Increasing Physical Exercise through Action and Coping Planning
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Procedure
2.4. Data Cleaning and Analysis
3. Results
3.1. Reliability Analyses
3.2. Primary Analysis of Hierarchal Multiple Regression
3.2.1. Assumptions Testing
3.2.2. Regression Model
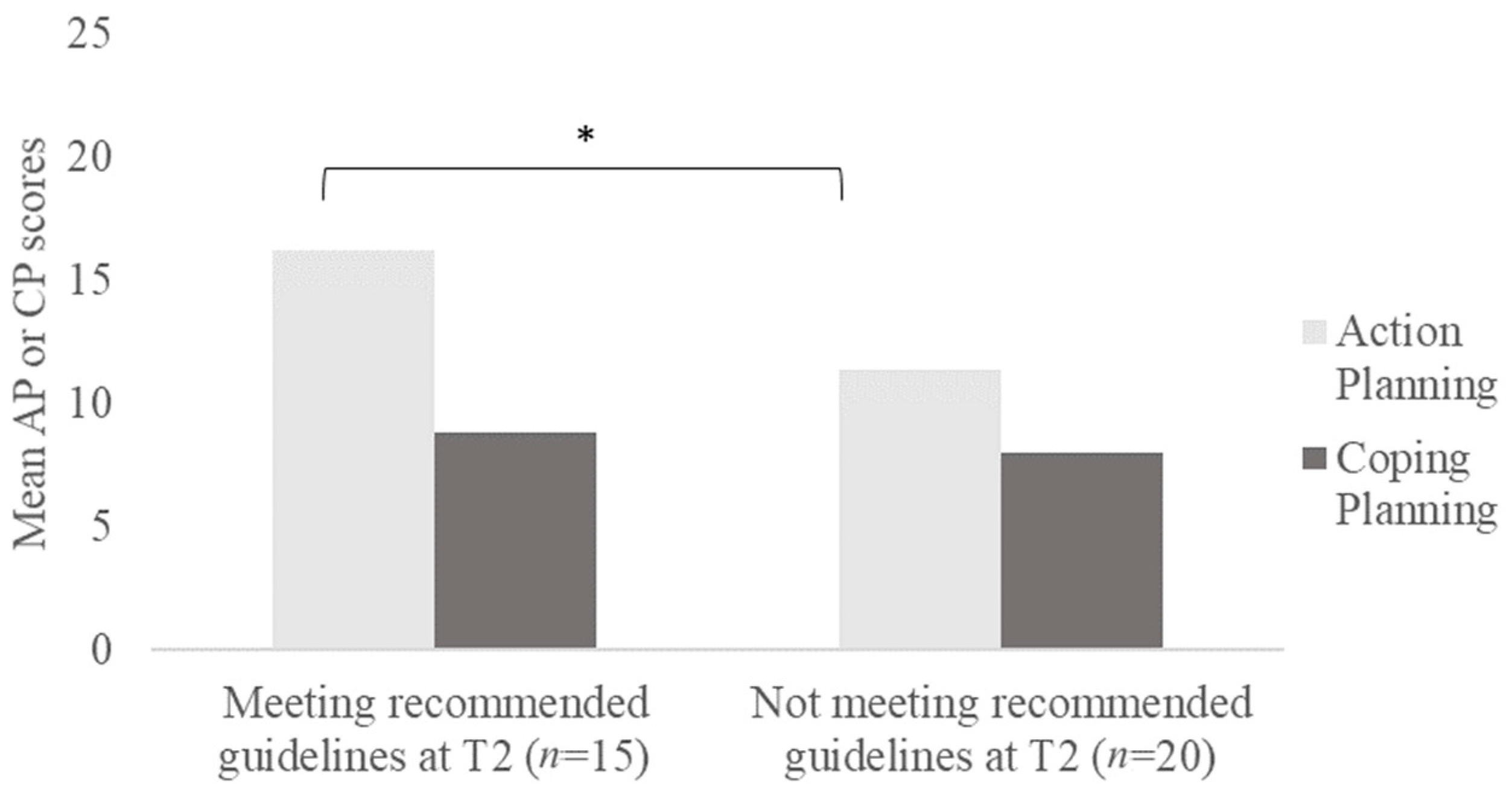
3.2.3. t-Test Analysis for Action and Coping Planning Scores
3.3. Supplementary Questions Examining Participants’ Perspectives
4. Discussion
4.1. Summary of Key Findings
4.2. Overall Increase in Exercise Behaviours in Our Study
4.2.1. Action Planning to Initiate Behaviour Change
4.2.2. Coping Planning Unable to Help Individuals Increase Exercise Behaviours
4.2.3. Comparison with Singaporeans’ Exercise Behaviours
4.3. Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1 · 9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef] [Green Version]
- Warburton, D.E.R. Health benefits of physical activity: The evidence. Can. Med. Assoc. J. 2006, 174, 801–809. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fox, K.R. The influence of physical activity on mental well-being. Public Health Nutr. 1999, 2, 411–418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- White, R.L.; Babic, M.J.; Parker, P.D.; Lubans, D.R.; Astell-Burt, T.; Lonsdale, C. Domain-Specific Physical Activity and Mental Health: A Meta-analysis. Am. J. Prev. Med. 2017, 52, 653–666. [Google Scholar] [CrossRef]
- Sniehotta, F.F.; Schwarzer, R.; Scholz, U.; Schüz, B. Action planning and coping planning for long-term lifestyle change: Theory and assessment. Eur. J. Soc. Psychol. 2005, 35, 565–576. [Google Scholar] [CrossRef]
- Sniehotta, F.F.; Scholz, U.; Schwarzer, R. Bridging the intention–behaviour gap: Planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychol. Health 2005, 20, 143–160. [Google Scholar] [CrossRef]
- Sports Index Participation Trends 2015 [Internet]. 2016. Available online: https://www.sportsingapore.gov.sg/-/media/SSC/Corporate/Files/About/Publications/Sports-Index-2015.pdf?la=en&hash=F4CF468F2C02E632172CB1937F8A5384F6E59692 (accessed on 13 November 2020).
- Gollwitzer, P.M. Implementation Intentions: Strong Effects of Simple Plans. Am. Psychol. 1999, 54, 493–503. [Google Scholar] [CrossRef]
- Schwarzer, R.; Luszczynska, A. How to overcome health-compromising behaviors: The health action process approach. Eur. Psychol. 2008, 13, 141–151. [Google Scholar] [CrossRef]
- Prochaska, J.O.; Velicer, W.F. The transtheoretical model of health behavior change. Am. J. Health Promot. 1997, 12, 38–48. [Google Scholar] [CrossRef]
- Scholz, U.; Nagy, G.; Schüz, B.; Ziegelmann, J.P. The role of motivational and volitional factors for self-regulated running training: Associations on the between- and within- person level. Br. J. Soc. Psychol. 2008, 47, 421–439. [Google Scholar] [CrossRef] [Green Version]
- Lachman, M.E.; Burack, O.R. Planning and Control Processes Across the Life Span: An Overview. Int. J. Behav. Dev. 1993, 16, 131–143. [Google Scholar] [CrossRef]
- Lippke, S.; Ziegelmann, J.P.; Schwarzer, R. Stage-specific adoption and maintenance of physical activity: Testing a three-stage model. Psychol. Sport Exerc. 2005, 6, 585–603. [Google Scholar] [CrossRef]
- Gollwitzer, P.M.; Sheeran, P. Implementation Intentions and Goal Achievement: A Meta-analysis of Effects and Processes. Adv. Exp. Soc. Psychol. 2006, 38, 69–119. [Google Scholar]
- Leventhal, H.; Singer, R.; Jones, S. Effects of fear and specificity of recommendation upon attitudes and behavior. J. Personal. Soc. Psychol. 1965, 2, 20–29. [Google Scholar] [CrossRef]
- Scholz, U.; Schüz, B.; Ziegelmann, J.P.; Lippke, S.; Schwarzer, R. Beyond behavioural intentions: Planning mediates between intentions and physical activity. Br. J. Health Psychol. 2008, 13, 479–494. [Google Scholar] [CrossRef] [Green Version]
- Ziegelmann, J.P.; Lippke, S.; Schwarzer, R. Adoption and maintenance of physical activity: Planning interventions in young, middle-aged, and older adults. Psychol. Health 2006, 21, 145–163. [Google Scholar] [CrossRef]
- Patterson, C.J.; Mischel, W. Effects of temptation-inhibiting and task-facilitating plans on self-control. J. Personal. Soc. Psychol. 1976, 33, 209–217. [Google Scholar] [CrossRef]
- Araújo-Soares, V.; McIntyre, T.; Sniehotta, F.F. Predicting changes in physical activity among adolescents: The role of self-efficacy, intention, action planning and coping planning. Health Educ. Res. 2009, 24, 128–139. [Google Scholar] [CrossRef]
- Carraro, N.; Gaudreau, P. Spontaneous and experimentally induced action planning and coping planning for physical activity: A meta-analysis. Psychol. Sport Exerc. 2013, 14, 228–248. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Processes 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Hagger, M.S.; Chatzisarantis, N.L.D.; Biddle, S.J.H. A meta-analytic review of the theories of reasoned action and planned behavior in physical activity: Predictive validity and the contribution of additional variables. J. Sport Exerc. Psychol. 2002, 24, 3–32. [Google Scholar] [CrossRef]
- Conner, M.; Sandberg, T.; Norman, P. Using Action Planning to Promote Exercise Behavior. Ann. Behav. Med. 2010, 40, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Ryan, R.M.; Deci, E.L. Self-Determination Theory and the Facilitation of Intrinsic Motivation, Social Development, and Well-Being. Am. Psychol. 2000, 55, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Gardner, B. Modelling motivation and habit in stable travel mode contexts. Transp. Res. Part F Traffic Psychol. Behav. 2009, 12, 68–76. [Google Scholar] [CrossRef]
- Rothman, A.J.; Sheeran, P.; Wood, W. Reflective and Automatic Processes in the Initiation and Maintenance of Dietary Change. Ann. Behav. Med. 2009, 38, 4–17. [Google Scholar] [CrossRef]
- Lally, P.; van Jaarsveld, C.H.M.; Potts, H.W.W.; Wardle, J. How are habits formed: Modelling habit formation in the real world. Eur. J. Soc. Psychol. 2010, 40, 998–1009. [Google Scholar] [CrossRef] [Green Version]
- Gardner, B.; Lally, P. Does intrinsic motivation strengthen physical activity habit? Modeling relationships between self-determination, past behaviour, and habit strength. J. Behav. Med. 2012, 36, 488–497. [Google Scholar] [CrossRef]
- Bargh, J.; Wyer, R.; Srull, T. Handbook of Social Cognition: Basic Processes; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1994. [Google Scholar]
- Ouellette, J.A.; Wood, W. Habit and intention in everyday life: The multiple processes by which past behavior predicts future behavior. Psychol. Bull. 1998, 124, 54–74. [Google Scholar] [CrossRef]
- De Bruijn, G.J.; Rhodes, R.E. Exploring exercise behavior, intention and habit strength relationships. Scand. J. Med. Sci. Sports 2011, 21, 482–491. [Google Scholar] [CrossRef]
- Gardner, B.; de Bruijn, G.-J.; Lally, P. A systematic review and meta-analysis of applications of the self-report habit index to nutrition and physical activity behaviours. Ann. Behav. Med. 2011, 42, 174–187. [Google Scholar] [CrossRef]
- Lally, P.; Gardner, B. Promoting habit formation. Health Psychol. Rev. 2013, 7, S137–S158. [Google Scholar] [CrossRef]
- Sniehotta, F.F. Towards a theory of intentional behaviour change: Plans, planning, and self-regulation. Br. J. Health Psychol. 2009, 14, 261–273. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 24 December 2021).
- Inauen, J.; Stocker, A.; Scholz, U. Why and for Whom May Coping Planning Have Adverse Effects? A Moderated Mediation Analysis. Appl. Psychol. Health Well-Being 2018, 10, 272–289. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.L.; French, D.P. What are the most effective intervention techniques for changing physical activity self-efficacy and physical activity behaviour—And are they the same? Health Educ. Res. 2011, 26, 308–322. [Google Scholar] [CrossRef]
- Poppe, L.; Crombez, G.; De Bourdeaudhuij, I.; Van der Mispel, C.; Shadid, S.; Verloigne, M. Experiences and opinions of adults with type 2 diabetes regarding a self-regulation-based ehealth intervention targeting physical activity and sedentary behaviour. Int. J. Environ. Res. Public Health 2018, 15, 954. [Google Scholar] [CrossRef] [Green Version]
- Schroé, H.; Van Dyck, D.; De Paepe, A.; Poppe, L.; Loh, W.W.; Verloigne, M.; Loeys, T.; De Bourdeaudhuij, I.; Crombez, G. Which behaviour change techniques are effective to promote physical activity and reduce sedentary behaviour in adults: A factorial randomized trial of an e- and m-health intervention. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 127. [Google Scholar] [CrossRef]
- The IPAQ Group. International Physical Activity Questionnaire; IPAQ, 2002. Available online: www.ipaq.ki.se (accessed on 22 March 2022).
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [Green Version]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the international physical activity questionnaire short form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef] [Green Version]
- The IPAQ Group. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)—Short and Long Forms; IPAQ, 2005. Available online: www.ipaq.ki.se (accessed on 22 March 2022).
- Fleig, L.; Pomp, S.; Parschau, L.; Barz, M.; Lange, D.; Schwarzer, R.; Lippke, S. From intentions via planning and behavior to physical exercise habits. Psychol. Sport Exerc. 2013, 14, 632–639. [Google Scholar] [CrossRef]
- Koring, M.; Richert, J.; Lippke, S.; Parschau, L.; Reuter, T.; Schwarzer, R. Synergistic effects of planning and self-efficacy on physical activity. Health Educ. Behav. 2012, 39, 152–158. [Google Scholar] [CrossRef]
- Ryan, R.M. Control and information in the intrapersonal sphere: An extension of cognitive evaluation theory. J. Personal. Soc. Psychol. 1982, 43, 450–461. [Google Scholar] [CrossRef]
- Center for Self-Determination Theory. Intrinsic Motivation Inventory (IMI). Available online: https://selfdeterminationtheory.org/intrinsic-motivation-inventory/ (accessed on 24 December 2021).
- McAuley, E.; Duncan, T.; Tammen, V.V. Psychometric properties of the Intrinsic Motivation Inventory in a competitive sport setting: A confirmatory factor analysis. Res. Q. Exerc. Sport 1989, 60, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Wilbur, J.; Miller, A.; Szalacha, L.; McAuley, E. Correlates of leisure-time physical activity in Korean immigrant women. West. J. Nurs. Res. 2008, 30, 620–638. [Google Scholar] [CrossRef] [PubMed]
- Norman, P.; Conner, M. The Theory of Planned Behavior and Exercise: Evidence for the Mediating and Moderating Roles of Planning on Intention-Behavior Relationships. J. Sport Exerc. Psychol. 2005, 27, 488–504. [Google Scholar] [CrossRef]
- Sheeran, P. Intention—Behavior relations: A conceptual and empirical review. Eur. Rev. Soc. Psychol. 2002, 12, 1–36. [Google Scholar] [CrossRef]
- Sheeran, P.; Milne, S.; Webb, T.L.; Gollwitzer, P. Implementation intentions and health behaviours. In Predicting Health Behavior, 2nd ed.; Conner, M., Norman, P., Eds.; Open University Press/McGraw Hill: Buckingham, UK, 2005; pp. 276–323. [Google Scholar]
- Schoenborn, C.A.; Adams, P.E. Health behaviors of adults: United States, 2005–2007. Vital Health Stat 10 2010, 245, 132. [Google Scholar]
- Bu, E.Q.L.; Chung, H.J. Barriers towards exercise and physical activity of different ethnic groups in middle-aged female Singaporeans. J. Exerc. Rehabil. 2018, 14, 739–745. [Google Scholar] [CrossRef]
- Arora, T.; Grey, I. Health behaviour changes during COVID-19 and the potential consequences: A mini-review. J. Health Psychol. 2020, 25, 1155–1163. [Google Scholar] [CrossRef]
- Morrey, L.B.; Roberts, W.O.; Wichser, L. Exercise-related mental health problems and solutions during the COVID-19 pandemic. Curr. Sports Med. Rep. 2020, 19, 194–195. [Google Scholar] [CrossRef]
- Kwek, K. Coronavirus: Work out at home, urges SportSG, but if you exercise outdoors you may do so with those from your same household. The Straits Times, 21 May 2020. [Google Scholar]
| Variable | Female (n = 49) | Male (n = 36) | Overall Sample (n = 85) | |||
|---|---|---|---|---|---|---|
| Age | ||||||
| Mean (sd) | 25.7 (7.07) | 26.1 (5.86) | 25.8 (6.54) | |||
| Range | 18–55 | 19–56 | 18–56 | |||
| n | % | n | % | n | % | |
| Ethnic representation | ||||||
| Chinese | 40 | 81.6 | 32 | 88.9 | 72 | 84.7 |
| Malay | 2 | 4.1 | 1 | 2.8 | 3 | 3.5 |
| Indian | 2 | 4.1 | - | - | 2 | 2.4 |
| Other | 5 | 10.2 | 3 | 8.3 | 8 | 9.4 |
| Presence of past injuries | 6 | 12.2 | 9 | 25.0 | 15 | 17.6 |
| Met WHO recommend | ||||||
| Time point 1 | 29 | 59.2 | 21 | 58.3 | 50 | 58.8 |
| Time point 2 | 35 | 71.4 | 26 | 72.8 | 61 | 71.8 |
| Possible Response Range | M | SD | Min | Max | |
|---|---|---|---|---|---|
| Motivation to exercise | 10.0–70.0 | 59.9 | 6.9 | 41.0 | 70.0 |
| Action planning scores | 5.0–25.0 | 16.6 | 5.8 | 5.0 | 25.0 |
| Coping planning scores | 5.0–25.0 | 10.2 | 5.0 | 5.0 | 25.0 |
| Past exercise habits (T1–14 days) | |||||
| Moderate exercise | |||||
| Frequency (days) | 0.0–14.0 | 2.6 | 3.0 | 0.0 | 14.0 |
| Duration per session (min) | ≥0 | 28.0 | 34.4 | 0.0 | 180.0 |
| Total time (min) | 113.8 | 290.7 | 0.0 | 2520.0 | |
| Vigorous exercise | |||||
| Frequency (days) | 0.0–14.0 | 4.3 | 3.6 | 0.0 | 14.0 |
| Duration per session (min) | ≥0 | 44.7 | 35.3 | 0.0 | 150.0 |
| Total time (min) | 250.6 | 278.4 | 0.0 | 1260.0 | |
| Walking | 310.8 | 443.9 | 0.0 | 1980.0 | |
| Moderate + Vigorous (min) | 364.4 | 385.1 | 0.0 | 2520.0 | |
| Intentions to exercise | |||||
| Moderate exercise | |||||
| Frequency (days) | 0.0–14.0 | 3.9 | 3.7 | 0.0 | 14.0 |
| Duration per session (min) | ≥0 | 32.6 | 33.6 | 0.0 | 180.0 |
| Total time (min) | 159.8 | 290.3 | 0.0 | 2520.0 | |
| Vigorous exercise | |||||
| Frequency (days) | 0.0–14.0 | 5.6 | 3.6 | 0.0 | 14.0 |
| Duration per session (min) | ≥0 | 24.9 | 31.6 | 0.0 | 150.0 |
| Total time (min) | 288.0 | 279.1 | 0.0 | 1440.0 | |
| Walking | 288.0 | 343.0 | 0.0 | 1680.0 | |
| Moderate + Vigorous (min) | 447.8 | 387.3 | 0.0 | 2520.0 | |
| Actual exercise behaviour (T2) | |||||
| Moderate exercise | |||||
| Frequency (days) | 0.0–14.0 | 3.5 | 3.3 | 0.0 | 14.0 |
| Duration per session (min) | ≥0 | 39.1 | 42.7 | 0.0 | 200.0 |
| Total time (min) | 153.2 | 203.8 | 0.0 | 1400.0 | |
| Vigorous exercise | |||||
| Frequency (days) | 0.0–14.0 | 4.3 | 3.4 | 0.0 | 12.0 |
| Duration per session (min) | ≥0 | 41.3 | 33.8 | 0.0 | 180.0 |
| Total time (min) | 226.6 | 235.0 | 0.0 | 1080.0 | |
| Walking | 313.0 | 394.0 | 0.0 | 2100.0 | |
| Moderate + Vigorous (min) | 379.7 | 306.6 | 0.0 | 1400.0 | |
| Change in exercise behaviour (T2-T1) | |||||
| Moderate exercise (min) | 39.4 | 209.4 | −1120.0 | 690.0 | |
| Vigorous exercise (min) | −24.1 | 173.1 | −720.0 | 360.0 | |
| Moderate + Vigorous (min) | 15.3 | 274.9 | −1120.0 | 930.0 | |
| Effectiveness of planning | 1.0–7.0 | 3.8 | 1.7 | 1.0 | 7.0 |
| Confidence to continue exercise behaviour | 1.0–7.0 | 4.7 | 1.6 | 1.0 | 7.0 |
| Prior habit of planning | 1.0–7.0 | 4.3 | 1.9 | 1.0 | 7.0 |
| Model | Variable | B | SE B | t | p | 95% CI | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Motivation | 0.01 | −0.01 | 0.01 | 3.20 | 4.34 | 0.08 | 0.74 | 0.46 | −0.54, 11.8 |
| 2 | Motivation | 0.27 | 0.26 | 0.27 ^ | 5.48 | 3.76 | 0.14 | 1.46 | 0.15 | −1.99, 12.9 |
| Intentions | −0.37 | 0.07 | −0.52 | −5.47 | 0.00 ** | −0.50, −0.23 | ||||
| 3 | Motivation | 0.41 | 0.39 | 0.14 ^ | 5.16 | 3.40 | 0.13 | 1.52 | 0.13 | −1.61, 11.9 |
| Intentions | 0.22 | 0.15 | 0.31 | 1.49 | 0.14 | −0.08, 0.51 | ||||
| Habits | −0.65 | 0.15 | −0.91 | −4.38 | 0.00 ** | −0.94, −0.35 | ||||
| 4 | Motivation | 0.44 | 0.42 | 0.03 ^ | 2.23 | 3.59 | 0.06 | 0.62 | 0.54 | −4.91, 9.38 |
| Intentions | 0.22 | 0.14 | 0.30 | 1.54 | 0.14 | −0.07, 0.50 | ||||
| Habits | −0.70 | 0.15 | −0.98 | −4.84 | 0.00 ** | −0.99, −0.41 | ||||
| Action Planning | 9.98 | 4.62 | 0.21 | 2.60 | 0.03 * | 0.79, 19.2 | ||||
| 5 | Motivation | 0.45 | 0.42 | 0.01 | 2.95 | 3.68 | 0.07 | 0.80 | 0.42 | −4.36, 10.3 |
| Intentions | 0.24 | 0.15 | 0.34 | 1.65 | 0.10 | −0.05, 0.54 | ||||
| Habits | −0.72 | 0.15 | −1.01 | −4.84 | 0.00 ** | −1.01, −0.42 | ||||
| Action Planning | 1254 | 5.35 | 0.26 | 2.34 | 0.02 * | 1.85, 23.2 | ||||
| Coping Planning | −5.69 | 6.09 | −0.10 | −0.94 | 0.35 | −17.8, 6.42 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wee, Z.Q.C.; Dillon, D. Increasing Physical Exercise through Action and Coping Planning. Int. J. Environ. Res. Public Health 2022, 19, 3883. https://doi.org/10.3390/ijerph19073883
Wee ZQC, Dillon D. Increasing Physical Exercise through Action and Coping Planning. International Journal of Environmental Research and Public Health. 2022; 19(7):3883. https://doi.org/10.3390/ijerph19073883
Chicago/Turabian StyleWee, Zhi Qiang Clement, and Denise Dillon. 2022. "Increasing Physical Exercise through Action and Coping Planning" International Journal of Environmental Research and Public Health 19, no. 7: 3883. https://doi.org/10.3390/ijerph19073883
APA StyleWee, Z. Q. C., & Dillon, D. (2022). Increasing Physical Exercise through Action and Coping Planning. International Journal of Environmental Research and Public Health, 19(7), 3883. https://doi.org/10.3390/ijerph19073883







