Clinical Outcomes in Routine Evaluation Measures for Patients Discharged from Acute Psychiatric Care: Four-Arm Peer and Text Messaging Support Controlled Observational Study
Abstract
:1. Background
2. Methods
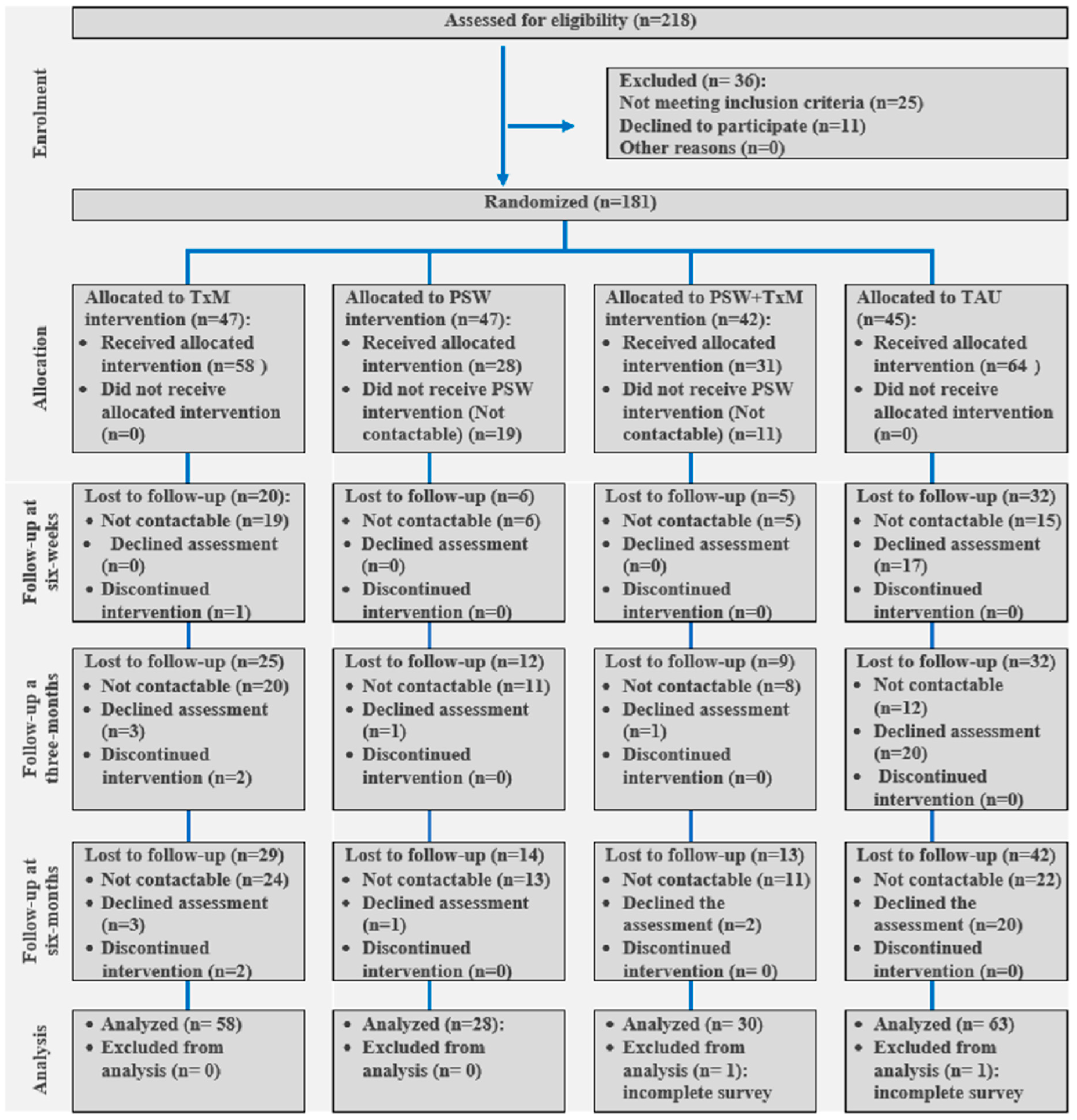
2.1. Study Design
2.2. Patients
2.3. Treatment Interventions
2.4. Outcome
CORE-OM
- Subjective well-being (4 items, e.g., “I have felt overwhelmed by my problems”);
- Problems/symptoms (12 items, e.g., “I have had difficulty getting to sleep or staying asleep”);
- Functioning (12 items; e.g., “I have been able to do most things I needed to”);
- Reliable change: The reliable change index (RCI) is used to assess pre–post change, and 0.50 (clinical score of 5) is the cut-off score [10], i.e., clinical score changes greater than 5 are significant.
- 3.
2.5. Sample Size
2.6. Data Analysis
- Baseline data analysis:
- 2.
- Outcome analysis:
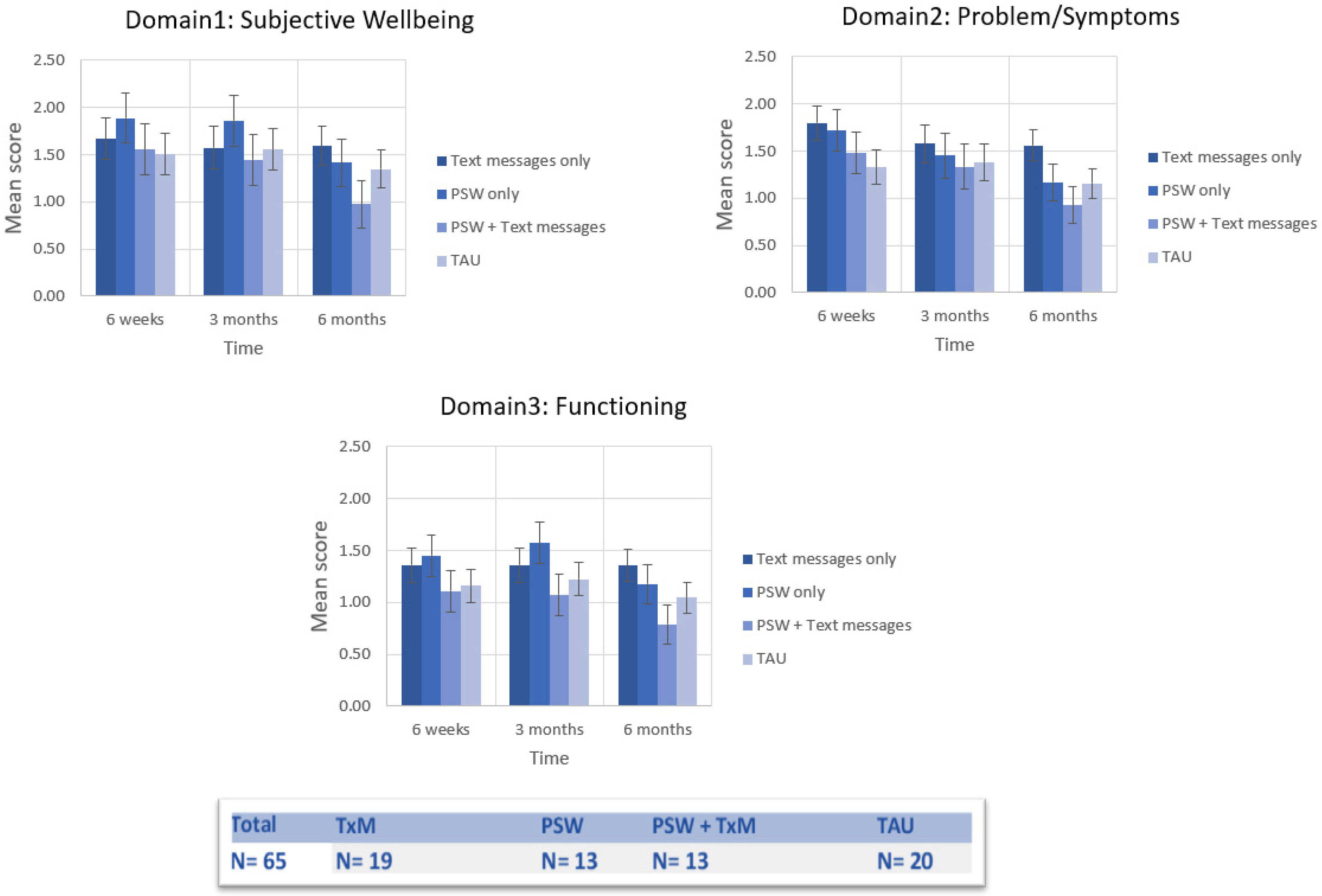
- Non-risk domains: As the risk domain was analyzed separately, the three other domains (subjective well-being, problems/symptoms, and functioning) were analyzed to assess cluster differences among the four study arms across the four time points using means (M) and standard deviations (SD). To assess the impact of the study arms on the three non-risk CORE-OM domains, a repeated measure multivariate analysis of covariance (MANCOVA) was used for patients completing all time points (PSW: n = 13; TxM: n = 19; PSW + TxM: n = 13; TAU: n = 20). We controlled for baseline scores when analyzing across follow-up timepoints (i.e., six-weeks, three-months, and six-months) We ran the analysis with the treatment intervention (TxM yes/no and PSW yes/no) as the independent variable and mean scores of CORE-OM domains as the dependent variables while controlling for baseline scores as covariates. With regard to MANCOVA post-hoc test, Bonferroni corrections were used to control for multiple comparison error rate changes for post-hoc pairwise analyses.
- All-item analysis: For CORE-OM all-item analysis (the total score of the scale), the change parameters discussed above, including CORE-OM recovery, reliable change, clinical change, and the change in prevalence, were measured. For this analysis, we compared the baseline data to six-month data only in order to examine the overall change from the beginning to the end of the intervention for the four study groups. Data are reported as proportions and percentages.
- Risk domain: As the score of the risk domain correlates poorly with the nonrisk items [43], a separate analysis for risk score was carried out to examine prevalence and the associated change at the end of the study across the four groups using chi-square analysis. A client was deemed at risk if they scored ≥1 on the risk subscale.
3. Results
3.1. Nonrisk Domains
3.2. All-Item Analysis
- Reliable improvement: Overall, 31/82 (37.8%) participants on the all-item score met the criteria for reliable improvement at six months. The TxM + PSW group scored the highest (58.8%).
- Clinical change: Out of the eligible participants, 15/49 (30.6%) on the all-item score met the criteria for clinical change at six months. The TxM + PSW group scored the highest (45.5%).
- Recovery: Out of the eligible participants, 14/49 (28.6%) met the criteria for recovery (reliable and clinically significant change) on the all-item score. Of them, 5/11 (45.5%) were from the TxM + PSW group.
3.3. Risk Subscore Prevalence Analysis
4. Discussion
4.1. Scale Outcome across the Intervention Groups
4.2. Risk Score
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Faessler, L.; Kutz, A.; Haubitz, S.; Mueller, B.; Perrig-Chiello, P.; Schuetz, P. Psychological distress in medical patients 30 days following an emergency department admission: Results from a prospective, observational study. BMC Emerg. Med. 2016, 16, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chavasiri, S. Depression and Quality of Life in Spinal Cord Injury Patients Living in the Community after Hospital Discharge. Siriraj Med. J. 2020, 72, 59–66. [Google Scholar] [CrossRef] [Green Version]
- Chung, C.R.; Yoo, H.J.; Park, J.; Ryu, S. Cognitive Impairment and Psychological Distress at Discharge from Intensive Care Unit. Psychiatry Investig. 2017, 14, 376–379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vlake, J.H.; Wesselius, S.; van Genderen, M.E.; van Bommel, J.; Boxma-de Klerk, B.; Wils, E.-J. Psychological distress and health-related quality of life in patients after hospitalization during the COVID-19 pandemic: A single-center, observational study. PLoS ONE 2021, 16, e0255774. [Google Scholar] [CrossRef] [PubMed]
- Walter, F.; Carr, M.J.; Mok, P.; Antonsen, S.; Pedersen, C.B.; Appleby, L.; Fazel, S.; Shaw, J.; Webb, R.T. Multiple adverse outcomes following first discharge from inpatient psychiatric care: A national cohort study. Lancet Psychiatry 2019, 6, 582–589. [Google Scholar] [CrossRef] [Green Version]
- Loch, A.A. Discharged from a mental health admission ward: Is it safe to go home? A review on the negative outcomes of psychiatric hospitalization. Psychol. Res. Behav. Manag. 2014, 7, 137–145. [Google Scholar] [CrossRef] [Green Version]
- Hunt, I.M.; Kapur, N.; Webb, R.; Robinson, J.; Burns, J.; Shaw, J.; Appleby, L. Suicide in recently discharged psychiatric patients: A case-control study. Psychol. Med. 2009, 39, 443–449. [Google Scholar] [CrossRef]
- Large, M.; Sharma, S.; Cannon, E.; Ryan, C.; Nielssen, O. Risk Factors for Suicide Within a Year of Discharge from Psychiatric Hospital: A Systematic Meta-Analysis. Aust. N. Z. J. Psychiatry 2011, 45, 619–628. [Google Scholar] [CrossRef]
- Lorentzen, V.; Handegård, B.H.; Moen, C.M.; Solem, K.; Lillevoll, K.; Skre, I. CORE-OM as a routine outcome measure for adolescents with emotional disorders: Factor structure and psychometric properties. BMC Psychol. 2020, 8, 86. [Google Scholar] [CrossRef]
- Barkham, M.; Mellor-Clark, J.; Connell, J.; Cahill, J. A core approach to practice-based evidence: A brief history of the origins and applications of the CORE-OM and CORE System. Couns. Psychother. Res. 2006, 6, 3–15. [Google Scholar] [CrossRef]
- Barkham, M.; Margison, F.; Leach, C.; Lucock, M.; Mellor-Clark, J.; Evans, C.; Benson, L.; Connell, J.; Audin, K.; McGrath, G. Service profiling and outcomes benchmarking using the CORE-OM: Toward practice-based evidence in the psychological therapies. J. Consult. Clin. Psychol. 2001, 69, 184–196. [Google Scholar] [CrossRef] [PubMed]
- Phillips, M.S.; Steelesmith, D.L.; Campo, J.V.; Pradhan, T.; Fontanella, C.A. Factors Associated with Multiple Psychiatric Readmissions for Youth with Mood Disorders. J. Consult. Clin. Psychol. 2020, 59, 619–631. [Google Scholar] [CrossRef] [PubMed]
- Kalb, L.G.; Stapp, E.K.; Ballard, E.D.; Holingue, C.; Keefer, A.; Riley, A. Trends in Psychiatric Emergency Department Visits Among Youth and Young Adults in the US. Pediatrics 2019, 143, e20182192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bardach, N.S.; Doupnik, S.K.; Rodean, J.; Zima, B.T.; Gay, J.C.; Nash, C.; Tanguturi, Y.; Coker, T.R. ED Visits and Readmissions After Follow-up for Mental Health Hospitalization. Pediatrics 2020, 145, e20192872. [Google Scholar] [CrossRef] [PubMed]
- Elhassan, N.M.; Elhusein, B.; Al Abdulla, M.; Saad, T.A.; Kumar, R. Sociodemographic and clinical characteristics of patients with recurrent psychiatric readmissions in Qatar. J. Int. Med. Res. 2020, 48, 300060520977382. [Google Scholar] [CrossRef]
- Kalseth, J.; Lassemo, E.; Wahlbeck, K.; Haaramo, P.; Magnussen, J. Psychiatric readmissions and their association with environmental and health system characteristics: A systematic review of the literature. BMC Psychiatry 2016, 16, 376. [Google Scholar] [CrossRef]
- Donisi, V.; Tedeschi, F.; Wahlbeck, K.; Haaramo, P.; Amaddeo, F. Pre-discharge factors predicting readmissions of psychiatric patients: A systematic review of the literature. BMC Psychiatry 2016, 16, 449. [Google Scholar] [CrossRef]
- Chavez, L.J.; Liu, C.-F.; Tefft, N.; Hebert, P.L.; Clark, B.J.; Rubinsky, A.D.; Lapham, G.T.; Bradley, K.A. Unhealthy alcohol use in older adults: Association with readmissions and emergency department use in the 30 days after hospital discharge. Drug Alcohol Depend. 2016, 158, 94–101. [Google Scholar] [CrossRef] [Green Version]
- Schmutte, T.; Dunn, C.; Sledge, W. Characteristics of Inpatients with a History of Recurrent Psychiatric Hospitalizations: A Matched-Control Study. Psychiatr. Serv. 2009, 60, 1683–1685. [Google Scholar] [CrossRef]
- Shalaby, R.A.H.; Agyapong, V.I.O. Peer Support in Mental Health: Literature Review. JMIR Ment. Health 2020, 7, e15572. [Google Scholar] [CrossRef]
- Chinman, M.; George, P.; Dougherty, R.H.; Daniels, A.S.; Ghose, S.S.; Swift, A.; Delphin-Rittmon, M.E. Peer support services for individuals with serious mental illnesses: Assessing the evidence. Psychiatr. Serv. 2014, 65, 429–441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davidson, L.; Bellamy, C.; Guy, K.; Miller, R. Peer support among persons with severe mental illnesses: A review of evidence and experience. World Psychiatry Off. J. World Psychiatr. Assoc. 2012, 11, 123–128. [Google Scholar] [CrossRef] [Green Version]
- Aguilera, A.; Muñoz, R.F. Text Messaging as an Adjunct to CBT in Low-Income Populations: A Usability and Feasibility Pilot Study. Prof. Psychol. Res. Pract. 2011, 42, 472–478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agyapong, V.I.; McLoughlin, D.M.; Farren, C.K. Six-months outcomes of a randomised trial of supportive text messaging for depression and comorbid alcohol use disorder. J. Affect. Disord. 2013, 151, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Agyapong, V.I.; Milnes, J.; McLoughlin, D.M.; Farren, C.K. Perception of patients with alcohol use disorder and comorbid depression about the usefulness of supportive text messages. Technol. Health Care 2013, 21, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Agyapong, V.I.; Mrklas, K.; Juhás, M.; Omeje, J.; Ohinmaa, A.; Dursun, S.M.; Greenshaw, A.J. Cross-sectional survey evaluating Text4Mood: Mobile health program to reduce psychological treatment gap in mental healthcare in Alberta through daily supportive text messages. BMC Psychiatry 2016, 16, 378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sledge, W.H.; Lawless, M.; Sells, D.; Wieland, M.; O’Connell, M.J.; Davidson, L. Effectiveness of peer support in reducing readmissions of persons with multiple psychiatric hospitalizations. Psychiatry Serv. 2011, 62, 541–544. [Google Scholar] [CrossRef]
- McGuire, A.B.; Powell, K.G.; Treitler, P.C.; Wagner, K.D.; Smith, K.P.; Cooperman, N.; Robinson, L.; Carter, J.; Ray, B.; Watson, D.P. Emergency department-based peer support for opioid use disorder: Emergent functions and forms. J. Subst. Abus. Treat. 2019, 108, 82–87. [Google Scholar] [CrossRef] [Green Version]
- Urichuk, L.; Hrabok, M.; Hay, K.; Spurvey, P.; Sosdjan, D.; Knox, M.; Fu, A.; Surood, S.; Brown, R.; Coulombe, J.; et al. Enhancing peer support experience for patients discharged from acute psychiatric care: Protocol for a randomised controlled pilot trial. BMJ Open 2018, 8, e022433. [Google Scholar] [CrossRef] [Green Version]
- Kilbourne, A.M.; Beck, K.; Spaeth-Rublee, B.; Ramanuj, P.; O’Brien, R.W.; Tomoyasu, N.; Pincus, H.A. Measuring and improving the quality of mental health care: A global perspective. World Psychiatry 2018, 17, 30–38. [Google Scholar] [CrossRef] [Green Version]
- Roe, D.; Slade, M.; Jones, N. The utility of patient-reported outcome measures in mental health. World Psychiatry Off. J. World Psychiatr. Assoc. 2022, 21, 56–57. [Google Scholar] [CrossRef] [PubMed]
- Davidson, L.; Tondora, J. Person-centred care planning as foundational to clinical practice. World Psychiatry Off. J. World Psychiatr. Assoc. (WPA) 2022, 21, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Shalaby, R.; Hrabok, M.; Spurvey, P.; El-Magd, R.M.A.; Knox, M.; Rude, R.; Vuong, W.; Surood, S.; Urichuk, L.; Snaterse, M.; et al. Recovery Following Peer and Text Messaging Support After Discharge from Acute Psychiatric Care in Edmonton, Alberta: Controlled Observational Study. JMIR Form Res. 2021, 5, e27137. [Google Scholar] [CrossRef] [PubMed]
- Lyne, K.J.; Barrett, P.; Evans, C.; Barkham, M. Dimensions of variation on the CORE-OM. Br. J. Clin. Psychol. 2006, 45 Pt 2, 185–203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Falkenström, F.; Kumar, M.; Zahid, A.; Kuria, M.; Othieno, C. Factor analysis of the Clinical Outcomes in Routine Evaluation—Outcome Measures (CORE-OM) in a Kenyan sample. BMC Psychol. 2018, 6, 48. [Google Scholar] [CrossRef] [PubMed]
- Outcome Evaluation (Core Report) 2011–2012 Counselling Services. Available online: https://www.brookes.ac.uk/Documents/Students/Wellbeing/Counselling/Outcome-Report-2011-2012/ (accessed on 21 July 2021).
- Sales, C.M.; Neves, I.T.; Alves, P.G.; Ashworth, M. Capturing and missing the patient’s story through outcome measures: A thematic comparison of patient-generated items in PSYCHLOPS with CORE-OM and PHQ-9. Health Expect. Int. J. Public Particip. Health Care Health Policy 2018, 21, 615–619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brand, C.; Ward, F.; MacDonagh, N.; Cunningham, S.; Timulak, L. A national evaluation of the Irish public health counselling in primary care service-examination of initial effectiveness data. BMC Psychiatry 2021, 21, 227. [Google Scholar]
- Evans, C.; Connell, J.; Barkham, M.; Margison, F.; McGrath, G.; Mellor-Clark, J.; Audin, K. Towards a standardised brief outcome measure: Psychometric properties utility of the, CORE–OM. Br. J. Psychiatry 2002, 180, 51–60. [Google Scholar] [CrossRef]
- Haynes, R.B. Clinical Epidemiology: How to Do Clinical Practice Research; Lippincott Williams & Wilkins: Hongkong, China, 2012. [Google Scholar]
- IBM. IBM Support. Release Notes—IBM® SPSS® Statistics 25.0. Available online: https://www.ibm.com/support/pages/release-notes-ibm%C2%AE-spss%C2%AE-statistics-250 (accessed on 8 December 2020).
- Ruxton, G.D. The unequal variance t-test is an underused alternative to Student’s t-test and the Mann–Whitney U test. Behav. Ecol. 2006, 17, 688–690. [Google Scholar] [CrossRef]
- Serralta, F.B.; Zibetti, M.R.; Evans, C. Psychological Distress of University Workers during COVID-19 Pandemic in Brazil. Int. J. Environ. Res. Public Health 2020, 17, 8520. [Google Scholar] [CrossRef]
- Zeldovich, M.; Alexandrowicz, R.W. Comparing outcomes: The Clinical Outcome in Routine Evaluation from an international point of view. Int. J. Methods Psychiatry Res. 2019, 28, e1774. [Google Scholar] [CrossRef] [PubMed]
- Werbart, A.; Levin, L.; Andersson, H.; Sandell, R. Everyday evidence: Outcomes of psychotherapies in Swedish public health services. Psychotherapy 2013, 50, 119–130. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. 2017 Licence: CC BY-NC-SA 3.0 IGO. Available online: https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf;jsessionid=9CB70AF65B16E393152C34AF19CBB754?sequence=1 (accessed on 9 December 2020).
- Gibbard, I.; Hanley, T. A five-year evaluation of the effectiveness of person-centred counselling in routine clinical practice in primary care. Couns. Psychother. Res. 2008, 8, 215–222. [Google Scholar] [CrossRef]
- Barkham, M.; Stiles, W.B.; Connell, J.; Mellor-Clark, J. Psychological treatment outcomes in routine NHS services: What do we mean by treatment effectiveness? Psychol. Psychother. 2012, 85, 1–16. [Google Scholar] [CrossRef]
- Agyapong, V.I.O.; Juhás, M.; Ohinmaa, A.; Omeje, J.; Mrklas, K.; Suen, V.Y.M.; Dursun, S.M.; Greenshaw, A.J. Randomized controlled pilot trial of supportive text messages for patients with depression. BMC Psychiatry 2017, 17, 286. [Google Scholar] [CrossRef] [Green Version]
- Bauer, S.; Okon, E.; Meermann, R.; Kordy, H. Technology-enhanced maintenance of treatment gains in eating disorders: Efficacy of an intervention delivered via text messaging. J. Consult. Clin. Psychol. 2012, 80, 700–706. [Google Scholar] [CrossRef]
- Pijnenborg, G.H.M.; Withaar, F.K.; Brouwer, W.H.; Timmerman, M.E.; Bosch, R.J.V.D.; Evans, J.J. The efficacy of SMS text messages to compensate for the effects of cognitive impairments in schizophrenia. Br. J. Clin. Psychol. 2010, 49, 259–274. [Google Scholar] [CrossRef]
- O’Reilly, H.; Hagerty, A.; O’Donnell, S.; Farrell, A.; Hartnett, D.; Murphy, E.; Kehoe, E.G.; Agyapong, V.I.O.; McLoughlin, D.M.; Farren, C. Alcohol Use Disorder and Comorbid Depression: A Randomized Controlled Trial Investigating the Effectiveness of Supportive Text Messages in Aiding Recovery. Alcohol Alcohol. 2019, 54, 551–558. [Google Scholar] [CrossRef]
- Agyapong, V.I.; Ahern, S.; McLoughlin, D.; Farren, C. Supportive text messaging for depression and comorbid alcohol use disorder: Single-blind randomised trial. J. Affect. Disord. 2012, 141, 168–176. [Google Scholar] [CrossRef]
- Saleem, J.J.; Read, J.M.; Loehr, B.M.; Frisbee, K.L.; Wilck, N.R.; Murphy, J.J.; Vetter, B.M.; Herout, J. Veterans’ response to an automated text messaging protocol during the COVID-19 pandemic. J. Am. Med. Inform. Assoc. 2020, 27, 1300–1305. [Google Scholar] [CrossRef]
- Agyapong, V.I.; Hrabok, M.; Shalaby, R.; Vuong, W.; Noble, J.M.; Gusnowski, A.; Mrklas, K.; Li, D.; Urichuck, L.; Snaterse, M.; et al. Text4Hope: Receiving Daily Supportive Text Messages for 3 Months During the COVID-19 Pandemic Reduces Stress, Anxiety, and Depression. Disaster Med. Public Health Prep. 2021, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Agyapong, V.I.O.; Hrabok, M.; Vuong, W.; Shalaby, R.; Noble, J.M.; Gusnowski, A.; Greiner, R.; Li, X.; Cao, B.; Greenshaw, A.J.; et al. Changes in Stress, Anxiety, and Depression Levels of Subscribers to a Daily Supportive Text Message Program (Text4Hope) During the COVID-19 Pandemic: Cross-Sectional Survey Study. JMIR Ment. Health 2020, 7, e22423. [Google Scholar] [CrossRef] [PubMed]
- Agyapong, V.; Shalaby, R.; Hrabok, M.; Vuong, W.; Noble, J.; Gusnowski, A.; Mrklas, K.; Li, D.; Snaterse, M.; Surood, S.; et al. Mental Health Outreach via Supportive Text Messages during the COVID-19 Pandemic: Improved Mental Health and Reduced Suicidal Ideation after Six Weeks in Subscribers of Text4Hope Compared to a Control Population. Int. J. Environ. Res. Public Health 2021, 18, 2157. [Google Scholar] [CrossRef] [PubMed]
- Mental Health Foundation. Peer Support. 2012. Available online: https://www.mentalhealth.org.uk/sites/default/files/need_2_know_peer_support1.pdf (accessed on 24 July 2021).
- Best, D.W.; Lubman, D.I. The recovery paradigm—A model of hope and change for alcohol and drug addiction. Aust. Fam. Physician 2012, 41, 593–597. [Google Scholar]
- Druss, B.G.; Zhao, L.; Silke, A.; Bona, J.R.; Fricks, L.; Jenkins-Tucker, S.; DiClemente, R.; Sterling, E.; Lorig, K. The Health and Recovery Peer (HARP) Program: A peer-led intervention to improve medical self-management for persons with serious mental illness. Schizophr. Res. 2010, 118, 264–270. [Google Scholar] [CrossRef] [Green Version]
- Hardy, S.; Hallett, N.; Chaplin, E. Evaluating a peer support model of community wellbeing for mental health: A coproduction approach to evaluation. Ment. Health Prev. 2019, 13, 149–158. [Google Scholar] [CrossRef]
- McBeath, M.; Drysdale, M.T.; Bohn, N. Work-integrated learning and the importance of peer support and sense of belonging. Educ. Train. 2018, 60, 39–53. [Google Scholar] [CrossRef]
- Burke, E.M.; Pyle, M.; Machin, K.; Morrison, A.P. Providing mental health peer support 1: A Delphi study to develop consensus on the essential components, costs, benefits, barriers and facilitators. Int. J. Soc. Psychiatry 2018, 64, 799–812. [Google Scholar] [CrossRef]
- Byrom, N. An evaluation of a peer support intervention for student mental health. J. Ment. Health 2018, 27, 240–246. [Google Scholar] [CrossRef]
- Burke, E.M.; Pyle, M.; Morrison, A.P.; Machin, K. Providing mental health peer support 2: Relationships with empowerment, hope, recovery, quality of life and internalised stigma. Int. J. Soc. Psychiatry 2018, 64, 745–755. [Google Scholar] [CrossRef]
- Lawn, S.; Smith, A.; Hunter, K. Mental health peer support for hospital avoidance and early discharge: An Australian example of consumer driven and operated service. J. Health 2009, 17, 498–508. [Google Scholar] [CrossRef]
- Johnson, S.; Lamb, D.; Marston, L.; Osborn, D.; Mason, O.; Henderson, C.; Ambler, G.; Milton, A.; Davidson, M.; Christoforou, M.; et al. Peer-supported self-management for people discharged from a mental health crisis team: A randomised controlled trial. Lancet 2018, 392, 409–418. [Google Scholar] [CrossRef] [Green Version]
- Rodgers, M.; Dalton, J.; Harden, M.; Street, A.; Parker, G.; Eastwood, A. Integrated Care to Address the Physical Health Needs of People with Severe Mental Illness: A Mapping Review of the Recent Evidence on Barriers, Facilitators and Evaluations. Int. J. Integr. Care 2018, 18, 9. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H. Effects of a Volunteer-Run Peer Support Program on Health and Satisfaction with Social Support of Older Adults Living Alone. J. Korean Acad. Nurs. 2012, 42, 525–536. [Google Scholar] [CrossRef] [PubMed]
- Dorgo, S.; Robinson, K.M.; Bader, J. The effectiveness of a peer-mentored older adult fitness program on perceived physical, mental, and social function. J. Am. Acad. Nurse Pract. 2009, 21, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Chapin, R.K.; Sergeant, J.F.; Landry, S.; Leedahl, S.N.; Rachlin, R.; Koenig, T.; Graham, A. Reclaiming joy: Pilot evaluation of a mental health peer support program for older adults who receive Medicaid. Gerontologist 2013, 53, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Sokol, R.; Fisher, E. Peer Support for the Hardly Reached: A Systematic Review. Am. J. Public Health 2016, 106, e1–e8. [Google Scholar] [CrossRef]
- Reynolds, W.; Lauder, W.; Sharkey, S.; Maciver, S.; Veitch, T.; Cameron, D. The effects of a transitional discharge model for psychiatric patients. J. Psychiatr. Ment. Health Nurs. 2004, 11, 82–88. [Google Scholar] [CrossRef]
- Shalaby, R.; Hrabok, M.; Spurvey, P.; Abou El-Magd, R.M.; Knox, M.; Rude, R.; Vuong, W.; Urichuk, L.; Surood, S.; Agyapong, V.I.O. Reducing readmission rates for individuals discharged from acute psychiatric care in Alberta using peer and text message support: Protocol for an innovative supportive program. BMC Health Serv. Res. 2022, 22, 332. [Google Scholar]
| Baseline Characteristics n (%) | Nondropout | Dropout | χ2/t Value | p |
|---|---|---|---|---|
| n = 151 | n = 30 | |||
| Age (years) | 41.37 | 41.19 | t(179) = 0.07 | 0.94 |
| Sex recorded at birth | χ2(1) = 0.70 | 0.4 | ||
| Male | 63 (80.8) | 15 (19.2) | ||
| Female | 88 (85.4) | 15 (14.6) | ||
| Ethnicity | χ2(2) = 4.66 | 0.1 | ||
| Indigenous | 18 (72.0) | 7 (28.0) | ||
| European/Caucasian | 104 (83.2) | 21 (16.8) | ||
| Other | 29 (93.5) | 2 (6.5) | ||
| Educational Level | χ2(2) = 2.96 | 0.23 | ||
| Less than high school | 26 (89.7) | 3 (10.3) | ||
| High school degree or equivalent | 38 (76.0) | 12 (24.0) | ||
| Above high school education | 85 (85.0) | 15 (15.0) | ||
| Employment Status | χ2(1) = 0.26 | 0.61 | ||
| Employed | 47 (85.5) | 8 (14.5) | ||
| Unemployed | 103 (82.4) | 22 (17.6) | ||
| Relationship | χ2(2) = 0.94 | 0.62 | ||
| Married/common law/in relationships | 42 (87.5) | 6 (12.5) | ||
| Single | 68 (81.0) | 16 (19.0) | ||
| Divorced/separated/widowed | 39 (83.0) | 8 (17.0) | ||
| Admitting Diagnosis | χ2(2) = 0.51 | 0.77 | ||
| Depression/anxiety | 75 (81.5) | 17 (18.5) | ||
| Bipolar disorder | 45 (84.9) | 8 (15.1) | ||
| Psychotic disorder | 31 (86.1) | 5 (13.9) | ||
| CORE-OM Domains (Mean Score, SD) | n = 150 | n = 30 | ||
| Subjective well-being domain | 1.71 (1.02) | 1.83 (1.10) | t(178) = 0.58 | 0.56 |
| Problem/symptom domain | 1.75 (0.94) | 1.75 (1.09) | t(178) = 0.02 | 0.98 |
| Functioning domain | 1.38 (0.71) | 1.66 (0.91) | t(36.42) = 1.57 | 0.12 |
| Risk domain | 0.53 (0.68) | 0.57 (0.66) | t(178) = 0.29 | 0.77 |
| All items | 1.40 (0.73) | 1.52 (0.88) | t(37.45) = 0.68 | 0.5 |
| Nonrisk items | 1.59 (0.78) | 1.72 (0.97) | t(36.90) = 0.71 | 0.48 |
| Study Groups | Prevalence n/N (%) | ||||
|---|---|---|---|---|---|
| Reliable Change (Total = 82) | Clinical Change (Improvement) (Total = 49) | Recovery (Total = 49) | |||
| Improvement | No Change | Deterioration | |||
| TxM | 7/29 (24.1%) | 15/29 (51.7) | 7/29 (24.1) | 3/18 (16.7%) | 3/18 (16.7%) |
| PSW | 5/14 (35.7%) | 7/14 (50.0) | 2/14 (14.3) | 2/6 (33.3%) | 2/6 (33.3%) |
| TxM + PSW | 10/17 (58.8%) | 7/17 (41.2) | 0/17 (0) | 5/11 (45.5%) | 5/11 (45.5%) |
| TAU | 9/22 (40.9%) | 12/22 (54.5) | 1/22 (4.5) | 5/14 (35.7%) | 4/14 (28.6%) |
| Condition | Prevalence, n/Total Responses (%) | Change in Prevalence Rate (Sixth Month from Baseline) % | χ2 (df) | p Value | |
|---|---|---|---|---|---|
| Baseline | Sixth Month | ||||
| TxM | 18/29 (62.07) | 10/29 (34.48) | −27.59 | 4.42 (1) | 0.04 * |
| PSW | 7/14 (50.00) | 4/14 (28.57) | −21.43 | 1.35 (1) | 0.25 |
| TxM + PSW | 13/18 (72.2) | 4/18 (22.2) | −50.00 | 9.03 (1) | <0.01 * |
| TAU | 14/22 (63.64) | 12/22 (54.55) | −9.09 | 0.38 (1) | 0.54 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shalaby, R.; Spurvey, P.; Knox, M.; Rathwell, R.; Vuong, W.; Surood, S.; Urichuk, L.; Snaterse, M.; Greenshaw, A.J.; Li, X.-M.; et al. Clinical Outcomes in Routine Evaluation Measures for Patients Discharged from Acute Psychiatric Care: Four-Arm Peer and Text Messaging Support Controlled Observational Study. Int. J. Environ. Res. Public Health 2022, 19, 3798. https://doi.org/10.3390/ijerph19073798
Shalaby R, Spurvey P, Knox M, Rathwell R, Vuong W, Surood S, Urichuk L, Snaterse M, Greenshaw AJ, Li X-M, et al. Clinical Outcomes in Routine Evaluation Measures for Patients Discharged from Acute Psychiatric Care: Four-Arm Peer and Text Messaging Support Controlled Observational Study. International Journal of Environmental Research and Public Health. 2022; 19(7):3798. https://doi.org/10.3390/ijerph19073798
Chicago/Turabian StyleShalaby, Reham, Pamela Spurvey, Michelle Knox, Rebecca Rathwell, Wesley Vuong, Shireen Surood, Liana Urichuk, Mark Snaterse, Andrew J. Greenshaw, Xin-Min Li, and et al. 2022. "Clinical Outcomes in Routine Evaluation Measures for Patients Discharged from Acute Psychiatric Care: Four-Arm Peer and Text Messaging Support Controlled Observational Study" International Journal of Environmental Research and Public Health 19, no. 7: 3798. https://doi.org/10.3390/ijerph19073798







