Latent Classes of Polysubstance Use and Associations with HIV Risk and Structural Vulnerabilities among Cisgender Women Who Engage in Street-Based Transactional Sex in Baltimore City
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Analytical Sample
2.3. Measures
2.3.1. Latent Class Indicators
2.3.2. Covariates
2.3.3. Outcomes
2.4. Analysis
2.5. Ethical Statement
3. Results
3.1. Latent Classes of Polysubstance Use
3.2. Sociodemographic Correlates of Latent Class Membership
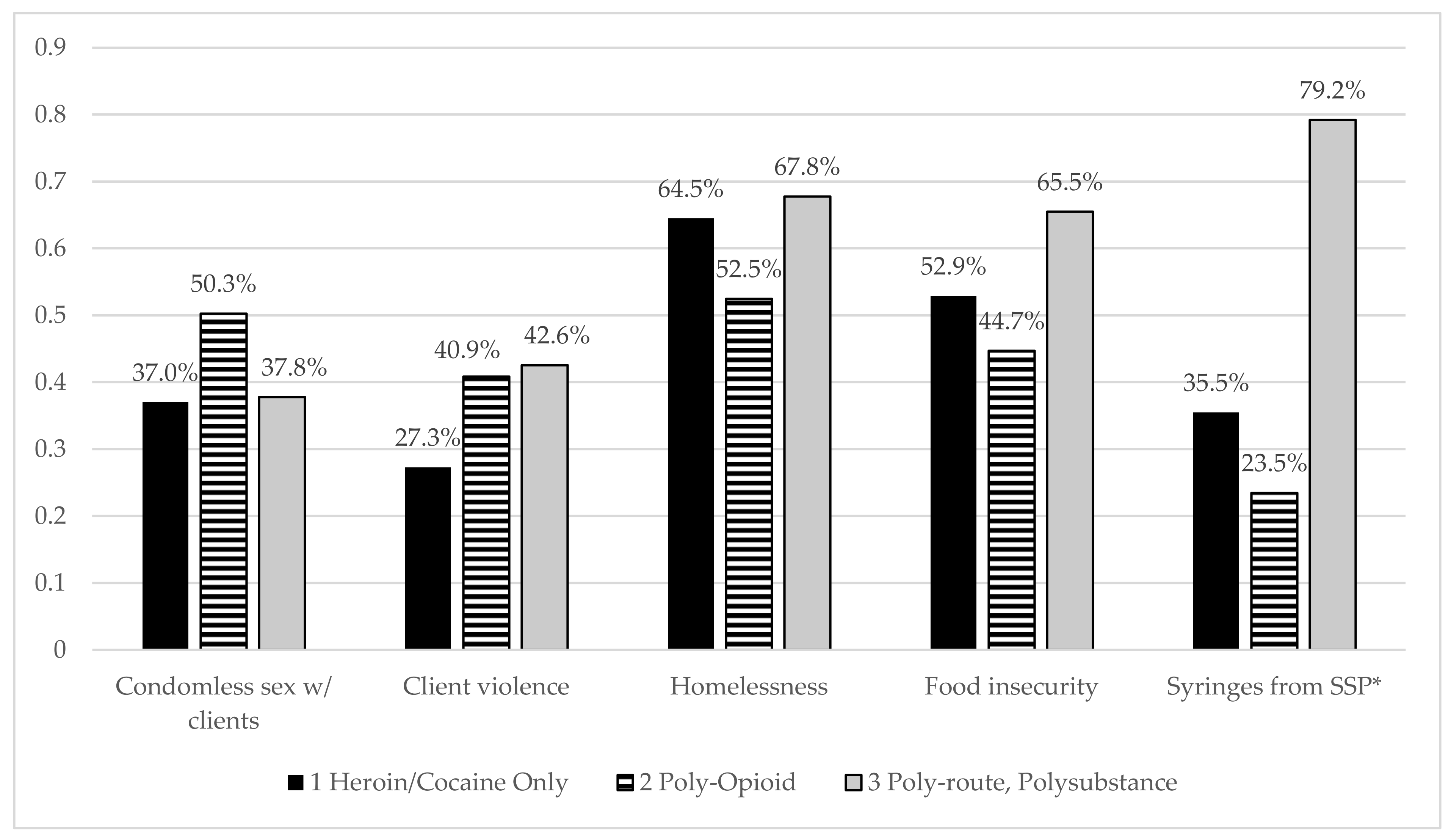
3.3. HIV-Related Risks and Structural Vulnerabilities by Latent Class
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baral, S.; Beyrer, C.; Muessig, K.; Poteat, T.; Wirtz, A.L.; Decker, M.R.; Sherman, S.G.; Kerrigan, D. Burden of HIV among female sex workers in low-income and middle-income countries: A systematic review and meta-analysis. Lancet Infect. Dis. 2012, 12, 538–549. [Google Scholar] [CrossRef]
- Prüss-Ustün, A.; Wolf, J.; Driscoll, T.; Degenhardt, L.; Neira, M.; Calleja, J.M.G. HIV Due to Female Sex Work: Regional and Global Estimates. PLoS ONE 2013, 8, e63476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shannon, K.; Crago, A.-L.; Baral, S.; Bekker, L.-G.; Kerrigan, D.; Decker, M.R.; Poteat, T.; Wirtz, A.L.; Weir, B.; Boily, M.-C.; et al. The global response and unmet actions for HIV and sex workers. Lancet 2018, 392, 698–710. [Google Scholar] [CrossRef]
- Paz-Bailey, G.; Noble, M.; Salo, K.; Tregear, S.J. Prevalence of HIV among U.S. Female Sex Workers: Systematic Review and Meta-analysis. AIDS Behav. 2016, 20, 2318–2331. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention (CDC). HIV Risk among Persons Who Exchange Sex for Money or Nonmonetary Items. 12 November 2019. Available online: https://www.cdc.gov/hiv/group/sexworkers.html (accessed on 18 October 2021).
- Miles, I.J.; Le, B.C.; Wejnert, C.; Oster, A.; Di Nenno, E.; Paz-Bailey, G. HIV infection among heterosexuals at increased risk—United States, 2010. MMWR. Morb. Mortal. Wkly. Rep. 2013, 62, 183–188. [Google Scholar]
- Sherman, S.G.; Park, J.N.; Galai, N.; Allen, S.T.; Huettner, S.S.; Silberzahn, B.E.; Decker, R.M.; Poteat, T.C.; Footer, K.H.A. Drivers of HIV Infection Among Cisgender and Transgender Female Sex Worker Populations in Baltimore City: Results from the SAPPHIRE Study. JAIDS J. Acquir. Immune Defic. Syndr. 2019, 80, 513–521. [Google Scholar] [CrossRef]
- Shannon, K.; Strathdee, S.; Goldenberg, S.; Duff, P.; Mwangi, P.; Rusakova, M.; Reza-Paul, S.; Lau, J.; Deering, K.; Pickles, M.; et al. Global epidemiology of HIV among female sex workers: Influence of structural determinants. Lancet 2015, 385, 55–71. [Google Scholar] [CrossRef] [Green Version]
- Blankenship, K.M.; Reinhard, E.; Sherman, S.G.; El-Bassel, N. Structural Interventions for HIV Prevention Among Women Who Use Drugs. JAIDS J. Acquir. Immune Defic. Syndr. 2015, 69, S140–S145. [Google Scholar] [CrossRef]
- Rouhani, S.; Allen, S.T.; Whaley, S.; White, R.H.; O’Rourke, A.; Schneider, K.E.; Kilkenny, M.E.; Weir, B.W.; Sherman, S.G. Food access among people who inject drugs in West Virginia. Harm Reduct. J. 2021, 18, 90. [Google Scholar] [CrossRef]
- Goldenberg, S.; Liyanage, R.; Braschel, M.; Shannon, K. Structural barriers to condom access in a community-based cohort of sex workers in Vancouver, Canada: Influence of policing, violence and end-demand criminalisation. BMJ Sex. Reprod. Health 2020, 46, 301–307. [Google Scholar] [CrossRef]
- Decker, M.R.; Park, J.N.; Allen, S.T.; Silberzahn, B.; Footer, K.; Huettner, S.; Galai, N.; Sherman, S.G. Inconsistent Condom Use Among Female Sex Workers: Partner-specific Influences of Substance Use, Violence, and Condom Coercion. AIDS Behav. 2020, 24, 762–774. [Google Scholar] [CrossRef]
- Lim, S.; Park, J.N.; Kerrigan, D.L.; Sherman, S.G. Severe Food Insecurity, Gender-Based Violence, Homelessness, and HIV Risk among Street-based Female Sex Workers in Baltimore, Maryland. AIDS Behav. 2019, 23, 3058–3063. [Google Scholar] [CrossRef]
- Azim, T.; Bontell, I.; Strathdee, S. Women, drugs and HIV. Int. J. Drug Policy 2015, 26 (Suppl. S1), S16–S21. [Google Scholar] [CrossRef] [Green Version]
- Strathdee, S.; Philbin, M.M.; Semple, S.J.; Pu, M.; Orozovich, P.; Martinez, G.; Lozada, R.; Fraga, M.; de la Torre, A.; Staines, H.; et al. Correlates of injection drug use among female sex workers in two Mexico—U.S. border cities. Drug Alcohol Depend. 2008, 92, 132–140. [Google Scholar] [CrossRef] [Green Version]
- Roberts, A.; Mathers, B.; Degenhardt, L. Women Who Inject Drugs: A Review of Their Risks, Experiences and Needs; A Report Prepared on Behalf of the Reference Group to the United Nations on HIV and Injecting Drug Use; National Drug and Alcohol Research Centre (NDARC), University of New South Wales: Sydney, Australia, 2010. [Google Scholar]
- Blum, R.W.; McNeely, C.A.; Nonnemaker, J. Vulnerability, Risk, and Protection in Adolescent Risk and Vulnerability: Concepts and Measurement; Institute of Medicine and National Research Council (US), National Academies Press: Washington, DC, USA, 2001. [Google Scholar] [CrossRef]
- Cleland, C.; Jarlais, D.C.D.; Perlis, E.T.; Stimson, G.V.; Poznyak, V.B. HIV risk behaviors among female IDUs in developing and transitional countries. BMC Public Health 2007, 7, 271. [Google Scholar] [CrossRef] [Green Version]
- Glick, J.L.; Lim, S.; Beckham, S.W.; Tomko, C.; Park, J.N.; Sherman, S.G. Structural vulnerabilities and HIV risk among sexual minority female sex workers (SM-FSW) by identity and behavior in Baltimore, MD. Harm Reduct. J. 2020, 17, 43. [Google Scholar] [CrossRef]
- Sherman, S.G.; Latkin, C.A.; Gielen, A.C. Social Factors Related to Syringe Sharing among Injection Partners: A Focus on Gender. Subst. Use Misuse 2001, 36, 2113–2136. [Google Scholar] [CrossRef]
- Decker, M.R.; Wirtz, A.L.; Baral, S.; Peryshkina, A.; Mogilnyi, V.; Weber, R.A.; Stachowiak, J.; Go, V.; Beyrer, C. Injection drug use, sexual risk, violence and STI/HIV among Moscow female sex workers. Sex. Transm. Infect. 2012, 88, 278–283. [Google Scholar] [CrossRef]
- Pinkham, S.; Malinowska-Sempruch, K. Women, Harm Reduction and HIV. Reprod. Health Matters 2008, 16, 168–181. [Google Scholar] [CrossRef]
- United Nations. World Drug Report. 2015. Available online: https://www.unodc.org/wdr2015/ (accessed on 18 October 2021).
- Strathdee, S.A.; West, B.S.; Reed, E.; Moazen, B.; Azim, T.; Dolan, K. Substance Use and HIV Among Female Sex Workers and Female Prisoners. JAIDS J. Acquir. Immune Defic. Syndr. 2015, 69, S110–S117. [Google Scholar] [CrossRef] [Green Version]
- Trenz, R.C.; Scherer, M.; Duncan, A.; Harrell, P.T.; Moleko, A.G.; Latimer, W.W. Latent class analysis of polysubstance use, sexual risk behaviors, and infectious disease among South African drug users. Drug Alcohol Depend. 2013, 132, 441–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carter, A.; Roth, E.A.; Ding, E.; Milloy, M.-J.; Kestler, M.; Jabbari, S.; Webster, K.; de Pokomandy, A.; Loutfy, M.; Kaida, A.; et al. Substance Use, Violence, and Antiretroviral Adherence: A Latent Class Analysis of Women Living with HIV in Canada. AIDS Behav. 2018, 22, 971–985. [Google Scholar] [CrossRef] [PubMed]
- Floyd, L.J.; Hedden, S.; Lawson, A.; Salama, C.; Moleko, A.G.; Latimer, W. The Association Between Poly-Substance Use, Coping, and Sex Trade Among Black South African Substance Users. Subst. Use Misuse 2010, 45, 1971–1987. [Google Scholar] [CrossRef] [PubMed]
- Latkin, A.C.; Forman, V.; Knowlton, A.; Sherman, S. Norms, social networks, and HIV-related risk behaviors among urban disadvantaged drug users. Soc. Sci. Med. 2003, 56, 465–476. [Google Scholar] [CrossRef]
- Coffin, P.O.; Santos, G.M.; Matheson, T.; Behar, E.; Rowe, C.; Rubin, T.; Silvis, J.; Vittinghoff, E. Behavioral intervention to reduce opioid overdose among high-risk persons with opioid use disorder: A pilot randomized controlled trial. PLoS ONE 2017, 12, e0183354. [Google Scholar] [CrossRef]
- Sherman, S.G.; Sutcliffe, C.; Srirojn, B.; Latkin, C.A.; Aramratanna, A.; Celentano, D.D. Evaluation of a peer network intervention trial among young methamphetamine users in Chiang Mai, Thailand. Soc. Sci. Med. 2009, 68, 69–79. [Google Scholar] [CrossRef] [Green Version]
- Garfein, R.S.; Golub, E.T.; Greenber, A.E.; Hagan, H.; Hanson, D.L.; Hudson, S.M.; Kapadia, F.; Latka, M.H.; Ouellet, L.J.; Purcell, D.; et al. A peer-education intervention to reduce injection risk behaviors for HIV and hepatitis C virus infection in young injection drug users. AIDS 2007, 21, 1923–1932. [Google Scholar] [CrossRef] [Green Version]
- Latkin, C.A.; Donnell, D.; Metzger, D.; Sherman, S.; Aramrattna, A.; Davis-Vogel, A.; Quan, V.M.; Gandham, S.; Vongchak, T.; Perdue, T.; et al. The efficacy of a network intervention to reduce HIV risk behaviors among drug users and risk partners in Chiang Mai, Thailand and Philadelphia, USA. Soc. Sci. Med. 2009, 68, 740–748. [Google Scholar] [CrossRef] [Green Version]
- Baral, S.; Holland, C.E.; Shannon, K.; Logie, C.; Semugoma, P.; Sithole, B.; Erin, P.; Fatou, D.; Chris, B. Enhancing Benefits or Increasing Harms: Community Responses for HIV Among Men Who Have Sex with Men, Transgender Women, Female Sex Workers, and People Who Inject Drugs. JAIDS J. Acquir. Immune Defic. Syndr. 2014, 66, S319–S328. [Google Scholar] [CrossRef] [Green Version]
- Wechsberg, W.M.; Luseno, W.K.; Lam, W.K.; Parry, C.D.; Morojele, N. Substance Use, Sexual Risk, and Violence: HIV Prevention Intervention with Sex Workers in Pretoria. AIDS Behav. 2006, 10, 131–137. [Google Scholar] [CrossRef]
- Wechsberg, W.M.; Wu, L.-T.; Azule, W.; Parry, C.D.; Browne, A.F.; Luseno, W.K.; Kline, T.; Gentry, A. Substance abuse, treatment needs and access among female sex workers and non-sex workers in Pretoria, South Africa. Subst. Abus. Treat. Prev. Policy 2009, 4, 11. [Google Scholar] [CrossRef] [Green Version]
- Tegang, S.-P.; Abdallah, S.; Emukule, G.; Luchters, S.; Kingola, N.; Barasa, M.; Mucheke, S.; Mwarogo, P. Concurrent sexual and substance-use risk behaviours among female sex workers in Kenya’s Coast Province: Findings from a behavioural monitoring survey. SAHARA J. Soc. Asp. HIV/AIDS Res. Alliance 2010, 7, 10–16. [Google Scholar] [CrossRef]
- Tomczyk, S.; Isensee, B.; Hanewinkel, R. Latent classes of polysubstance use among adolescents—A systematic review. Drug Alcohol Depend. 2016, 160, 12–29. [Google Scholar] [CrossRef]
- Roth, A.M.; Armenta, R.A.; Wagner, K.D.; Roesch, S.C.; Bluthenthal, R.; Cuevas-Mota, J.; Garfein, R.S. Patterns of Drug Use, Risky Behavior, and Health Status Among Persons Who Inject Drugs Living in San Diego, California: A Latent Class Analysis. Subst. Use Misuse 2015, 50, 205–214. [Google Scholar] [CrossRef] [Green Version]
- Schneider, K.E.; Park, J.N.; Allen, S.T.; Weir, B.W.; Sherman, S.G. Patterns of polysubstance use and overdose among people who inject drugs in Baltimore, Maryland: A latent class analysis. Drug Alcohol Depend. 2019, 201, 71–77. [Google Scholar] [CrossRef]
- Wu, L.-T.; Ling, W.; Burchett, B.; Blazer, D.G.; Yang, C.; Pan, J.-J.; Reeve, B.B.; Woody, G.E. Use of item response theory and latent class analysis to link poly-substance use disorders with addiction severity, HIV risk, and quality of life among opioid-dependent patients in the Clinical Trials Network. Drug Alcohol Depend. 2011, 118, 186–193. [Google Scholar] [CrossRef] [Green Version]
- Patra, J.; Fischer, B.; Maksimowska, S.; Rehm, J. Profiling poly-substance use typologies in a multi-site cohort of illicit opioid and other drug users in Canada—A latent class analysis. Addict. Res. Theory 2009, 17, 168–185. [Google Scholar] [CrossRef]
- Harrell, P.; Mancha, B.; Petras, H.; Trenz, R.; Latimer, W. Latent classes of heroin and cocaine users predict unique HIV/HCV risk factors. Drug Alcohol Depend. 2012, 122, 220–227. [Google Scholar] [CrossRef] [Green Version]
- Schneider, K.E.; O’Rourke, A.; White, R.H.; Park, J.N.; Musci, R.J.; Kilkenny, M.E.; Sherman, S.G.; Allen, S.T. Polysubstance use in rural West Virginia: Associations between latent classes of drug use, overdose, and take-home naloxone. Int. J. Drug Policy 2020, 76, 102642. [Google Scholar] [CrossRef]
- Schneider, K.E.; White, R.H.; Musci, R.J.; O’Rourke, A.; Kilkenny, M.E.; Sherman, S.G.; Allen, S.T. The Relationship Between Polysubstance Injection Drug Use, HIV Risk Behaviors, and Interest in Pre-Exposure Prophylaxis (PrEP) Among People Who Inject Drugs in Rural West Virginia. J. Stud. Alcohol Drugs 2020, 81, 740–749. [Google Scholar] [CrossRef]
- Reynolds, G.L.; Fisher, D.G. A latent class analysis of alcohol and drug use immediately before or during sex among women. Am. J. Drug Alcohol Abus. 2018, 45, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Karamouzian, M.; Pilarinos, A.; Hayashi, K.; Buxton, J.A.; Kerr, T. Latent patterns of polysubstance use among people who use opioids: A systematic review. Int. J Drug Policy 2022, 102, 103584. [Google Scholar] [CrossRef]
- Straus, M.A.; Hamby, S.L.; Boney-McCoy, S.E.; Sugarman, D.B. The Revised Conflict Tactics Scales (CTS2): Development and Preliminary Psychometric Data. J. Fam. Issues 1996, 17, 283–316. [Google Scholar] [CrossRef]
- Grace-Martin, K. Two Recommended Solutions for Missing Data: Multiple Imputation and Maximum Likelihood. 2014. Available online: https://www.theanalysisfactor.com/missing-data-two-recommended-solutions/ (accessed on 20 October 2021).
- NylundK, L.; Asparouhov, T.; Muthén, B.O. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct. Equ. Model. Multidiscip. J. 2007, 14, 535–569. [Google Scholar] [CrossRef]
- Asparouhouv, T.; Muthen, B. Appendices for auxiliary variables in mixture modeling: 3-step approaches using Mplus. In MPlus User’s Guide; Mplus: Los Angeles, CA, USA, 2013. [Google Scholar]
- Asparouhov, T.; Muthen, B. Auxiliary variables in mixture modeling: Using the BCH method in Mplus to estimate a distal outcome model and an arbitrary secondary model. Mplus Web Notes 2014, 21, 1–22. [Google Scholar]
- Centers for Disease Control and Prevention. Syringe Services Programs (SSPs). 2019. Available online: https://www.cdc.gov/ssp/index.html (accessed on 11 October 2021).
- Huo, D.; Bailey, S.L.; Hershow, R.C.; Ouellet, L. Drug Use and HIV Risk Practices of Secondary and Primary Needle Exchange Users. AIDS Educ. Prev. 2005, 17, 170–184. [Google Scholar] [CrossRef]
- Adams, J.M. Making the Case for Syringe Services Programs. Public Health Rep. 2020, 135, 10S–12S. [Google Scholar] [CrossRef]
- Hagan, H.; McGough, J.P.; Thiede, H.; Hopkins, S.; Duchin, J.; Alexander, E. Reduced injection frequency and increased entry and retention in drug treatment associated with needle-exchange participation in Seattle drug injectors. J. Subst. Abus. Treat. 2000, 19, 247–252. [Google Scholar] [CrossRef]
- Jarlais, D.C.D.; Nugent, A.; Solberg, A.; Feelemyer, J.; Mermin, J.; Holtzman, D. Syringe Service Programs for Persons Who Inject Drugs in Urban, Suburban, and Rural Areas—United States, 2013. MMWR. Morb. Mortal. Wkly. Rep. 2015, 64, 1337–1341. [Google Scholar] [CrossRef] [Green Version]
- Allen, S.T.; White, R.H.; O’Rourke, A.; Schneider, K.E.; Weir, B.W.; Lucas, G.M.; Kilkenny, M.E.; Sherman, S.G. Syringe Coverage Among People Who Inject Drugs in West Virginia, USA. AIDS Behav. 2021, 25, 3377–3385. [Google Scholar] [CrossRef]
- Bartholomew, T.S.; Tookes, H.E.; Bullock, C.; Onugha, J.; Forrest, D.W.; Feaster, D.J. Examining risk behavior and syringe coverage among people who inject drugs accessing a syringe services program: A latent class analysis. Int. J. Drug Policy 2020, 78, 102716. [Google Scholar] [CrossRef]
- Andraka-Christou, B. Addressing Racial And Ethnic Disparities In The Use Of Medications For Opioid Use Disorder. Health Affairs 2021, 40, 920–927. [Google Scholar] [CrossRef]
- Sullivan, P.S.; Woodyatt, C.; Koski, C.; Pembleton, E.; McGuinness, P.; Taussig, J.; Ricca, A.; Luisi, N.; Mokotoff, E.; Benbow, N.; et al. A Data Visualization and Dissemination Resource to Support HIV Prevention and Care at the Local Level: Analysis and Uses of the AIDSVu Public Data Resource. J. Med. Internet Res. 2020, 22, e23173. [Google Scholar] [CrossRef]
- Singer, M. Introduction to Syndemics: A Critical Systems Approach to Public and Community Health; Jossey-Bass: San Francisco, CA, USA, 2009. [Google Scholar]
- Park, J.N.; Rouhani, S.; Beletsky, L.; Vincent, L.; Saloner, B.; Sherman, S.G. Situating the Continuum of Overdose Risk in the Social Determinants of Health: A New Conceptual Framework. Milbank Q. 2020, 98, 700–746. [Google Scholar] [CrossRef]
- Collins, A.B.; Boyd, J.; Cooper, H.L.; McNeil, R. The intersectional risk environment of people who use drugs. Soc. Sci. Med. 2019, 234, 112384. [Google Scholar] [CrossRef]
- Allen, S.T.; White, R.H.; O’Rourke, A.; Ahmad, N.J.; Hazelett, T.; Kilkenny, M.E.; Sherman, S.G. Correlates of transactional sex among a rural population of people who inject drugs. AIDS Behav. 2020, 24, 775–781. [Google Scholar] [CrossRef]
- Poteat, T.; Scheim, A.; Xavier, J.; Reisner, S.; Baral, S. Global Epidemiology of HIV Infection and Related Syndemics Affecting Transgender People. J. Acquir. Immune Defic. Syndr. 2016, 72, S210–S219. [Google Scholar] [CrossRef] [Green Version]
| Characteristics | Total n (%) |
|---|---|
| Demographics | |
| Age, mean (sd) | 35.8 (8.9) |
| Race/ethnicity | |
| BIPOC and Hispanic | 80 (32.8) |
| Non-Hispanic White | 164 (67.2) |
| Education | |
| Less than high school | 127 (52.0) |
| 12th grade or GED | 117 (48.0) |
| Drug use (past 3 months) | |
| Injection | |
| Any injection drug use | 165 (67.6) |
| Cocaine | 62 (25.4) |
| Heroin | 163 (66.8) |
| Speedball (heroin and cocaine together) | 56 (23.0) |
| Non-injection | |
| Cocaine/crack | 213 (87.3) |
| Heroin | 104 (42.6) |
| Heroin + cocaine together (n = 116 missing) | 22 (9.0) |
| Opioid pain relievers (n = 2 missing) | 71 (29.1) |
| Benzodiazepines | 73 (29.9) |
| Buprenorphine/Suboxone | 41 (16.8) |
| Outcomes (past 3 months) | |
| Condomless sex with clients (n = 1 missing) | 98 (40.1) |
| Food insecurity | 134 (54.9) |
| Housing insecurity | 153 (62.7) |
| Client violence (physical or sexual) | 86 (35.3) |
| Obtained syringes at SSP 1 vs. other location | 113 (46.3) |
| # Classes | Smallest Class | Log Likelihood | AIC | BIC | Entropy | LMR p-Value | Blrt p-Value |
|---|---|---|---|---|---|---|---|
| 1 | - | −1148.448 | 2134.896 | 2346.37 | - | - | - |
| 2 | 73 | −1056.847 | 2151.693 | 2218.14 | 0.836 | 0.000 | 0.000 |
| 3 | 52 | −1031.448 | 2120.896 | 2222.314 | 0.783 | 0.0016 | 0.000 |
| 4 | 35 | −1015.99 | 2109.979 | 2246.369 | 0.815 | 0.1544 | 0.000 |
| 5 | 25 | −1001.259 | 2100.517 | 2271.897 | 0.836 | 0.4855 | 0.020 |
| Class 1 Heroin/Cocaine Only Use n = 118 (48.4%) | Class 2 Poly-Opioid n = 52 (21.3%) | Class 3 Poly-Route, Polysubstance n = 74 (30.3%) | ||||
|---|---|---|---|---|---|---|
| Inj. heroin | 0.584 |  | 0.389 |  | 1.000 |  |
| Inj. cocaine | 0.042 | 0.000 | 0.754 | |||
| Inj. speedball | 0.015 | 0.000 | 0.717 | |||
| Heroin | 0.397 | 0.584 | 0.350 | |||
| Cocaine/crack | 0.870 | 0.709 | 1.000 | |||
| Heroin and cocaine | 0.089 | 0.116 | 0.421 | |||
| Opioid pain relievers | 0.000 | 0.749 | 0.375 | |||
| Benzodiazepines | 0.137 | 0.549 | 0.346 | |||
| Bupr./Suboxone | 0.044 | 0.362 | 0.202 | |||
| 0.50 | 0.50 | 0.50 | ||||
| Class 1 | Class 2 | 2 vs. 1 | Class 3 | 3 vs. 1 | 3 vs. 2 | ||||
|---|---|---|---|---|---|---|---|---|---|
| % | % | β | p-Value | % | β | p-Value | β | p-Value | |
| Age (mean) | 37.3 | 35.5 | −0.033 | 0.181 | 34.0 | −0.041 | 0.038 | −0.008 | 0.746 |
| Race | 0.851 | 0.046 | −0.239 | 0.546 | −1.09 | 0.012 | |||
| BIPOC and Hispanic | 30.8 | 48.2 | 23.9 | ||||||
| White, non-Hispanic | 69.2 | 51.8 | 76.1 | ||||||
| Education < HS | 51.1 | 45.4 | −0.316 | 0.452 | 58.4 | 0.240 | 0.481 | 0.557 | 0.187 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beckham, S.W.; Glick, J.L.; Schneider, K.E.; Allen, S.T.; Shipp, L.; White, R.H.; Park, J.N.; Sherman, S.G. Latent Classes of Polysubstance Use and Associations with HIV Risk and Structural Vulnerabilities among Cisgender Women Who Engage in Street-Based Transactional Sex in Baltimore City. Int. J. Environ. Res. Public Health 2022, 19, 3783. https://doi.org/10.3390/ijerph19073783
Beckham SW, Glick JL, Schneider KE, Allen ST, Shipp L, White RH, Park JN, Sherman SG. Latent Classes of Polysubstance Use and Associations with HIV Risk and Structural Vulnerabilities among Cisgender Women Who Engage in Street-Based Transactional Sex in Baltimore City. International Journal of Environmental Research and Public Health. 2022; 19(7):3783. https://doi.org/10.3390/ijerph19073783
Chicago/Turabian StyleBeckham, Sam Wilson, Jennifer L. Glick, Kristin E. Schneider, Sean T. Allen, Lillian Shipp, Rebecca Hamilton White, Ju Nyeong Park, and Susan G. Sherman. 2022. "Latent Classes of Polysubstance Use and Associations with HIV Risk and Structural Vulnerabilities among Cisgender Women Who Engage in Street-Based Transactional Sex in Baltimore City" International Journal of Environmental Research and Public Health 19, no. 7: 3783. https://doi.org/10.3390/ijerph19073783






