Public Compliance Matters in Evidence-Based Public Health Policy: Evidence from Evaluating Social Distancing in the First Wave of COVID-19
Abstract
:1. Introduction
2. Literature Review
2.1. The Differentiating Function of Evidence in COVID-19 from Traditional Public Policy
2.2. The Exploring Debate on the Determinants of Social Distancing Practice and Its Impact
3. Data and Methods
3.1. Data and Variables
3.2. Estimation Technique
4. Results
4.1. Public Compliance Conditions
4.2. Policy Magnitude Co-Weights
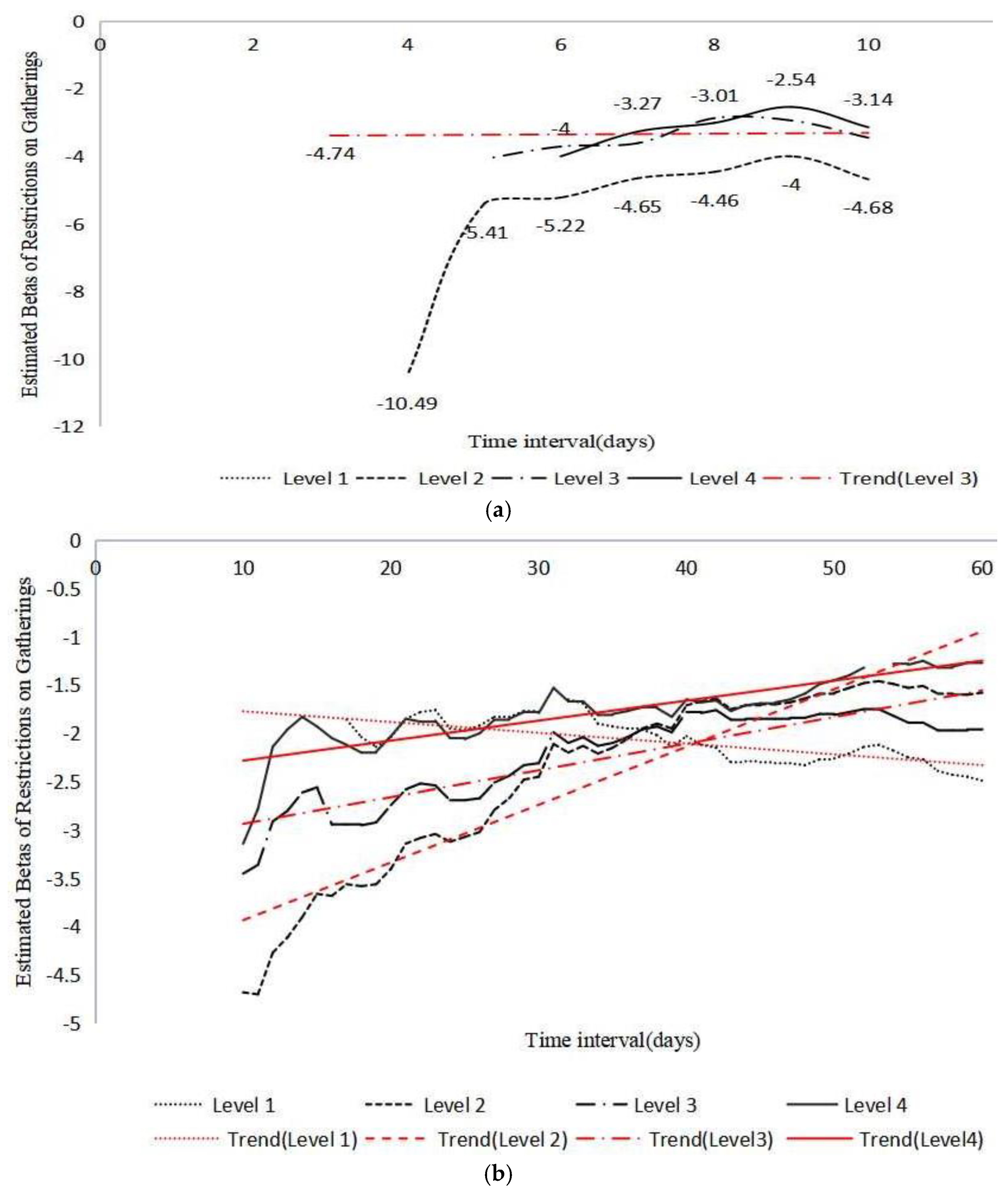
4.3. Policy Duration Matters
5. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. WHO Coronavirus (COVID-19) Dashboard (as of 5:18 pm CET, 4 March 2022). 2022. Available online: https://covid19.who.int/ (accessed on 27 December 2021).
- The World Bank. COVID-19 to plunge global economy into worst recession since World War II. 2020. Available online: https://www.worldbank.org/en/news/press-release/2020/06/08/covid-19-to-plunge-global-economy-into-worst-recession-since-world-war-ii (accessed on 27 December 2021).
- The World Bank. World Development Report 2022: Finance for an equitable recovery. 2022. Available online: https://openknowledge.worldbank.org/bitstream/handle/10986/36883/9781464817304.pdf (accessed on 27 December 2021).
- Bowleg, L. We’re not all in this together: On COVID-19, intersectionality, and structural inequality. Am. J. Public Health 2020, 110, 917. [Google Scholar] [CrossRef] [PubMed]
- Musinguzi, G.; Asamoah, B.O. The science of social distancing and total lock down: Does it work? Whom does it benefit? Electron. J. Gen. Med. 2020, 17, em230. [Google Scholar] [CrossRef] [Green Version]
- Mudenda, S. Coronavirus disease (COVID-19): A global health problem. Int. J. Pharm. Pharmacol. 2020, 4, 1–2. [Google Scholar]
- Gesser-Edelsburg, A. How to make health and risk communication on social media more “social” during COVID-19. Risk Manag. Healthc. Policy 2021, 14, 3523–3540. [Google Scholar] [CrossRef] [PubMed]
- How States Can Promote Compliance with Social Distancing. 7 May 2020. Available online: https://hub.jhu.edu/2020/05/06/promoting-compliance-with-social-distancing/ (accessed on 10 December 2021).
- Bierwiaczonek, K.; Kunst, J.R.; Pich, O. Belief in COVID-19 conspiracy theories reduces social distancing over time. Appl. Psychology. Health Well-Being 2020, 12, 1270–1285. [Google Scholar] [CrossRef] [PubMed]
- Alfano, V.; Ercolano, S. The efficacy of lockdown against COVID-19: A cross-country panel analysis. Appl. Health Econ. Health Policy 2020, 18, 507–517. [Google Scholar] [CrossRef]
- HARVARD. How COVID-19 Has Changed Public Policy. 2020. Available online: https://www.hks.harvard.edu/faculty-research/policy-topics/public-leadership-management/how-covid-19-has-changed-public-policy (accessed on 27 December 2021).
- Lamont, T. But does it work?Evidence, policy-making and systems thinking—Comment on “what can policy-makers get out of systems thinking? Policy partners’ experiences of a systems-focused research collaboration in preventive health”. Int. J. Health Policy Manag. 2020, 10, 287–289. [Google Scholar] [CrossRef]
- Oliver, K.A.; Vocht, F.D. Defining ‘evidence’ in public health: A survey of policymakers’ uses and preferences. Eur. J. Public Health 2017, 27, 112–117. [Google Scholar] [CrossRef] [Green Version]
- Gollust, S.E.; Fowler, E.F.; Niederdeppe, J. Television news coverage of public health issues and implications for public health policy and practice. Annu. Rev. Public Health 2019, 40, 167–185. [Google Scholar] [CrossRef] [Green Version]
- Van de Goor, I.; Hämäläinenb, R.-M.; Syedc, A.; Laud, C.J.; Sandue, P.; Spitters, H.; Karlssonf, L.E.; Dulf, D.; Valente, A.; Castellani, T.; et al. Determinants of evidence use in public health policy making: Results from a study across six EU countries. Health Policy 2017, 121, 273–281. [Google Scholar] [CrossRef]
- McCaughey, D.; Bruning, N.S. Debate Rationality versus reality: The challenges of evidence-based decision making for health policy makers. Implement. Sci. 2010, 5, 39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arcand, J.-L. The (lack of) impact of impact: Why impact evaluations seldom lead to evidence-based policymaking. Revue d’économie du développement 2013, 21, 193–218. [Google Scholar] [CrossRef] [Green Version]
- Cairney, P.; Oliver, K.; Wellstead, A. To bridge the divide between evidence and policy: Reduce ambiguity as much as uncertainty. Evid. Public Adm. 2016, 76, 399–402. [Google Scholar] [CrossRef] [Green Version]
- Innvær, S.; Vist, G.; Trommald, M.; Oxman, A. Health policy-makers’ perceptions of their use of evidence: A systematic review. J. Health Serv. Res. Policy 2002, 7, 239–244. [Google Scholar] [CrossRef]
- Field, P.; Gauld, R.; Lawrence, M. Evidence-informed health policy—The crucial role of advocacy. Int. J. Clin. Pract. 2012, 66, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Onwujekwe, O.; Uguru, N.; Russo, G.; Etiaba, E.; Mbachu, C.; Mirzoev, T.; Uzochukwu, B. Role and use of evidence in policymaking: An analysis of case studies from the health sector in Nigeria. Health Res. Policy Syst. 2015, 13, 46. [Google Scholar] [CrossRef] [PubMed]
- Ogilvie, D.; Craig, P.; Griffin, S.J.; Macintyre, S.; Wareham, N.J. A translational framework for public health research. BMC Public Health 2009, 9, 116. [Google Scholar] [CrossRef] [Green Version]
- Cairney, P.; Yamazaki, M. A comparison of tobacco policy in the UK and Japan: If the scientific evidence is identical, why is there a major difference in policy? J. Comp. Policy Anal. Res. Pract. 2018, 20, 253–268. [Google Scholar] [CrossRef]
- Akpan, D. Translating evidence into public health practice. J. Health Med. Nurs. 2017, 38, 61–64. [Google Scholar]
- Oksanen, A.; Kaakinen, M.; Latikka, R.; Savolainen, I.; Savela, N.; Koivula, A. Regulation and trust: 3-month follow-up study on COVID-19 mortality in 25 European countries. JMIR Public Health Surveill. 2020, 6, e19218. [Google Scholar] [CrossRef]
- Nutbeam, D. COVID-19: Lessons in risk communication and public trust. Public Health Res. Pract. 2020, 30, 3022006. [Google Scholar] [CrossRef] [PubMed]
- Sohrabi, C.; Alsafi, Z.; O’Neill, N.K.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, R.A. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Hartley, D.M.; Perencevich, E.N. Public health interventions for COVID-19: Emerging evidence and implications for an evolving public health crisis. JAMA 2020, 323, 1908–1909. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Flynn, J. Confronting the big challenges of our time: Making a difference during and after COVID-19. Public Manag. Rev. 2020, 23, 961–980. [Google Scholar] [CrossRef]
- WHO. Coronavirus Disease (COVID-19): How Is It Transmitted? 2021. Available online: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-how-is-it-transmitted (accessed on 27 December 2021).
- Chang, S.; Wilson, M.L.; Lewis, B.; Mehrab, Z.; Dudakiya, K.K.; Pierson, E.; Koh, P.W.; Gerardin, J.; Redbird, B.; Grusky, D.B.; et al. Supporting COVID-19 policy response with large-scale mobility-based modeling. medRxiv 2021, 2632–2642. [Google Scholar] [CrossRef]
- Glass, R.J.; Glass, L.M.; Beyeler, W.E.; Min, H.J. Targeted social distancing design for pandemic influenza. Emerg. Infect. Dis. 2006, 12, 1671–1681. [Google Scholar] [CrossRef]
- Siedner, M.J.; Harling, G.; Reynolds, Z.; Gilbert, R.F.; Haneuse, S.; Venkataramani, A.S.; Tsai, A.C. Correction: Social distancing to slow the US COVID-19 epidemic: Longitudinal pretest-posttest comparison group study. PLoS Med. 2020, 17, e1003376. [Google Scholar] [CrossRef]
- Liu, H.; Chen, C.; Cruz-Cano, R.; Guida, J.L.; Lee, M. Public compliance with social distancing measures and SARS-CoV-2 spread: A quantitative analysis of 5 states. Public Health Rep. 2021, 136, 475–482. [Google Scholar] [CrossRef]
- Greenstone, M.; Nigam, V. Does Social Distancing Matter? University of Chicago, Becker Friedman Institute for Economics Working Paper No. 2020-26 2020. Available online: https://bfi.uchicago.edu/wp-content/uploads/BFI_WP_202026.pdf (accessed on 15 June 2020).
- Matrajt, L.; Leung, T. Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerg. Infect. Dis. 2020, 26, 1740–1748. [Google Scholar] [CrossRef]
- Courtemanche, C.; Garuccio, J.; Le, A.; Pinkston, J.; Yelowitz, A. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff. 2020, 39, 1237–1246. [Google Scholar] [CrossRef]
- An, B.Y.; Porcher, S.; Tang, S.-Y.; Kim, E.E. Policy design for COVID-19: Worldwide evidence on the efficacies of early mask mandates and other policy interventions. Public Adm. Rev. 2021, 81, 1157–1182. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, N.M.; Cummings, D.A.T.; Fraser, C.; Cajka, J.C.; Cooley, P.C.; Burke, D.S. Strategies for mitigating an influenza pandemic. Nature 2006, 442, 448–452. [Google Scholar] [CrossRef] [PubMed]
- Aliyu, A.A. Public health ethics and the COVID-19 pandemic. Ann. Afr. Med. 2021, 20, 157–163. [Google Scholar]
- Nilsen, P.; Seing, I.; Ericsson, C.; Andersen, O.; Stefánsdóttir, N.T.; Tjørnhøj-Thomsen, T.; Kallemose, T.; Kirk, J.W. Implementing social distancing policy measures in the battle against the coronavirus: Protocol of a comparative study of Denmark and Sweden. Implement. Sci. Commun. 2020, 1, 77. [Google Scholar] [CrossRef] [PubMed]
- Plohl, N.; Musil, B. Modeling compliance with COVID-19 prevention guidelines: The critical role of trust in science. Psychol. Health Med. 2020, 26, 1–12. [Google Scholar]
- Maaravi, Y.; Levy, A.; Gur, T.; Confino, D.; Segal, S. “The tragedy of the commons”: How individualism and collectivism affected the spread of the COVID-19 pandemic. Front. Public Health 2021, 9, 627559. [Google Scholar] [CrossRef]
- Gualda, E.; Krouwel, A.; Palacios-Gálvez, M.; Morales-Marente, E.; Rodríguez-Pascual, I.; García-Navarro, E.B. Social distancing and COVID-19: Factors associated with compliance with social distancing norms in Spain. Front. Psychol. 2021, 12, 727225. [Google Scholar] [CrossRef] [PubMed]
- Hansen, A.C.; Farewell, C.V.; Jewell, J.S.; Leiferman, J.A. Exploring predictors of social distancing compliance in the United States during the COVID-19 pandemic. Disaster Med. Public Health Prep. 2021, 1–7. [Google Scholar] [CrossRef]
- Sturman, D.; Auton, J.C.; Thacker, J. Knowledge of social distancing measures and adherence to restrictions during the COVID-19 pandemic. Health Promot. J. Aust. 2021, 32, 344–351. [Google Scholar] [CrossRef]
- Nivette, A.; Ribeaud, D.; Murray, A.; Steinhoff, A.; Bechtiger, L.; Hepp, U.; Shanahan, L.; Eisner, M. Non-compliance with COVID-19-related public health measures among young adults in Switzerland: Insights from a longitudinal cohort study. Soc. Sci. Med. 2021, 268, 113370. [Google Scholar] [CrossRef]
- Aubert, C.; Augeraud-Véron, E. The relative power of individual distancing efforts and public policies to curb the COVID-19 epidemics. PLoS ONE 2021, 16, e0250764. [Google Scholar] [CrossRef] [PubMed]
- Clements, J.M. Knowledge and behaviors toward COVID-19 among US residents during the early days of the pandemic: Cross-sectional online questionnaire. JMIR Public Health Surveill. 2020, 6, e19161. [Google Scholar] [CrossRef] [PubMed]
- Castaneda, M.A.; Saygili, M. The effect of shelter-in-place orders on social distancing and the spread of the COVID-19 pandemic: A study of Texas. Front. Public Health 2020, 8, 596607. [Google Scholar] [CrossRef] [PubMed]
- Yezli, S.; Khan, A.A. COVID-19 social distancing in the Kingdom of Saudi Arabia: Bold measures in the face of political, economic, social and religious challenges. Travel Med. Infect. Dis. 2020, 37, 101692. [Google Scholar] [CrossRef] [PubMed]
- Andersen, M. Early Evidence on Social Distancing in Response to COVID-19 in the United States. 2020. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3569368 (accessed on 27 December 2021).
- Anderson, R.M.; Heesterbeek, H.; Klinkenberg, D.; Hollingsworth, T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet 2020, 395, 931–934. [Google Scholar] [CrossRef]
- Siordia, J.A. Epidemiology and clinical features of COVID-19: A review of current literature. J. Clin. Virol. 2020, 127, 104357. [Google Scholar] [CrossRef]
- Khataee, H.; Scheuring, I.; Czirók, A.; Neufeld, Z. Effects of social distancing on the spreading of COVID-19 inferred from mobile phone data. Sci. Rep. 2021, 11, 1661. [Google Scholar] [CrossRef]
- Stein, R.A. COVID-19 and rationally layered social distancing. Int. J. Clin. Pract. 2020, 74, e13501. [Google Scholar] [CrossRef]
- Fang, H.; Wang, L.; Yang, Y. Human Mobility Restrictions and the Spread of the Novel Coronavirus (2019-NCOV) in China. 2020. Available online: https://www.nber.org/papers/w26906 (accessed on 28 June 2020).
- Ahammer, A.; Halla, M.; Lackner, M. Mass Gatherings Contributed to Early COVID-19 Spread: Evidence from US Sports. CDL Aging, Health, Labor Working Papers 2020. Available online: https://ideas.repec.org/p/jku/cdlwps/wp2003.html (accessed on 1 July 2020).
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef]
- Wang, C. Evidence and policy response in COVID-19: A comparative analysis of selected European countries. 2020; Unpublished working paper. [Google Scholar]
- Suzuki, K.; Hasegawa, T.; Kano, N.; Okamoto, Y. A study of the effect of wearing face masks in preventing COVID-19 transmission in the United States of America. Public Adm. Policy 2021, 24, 275–289. [Google Scholar] [CrossRef]
- Bassanello, M.; Pasini, L.; Senzolo, M.; Gambaro, A.; Roman, M.; Coli, U.; D’Aquino, M. Epidemiological study in a small rural area of Veneto (Italian region) during SARS-Cov-2 pandemia. Sci. Rep. 2021, 11, 23247. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.; Mindermann, S.; Rogers-Smith, C.; Leech, G.; Snodin, B.; Ahuja, J.; Sandbrink, J.B.; Monrad, J.T.; Altman, G.; Dhaliwal, G.; et al. Understanding the effectiveness of government interventions against the resurgence of COVID-19 in Europe. Nat. Commun. 2021, 12, 5820. [Google Scholar] [CrossRef] [PubMed]
- Patterson-Lomba, O. Optimal timing for social distancing during an epidemic. medRxiv 2020. Available online: https://www.medrxiv.org/content/10.1101/2020.03.30.20048132v1.full.pdf (accessed on 1 September 2020).
- Ogilvie, D.; Adams, J.; Bauman, A.; Gregg, E.W.; Panter, J.; Siegel, K.R.; Wareham, N.J.; White, M. Using natural experimental studies to guide public health action: Turning the evidence-based medicine paradigm on its head. J. Epidemiol. Community Health 2019, 74, 203–208. [Google Scholar] [CrossRef] [Green Version]
- Fezzi, C.; Fanghella, V. Tracking GDP in real-time using electricity market data: Insights from the first wave of COVID-19 across Europe. Eur. Econ. Rev. 2021, 139, 103907. [Google Scholar] [CrossRef] [PubMed]
- Simonetti, O.; Martini, M.; Armocida, E. COVID-19 and Spanish flu-18: Review of medical and social parallelisms between two global pandemics. J. Prev. Med. Hyg. 2021, 62, E613–E620. [Google Scholar]
- Bonaccorsi, G.; Pierri, F.; Cinelli, M.; Flori, A.; Galeazzi, A.; Porcelli, F.; Schmidt, A.L.; Valensise, C.M.; Scala, A.; Quattrociocchi, W.; et al. Economic and social consequences of human mobility restrictions under COVID-19. Proc. Natl. Acad. Sci. USA 2020, 117, 15530–15535. [Google Scholar] [CrossRef]
- Maharaj, S.; Kleczkowski, A. Controlling epidemic spread by social distancing: Do it well or not at all. BMC Public Health 2012, 12, 679. [Google Scholar] [CrossRef] [Green Version]
- Reluga, T.C. Game theory of social distancing in response to an epidemic. PLoS Comput. Biol. 2010, 6, e1000793. [Google Scholar] [CrossRef]
- Lewnard, J.A.; Lo, N.C. Scientific and ethical basis for social-distancing interventions against COVID-19. Lancet Infect. Dis. 2020, 20, 631–633. [Google Scholar] [CrossRef] [Green Version]
- Lake, M.A. What we know so far: COVID-19 current clinical knowledge and research. Clin. Med. 2020, 20, 124–127. [Google Scholar] [CrossRef] [Green Version]
- Gollier, C. Pandemic economics: Optimal dynamic confinement under uncertainty and learning. Geneva Risk Insur. Rev. 2020, 45, 80–93. [Google Scholar] [CrossRef] [PubMed]
- Bavel, J.J.V.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Crockett, M.J.; Crum, A.J.; Douglas, K.M.; Druckman, J.N.; et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef] [PubMed]
| Variables | Data Sources | Observations | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|---|---|
| cases | ECDC | 17,812 | 373.236 | 2006.523 | 0 | 48,529 |
| gre | OxCGRT | 17,812 | - | - | 0 | 1 |
| days | OxCGRT | 17,812 | 28.034 | 27.810 | 0 | 141 |
| resg | OxCGRT | 17,812 | - | - | 0 | 4 |
| dnst | World Bank | 17,812 | 237.710 | 780.456 | 0.136 | 7952.998 |
| Dependent Variable: Cases | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Restriction on Gatherings (resg) | 938.265 *** (29.874) | 979.915 *** (31.282) | |
| Population Density (dnst) | −0.035 (0.127) | 0.073 (0.136) | |
| Restriction on Gatherings × Population Density | −0.135 *** (0.030) | ||
| Constant | −393.345 *** (90.551) | 297.389 *** (86.851) | −420.428 *** (95.387) |
| Observations | 17,812 | 17,812 | 17,812 |
| Log Likelihood | −156,363.800 | −156,848.100 | −156,357.600 |
| Akaike Inf. Crit. | 312,735.600 | 313,704.100 | 312,727.200 |
| Bayesian Inf. Crit. | 312,766.800 | 313,735.300 | 312,773.900 |
| Dependent Variable: Cases | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Level 1 | −436.224 (280.420) | 16.019 (231.021) | −658.557 *** (246.059) |
| Level 2 | −485.387 ** (208.981) | −472.733 ** (208.277) | −1147.309 *** (225.623) |
| Level 3 | −403.168 ** (197.717) | −403.980 ** (197.840) | −1078.556 *** (221.733) |
| Level 4 | 383.896 * (205.047) | 347.572 * (204.914) | −327.004 (217.733) |
| Population Density (dnst) | 2.697 ** (1.371) | −1.147 *** (0.439) | |
| Level 2 × Population Density | −3.758 *** (1.302) | ||
| Level 3 × Population Density | −3.773 *** (1.302) | ||
| Level 4 × Population Density | −3.898 *** (1.301) | ||
| Observations | 12,024 | 12,024 | 12,024 |
| R2 | 0.734 | 0.733 | 0.733 |
| Adjusted R2 | 0.727 | 0.726 | 0.726 |
| Residual Std. Error | 1291.405 (df = 11,723) | 1292.377 (df = 11,726) | 1292.377 (df = 11,726) |
| F Statistic | 107.291 *** (df = 301; 11,723) | 108.139 *** (df = 298; 11,726) | 108.139 *** (df = 298; 11,726) |
| Time Interval | Restriction on Gatherings Level: | |||
|---|---|---|---|---|
| Level 1 | Level 2 | Level 3 | Level 4 | |
| 3 days | −3.277 | −3.375 * | −2.738 ** | −4.738 ** |
| (2.011) | (1.855) | (1.301) | (2.052) | |
| 7 days | 0.803 | −4.646 *** | −3.612 *** | −3.267 ** |
| (1.666) | (1.359) | (1.225) | (1.337) | |
| 15 days | −1.227 | −3.662 *** | −2.563 *** | −1.930 ** |
| (0.924) | (0.868) | (0.824) | (0.837) | |
| 30 days | −1.764 ** | −2.454 *** | −2.308 *** | −1.785 *** |
| (0.788) | (0.701) | (0.660) | (0.676) | |
| 40 days | −2.028 *** | −1.711 *** | −1.780 *** | −1.654 *** |
| (0.770) | (0.663) | (0.619) | (0.637) | |
| 50 days | −2.262 *** | −1.582 ** | −1.813 *** | −1.453 ** |
| (0.782) | (0.660) | (0.622) | (0.633) | |
| 60 days | −2.495 *** | −1.576 ** | −1.945 *** | −1.269 ** |
| (0.791) | (0.658) | (0.623) | (0.630) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, C.; Li, H. Public Compliance Matters in Evidence-Based Public Health Policy: Evidence from Evaluating Social Distancing in the First Wave of COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 4033. https://doi.org/10.3390/ijerph19074033
Wang C, Li H. Public Compliance Matters in Evidence-Based Public Health Policy: Evidence from Evaluating Social Distancing in the First Wave of COVID-19. International Journal of Environmental Research and Public Health. 2022; 19(7):4033. https://doi.org/10.3390/ijerph19074033
Chicago/Turabian StyleWang, Caixia, and Huijie Li. 2022. "Public Compliance Matters in Evidence-Based Public Health Policy: Evidence from Evaluating Social Distancing in the First Wave of COVID-19" International Journal of Environmental Research and Public Health 19, no. 7: 4033. https://doi.org/10.3390/ijerph19074033







