COVID-19 in Malaysia: Descriptive Epidemiologic Characteristics of the First Wave
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Characteristics of COVID-19 Cases in the First Wave
3.2. Spatial Spread
3.3. Estimation of Reproduction Number
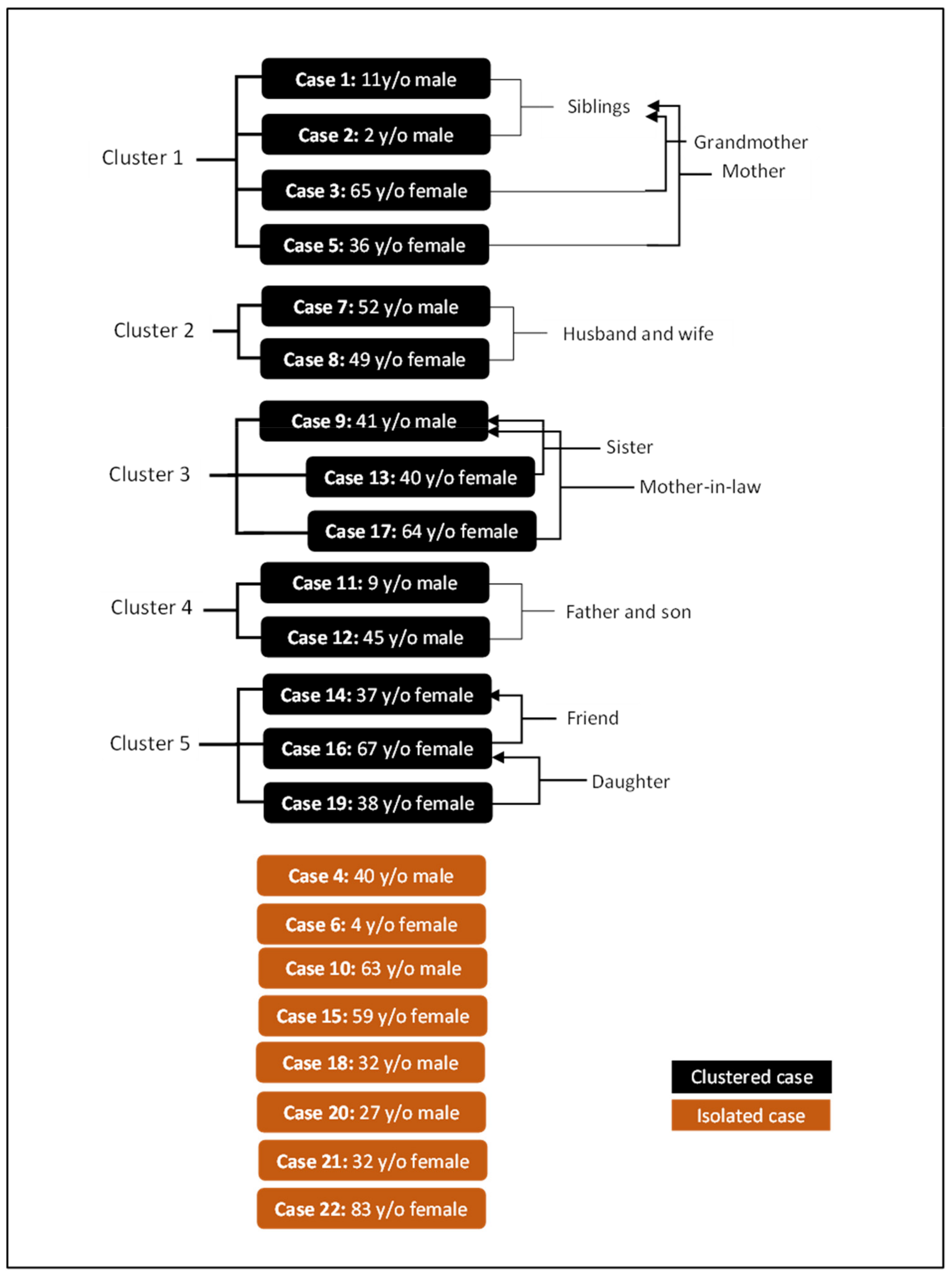
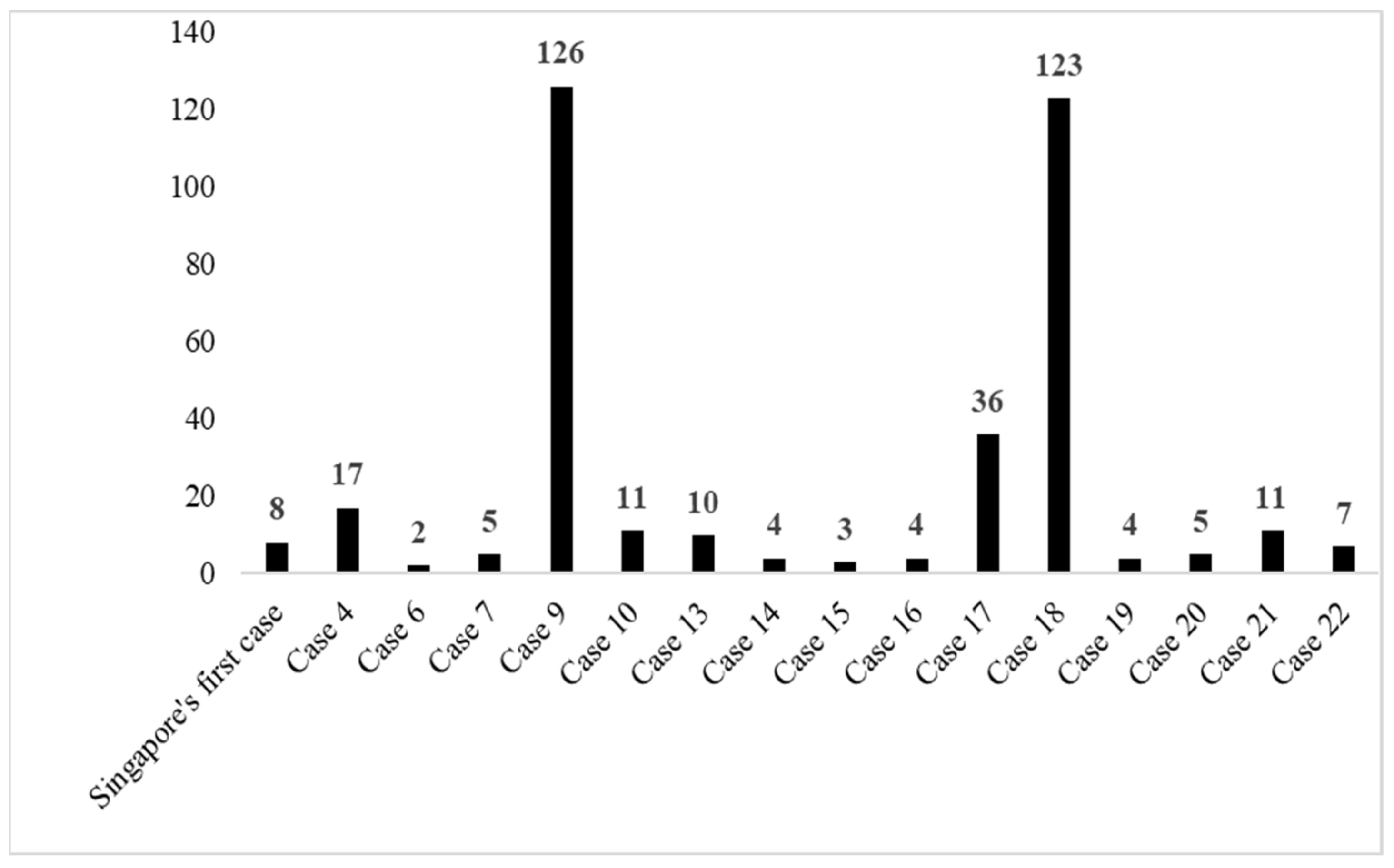
3.4. Epidemiological Link
3.5. Characteristics of Close Contacts
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 2 January 2021).
- Kirtipal, N.; Bharadwaj, S.; Kang, S.G. From SARS to SARS-CoV-2, insights on structure, pathogenicity and immunity aspects of pandemic human coronaviruses. Infect. Genet. Evol. 2020, 85, 104502. [Google Scholar] [CrossRef] [PubMed]
- Hui, D.S.C.; Chan, M.C.H.; Wu, A.K.; Ng, P.C.P. Severe acute respiratory syndrome (SARS): Epidemiology and clinical features. Postgrad. Med. J. 2004, 80, 373–381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Middle East Respiratory Syndrome Coronavirus (MERS-CoV). Available online: https://www.who.int/news-room/fact-sheets/detail/middle-east-respiratory-syndrome-coronavirus-(mers-cov) (accessed on 2 January 2021).
- World Health Organization. Weekly Epidemiological Update-9 February 2021. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update---9-february-2021 (accessed on 11 February 2021).
- World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report–27. 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/331116/nCoVsitrep16Feb2020-eng.pdf?sequence=1&isAllowed=y (accessed on 2 January 2021).
- Herng, L.C.; Singh, S.; Sundram, B.M.; Zamri, A.S.; Vei, T.C.; Aris, T.; Ibrahim, H.; Abdullah, N.H.; Dass, S.C.; Gill, B.S. The effects of super spreading events and movement control measures on the COVID-19 pandemic in Malaysia. Sci. Rep. 2022, 12, 2197. [Google Scholar] [CrossRef]
- Zamri, A.S.; Singh, S.; Ghazali, S.M.; Herng, L.C.; Dass, S.C.; Aris, T.; Ibrahim, H.M.; Gill, B.S. Effectiveness of the movement control measures during the third wave of COVID-19 in Malaysia. Epidemiol. Health 2021, 43, e2021073. [Google Scholar] [CrossRef]
- Kenyataan Akhbar KPK 4 Mac 2020–Situasi Semasa Jangkitan Penyakit Coronavirus 2019 (COVID-19) di Malaysia. Available online: https://kpkesihatan.com/2020/03/04/kenyataan-akhbar-kpk-4-mac-2020-situasi-semasa-jangkitan-penyakit-coronavirus-2019-covid-19-di-malaysia/ (accessed on 2 January 2021).
- Ministry of Health Malaysia. COVID-19 Management Guidelines in Malaysia No.3/2020. Available online: https://covid-19.moh.gov.my/garis-panduan/garis-panduan-kkm (accessed on 21 July 2021).
- Gill, B.S.; Jayaraj, V.J.; Singh, S.; Ghazali, S.M.; Cheong, Y.L.; Md Iderus, N.H.; Sundram, B.M.; Aris, T.B.; Mohd Ibrahim, H.; Hong, B.H.; et al. Modelling the effectiveness of epidemic control measures in preventing the transmission of COVID-19 in Malaysia. Int. J. Environ. Res. Public Health 2020, 17, 5509. [Google Scholar] [CrossRef] [PubMed]
- Imperial College London. ODIN Editor. Available online: https://shiny.dide.imperial.ac.uk/infectiousdiseasemodels-2019/introduction/ (accessed on 9 February 2021).
- Ministry of Health Malaysia. Situasi Terkini COVID-19 di Malaysia. Available online: http://covid-19.moh.gov.my/terkini (accessed on 2 January 2021).
- Department of Statistics Malaysia. Demographic Statistics Third Quarter 2019, Malaysia. 2019. Available online: https://www.dosm.gov.my/v1/index.php/index.php?r=column/cthemeByCat&cat=430&bul_id=YkdwYkZYOVQ5WFJ4dXhEelNpbGRmZz09&menu_id=L0pheU43NWJwRWVSZklWdzQ4TlhUUT09 (accessed on 2 January 2021).
- Backer, J.A.; Klinkenberg, D.; Wallinga, J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Eurosurveillance 2020, 25, 2000062. [Google Scholar] [CrossRef] [Green Version]
- Read, J.M.; Bridgen, J.R.; Cummings, D.A.; Ho, A.; Jewell, C.P. Novel coronavirus 2019-nCoV: Early estimation of epidemiological parameters and epidemic predictions. Philos. Trans. R. Soc. B 2021, 376, 1829. [Google Scholar] [CrossRef]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.; Lau, E.H.; Wong, J.Y.; et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef] [Green Version]
- Micallef, S.; Piscopo, T.V.; Casha, R.; Borg, D.; Vella, C.; Zammit, M.A.; Borg, J.; Mallia, D.; Farrugia, J.; Vella, S.M.; et al. The first wave of COVID-19 in Malta- A national cross-sectional study. PLoS ONE 2020, 15, e0239389. [Google Scholar] [CrossRef]
- The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC Wkly. 2020, 2, 113–122. [Google Scholar] [CrossRef]
- Mouchtouri, V.A.; Christoforidou, E.P.; An der Heiden, M.A.; Lemos, C.M.; Fanos, M.; Rexroth, U.; Grote, U.; Belfroid, E.; Swaan, C.; Hadjichristodoulou, C. Exit and entry screening practices for infectious diseases among travelers at points of entry: Looking for evidence on public health impact. Int. J. Environ. Res. Public Health 2019, 16, 4638. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quilty, B.J.; Clifford, S.; Flasche, S.; Eggo, R.M.; CMMID nCoV working group. Effectiveness of airport screening at detecting travellers infected with novel coronavirus (2019-nCoV). Eurosurveillance 2020, 25, 2000080. [Google Scholar] [CrossRef] [PubMed]
- Sun, K.; Chen, J.; Viboud, C. Early epidemiological analysis of the coronavirus disease 2019 outbreak based on crowdsourced data: A population-level observational study. Lancet Digit. Health 2020, 2, e201–e208. [Google Scholar] [CrossRef]
- Xu, X.W.; Wu, X.X.; Jiang, X.G.; Xu, K.J.; Ying, L.J.; Ma, C.L.; Li, S.B.; Wang, H.Y.; Zhang, S.; Gao, H.N.; et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: Retrospective case series. BMJ 2020, 368, m792. [Google Scholar] [CrossRef] [Green Version]
- Cheng, H.Y.; Jian, S.W.; Liu, D.P.; Ng, T.C.; Huang, W.T.; Lin, H.H. Contact tracing assessment of COVID-19 transmission dynamics in Taiwan and risk at different exposure periods before and after symptom onset. JAMA Intern. Med. 2020, 180, 1156–1163. [Google Scholar] [CrossRef]
- Chan, J.F.W.; Yuan, S.; Kok, K.H.; To, K.K.W.; Chu, H.; Yang, J.; Xing, F.; Liu, J.; Yip, C.C.Y.; Poon, R.W.S.; et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet 2020, 395, 514–523. [Google Scholar] [CrossRef] [Green Version]
- South Korea Adds 114 Virus Cases, Warns on Seoul Cluster|Channel News Asia. Available online: https://www.channelnewsasia.com/asia/coronavirus-south-korea-seoul-cluster-new-covid-19-cases-771541 (accessed on 11 February 2021).
- Pung, R.; Chiew, C.J.; Young, B.E.; Chin, S.; Chen, M.I.; Clapham, H.E.; Cook, A.R.; Maurer-Stroh, S.; Toh, M.P.; Poh, C.; et al. Investigation of three clusters of COVID-19 in Singapore: Implications for surveillance and response measures. Lancet 2020, 395, 1039–1046. [Google Scholar] [CrossRef]
- Nishiura, H.; Linton, N.M.; Akhmetzhanov, A.R. Serial interval of novel coronavirus (COVID-19) infections. Int. J. Infect. Dis. 2020, 93, 284–286. [Google Scholar] [CrossRef]
- Yuan, Z.; Xiao, Y.; Dai, Z.; Huang, J.; Zhang, Z.; Chen, Y. Modelling the effects of Wuhan’s lockdown during COVID-19, China. Bull. World Health Organ. 2020, 98, 484–494. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus: All Short-Term Visitors Barred from Entering or Transiting in Singapore from Monday, 11.59 pm|The Straits Times. Available online: https://www.straitstimes.com/singapore/health/coronavirus-all-short-term-visitors-barred-from-entering-and-transiting-in (accessed on 11 February 2021).
- Lockdown Upends People’s Lives|Bangkok Post. Available online: https://www.bangkokpost.com/thailand/general/1887940/lockdown-upends-peoples-lives (accessed on 11 February 2021).
- Chinazzi, M.; Davis, J.T.; Ajelli, M.; Gioannini, C.; Litvinova, M.; Merler, S.; Pastore y Piontti, A.; Mu, K.; Rossi, L.; Sun, K.; et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science 2020, 368, 395–400. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Summary of Probable SARS Cases with Onset of Illness from 1 November 2002 to 31 July 2003. Available online: https://www.who.int/publications/m/item/summary-of-probable-sars-cases-with-onset-of-illness-from-1-november-2002-to-31-july-2003 (accessed on 8 March 2022).
- Chan-Yeung, M.; Xu, R.H. SARS: Epidemiology. Respirology 2003, 8 (Suppl. 1), S9–S14. [Google Scholar] [CrossRef] [PubMed]
- Kementerian Kesihatan Malaysia. Soalan Lazim (FAQ) Rasmi Berkaitan COVID-19 oleh Kementerian Kesihatan Malaysia. Available online: https://covid-19.moh.gov.my/faqsop/faq-covid-19-kkm (accessed on 8 March 2022).
- Dass, S.C.; Kwok, W.M.; Gibson, G.J.; Gill, B.S.; Sundram, B.M.; Singh, S. A data driven change-point epidemic model for assessing the impact of large gathering and subsequent movement control order on COVID-19 spread in Malaysia. PLoS ONE 2021, 16, e0252136. [Google Scholar]




| Parameter | Description | Value | Source |
|---|---|---|---|
| n | Total human population in Malaysia | 32,000,000 | Department of Statistics Malaysia, 2019 [14] |
| 1/φ | Incubation period | 5.2 days | Backer et al., 2020 [15] |
| Force of infection | 0.052 | Gill et al., 2020 [11] | |
| Infectious period | 3.6 days | Read et al., 2020 [16] | |
| ε | Death rate due to COVID-19 | 0 | Parameter estimated in this study |
| ζ | The average number of contacts per day per case | 4.82 | Parameter estimated in this study |
| q | The proportion of close contact traced per day | 0.23 | Gill et al., 2020 [11] |
| 1/θ | The duration of quarantine | 14 | Gill et al., 2020 [11] |
| κ | The proportion of exposed persons who performed effective precautions | 0.05 | Gill et al., 2020 [11] |
| The mean daily rate at which infectious cases are isolated | 0.3 | Parameter estimated in this study |
| Characteristics | n (%) |
|---|---|
| Gender | |
| Female | 12 (54.5) |
| Male | 10 (45.5) |
| Age mean (SD) (year) | 40.7 (21.6) |
| 1–9 (Child) | 3 (13.6) |
| 10–18 (Adolescent) | 1 (4.5) |
| >18–64 (Adult) | 15 (68.1) |
| ≥65 (Older adult) | 3 (13.6) |
| Nationality | |
| Chinese | 15 (68.2) |
| Malaysian | 6 (27.3) |
| United States | 1 (4.5) |
| Type of case | |
| Imported | 20 (90.9) |
| Local transmission | 2 (9.1) |
| Symptomatic | |
| No | 2 (9.1) |
| Yes | 20 (90.9) |
| Comorbidity | |
| No | 21 (95.5) |
| Yes | 1 (4.5) |
| Symptoms (n = 20) | |
| Fever | 17 (85.0) |
| Cough | 14 (70.0) |
| Sore throat | 4 (20.0) |
| Myalgia | 3 (15.0) |
| Headache | 4 (20.0) |
| Running nose | 4 (20.0) |
| Lethargy | 1 (5.0) |
| Shortness of breath | 2 (10.0) |
| Diarrhoea | 3 (15.0) |
| Chest pain | 1 (5.0) |
| Haemoptysis | 1 (5.0) |
| Nasal congestion | 1 (5.0) |
| Onset of symptoms * | |
| Upon arrival in Malaysia | 4 (20.0) |
| After arrival and before/at admission | 13 (65.0) |
| After admission | 1 (5.0) |
| No symptoms | 2 (10.0) |
| Duration from arrival to admission (Min-Max, Mean (SD)) * | |
| Overall | 0–19, 6.8 (6.8) |
| Symptomatic at arrival (n = 4) | 0–10, 3.3 (4.6) |
| Asymptomatic at arrival (n = 16) | 0–19, 7.6 (7.1) |
| Admitting hospital | |
| Hospital Sungai Buloh, Selangor | 8 (36.4) |
| Hospital Permai, Johor | 4 (18.2) |
| Hospital Kuala Lumpur | 4 (18.2) |
| Hospital Tuanku Jaafar, Negeri Sembilan | 2 (9.1) |
| Hospital Sultanah Maliha, Langkawi | 2 (9.1) |
| Hospital Sultanah Bahiyah, Kedah | 2 (9.1) |
| Case severity | |
| Mild | 19 (86.4) |
| Severe | 3 (13.6) |
| Treatment | |
| Symptomatic | 18 (82.0) |
| Antiviral | 4 (18.0) |
| Duration of hospitalization | 4–23, 14.9 (5.8) |
| Characteristic | n (%) |
|---|---|
| Age (n = 259) | |
| 1–9 (Child) | 18 (6.9) |
| 10–18 (Adolescent) | 18 (6.9) |
| 19–64 (Adult) | 205 (79.2) |
| ≥65 (Older adult) | 18 (6.9) |
| Gender (n = 329) | |
| Male | 140 (42.6) |
| Female | 189 (57.4) |
| Nationality (n = 350) | |
| Malaysia | 274 (78.3) |
| China | 53 (15.1) |
| Singapore | 13 (3.7) |
| France | 2 (0.6) |
| US | 2 (0.6) |
| India | 1 (0.3) |
| Indonesia | 1 (0.3) |
| Japan | 1 (0.3) |
| Korea | 1 (0.3) |
| New Zealand | 1 (0.3) |
| Taiwan | 1 (0.3) |
| Type of contact (n = 368) | |
| Health care worker | 106 (29.3) |
| Contacts on flight * | 94 (26.0) |
| Family | 53 (14.6) |
| Work colleague | 7 (1.9) |
| Other contacts ** | 102 (28.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghazali, S.M.; Singh, S.; Zulkifli, A.A.; Cheong, Y.L.; Md Iderus, N.H.; Md Zamri, A.S.S.; Ahmad Jaafar, N.; Lai, C.H.; Wan Mohamed Noor, W.N.; Rusli, N.; et al. COVID-19 in Malaysia: Descriptive Epidemiologic Characteristics of the First Wave. Int. J. Environ. Res. Public Health 2022, 19, 3828. https://doi.org/10.3390/ijerph19073828
Ghazali SM, Singh S, Zulkifli AA, Cheong YL, Md Iderus NH, Md Zamri ASS, Ahmad Jaafar N, Lai CH, Wan Mohamed Noor WN, Rusli N, et al. COVID-19 in Malaysia: Descriptive Epidemiologic Characteristics of the First Wave. International Journal of Environmental Research and Public Health. 2022; 19(7):3828. https://doi.org/10.3390/ijerph19073828
Chicago/Turabian StyleGhazali, Sumarni Mohd, Sarbhan Singh, Asrul Anuar Zulkifli, Yoon Ling Cheong, Nuur Hafizah Md Iderus, Ahmed Syahmi Syafiq Md Zamri, Nadhar Ahmad Jaafar, Chee Herng Lai, Wan Noraini Wan Mohamed Noor, Norhayati Rusli, and et al. 2022. "COVID-19 in Malaysia: Descriptive Epidemiologic Characteristics of the First Wave" International Journal of Environmental Research and Public Health 19, no. 7: 3828. https://doi.org/10.3390/ijerph19073828
APA StyleGhazali, S. M., Singh, S., Zulkifli, A. A., Cheong, Y. L., Md Iderus, N. H., Md Zamri, A. S. S., Ahmad Jaafar, N., Lai, C. H., Wan Mohamed Noor, W. N., Rusli, N., Chong, C. K., Aris, T., Mohd Ibrahim, H., Dass, S. C., & Gill, B. S. (2022). COVID-19 in Malaysia: Descriptive Epidemiologic Characteristics of the First Wave. International Journal of Environmental Research and Public Health, 19(7), 3828. https://doi.org/10.3390/ijerph19073828






