A Shot in the Arm for Vaccination Intention: The Media and the Health Belief Model in Three Chinese Societies
Abstract
1. Introduction
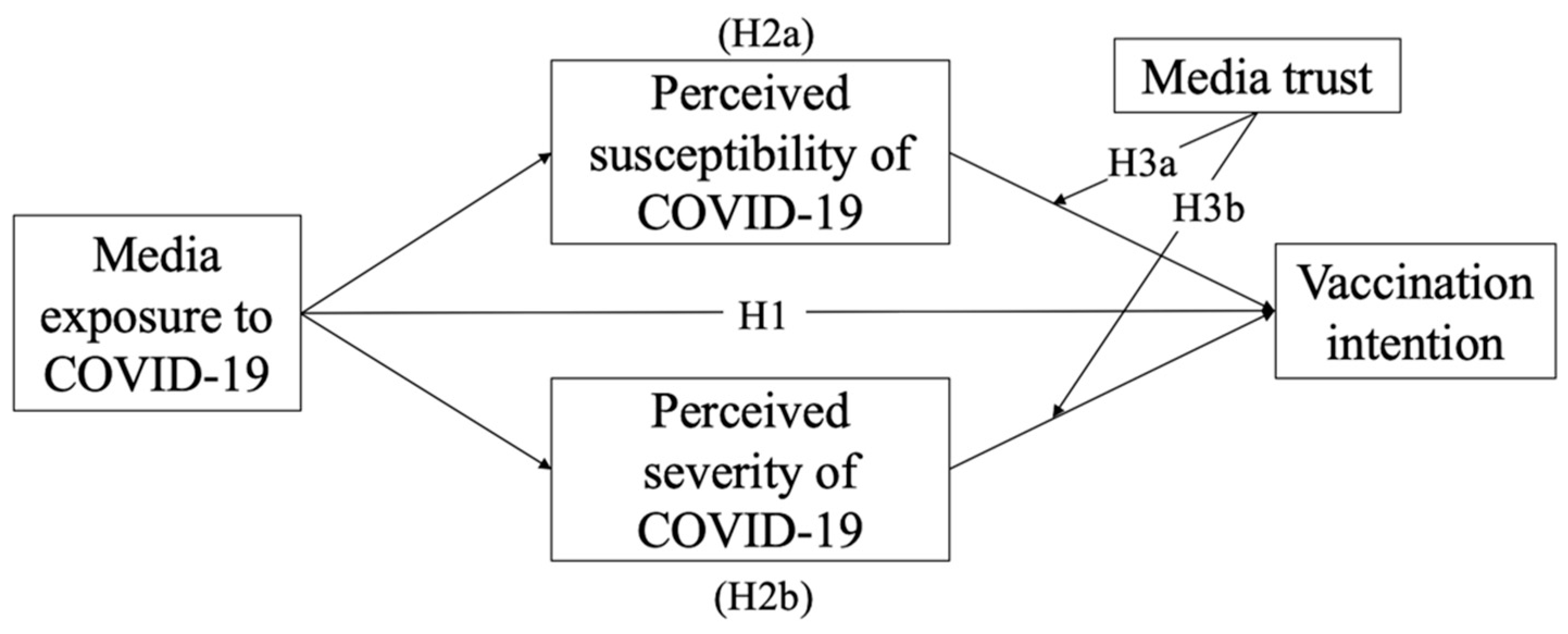
1.1. Media Exposure
1.2. Perceived Susceptibility and Perceived Severity in the HBM
1.3. Media Trust
2. Subjects and Methods
2.1. Participants and Procedure
2.2. Demographics of the Sample
2.3. Measures
3. Results
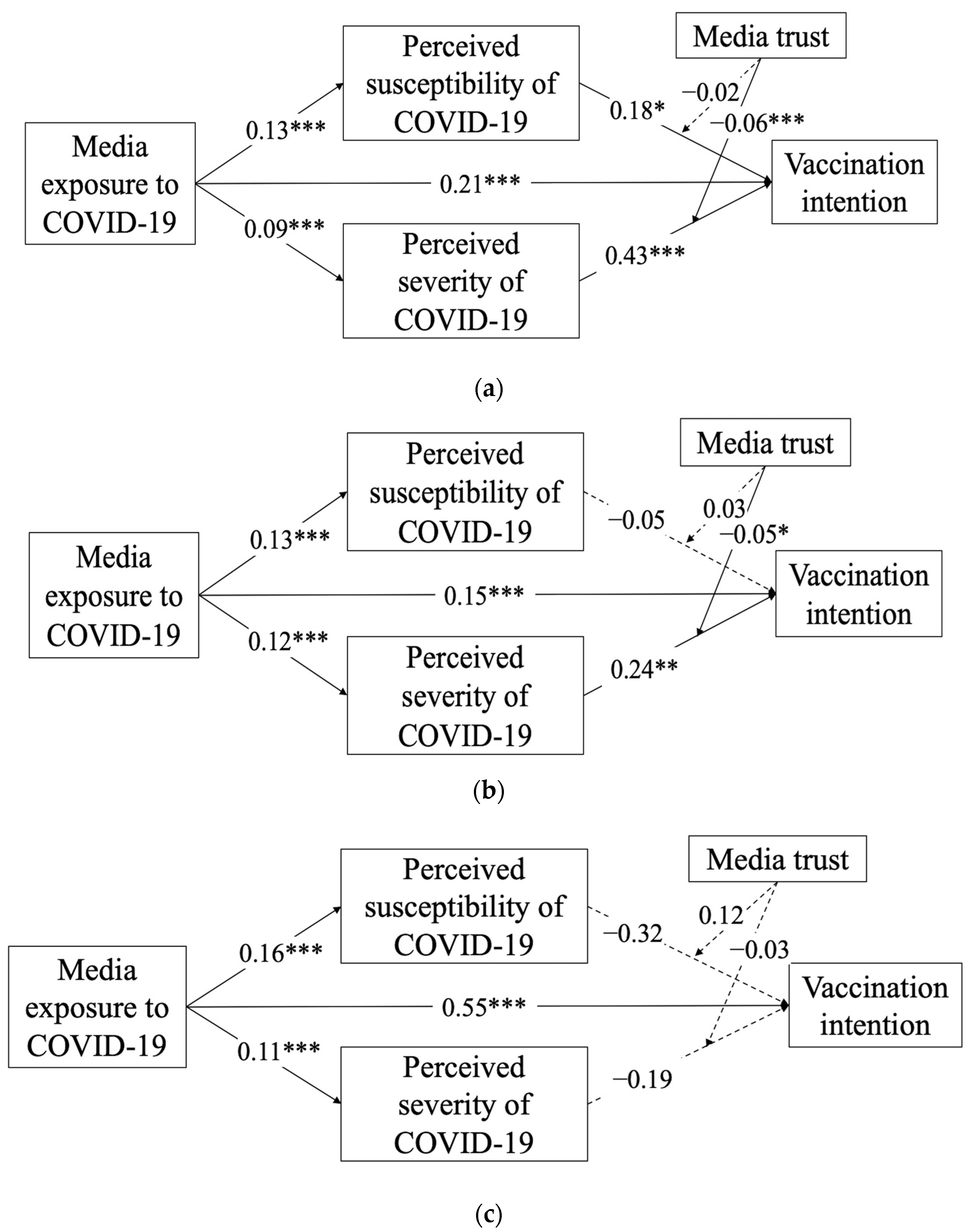
Hypotheses Testing
4. Discussion
4.1. Media Exposure—Golden Ticket to Vaccination Intention
4.2. The Mediating Effects of Perceived Susceptibility and Severity
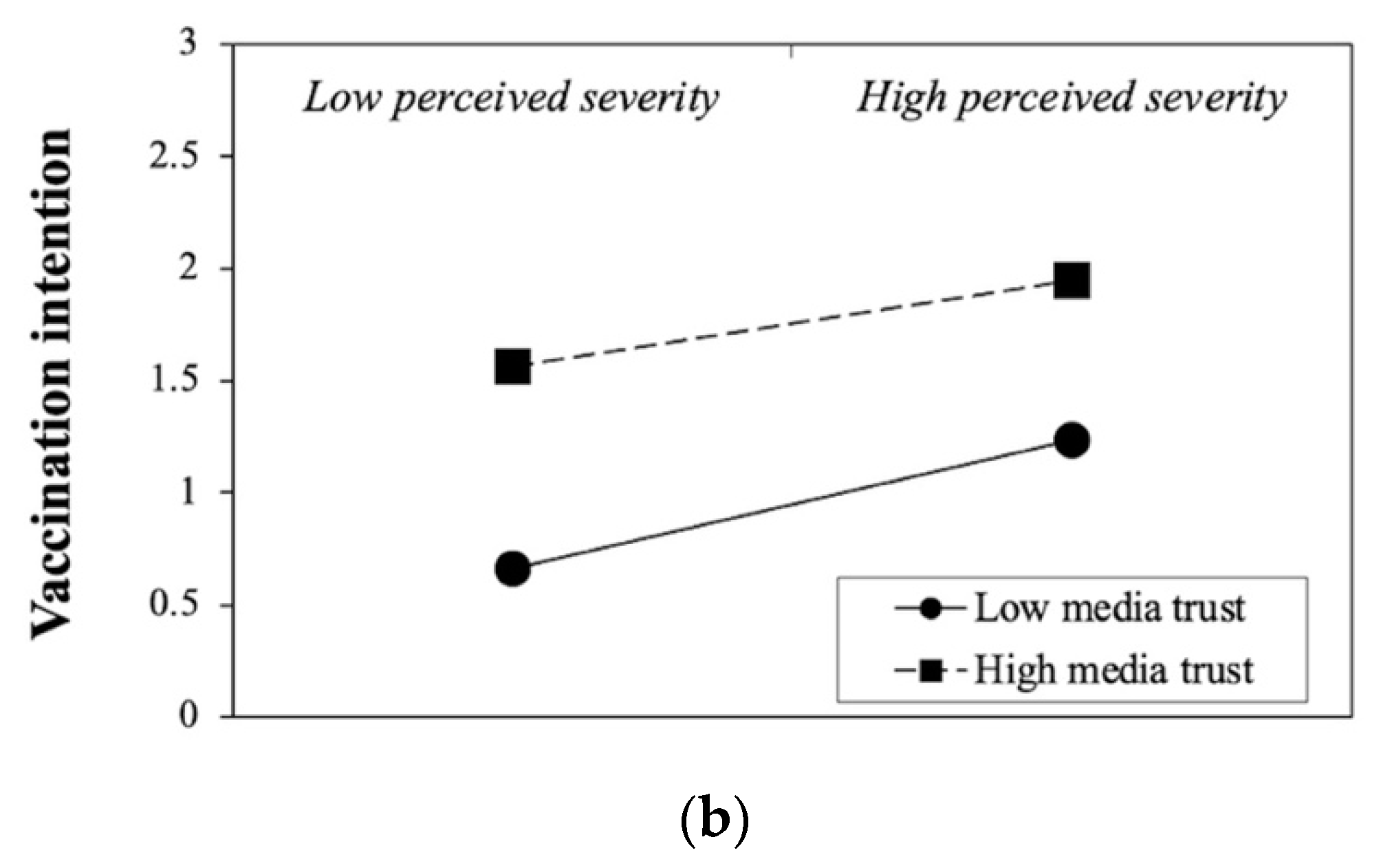
4.3. The Surprising Moderating Effect of Media Trust
4.4. Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Vaccine Efficacy, Effectiveness and Protection; WHO: Geneve, Switzerland, 2021. [Google Scholar]
- Mathieu, E.; Ritchie, H.; Ortiz-Ospina, E.; Roser, M.; Hasell, J.; Appel, C.; Giattino, C.; Rodés-Guirao, L. A global database of COVID-19 vaccinations. Nat. Hum. Behav. 2021, 5, 947–953. [Google Scholar] [CrossRef] [PubMed]
- Gellin, B. Vaccines and infectious diseases: Putting risk into perspective. In American Medical Association Briefing on Microbial Threats; National Press Club: Washington, DC, USA, 2000. [Google Scholar]
- Zhu, D.; Lv, M.; Bai, Y.; Wu, J.; He, P. Cost-effectiveness analysis of quadrivalent seasonal influenza vaccines in Beijing: A modeling analysis. Vaccine 2022, 40, 994–1000. [Google Scholar] [CrossRef] [PubMed]
- Fiore, A.E.; Bridges, C.B.; Cox, N.J. Seasonal influenza vaccines. Vaccines Pandemic Influenza 2009, 333, 43–82. [Google Scholar]
- Chang, Y.; Brewer, N.T.; Rinas, A.C.; Schmitt, K.; Smith, J.S. Evaluating the impact of human papillomavirus vaccines. Vaccine 2009, 27, 4355–4362. [Google Scholar] [CrossRef] [PubMed]
- Tartof, S.Y.; Slezak, J.M.; Fischer, H.; Hong, V.; Ackerson, B.K.; Ranasinghe, O.N.; Frankland, T.B.; Ogun, O.A.; Zamparo, J.M.; Gray, S. Effectiveness of mRNA BNT162b2 COVID-19 vaccine up to 6 months in a large integrated health system in the USA: A retrospective cohort study. Lancet 2021, 398, 1407–1416. [Google Scholar] [CrossRef]
- Lopez Bernal, J.; Andrews, N.; Gower, C.; Gallagher, E.; Simmons, R.; Thelwall, S.; Stowe, J.; Tessier, E.; Groves, N.; Dabrera, G.; et al. Effectiveness of Covid-19 Vaccines against the B.1.617.2 (Delta) Variant. N. Engl. J. Med. 2021, 385, 585–594. [Google Scholar] [CrossRef]
- Dean, N.E.; Hogan, J.W.; Schnitzer, M.E. Covid-19 vaccine effectiveness and the test-negative design. N. Engl. J. Med. 2021, 385, 1431–1433. [Google Scholar] [CrossRef]
- World Health Organization. Leaders Make Urgent Call to Accelerate Vaccination Globally and In Africa; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Kaleem, J.; Castleman, T.; Read, R. Why are vaccination rates so low? We found the worst county in each state and asked the politicians. The Los Angeles Times, 9 August 2021. Available online: https://www.latimes.com/world-nation/story/2021-08-09/la-na-least-vaccinated-covid-coronavirus (accessed on 9 August 2021).
- Our World in Data. Coronavirus (COVID-19) Vaccinations. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 9 December 2021).
- World Health Organization. Ten Threats to Global Health in 2019; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- World Health Organization. COVID-19 Vaccine Communications Webinar Series: Co-Convened by the World Health Organization, UNICEF and Religions for Peace, Part 2; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Chan, P.K.; Wong, M.C.; Wong, E.L. Vaccine hesitancy and COVID-19 vaccination in Hong Kong. Hong Kong Med. J. 2021, 27, 90–91. [Google Scholar] [CrossRef]
- Garfin, D.R.; Silver, R.C.; Holman, E.A. The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure. Health Psychol. 2020, 39, 355. [Google Scholar] [CrossRef]
- Nguyen, H.; Nguyen, A. Covid-19 misinformation and the social (media) amplification of risk: A Vietnamese perspective. Media Commun. 2020, 8, 444–447. [Google Scholar] [CrossRef]
- Strekalova, Y.A.; Krieger, J.L. Social Amplification of Risk in Health and Risk Messaging. Oxf. Res. Encycl. Commun. 2017. [Google Scholar] [CrossRef]
- Chen, W.; Stoecker, C. Mass media coverage and influenza vaccine uptake. Vaccine 2020, 38, 271–277. [Google Scholar] [CrossRef]
- Cao, B.; Gupta, S.; Wang, J.; Hightow-Weidman, L.B.; Muessig, K.E.; Tang, W.; Pan, S.; Pendse, R.; Tucker, J.D. Social media interventions to promote HIV testing, linkage, adherence, and retention: Systematic review and meta-analysis. J. Med. Internet Res. 2017, 19, e394. [Google Scholar] [CrossRef] [PubMed]
- Asare, M.; Lanning, B.A.; Isada, S.; Rose, T.; Mamudu, H.M. Feasibility of Utilizing Social Media to Promote HPV Self-Collected Sampling among Medically Underserved Women in a Rural Southern City in the United States (U.S.). Int. J. Environ. Res. Public Health 2021, 18, 10820. [Google Scholar] [CrossRef]
- On, J.; Park, H.-A.; Song, T.-M. Sentiment Analysis of Social Media on Childhood Vaccination: Development of an Ontology. J. Med. Internet Res. 2019, 21, e13456. [Google Scholar] [CrossRef] [PubMed]
- Ortiz, R.R.; Smith, A.; Coyne-Beasley, T. A systematic literature review to examine the potential for social media to impact HPV vaccine uptake and awareness, knowledge, and attitudes about HPV and HPV vaccination. Hum. Vaccines Immunother. 2019, 15, 1465–1475. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Featherstone, J.D.; Calabrese, C.; Wojcieszak, M. Effects of fact-checking social media vaccine misinformation on attitudes toward vaccines. Prev. Med. 2021, 145, 106408. [Google Scholar] [CrossRef] [PubMed]
- Kohring, M.; Matthes, J. Trust in news media: Development and validation of a multidimensional scale. Commun. Res. 2007, 34, 231–252. [Google Scholar] [CrossRef]
- Lin, W.-Y.; Zhang, X.; Song, H.; Omori, K. Health information seeking in the Web 2.0 age: Trust in social media, uncertainty reduction, and self-disclosure. Comput. Hum. Behav. 2016, 56, 289–294. [Google Scholar] [CrossRef]
- Rosenstock, I. Why people use health services. Milbank Meml. Fund. Q. 1966, 44, 94–127. [Google Scholar] [CrossRef]
- Harrison, J.A.; Mullen, P.D.; Green, L.W. A meta-analysis of studies of the health belief model with adults. Health Educ. Res. 1992, 7, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, C.J. A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Commun. 2010, 25, 661–669. [Google Scholar] [CrossRef]
- World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19); WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Liu, D.; Komissarov, A.S. Coronavirus as a Political Factor: Western and Chinese Versions of SARS-CoV-2 Origin and the Ways of Its Treatment. Beac. J. Stud. Ideol. Ment. Dimens. 2021, 4, 020310371. [Google Scholar] [CrossRef]
- Huang, Y.-H. A revisit of symmetrical communication from an international perspective: Status, effect, and future research directions. In The Future of Excellence in Public Relations and Communication Management: Challenges for the Next Generation; Routledge: London, UK, 2007; pp. 235–262. [Google Scholar]
- Huang, Y.-H. Theorizing Chinese communication research: A holistic framework for comparative studies. Chin. J. Commun. 2010, 3, 95–113. [Google Scholar] [CrossRef]
- Huang, Y.-H.C.; Lu, Y.; Kao, L.; Choy, C.H.Y.; Chang, Y.-t. Mainframes and mandarins: The impact of internet use on institutional trust in East Asia. Telecommun. Policy 2020, 44, 101912. [Google Scholar] [CrossRef]
- Slater, M.D. Operationalizing and analyzing exposure: The foundation of media effects research. J. Mass Commun. Q. 2004, 81, 168–183. [Google Scholar] [CrossRef]
- Moorhead, S.A.; Hazlett, D.E.; Harrison, L.; Carroll, J.K.; Irwin, A.; Hoving, C. A new dimension of health care: Systematic review of the uses, benefits, and limitations of social media for health communication. J. Med. Internet Res. 2013, 15, e1933. [Google Scholar] [CrossRef] [PubMed]
- Balatsoukas, P.; Kennedy, C.M.; Buchan, I.; Powell, J.; Ainsworth, J. The role of social network technologies in online health promotion: A narrative review of theoretical and empirical factors influencing intervention effectiveness. J. Med. Internet Res. 2015, 17, e3662. [Google Scholar] [CrossRef]
- Flay, B.R.; DiTecco, D.; Schlegel, R.P. Mass media in health promotion: An analysis using an extended information-processing model. Health Educ. Q. 1980, 7, 127–147. [Google Scholar] [CrossRef]
- Santoro, E.; Castelnuovo, G.; Zoppis, I.; Mauri, G.; Sicurello, F. Social media and mobile applications in chronic disease prevention and management. Front. Psychol. 2015, 6, 567. [Google Scholar] [CrossRef]
- Pearl, R.L.; Dovidio, J.F.; Puhl, R.M.; Brownell, K.D. Exposure to weight-stigmatizing media: Effects on exercise intentions, motivation, and behavior. J. Health Commun. 2015, 20, 1004–1013. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.J.; Coughlin, S.S.; Lyons, E.J. Social media and mobile technology for cancer prevention and treatment. Am. Soc. Clin. Oncol. Educ. Book 2017, 37, 128–137. [Google Scholar] [CrossRef] [PubMed]
- LaCroix, J.M.; Snyder, L.B.; Huedo-Medina, T.B.; Johnson, B.T. Effectiveness of mass media interventions for HIV prevention, 1986–2013: A meta-analysis. JAIDS J. Acquir. Immune Defic. Syndr. 2014, 66, S329–S340. [Google Scholar] [CrossRef] [PubMed]
- Nunez-Smith, M.; Wolf, E.; Huang, H.M.; Chen, P.G.; Lee, L.; Emanuel, E.J.; Gross, C.P. Media exposure and tobacco, illicit drugs, and alcohol use among children and adolescents: A systematic review. Subst. Abus. 2010, 31, 174–192. [Google Scholar] [CrossRef] [PubMed]
- Woo, H.; Cho, Y.; Shim, E.; Lee, J.-K.; Lee, C.-G.; Kim, S.H. Estimating influenza outbreaks using both search engine query data and social media data in South Korea. J. Med. Internet Res. 2016, 18, e4955. [Google Scholar] [CrossRef] [PubMed]
- Odone, A.; Ferrari, A.; Spagnoli, F.; Visciarelli, S.; Shefer, A.; Pasquarella, C.; Signorelli, C. Effectiveness of interventions that apply new media to improve vaccine uptake and vaccine coverage: A systematic review. Hum. Vaccines Immunother. 2015, 11, 72–82. [Google Scholar] [CrossRef] [PubMed]
- Gollust, S.E.; LoRusso, S.M.; Nagler, R.H.; Fowler, E.F. Understanding the role of the news media in HPV vaccine uptake in the United States: Synthesis and commentary. Hum. Vaccines Immunother. 2016, 12, 1430–1434. [Google Scholar] [CrossRef]
- Lin, C.A.; Lagoe, C. Effects of news media and interpersonal interactions on H1N1 risk perception and vaccination intent. Commun. Res. Rep. 2013, 30, 127–136. [Google Scholar] [CrossRef]
- Benis, A.; Khodos, A.; Ran, S.; Levner, E.; Ashkenazi, S. Social Media Engagement and Influenza Vaccination during the COVID-19 Pandemic: Cross-sectional Survey Study. J. Med. Internet Res. 2021, 23, e25977. [Google Scholar] [CrossRef]
- Puri, N.; Coomes, E.A.; Haghbayan, H.; Gunaratne, K. Social media and vaccine hesitancy: New updates for the era of COVID-19 and globalized infectious diseases. Hum. Vaccines Immunother. 2020, 16, 2586–2593. [Google Scholar] [CrossRef]
- Li, X.; Liu, Q. Social media use, eHealth literacy, disease knowledge, and preventive behaviors in the COVID-19 pandemic: Cross-sectional study on Chinese netizens. J. Med. Internet Res. 2020, 22, e19684. [Google Scholar] [CrossRef] [PubMed]
- Gehrau, V.; Fujarski, S.; Lorenz, H.; Schieb, C.; Blöbaum, B. The Impact of Health Information Exposure and Source Credibility on COVID-19 Vaccination Intention in Germany. Int. J. Environ. Res. Public Health 2021, 18, 4678. [Google Scholar] [CrossRef] [PubMed]
- Lo, S.-Y.; Li, S.-C.S.; Wu, T.-Y. Exploring Psychological Factors for COVID-19 Vaccination Intention in Taiwan. Vaccines 2021, 9, 764. [Google Scholar] [CrossRef] [PubMed]
- Strecher, V.J.; Rosenstock, I.M. The Health Belief Model; Jossey-Bass: San Francisco, CA, USA, 1997. [Google Scholar]
- Witte, K. Putting the fear back into fear appeals: The extended parallel process model. Commun. Monogr. 1992, 59, 329–349. [Google Scholar] [CrossRef]
- Champion, V.L.; Monahan, P.O.; Springston, J.K.; Russell, K.; Zollinger, T.W.; Saywell, R.M., Jr.; Maraj, M. Measuring mammography and breast cancer beliefs in African American women. J. Health Psychol. 2008, 13, 827–837. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.L.; Jensen, J.D.; Scherr, C.L.; Brown, N.R.; Christy, K.; Weaver, J. The health belief model as an explanatory framework in communication research: Exploring parallel, serial, and moderated mediation. Health Commun. 2015, 30, 566–576. [Google Scholar] [CrossRef] [PubMed]
- El-Toukhy, S. Parsing susceptibility and severity dimensions of health risk perceptions. J. Health Commun. 2015, 20, 499–511. [Google Scholar] [CrossRef]
- Janz, N.K.; Becker, M.H. The health belief model: A decade later. Health Educ. Q. 1984, 11, 1–47. [Google Scholar] [CrossRef]
- Sukeri, S.; Zahiruddin, W.M.; Shafei, M.N.; Hamat, R.A.; Osman, M.; Jamaluddin, T.Z.M.T.; Daud, A.B. Perceived severity and susceptibility towards leptospirosis infection in Malaysia. Int. J. Environ. Res. Public Health 2020, 17, 6362. [Google Scholar] [CrossRef]
- Van der Snoek, E.M.; de Wit, J.B.; Götz, H.M.; Mulder, P.G.; Neumann, M.H.; van der Meijden, W.I. Incidence of sexually transmitted diseases and HIV infection in men who have sex with men related to knowledge, perceived susceptibility, and perceived severity of sexually transmitted diseases and HIV infection: Dutch MSM–cohort study. Sex. Transm. Dis. 2006, 33, 193–198. [Google Scholar] [CrossRef]
- Yang, Z.J. Predicting young adults’ intentions to get the H1N1 vaccine: An integrated model. J. Health Commun. 2015, 20, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Huang, Y.-H.C.; Wu, Q.; Fong, I.W.-Y. Exploring the Effects of Instructional Message Strategies on Risk Perceptions and Behavioral Intentions: The Case of a Substandard Vaccine Incident. SAGE Open 2021, 11, 21582440211061525. [Google Scholar] [CrossRef]
- Zhang, X.; Zhou, S. Clicking health risk messages on social media: Moderated mediation paths through perceived threat, perceived efficacy, and fear arousal. Health Commun. 2019, 34, 1359–1368. [Google Scholar] [CrossRef]
- Mahmood, Q.K.; Jafree, S.R.; Mukhtar, S.; Fischer, F. Social Media Use, Self-Efficacy, Perceived Threat, and Preventive Behavior in Times of COVID-19: Results of a Cross-Sectional Study in Pakistan. Front. Psychol. 2021, 12, 2354. [Google Scholar] [CrossRef] [PubMed]
- Bodelet, C.; Bodelet, J.; Landelle, C.; Gauchet, A. Seasonal flu vaccination, a matter of emotion? An experimental study on role of compassion, socioeconomic status and perceived threat among healthcare workers. Psychol. Health 2021, 36, 1461–1479. [Google Scholar] [CrossRef] [PubMed]
- Khubchandani, J.; Sharma, S.; Price, J.H.; Wiblishauser, M.J.; Sharma, M.; Webb, F.J. COVID-19 vaccination hesitancy in the United States: A rapid national assessment. J. Commun. Health 2021, 46, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Song, Z.; Liu, X.; Xiang, P.; Lin, Y.; Dai, L.; Guo, Y.; Liao, J.; Chen, Y.; Liang, Y.; Sun, Y. The Current Status of Vaccine Uptake and the Impact of COVID-19 on Intention to Vaccination in Patients with COPD in Beijing. Int. J. Chronic Obstr. Pulm. Dis. 2021, 16, 3337. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Dean, J.; Yin, Y.; Wang, D.; Sun, Y.; Zhao, Z.; Wang, J. Determinants of COVID-19 Vaccine Acceptance and Hesitancy: A Health Care Student-Based Online Survey in Northwest China. Front. Public Health 2021, 9, 777565. [Google Scholar] [CrossRef]
- Niu, Z.; Willoughby, J.; Zhou, R. Associations of Health Literacy, Social Media Use, and Self-Efficacy With Health Information–Seeking Intentions Among Social Media Users in China: Cross-sectional Survey. J. Med. Internet Res. 2021, 23, e19134. [Google Scholar] [CrossRef]
- Liu, C.; Liu, Y. Media exposure and anxiety during COVID-19: The mediation effect of media vicarious traumatization. Int. J. Environ. Res. Public Health 2020, 17, 4720. [Google Scholar] [CrossRef]
- Jones, C.J.; Smith, H.; Llewellyn, C. Evaluating the effectiveness of health belief model interventions in improving adherence: A systematic review. Health Psychol. Rev. 2014, 8, 253–269. [Google Scholar] [CrossRef]
- Fishbein, M.; Cappella, J.N. The role of theory in developing effective health communications. J. Commun. 2006, 56, S1–S17. [Google Scholar] [CrossRef]
- Schoorman, F.D.; Mayer, R.C.; Davis, J.H. An integrative model of organizational trust: Past, present, and future. Acad. Manag. Rev. 2007, 32, 344–354. [Google Scholar] [CrossRef]
- Pavlou, P.A. Consumer acceptance of electronic commerce: Integrating trust and risk with the technology acceptance model. Int. J. Electron. Commer. 2003, 7, 101–134. [Google Scholar]
- Lee, C. ICT standards: Building a trusted information society [commentary]. IEEE Commun. Mag. 2015, 53, 5. [Google Scholar] [CrossRef]
- Brown-Johnson, C.G.; Boeckman, L.M.; White, A.H.; Burbank, A.D.; Paulson, S.; Beebe, L.A. Trust in health information sources: Survey analysis of variation by sociodemographic and tobacco use status in Oklahoma. JMIR Public Health Surveill. 2018, 4, e6260. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Liu, D.; Dong, Y. Self-esteem and problematic smartphone use among adolescents: A moderated mediation model of depression and interpersonal trust. Front. Psychol. 2019, 10, 2872. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.-H.C.; Wang, X.; Fong, I.W.-Y.; Wu, Q. Examining the Role of Trust in Regulators in Food Safety Risk Assessment: A Cross-regional Analysis of Three Chinese Societies Using an Integrative Framework. SAGE Open 2021, 11, 21582440211061579. [Google Scholar] [CrossRef]
- Lee, C.-J.; Hornik, R.C. Physician trust moderates the Internet use and physician visit relationship. J. Health Commun. 2009, 14, 70–76. [Google Scholar] [CrossRef]
- Meyer, P. Defining and measuring credibility of newspapers: Developing an index. J. Q. 1988, 65, 567–574. [Google Scholar] [CrossRef]
- Williams, A.E. Trust or bust?: Questioning the relationship between media trust and news attention. J. Broadcast. Electron. Media 2012, 56, 116–131. [Google Scholar] [CrossRef]
- Strömbäck, J.; Tsfati, Y.; Boomgaarden, H.; Damstra, A.; Lindgren, E.; Vliegenthart, R.; Lindholm, T. News media trust and its impact on media use: Toward a framework for future research. Ann. Int. Commun. Assoc. 2020, 44, 139–156. [Google Scholar] [CrossRef]
- Tsfati, Y.; Ariely, G. Individual and contextual correlates of trust in media across 44 countries. Commun. Res. 2014, 41, 760–782. [Google Scholar] [CrossRef]
- Tokuda, Y.; Fujii, S.; Jimba, M.; Inoguchi, T. The relationship between trust in mass media and the healthcare system and individual health: Evidence from the AsiaBarometer Survey. BMC Med. 2009, 7, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Liuccio, M.; Lu, J. Mobile Media and Trust in Sources of Health Information: A Comparative Study in 26 European Countries. La Clin. Ter. 2020, 171, e321–e327. [Google Scholar] [PubMed]
- Wu, Y.; Shen, F. Exploring the impacts of media use and media trust on health behaviors during the COVID-19 pandemic in China. J. Health Psychol. 2021, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Taha, S.A.; Matheson, K.; Anisman, H. The 2009 H1N1 influenza pandemic: The role of threat, coping, and media trust on vaccination intentions in Canada. J. Health Commun. 2013, 18, 278–290. [Google Scholar] [CrossRef] [PubMed]
- Moy, P.; Scheufele, D.A. Media effects on political and social trust. J. Mass Commun. Q. 2000, 77, 744–759. [Google Scholar] [CrossRef]
- Hmielowski, J.D.; Feldman, L.; Myers, T.A.; Leiserowitz, A.; Maibach, E. An attack on science? Media use, trust in scientists, and perceptions of global warming. Public Underst. Sci. 2014, 23, 866–883. [Google Scholar] [CrossRef] [PubMed]
- Porumbescu, G.A. Comparing the effects of e-government and social media use on trust in government: Evidence from Seoul, South Korea. Public Manag. Rev. 2016, 18, 1308–1334. [Google Scholar] [CrossRef]
- Schranz, M.; Schneider, J.; Eisenegger, M. Media trust and media use. In Trust in Media and Journalism; Springer: Berlin/Heidelberg, Germany, 2018; pp. 73–91. [Google Scholar]
- Hopmann, D.N.; Shehata, A.; Strömbäck, J. Contagious media effects: How media use and exposure to game-framed news influence media trust. Mass Commun. Soc. 2015, 18, 776–798. [Google Scholar] [CrossRef]
- Jiang, X.; Hwang, J.; Shah, D.V.; Ghosh, S.; Brauer, M. News attention and social-distancing behavior amid covid-19: How media trust and social norms moderate a mediated relationship. Health Commun. 2021, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.T.; Bautista, J.R. Predicting intention to take protective measures during haze: The roles of efficacy, threat, media trust, and affective attitude. J. Health Commun. 2016, 21, 790–799. [Google Scholar] [CrossRef] [PubMed]
- International Update: Covid Delta Variant Sweeps Across China—Infections Reach 19 of 31 Provinces. Pharmaceutical Technology. Available online: https://www.pharmaceutical-technology.com/special-focus/covid-19/international-update-covid-delta-variant-sweeps-across-china-infections-reach-19-of-31-provinces/ (accessed on 3 November 2021).
- Brislin, R.W. Back-translation for cross-cultural research. J. Cross-Cult. Psychol. 1970, 1, 185–216. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Champion, V.L. Revised susceptibility, benefits, and barriers scale for mammography screening. Res. Nurs. Health 1999, 22, 341–348. [Google Scholar] [CrossRef]
- Yang, J.Z.; Pittman, M.M. The silver lining of shame: Framing HPV to influence vaccination intentions. Health Commun. 2017, 32, 987–994. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2017. [Google Scholar]
- Hayes, A.F. PROCESS: A Versatile Computational Tool for Observed Variable Mediation, Moderation, and Conditional Process Modeling [White Paper]. 2012. Available online: http://www.afhayes.com/public/process2012.pdf (accessed on 9 August 2021).
- Smith, M.E.; Reid, D.M.; Jones, C.E.; Jordan, J.V.; Kautz, C.A.; Shulman, N.R. Binding of quinine-and quinidine-dependent drug antibodies to platelets is mediated by the Fab domain of the immunoglobulin G and is not Fc dependent. J. Clin. Investig. 1987, 79, 912–917. [Google Scholar] [CrossRef]
- Kühner, M.K.; Raetzke, P.B. The effect of health beliefs on the compliance of periodontal patients with oral hygiene instructions. J. Periodontol. 1989, 60, 51–56. [Google Scholar] [CrossRef]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Wendt, A.E. The agent-structure problem in international relations theory. Int. Organ. 1987, 41, 335–370. [Google Scholar] [CrossRef]
- Hsu, F.; Hioe, B.; Liu, W. Collective Statement on Taiwan Independence: Building Global Solidarity and Rejecting US Military Empire. Am. Q. 2017, 69, 465–468. [Google Scholar] [CrossRef]
- Soon, L.G. Differences in ethical judgement between Chinese and Singaporeans: Individual reactions to self and organisational interest considerations. Singap. Manag. Rev. 2003, 25, 1–25. [Google Scholar]
- Laaksonen, T.; Pajunen, K.; Kulmala, H.I. Co-evolution of trust and dependence in customer–supplier relationships. Ind. Mark. Manag. 2008, 37, 910–920. [Google Scholar] [CrossRef]
- Singh, M.P. Trust as dependence: A logical approach. In Proceedings of the 10th International Conference on Autonomous Agents and Multiagent Systems, Taipei Taiwan, 2–6 May 2011; Volume 2, pp. 863–870. [Google Scholar]
- Wang, J.; Zhu, H.; Lai, X.; Zhang, H.; Huang, Y.; Feng, H.; Lyu, Y.; Jing, R.; Guo, J.; Fang, H. From COVID-19 Vaccination Intention to Actual Vaccine Uptake: A Longitudinal Study Among Chinese Adults After Six Months of a National Vaccination Campaign. Expert Rev. Vaccines 2021, 21, 385–395. [Google Scholar] [CrossRef] [PubMed]
- Xin Hua News. The third wave of pandemic in Hong Kong is Controlled. Xin Hua News, 2020; S61–S62. Available online: http://www.xinhuanet.com/gangao/2020-09/25/c_1126542087.htm (accessed on 9 August 2021).
- Sakwa, R. Pandemic and New Division of the World. Beac. J. Stud. Ideol. Ment. Dimens. 2021, 4, 010110339. [Google Scholar] [CrossRef]
- Huang, Y.-H.; Bedford, O.; Zhang, Y. The relational orientation framework for examining culture in Chinese societies. Cult. Psychol. 2018, 24, 477–490. [Google Scholar] [CrossRef]

| Mainland | Taiwan | Hong Kong | |
|---|---|---|---|
| Gender (male: female) | 1:1.004 | 1:1.278 | 1:1.128 |
| Age (over 40) | 53.3% | 29.7% | 59% |
| Monthly household income (Mean) | CNY 15,001–25,000 (USD 2330–3885) | TWD 40,001–50,000 (USD 1424–1780) | HKD 30,001–40,000 (USD 3857–5142) |
| Education (at least B.A.) | 57.5% | 71% | 35.3% |
| Top residential areas | Guangdong Province (7%) Anhui Province (6.8%) Jiangsu Province (6.8%) | New Taipei City (20%) Taipei City (14.5%) | New Territories (50%) Kowloon (32.1%) Hong Kong Island (17.5%) |
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| Mainland China (n = 3389) | |||||
| 1. Media exposure to COVID-19 pandemic | - | ||||
| 2. Perceived susceptibility of COVID-19 | 0.13 *** | - | |||
| 3. Perceived severity of COVID-19 | 0.10 *** | 0.51 *** | - | ||
| 4. Media trust | 0.39 *** | 0.21 *** | 0.16 *** | - | |
| 5. Vaccination intention | 0.31 *** | 0.17 *** | 0.25 *** | 0.41 *** | - |
| Taiwan (n = 3000) | |||||
| 1. Media exposure to COVID-19 pandemic | - | ||||
| 2. Perceived susceptibility of COVID-19 | 0.11 *** | - | |||
| 3. Perceived severity of COVID-19 | 0.07 *** | 0.54 *** | - | ||
| 4. Media trust | 0.29 *** | 0.15 *** | 0.07 *** | - | |
| 5. Vaccination intention | 0.17 *** | 0.17 *** | 0.13 *** | 0.24 *** | - |
| Hong Kong (n = 3248) | |||||
| 1. Media exposure to COVID-19 pandemic | - | ||||
| 2. Perceived susceptibility of COVID-19 | 0.14 *** | - | |||
| 3. Perceived severity of COVID-19 | 0.10 *** | 0.28 *** | - | ||
| 4. Media trust | 0.33 *** | 0.05 ** | −0.03 | - | |
| 5. Vaccination intention | 0.20 *** | 0.03 | −0.07 *** | 0.25 *** | - |
| Mediators | Perceived Susceptibility | Perceived Severity | ||||||
|---|---|---|---|---|---|---|---|---|
| β | p | B (Boot SE) | Boot 95% CI | β | p | B (Boot SE) | Boot 95% CI | |
| Mainland | 0.07 | < 0.001 | 0.009 (0.003) | [0.004, 0.015] | 0.13 | < 0.001 | 0.012 (0.004) | [0.006, 0.020] |
| Taiwan | 0.08 | < 0.001 | 0.011 (0.004) | [0.004, 0.021] | 0.05 | < 0.05 | 0.006 (0.003) | [0.001, 0.012] |
| HK | 0.14 | < 0.05 | 0.023 (0.014) | [−0.003, 0.053] | −0.35 | < 0.001 | −0.040 (0.010) | [−0.062, −0.021] |
| Mediators | Perceived Susceptibility | Perceived Severity | ||||||
|---|---|---|---|---|---|---|---|---|
| β | p | B (Boot SE) | Boot 95% CI | β | p | B (Boot SE) | Boot 95% CI | |
| Mainland | −0.02 | 0.07 | −0.003 (0.003) | [−0.009, 0.002] | −0.06 | < 0.001 | −0.006 (0.002) | [−0.011, −0.002] |
| Taiwan | 0.03 | 0.21 | 0.003 (0.004) | [−0.004, 0.012] | −0.05 | < 0.05 | −0.006 (0.003) | [−0.013, −0.001] |
| HK | 0.12 | 0.06 | 0.020 (0.014) | [−0.006, 0.048] | −0.03 | 0.66 | −0.004 (0.010) | [−0.023, 0.015] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, R.; Huang, Y.-H.C.; Sun, J.; Lau, J.; Cai, Q. A Shot in the Arm for Vaccination Intention: The Media and the Health Belief Model in Three Chinese Societies. Int. J. Environ. Res. Public Health 2022, 19, 3705. https://doi.org/10.3390/ijerph19063705
Liu R, Huang Y-HC, Sun J, Lau J, Cai Q. A Shot in the Arm for Vaccination Intention: The Media and the Health Belief Model in Three Chinese Societies. International Journal of Environmental Research and Public Health. 2022; 19(6):3705. https://doi.org/10.3390/ijerph19063705
Chicago/Turabian StyleLiu, Ruoheng, Yi-Hui Christine Huang, Jie Sun, Jennifer Lau, and Qinxian Cai. 2022. "A Shot in the Arm for Vaccination Intention: The Media and the Health Belief Model in Three Chinese Societies" International Journal of Environmental Research and Public Health 19, no. 6: 3705. https://doi.org/10.3390/ijerph19063705
APA StyleLiu, R., Huang, Y.-H. C., Sun, J., Lau, J., & Cai, Q. (2022). A Shot in the Arm for Vaccination Intention: The Media and the Health Belief Model in Three Chinese Societies. International Journal of Environmental Research and Public Health, 19(6), 3705. https://doi.org/10.3390/ijerph19063705






