
| PFMT habit | Refers to whether a woman performed “satisfied PFMT”, which refers to PFMT at least once a week for 20 min in total in the past 3 months: Yes for performing satisfied PFMT in the past 3 months. No for not performing satisfied PFMT in the past 3 months. |
| Constipation history | Constipation refers to whether woman often felt defecation difficultly in the past 6 months and is categorized according to the potential impacts on the PFM as: Yes for often constipation in the past 6 months. No for recallable occasional constipation or no recallable constipation. |
| Smoking history | Refers to whether woman smokes or has ever smoked in her lifetime: Yes for current smoking or ever smoked. No for no smoking in her life. |
| Number of gestations | Refers to the number of gestation(s) a woman has had, including born, aborted, and in gestation. |
| Number of abortions | Refers to the number of abortion(s) a woman has had. |
| All Participants | |
|---|---|
| Age (years) | 30 (28~32) |
| Gestational weeks | 12 (11~12) |
| Pro-gestational BMI (kg/m2) | 20.80 (19.30~22.68) |
| Toilet type | |
| Sitting-toilet dominant | 322 (84.7%) |
| Squatting-toilet dominant | 54 (14.2%) |
| Not specified | 4 (1.1%) |
| PFMT habit | |
| Yes | 14 (3.7%) |
| No | 366 (96.3%) |
| POP-Q: | |
| Aa (cm) | −3.0 (−3.0~−3.0) |
| Ba (cm) | −3.0 (−3.0~−3.0) |
| Ap (cm) | −3.0 (−3.0~−3.0) |
| Bp (cm) | −3.0 (−3.0~−3.0) |
| C (cm) | −6.0 (−7.0~−6.0) |
| D (cm) | −7.5 (−8.0~−7.5) |
| Pb (cm) | 3.0 (2.5~3.5) |
| Gh (cm) | 3.0 (2.5~4.0) |
| TVL (cm) | 8.0 (7.5~8.0) |
| MOS | |
| Grade 0 | 2 (0.5%) |
| Grade 1 | 9 (2.4%) |
| Grade 2 | 42 (11.3%) |
| Grade 3 | 98 (25.8%) |
| Grade 4 | 141 (37.1%) |
| Grade 5 | 87 (22.9%) |
| Mean grade | 3.65 ± 1.058 |
| Group 1 (n = 228) | Group 2 (n = 98) | Group 3 (n = 54) | OR (95% CI) | p | |
|---|---|---|---|---|---|
| Age (years) | 30 (28~32) | 30 (28~32) | 30 (28.5~32.5) | 1.030 (0.971~1.091) | 0.329 |
| Gestational weeks | 12 (11~12) | 12 (11~12) | 12 (11~13) | 1.027 (0.909~1.160) | 0.671 |
| Pro-gestational BMI (kg/m2) | |||||
| <18.5 | 166 (72.8%) | 65 (66.3%) | 44 (81.5%) | 1 | |
| 18.5–23.9 | 22 (9.6%) | 20 (20.4%) | 6 (11.1%) | 1.461 (0.814~2.620) | 0.204 |
| 24–27.9 | 27 (11.8%) | 10 (10.2%) | 4 (7.4%) | 0.747 (0.379~1.470) | 0.398 |
| ≥28 | 13 (5.7%) | 3 (3.1%) | 0 | 0.319 (0.087~1.167) | 0.084 |
| Number of gestations | 1 (1~2) | 1 (1~1) | 1 (1~1) | 0.631 (0.428~0.930) | 0.020 |
| Number of abortions | 0 (0~1) | 0 (0~0) | 0 (0~0) | 0.698 (0.494~0.986) | 0.041 |
| Educational status | |||||
| Graduate degree | 45 (55.6%) | 21 (25.9%) | 15 (18.5%) | 1 | |
| Undergraduate | 165 (60.2%) | 73 (26.6%) | 36 (13.1%) | 0.787 (0.486~1.274) | 0.330 |
| High school | 14 (70.0%) | 3 (15.0%) | 3 (15.0%) | 0.560 (0.202~1.550) | 0.264 |
| Secondary education | 4 (80.0%) | 1 (20.0%) | 0 | 0.282 (0.029~2.721) | 0.274 |
| Occupational category | |||||
| Brainwork | 156 (61.4%) | 62 (24.4%) | 36 (14.2%) | 1 | |
| Mild manual labor | 67 (57.8%) | 33 (28.4%) | 16 (13.8%) | 1.123 (0.728~1.733) | 0.599 |
| Medium manual labor | 5 (50.0%) | 3 (30%) | 2 (20.0%) | 1.578 (0.477~5.225) | 0.455 |
| Heavy manual labor | 0 | 0 | 0 | - | - |
| Working posture | |||||
| Sitting-posture dominant | 190 (59.6%) | 85 (26.6%) | 44 (13.8%) | 1 | |
| Standing-posture dominant | 18 (54.5%) | 8 (24.2%) | 7 (21.2%) | 1.331 (0.669~2.645) | 0.415 |
| Others | 20 (71.4%) | 5 (17.9%) | 3 (10.7%) | 0.609 (0.264~1.402) | 0.244 |
| Toilet type | |||||
| Sitting-toilet dominant | 207 (64.3%) | 78 (24.2%) | 37 (11.5%) | 1 | |
| Squatting-toilet dominant | 20 (37.0%) | 18 (33.3%) | 16 (29.6%) | 3.139 (1.820~5.412) | <0.001 |
| Not specified | 1 (25%) | 2 (50%) | 1 (25%) | 3.722 (0.605~22.897) | 0.156 |
| Family history of SUI | |||||
| Yes | 6 (54.5%) | 2 (18.2%) | 3 (27.3%) | 1 | |
| No | 149 (62.1%) | 56 (23.3%) | 35 (14.6%) | 0.623 (0.198~1.958) | 0.418 |
| Unclear | 73 (32%) | 40 (31.0%) | 16 (12.4%) | 0.723 (0.225~2.321) | 0.585 |
| Family history of POP | |||||
| Yes | 0 | 0 | 0 | - | - |
| No | 156 (62.4%) | 62 (24.8%) | 32 (12.8%) | 1 | |
| Unclear | 72 (55.4%) | 36 (27.7%) | 22 (16.9%) | 1.347 (0.889~2.042) | 0.160 |
| Constipation history | |||||
| Yes | 21 (65.6%) | 8 (25%) | 3 (9.4%) | 1 | |
| No | 207 (59.5%) | 90 (25.9%) | 51 (14.7%) | 1.345 (0.636~2.845) | 0.438 |
| Smoking history | |||||
| Yes | 4 (66.7%) | 2 (33.3%) | 0 | 1 | |
| No | 224 (59.9%) | 96 (25.7%) | 54 (14.4%) | 1.559 (0.276~8.808) | 0.615 |
| PFMT habit | |||||
| Yes | 8 (57.1%) | 4 (28.6%) | 2 (14.3%) | 1 | |
| No | 220 (60.1%) | 94 (25.7%) | 52 (14.2%) | 0.906 (0.319~2.574) | 0.906 |
| Group 1 (n = 228) | Group 2 (n = 98) | Group 3 (n = 54) | OR (95% CI) | p | |
|---|---|---|---|---|---|
| Left LAM thickness (mm) | 6.50 (5.70–7.60) | 6.35 (5.40–6.80) | 6.50 (6.20–7.78) | 0.994 (0.864–1.143) | 0.930 |
| Right LAM thickness (mm) | 6.60 (5.80–7.500) | 6.50 (5.50–6.93) | 6.60 (6.60–7.63) | 1.055 (0.917–1.215) | 0.453 |
| Right–left diameter of LH (cm) | 3.80 (3.40–4.00) | 3.80 (3.60–4.10) | 3.80 (3.70–3.94) | 1.056 (1.023–1.091) | 0.001 |
| Levator hiatus area (cm2) | 13.55 (11.90–15.66) | 13.55 (11.61–14.83) | 13.55 (12.35–14.07) | 0.949 (0.889–1.013) | 0.113 |
| p | OR | 95% CI | |
|---|---|---|---|
| Number of gestations | 0.465 | 0.729 | 0.312–1.703 |
| Number of abortions | 0.788 | 0.902 | 0.425–1.916 |
| Toilet type | |||
| Sitting-toilet dominant | 1 | ||
| Squatting-toilet dominant | <0.001 | 3.140 | 1.810–5.448 |
| Not specified | 0.114 | 4.575 | 0.694–30.144 |
| Right–left diameter of LH | 0.002 | 1.055 | 1.021–1.090 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gao, L.; Wang, S.; Zhang, D.; Zhu, H.; Jia, Y.; Wang, H.; Li, S.; Fu, X.; Sun, X.; Wang, J. Pelvic Floor Muscle Strength in the First Trimester of Primipara: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 3568. https://doi.org/10.3390/ijerph19063568
Gao L, Wang S, Zhang D, Zhu H, Jia Y, Wang H, Li S, Fu X, Sun X, Wang J. Pelvic Floor Muscle Strength in the First Trimester of Primipara: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(6):3568. https://doi.org/10.3390/ijerph19063568
Chicago/Turabian StyleGao, Lei, Shiyan Wang, Di Zhang, Hongmei Zhu, Yuanyuan Jia, Haibo Wang, Suhong Li, Xiuhong Fu, Xiuli Sun, and Jianliu Wang. 2022. "Pelvic Floor Muscle Strength in the First Trimester of Primipara: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 6: 3568. https://doi.org/10.3390/ijerph19063568
APA StyleGao, L., Wang, S., Zhang, D., Zhu, H., Jia, Y., Wang, H., Li, S., Fu, X., Sun, X., & Wang, J. (2022). Pelvic Floor Muscle Strength in the First Trimester of Primipara: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(6), 3568. https://doi.org/10.3390/ijerph19063568






