Organizational Framework Conditions for Workplace Health Management in Different Settings of Nursing—A Cross-Sectional Analysis in Germany
Abstract
:1. Introduction
- −
- health promoting capacity;
- −
- social capital;
- −
- workplace health promotion (as the first pillar of WHM);
- −
- operational integration management (as the second pillar of the WHM);
- −
- occupational safety (as the third pillar of WHM);
- −
- dealing with violence and aggression (as a special burden in nursing).
2. Materials and Methods
2.1. Study Design
2.2. Instrument for the Operationalization of WHM Structures and WHM Processes (WHM Check)
2.3. Statistical Analysis
3. Results
4. Discussion
4.1. Summary of Findings
4.2. Study Aims in Context
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Slotala, L. Stellschrauben mit großer Wirkung. In Pflege-Report 2019: Mehr Personal in der Langzeitpflege-Aber Woher? Jacobs, K., Kuhlmey, A., Greß, S., Klauber, J., Schwinger, A., Eds.; Springer: Berlin/Heidelberg, Germany, 2020; pp. 71–83. ISBN 978-3-662-58934-2. [Google Scholar]
- Schwinger, A.; Klauber, J.; Tsiasioti, C. Pflegepersonal heute und morgen. In Pflege-Report 2019: Mehr Personal in der Langzeitpflege-Aber Woher? Jacobs, K., Kuhlmey, A., Greß, S., Klauber, J., Schwinger, A., Eds.; Springer: Berlin/Heidelberg, Germany, 2020; pp. 3–21. ISBN 978-3-662-58934-2. [Google Scholar]
- Sell, L.; Bültmann, U.; Rugulies, R.; Villadsen, E.; Faber, A.; Søgaard, K. Predicting long-term sickness absence and early retirement pension from self-reported work ability. Int. Arch. Occup. Environ. Health 2009, 82, 1133–1138. [Google Scholar] [CrossRef] [PubMed]
- Drupp, M.; Meyer, M. Belast ungen und Arbeitsbedingungen bei Pflegeberufen–Arbeitsunfähigkeitsdaten und ihre Nutzung im Rahmen eines Betrieblichen Gesundheitsmanagements. In Pflege-Report 2019: Mehr Personal in der Langzeitpflege-Aber Woher? Jacobs, K., Kuhlmey, A., Greß, S., Klauber, J., Schwinger, A., Eds.; Springer: Berlin/Heidelberg, Germany, 2020; pp. 23–47. ISBN 978-3-662-58934-2. [Google Scholar]
- Ehegartner, V.; Kirschneck, M.; Frisch, D.; Schuh, A.; Kus, S. Arbeitsfähigkeit von Pflegekräften in Deutschland–welchen Präventionsbedarf hat das Pflegepersonal: Ergebnisse einer Expertenbefragung. Gesundheitswesen 2020, 82, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Schablon, A.; Wendeler, D.; Kozak, A.; Nienhaus, A.; Steinke, S. Prevalence and Consequences of Aggression and Violence towards Nursing and Care Staff in Germany—A Survey. Int. J. Environ. Res. Public Health 2018, 15, 1274. [Google Scholar] [CrossRef] [Green Version]
- Krupp, E.; Hielscher, V.; Kirchen-Peters, S. Betriebliche Gesundheitsförderung in der Pflege–Umsetzungsbarrieren und Handlungsansätze. In Pflege-Report 2019: Mehr Personal in der Langzeitpflege-Aber Woher? Jacobs, K., Kuhlmey, A., Greß, S., Klauber, J., Schwinger, A., Eds.; Springer: Berlin/Heidelberg, Germany, 2020; pp. 113–122. ISBN 978-3-662-58934-2. [Google Scholar]
- Barthelmes, I.W.; Bödeker, J.; Sörensen, K.-M.; Kleinlercher, J.O. Iga.Report 40. Wirksamkeit und Nutzen Arbeitsweltbezogener Gesundheitsförderung und Prävention.: Zusammenstellung der Wissenschaftlichen Evidenz 2012-2018; Initiative Gesundheit und Arbeit: Dresden, Germany, 2019. [Google Scholar]
- Pfannstiel, M.A.; Mehlich, H. BGM–Ein Erfolgsfaktor für Unternehmen; Springer Fachmedien Wiesbaden: Wiesbaden, Germany, 2018; ISBN 978-3-658-22737-1. [Google Scholar]
- Elke, G.; Gurt, J.; Möltner, H.; Externbrink, K. Arbeitsschutz und Betriebliche Gesundheitsförderung–Vergleichende Analyse der Prädiktoren und Moderatoren Guter Praxis; Bundesanstalt für Arbeitsschutz und Arbeitsmedizin: Dortmund, Germany, 2015. [Google Scholar]
- Bauer, S.; Geiger, L.; Niggemann, R.; Seidel, J. Medizinischer Dienst des Spitzenverbandes Bund der Krankenkassen e. V. (MDS. PRÄVENTIONSBERICHT 2020: Leistungen der gesetzlichen Krankenversicherung:Primärprävention und Gesundheitsförderung. Leistungen der sozialen Pflegeversicherung:Prävention in stationären Pflegeeinrichtungen. Berichtsjahr 2019. 2020. Available online: https://md-bund.de/fileadmin/dokumente/Publikationen/GKV/Praevention/2020/Praeventionsbericht_2020_barrierefrei.pdf (accessed on 7 January 2022).
- Badura, B.; Ritter, W.; Scherf, M. Betriebliches Gesundheitsmanagement-Ein Leitfaden Für Die Praxis; Sigma: Berlin, Germany, 1999; ISBN 3894048778. [Google Scholar]
- Hoek, R.J.A.; Havermans, B.M.; Houtman, I.L.D.; Brouwers, E.P.M.; Heerkens, Y.F.; Zijlstra-Vlasveld, M.C.; Anema, J.R.; van der Beek, A.J.; Boot, C.R.L. Stress Prevention@Work: A study protocol for the evaluation of a multifaceted integral stress prevention strategy to prevent employee stress in a healthcare organization: A cluster controlled trial. BMC Public Health 2017, 18, 26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wijnen, B.F.M.; Lokkerbol, J.; Boot, C.; Havermans, B.M.; van der Beek, A.J.; Smit, F. Implementing interventions to reduce work-related stress among health-care workers: An investment appraisal from the employer's perspective. Int. Arch. Occup. Environ. Health 2020, 93, 123–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olson, R.; Wright, R.R.; Elliot, D.L.; Hess, J.A.; Thompson, S.; Buckmaster, A.; Luther, K.; Wipfli, B. The COMPASS pilot study: A total worker Health™ intervention for home care workers. J. Occup. Environ. Med. 2015, 57, 406–416. [Google Scholar] [CrossRef] [PubMed]
- Nejati, A.; Shepley, M.; Rodiek, S.; Lee, C.; Varni, J. Restorative Design Features for Hospital Staff Break Areas: A Multi-Method Study. HERD Health Environ. Res. Des. J. 2016, 9, 16–35. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.; Han, K. Associations Among Nursing Work Environment and Health-Promoting Behaviors of Nurses and Nursing Performance Quality: A Multilevel Modeling Approach. J. Nurs. Scholarsh. 2018, 50, 403–410. [Google Scholar] [CrossRef] [PubMed]
- Kleina, T.; Brause, M.; Horn, A. Potenziale und Probleme der Gesundheitsförderung bei Pflegepersonal in stationären Pflegeeinrichtungen. Gesundheitswesen 2013, 75, A75. [Google Scholar] [CrossRef]
- GKV-Spitzenverband. Leitfaden Prävention: Handlungsfelder und Kriterien nach §20 Abs.2 SGBV: Berlin, Germany, 2020. Available online: http://www.bdem.de/pdf/Leitfaden-Praevention.pdf (accessed on 5 January 2022).
- Holden, R.J.; Or, C.K.L.; Alper, S.J.; Joy Rivera, A.; Karsh, B.-T. A change management framework for macroergonomic field research. Appl. Ergon. 2008, 39, 459–474. [Google Scholar] [CrossRef] [PubMed]
- Helfrich, C.D.; Damschroder, L.J.; Hagedorn, H.J.; Daggett, G.S.; Sahay, A.; Ritchie, M.; Damush, T.; Guihan, M.; Ullrich, P.M.; Stetler, C.B. A critical synthesis of literature on the promoting action on research implementation in health services (PARIHS) framework. Implement. Sci. 2010, 5, 82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.-Y.D.; Weiner, B.J.; Harrison, M.I.; Belden, C.M. Organizational transformation: A systematic review of empirical research in health care and other industries. Med. Care Res. Rev. 2013, 70, 115–142. [Google Scholar] [CrossRef] [PubMed]
- Semenic, S.; Childerhose, J.E.; Lauzière, J.; Groleau, D. Barriers, facilitators, and recommendations related to implementing the Baby-Friendly Initiative (BFI): An integrative review. J. Hum. Lact. 2012, 28, 317–334. [Google Scholar] [CrossRef] [PubMed]
- Kotter, J.P. Change Management-Das Unternehmen erfolgreich erneuern. In Harvard-Business-Manager: Das Wissen der Besten; Harvard-Business-Manager: Hamburg, Germany, 2008; Volume 30, pp. 140–153. [Google Scholar]
- Sozialgesetzbuch Fünftes Buch—Gesetzliche Krankenversicherung, § 20f Landesrahmenvereinbarungen zur Umsetzung der nationalen Präventionsstrategie: §20f SGB V; Deutscher Bundestag: Berlin, Germany, 1988.
- Biallas, B.; Schäfer, D.; Dejonghe, L.; Franz, L.; Petrowski, K.; Froböse, I.; Wilke, C. Präventionsreife in kleinen und mittleren Unternehmen. Prävention Und Gesundh. 2019, 14, 398–402. [Google Scholar] [CrossRef] [Green Version]
- Jung, J.; Nitzsche, A.; Neumann, M.; Wirtz, M.; Kowalski, C.; Wasem, J.; Stieler-Lorenz, B.; Pfaff, H. The Worksite Health Promotion Capacity Instrument (WHPCI): Development, validation and approaches for determining companies' levels of health promotion capacity. BMC Public Health 2010, 10, 550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pfaff, H.; Nitzsche, A.; Jung, J. Handbuch zum Healthy Organisational Resources and Strategies. (HORST) Fragebogen: Forschungsbericht 03-2008; Klinikum der Universität zu Köln, Institut und Poliklinik für Arbeitsmedizin, Sozialmedizin und Sozialhygiene Abteilung Medizinische Soziologie: Cologne, Germany, 2008. [Google Scholar]
- Bourdieu, P. Ökonomisches Kapital, kulturelles Kapital, soziales Kapital. In Handbuch Bildungs-und Erziehungssoziologie, 1st ed.; Bauer, U., Bittlingmayer, U.H., Scherr, A., Eds.; VS Verlag für Sozialwissenschaften: Wiesbaden, Germany, 2012; pp. 229–242. ISBN 978-3-531-17922-3. [Google Scholar]
- Berufsgenossenschaft für Gesundheitsdienst und Wohlfahrtspflege. Selbsteinschätzung Gewalt und Aggression. Available online: https://www.bgw-online.de/SharedDocs/Downloads/DE/Arbeitssicherheit_und_Gesundheitsschutz/Organisationsberatung/Selbsteinschaetzung_Download.pdf?__blob=publicationFile (accessed on 14 December 2021).
- Deutsche Rentenversicherung Baden-Württemberg. Praxisleitfaden für Kleine und Mittelständische Unternehmen. Available online: https://kom-consulting.de/pages/BEM_Broschuere_DRV-BW-2014.pdf (accessed on 8 March 2021).
- Hammer, A.; Pfaff, A. Der Einfluss von Sozialkapital im Krankenhausmanagement auf die Implementierung von Qualitätsmanagementsystemen in europäischen Krankenhäusern. German Medical Science GMS Publishing House; Hammer, A., Pfaff, H., Eds.; Deutscher Kongress für Versorgungsforschung: Düsseldorf, Germany, 2013. [Google Scholar] [CrossRef]
- Jacobs, K.; Kuhlmey, A.; Greß, S.; Klauber, J.; Schwinger, A. Pflege-Report 2019: Mehr Personal in der Langzeitpflege-Aber Woher? Springer: Berlin/Heidelberg, Germany, 2020; ISBN 978-3-662-58934-2. [Google Scholar]
- Koinig, I.; Diehl, S. Healthy Leadership and Workplace Health Promotion as a Pre-Requisite for Organizational Health. Int. J. Environ. Res. Public Health 2021, 18, 9260. [Google Scholar] [CrossRef] [PubMed]
- BKK Dachverband. Gesundheit und Arbeit-Blickpunkt Gesundheitswesen: BKK Gesundheitsatlas 2017; MWV Medizinisch Wissenschaftliche Verlagsgesellschaft: Berlin, Germany, 2017; ISBN 978-3-95466-341-5. [Google Scholar]
- Stier-Jarmer, M.; Frisch, D.; Oberhauser, C.; Berberich, G.; Schuh, A. The Effectiveness of a Stress Reduction and Burnout Prevention Program. Dtsch. Arztebl. Int. 2016, 113, 781–788. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liese, A.; Smieszkol, C.; Wittreck, H. Sicherheit und Gesundheitsschutzbei der Pflege: Abschlussbericht zum GDA-Arbeitsprogramm; Nationale Arbeitsschutzkonferenz, Geschäftsstelle der Nationalen Arbeitsschutzkonferenz: Berlin, Germany, 2013. [Google Scholar]
- Niehaus, M.; Marfels, B.; Vater, G.; Magin, J.; Werkstetter, E. Betriebliches Eingliederungsmanagement: Studie zur Umsetzung des Betrieblichen Eingliederungsmanagements nach § 84 Abs. 2 SGB IX: (Forschungsbericht /Bundesministerium für Arbeit und Soziales, FB374). Available online: https://nbn-resolving.org/urn:nbn:de:0168-ssoar-265779 (accessed on 14 January 2022).
- Weinstein, M.; Cheddie, K. Adoption and Implementation Barriers for Worksite Health Programs in the United States. Int. J. Environ. Res. Public Health 2021, 18, 12030. [Google Scholar] [CrossRef] [PubMed]
- Faller, G. Wearable und App: Was kommt auf uns zu? Gute Arb. 2020, 12, 25–30. [Google Scholar]
- Andrade, C. The Inconvenient Truth About Convenience and Purposive Samples. Indian J. Psychol. Med. 2021, 43, 86–88. [Google Scholar] [CrossRef] [PubMed]


| Care Facilities | Home-Based LTC (5; 31%) | LTC Facility (7; 44%) | Acute Care Hospital (4; 25%) |
|---|---|---|---|
| Number of all employees (nurses and others)(mean, (± SD), [min–max], (Med)) | 146 (±153) [16–326], (49) | 91 (±27) [56–131], (93) | 532 (±415) [158–1125] (422) |
| Company size (number of all employees; nurses and others) | |||
| <10 | 0 | 0 | 0 |
| 10–49 | 3 | 0 | 0 |
| 50–249 | 0 | 7 | 1 |
| >250 | 2 | 0 | 3 |
| Main Topic | Questionnaire | Response Option |
|---|---|---|
| Health promoting capacity [26,27] | Health promoting willingness index over three items [28] | Eleven-point Likert scale (from 0 = “do not agree at all”, 10 = “fully agree”) |
| Health promoting management index over nine items [28] | Eleven-point Likert scale (from 0 = “do not agree at all”, 10 = “fully agree”) | |
| Social capital | Social capital index over nine items [28] | Four-point Likert scale (1 = “do not agree at all”, 4 = “fully agree”) |
| Workplace health promotion | Workplace health activities index over six items [28] | Eleven-point Likert scale (0 = “do not agree at all”, 10 = “fully agree”) |
| Workplace health structures and supporting cooperation partner five items [28] | Four nominal scaled response options (“yes” and “no”) One non-standardized question (“work with cooperation partner”) | |
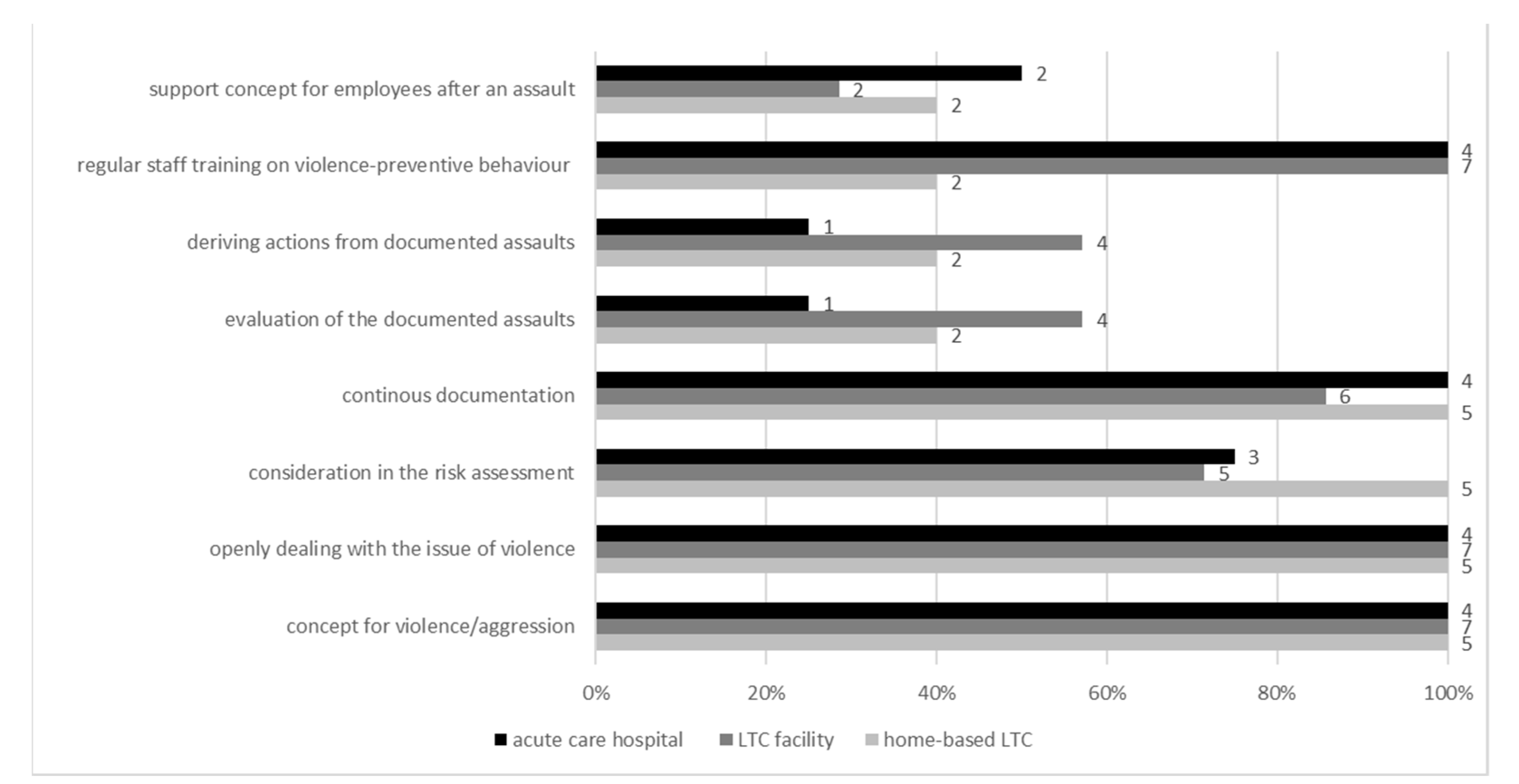
| Handling of incidents of violence and aggression | Handling of incidents of violence and aggression (against employees) eight items [30] | Nominal scaled response options (“yes” and “no”) |
| Operational integration management | Operational integration management four items [31] | Nominal scaled response options (“yes” and “no”) |
| Occupational safety | Occupational safety two items non-standardized question | Nominal scaled response options (“yes” and “no”) |
| Home-Based LTC (n = 5) | LTC Facilities (n = 7) | Acute Care Hospital (n = 4) | p * | |
|---|---|---|---|---|
| Health promoting willingness index (mean(±SD), [min:1–max:10]; (Med)) | 7.4 (±1.2) [6–9]; (7.0) | 6.8 (±1.8) [4–9]; (7.0) | 5.9 (±1.2) [4–7]; (6.0) | p = 0.368 |
| Health promoting management index (mean(±SD), [min:1–max:10]; (Med)) | 6.2 (±2.1) [4–9]; (5.8) | 5.5 (±2.9) [0–9]; (5.3) | 6.3 (±2.0) [5–9]; (5.6) | p = 0.831 |
| Social capital index (mean(±SD), [min:1–max:4]; (Med)) | 3.3 (±0.2) [3.0–3.8]; (3.4) | 3.1 (±0.4) [2.6–3.7]; (3.2) | 2.6 (±0.3) [2.3–3.9]; (2.7) | p = 0.015 |
| Workplace health activities index (mean(±SD), [min:1–max:10]; (Med)) | 6.3 (±2.6) [3–9]; (6.0) | 5.5 (±2.1) [2–9]; (6.0) | 5.1 (±1.0) [4–7]; (4.8) | p = 0.712 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bleier, H.; Lützerath, J.; Schaller, A. Organizational Framework Conditions for Workplace Health Management in Different Settings of Nursing—A Cross-Sectional Analysis in Germany. Int. J. Environ. Res. Public Health 2022, 19, 3693. https://doi.org/10.3390/ijerph19063693
Bleier H, Lützerath J, Schaller A. Organizational Framework Conditions for Workplace Health Management in Different Settings of Nursing—A Cross-Sectional Analysis in Germany. International Journal of Environmental Research and Public Health. 2022; 19(6):3693. https://doi.org/10.3390/ijerph19063693
Chicago/Turabian StyleBleier, Hannah, Jasmin Lützerath, and Andrea Schaller. 2022. "Organizational Framework Conditions for Workplace Health Management in Different Settings of Nursing—A Cross-Sectional Analysis in Germany" International Journal of Environmental Research and Public Health 19, no. 6: 3693. https://doi.org/10.3390/ijerph19063693
APA StyleBleier, H., Lützerath, J., & Schaller, A. (2022). Organizational Framework Conditions for Workplace Health Management in Different Settings of Nursing—A Cross-Sectional Analysis in Germany. International Journal of Environmental Research and Public Health, 19(6), 3693. https://doi.org/10.3390/ijerph19063693






