Comparative Study of Malocclusions between Cancer Patients and Healthy Peers
Abstract
:1. Introduction
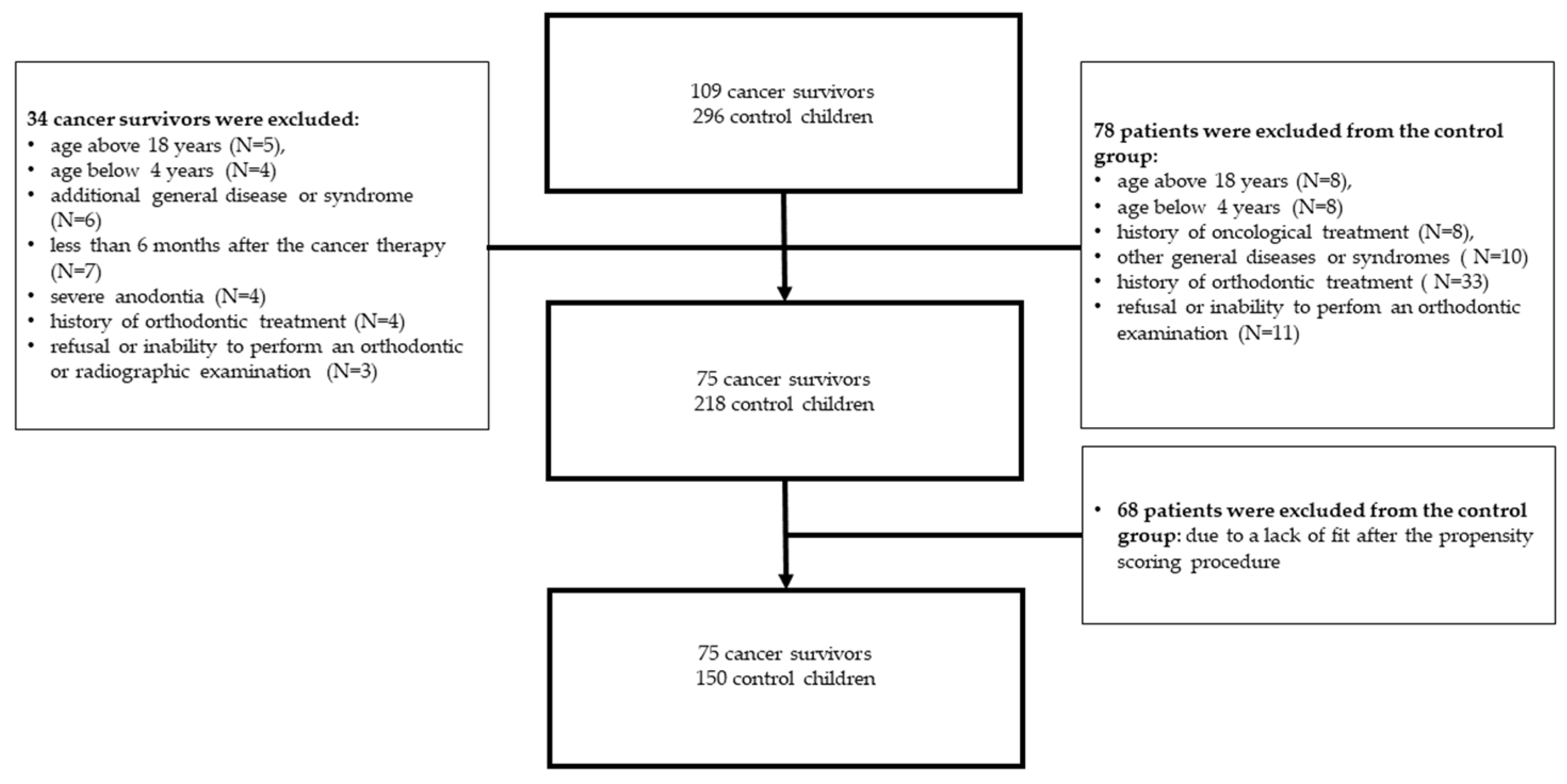
2. Materials and Methods
2.1. Study Group Description
2.2. Orthodontic Assessment in Both Groups
2.3. Assessment of Dental Anomalies and Dental Age in Cancer Group
2.4. Assessment of Treatment-Related Variables in Cancer Group
2.5. Statistical Analysis
3. Results
3.1. Comparison of Types of Dental Occlusion in Both Groups
3.2. Dental Anomalies and Dental Age Estimation in Cancer Patients
3.3. Cancer Treatment Related Variables and Subsequent Orthodontic Treatment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hassan, R.; Rahimah, A. Occlusion, malocclusion and method of measurements—An overview. Arch. Orofac. Sci. 2007, 2, 3–9. [Google Scholar]
- Andrews, L.F. The six keys to normal occlusion. Am. J. Orthod. 1972, 62, 296–309. [Google Scholar] [CrossRef]
- Ackerman, J.L.; Proffit, W.R.; Sarver, D.M. The emerging soft tissue paradigm in orthodontic diagnosis and treatment planning. Clin. Orthod. Res. 1999, 2, 49–52. [Google Scholar] [CrossRef] [PubMed]
- Stern, S.; Finke, H.; Strosinski, M.; Mueller-Hagedorn, S.; McNamara, J.A.; Stahl, F. Longitudinal changes in the dental arches and soft tissue profile of untreated subjects with normal occlusion. J. Orofac. Orthop./Fortschr. Kieferorthopädie 2020, 81, 192–208. [Google Scholar] [CrossRef] [PubMed]
- Davies, S.J. Malocclusion—A term in need of dropping or redefinition? Br. Dent. J. 2007, 202, 519–520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marmaite, U.; Kasparaviciene, K.; Sidlauskas, A.; Zasciurinskiene, E.; Vasiliauskas, A.; Juodzbalys, G. The prevalence of malocclusion and oral habits among 5–7-year-old children. Med. Sci. Monit. 2014, 20, 2036–2042. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zou, J.; Meng, M.; Law, C.S.; Rao, Y.; Zhou, X. Common dental diseases in children and malocclusion. Int. J. Oral Sci. 2018, 10, 7. [Google Scholar] [CrossRef]
- D’Onofrio, L. Oral dysfunction as a cause of malocclusion. Orthod. Craniofac. Res. 2019, 22, 43–48. [Google Scholar] [CrossRef]
- Hanisch, M.; Hanisch, L.; Kleinheinz, J.; Danesh, G.; Benz, K.; Jackowski, J. Orthodontically relevant manifestations in people with rare diseases. Med. Princ. Pract. 2019, 28, 216–221. [Google Scholar] [CrossRef]
- Sidorowicz, W.; Kubasiewicz-Ross, P.; Dominiak, M. Familial cherubism: Clinical and radiological features. Case report and review of the literature. Eur. J. Paediatr. Dent. 2018, 19, 213–217. [Google Scholar] [CrossRef]
- Vilar, L.; Vilar, C.F.; Lyra, R.; Lyra, R.; Naves, L.A. Acromegaly: Clinical features at diagnosis. Pituitary 2017, 20, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Proc, P.; Szczepańska, J.; Skiba, A.; Zubowska, M.; Fendler, W.; Młynarski, W. Dental anomalies as late adverse effect among young children treated for cancer. Cancer Res. Treat. 2016, 48, 658–667. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seremidi, K.; Kavvadia, K.; Kattamis, A.; Polychronopoulou, A. Dental late effects of antineoplastic treatment on childhood cancer survivors: Radiographic findings. Int. J. Paediatr. Dent. 2021, 31, 742–751. [Google Scholar] [CrossRef] [PubMed]
- Proc, P.; Szczepańska, J.; Zubowska, M.; Zalewska-Szewczyk, B.; Młynarski, W. The broad variability in dental age observed among childhood survivors is cancer specific. Cancer Res. Treat. 2021, 53, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Uslu, O.; Akçam, M.O.; Evirgen, S.; Cebeci, I. Prevalence of dental anomalies in various malocclusions. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 328–335. [Google Scholar] [CrossRef]
- Fernandez, C.C.A.; Pereira, C.V.C.A.; Luiz, R.R.; Vieira, A.R.; Costa, M.D.C. Dental anomalies in different growth and skeletal malocclusion patterns. Angle Orthod. 2017, 88, 195–201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pedreira, F.R.D.O.; De Carli, M.L.; Pedreira, R.D.P.G.; Ramos, P.D.S.; Pedreira, M.R.; Robazza, C.R.C.; Hanemann, J.A.C. Association between dental anomalies and malocclusion in Brazilian orthodontic patients. J. Oral Sci. 2016, 58, 75–81. [Google Scholar] [CrossRef] [Green Version]
- Bezroukov, V.; Freer, T.J.; Helm, S.; Kalamkarov, H.; Infirri, J.S.; Solow, B. Basic method for recording occlusal traits. Bull. World Health Organ. 1979, 57, 955–961. [Google Scholar]
- Hölttä, P.; Hovi, L.; Saarinen-Pihkala, U.M.; Peltola, J.; Alaluusua, S. Disturbed root development of permanent teeth after pediatric stem cell transplantation. Cancer 2005, 103, 1484–1493. [Google Scholar] [CrossRef] [PubMed]
- Demirjian, A.; Goldstein, H.; Tanner, J.M. A new system of dental age assessment. Hum. Biol. 1973, 45, 211–227. [Google Scholar]
- Lombardo, G.; Vena, F.; Negri, P.; Pagano, S.; Barilotti, C.; Paglia, L.; Colombo, S.; Orso, M.; Cianetti, S. Worldwide prevalence of malocclusion in the different stages of dentition: A systematic review and meta-analysis. Eur. J. Paediatr. Dent. 2020, 21, 115–123. [Google Scholar]
- Alhammadi, M.S.; Halboub, E.; Fayed, M.S.; Labib, A.; El-Saaidi, C. Global distribution of malocclusion traits: A systematic review. Dent. Press J. Orthod. 2018, 23, e1–e10. [Google Scholar] [CrossRef] [PubMed]
- Gudipaneni, R.K.; Aldahmeshi, R.F.; Patil, S.R.; Alam, M.K. The prevalence of malocclusion and the need for orthodontic treatment among adolescents in the northern border region of Saudi Arabia: An epidemiological study. BMC Oral Health 2018, 18, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferro, R.; Besostri, A.; Olivieri, A.; Stellini, E. Prevalence of occlusal traits and orthodontic treatment need in 14 year-old adolescents in Northeast Italy. Eur. J. Paediatr. Dent. 2016, 17, 36–42. [Google Scholar] [PubMed]
- De Groot, R.J.; Merkx, M.A.; Hamann, M.N.; Brand, H.S.; De Haan, A.F.; Rosenberg, A.J.; Speksnijder, C.M. Tongue function and its influence on masticatory performance in patients treated for oral cancer: A five-year prospective study. Support. Care Cancer 2020, 28, 1491–1501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neill, C.C.; Migliorati, C.; Trojan, T.; Kaste, S.; Karydis, A.; Rowland, C.; Parris, W. Experience and expertise regarding orthodontic management of childhood and adolescent cancer survivors. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 765–770. [Google Scholar] [CrossRef] [PubMed]
- Rijpstra, C.; Lisson, J.A. Etiology of anterior open bite: A review. J. Orofac. Orthop./Fortschr. Kieferorthopädie 2016, 77, 281–286. [Google Scholar] [CrossRef]
- Celikoglu, M.; Erdem, A.; Dane, A.; Demirci, T. Dental age assessment in orthodontic patients with and without skeletal malocclusions. Orthod. Craniofac. Res. 2011, 14, 58–62. [Google Scholar] [CrossRef]
- Dahllöf, G.; Jönsson, A.; Ulmner, M.; Huggare, J. Orthodontic treatment in long-term survivors after pediatric bone marrow transplantation. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 459–465. [Google Scholar] [CrossRef]
- Cordova, M.J.; Riba, M.B.; Spiegel, D. Post-traumatic stress disorder and cancer. Lancet Psychiatry 2017, 4, 330–338. [Google Scholar] [CrossRef] [Green Version]
- Mitus-Kenig, M.; Derwich, M.; Czochrowska, E.; Pawlowska, E. Quality of life in orthodontic cancer survivor patients—A prospective case-control Study. Int. J. Environ. Res. Public Health 2020, 17, 5824. [Google Scholar] [CrossRef] [PubMed]
- Mitus-Kenig, M.; Derwich, M.; Czochrowska, E.; Pawlowska, E. Cancer survivors present significantly lower long-term stability of orthodontic treatment: A prospective case-control study. Eur. J. Orthod. 2021, 43, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Corner, J.; Wagland, R.; Glaser, A.; Richards, S.M. Qualitative analysis of patients’ feedback from a PROMs survey of cancer patients in England. BMJ Open 2013, 3, e002316. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Cancer Type | Girls | Boys | Total N (%) |
|---|---|---|---|
| Acute leukemia | 9 | 25 | 34 (45.33%) |
| Wilms tumor | 6 | 5 | 11 (14.66%) |
| Neuroblastoma | 3 | 6 | 9 (12%) |
| Other soft tissue tumors | 2 | 7 | 9 (12%) |
| Brain tumor | 3 | 2 | 5 (6.66%) |
| Lymphoma | 0 | 4 | 4 (5.33%) |
| Hepatoblastoma | 0 | 3 | 3 (4%) |
| Total | 23 | 52 | 75 (100%) |
| Occlusion | Cancer N (%) | Control N (%) | p |
|---|---|---|---|
| Malocclusion | 49 (65.33%) | 99 (65.56%) | 0.9727 |
| Class I | 51 (68.00%) | 94 (62.25%) | 0.9361 |
| Class II (distocclusion) | 21 (28.00%) | 52 (34.44%) | 0.3670 |
| Class III (reversed overjet) | 6 (8.00%) | 3 (1.99%) | 0.0628 |
| Abnormal overjet (incisor protrusion) | 3 (4.00%) | 5 (3.31%) | 1.0000 |
| Crossbite anterior | 10 (13.33%) | 6 (3.97%) | 0.0136 |
| Crossbite posterior | 14 (18.67%) | 7 (4.64%) | 0.0012 |
| Open bite anterior | 1 (1.33%) | 13 (8.61%) | 0.0387 |
| Open bite posterior | 2 (2.67%) | 0 | 0.1091 |
| Deep bite | 1 (1.33%) | 12 (7.95%) | 0.0651 |
| Scissors bite | 0 | 2 (1.32%) | 1.0000 |
| Crowding/rotations | 6 (8.00%) | 15 (9.93%) | 0.8195 |
| Malalignment | 14 (18.67%) | 12 (7.95%) | 0.0310 |
| Spacing | 2 (2.67%) | 0 | 0.1091 |
| Midline shift/Mandibular displacement | 3 (4.00%) | 6 (3.97%) | 1.0000 |
| Maxillary narrowing | 1 (1.33%) | 11 (7.28) | 0.0662 |
| Occlusion | Agenesis of Teeth | p | Microdontic Teeth | p | Short Roots | p | |
|---|---|---|---|---|---|---|---|
| Malocclusion | no | 0 (0–2) | 0.2160 | 0 (0–2) | 0.7375 | 0 (0–0) | 0.6838 |
| yes | 0 (0–1) | 0 (0–2) | 0 (0–0) | ||||
| Class I | no | 0 (0–1.5) | 0.9061 | 0 (0–1.5) | 0.8482 | 0 (0–0) | 0.8479 |
| yes | 0 (0–1) | 0 (0–3) | 0 (0–0) | ||||
| Class II (distocclusion) | no | 0 (0–1) | 0.9922 | 0 (0–3) | 0.3874 | 0 (0–0) | 0.8606 |
| yes | 0 (0–1.5) | 0 (0–1) | 0 (0–0) | ||||
| Class III (reversed overjet) | no | 0 (0–2) | 0.2434 | 0 (0–2) | 1.0000 | 0 (0–0) | 0.5806 |
| yes | 0 (0–0) | 0 (0–4) | 0 (0–0) | ||||
| Abnormal overjet (incisors protrusion) | no | 0 (0-1) | 0.9527 | 0 (0–2) | 0.3433 | 0 (0–0) | 0.2241 |
| yes | 0 (0–3) | 2 (0–4) | 0 (0–2) | ||||
| Crossbite anterior | no | 0 (0–2) | 0.9093 | 0 (0–2) | 0.7432 | 0 (0–0) | 0.2143 |
| yes | 0 (0–1) | 0 (0–3.5) | 0 (0–4) | ||||
| Crossbite posterior | no | 0 (0–2) | 0.6998 | 0 (0–2) | 1.0000 | 0 (0–0) | 0.0161 |
| yes | 0 (0–1) | 0 (0–1) | 0 (0–2) | ||||
| Open bite posterior | no | 0 (0–1.5) | 0.3490 | 0 (0–2) | 0.6288 | 0 (0–0) | 0.6374 |
| yes | 0 (0–0) | 2 (0–4) | 0 (0–0) | ||||
| Crowding/rotations | no | 0 (0–2) | 0.1725 | 0 (0–2) | 0.7657 | 0 (0–0) | 0.5152 |
| yes | 0 (0–0) | 0.5 (0–2.5) | 0 (0–0) | ||||
| Malalignment | no | 0 (0–1.5) | 0.5333 | 0 (0–2) | 0.3360 | 0 (0–0) | 0.9388 |
| yes | 0 (0–0) | 1 (0–4) | 0 (0–0) | ||||
| Midline shift/Mandibular displacement | no | 0 (0–1) | 0.0127 | 0 (0–2) | 0.7617 | 0 (0–0) | 0.5505 |
| yes | 3 (1–7) | 1 (0–1) | 0 (0–0) |
| Crossbite | Delta DA-CA | p | |
|---|---|---|---|
| Class I | Yes | 0.53 (0.13–1.27) | 0.2611 |
| No | 1.02 (0.17–2.13) | ||
| Class II (distocclusion) | Yes | 0.92 (0.13–1.65) | 0.9936 |
| No | 0.53 (0.33–1.75) | ||
| Class III (reversed overjet) | Yes | 0.92 (0.17–1.75) | 0.4059 |
| No | 0.28 (−1.27–1.83) | ||
| Abnormal overjet (incisor protrusion) | Yes | 0.92 (0.13–1.75) | 0.9877 |
| No | 0.53 (0.33–2.12) | ||
| Crossbite anterior | Yes | 1.60 (0.53–2.67) | 0.2599 |
| No | 0.84 (0.15–1.46) | ||
| Crossbite posterior | Yes | 1.75 (1.12–3.17) | 0.0235 |
| No | 0.80 (0.13–1.27) | ||
| Crowding/rotations | Yes | 0.93 (0.22–1.83) | 0.4124 |
| No | 0.53 (0.08–1.02) | ||
| Malalignment | Yes | 1.07 (0.31–1.98) | 0.0226 |
| No | 0.12 (−0.23–0.73) | ||
| Spacing | Yes | 0.91 (0.15–1.7) | 0.6671 |
| No | 1.7 (0.22–3.18) |
| Mesio-Distal Changes | Transversal Changes | Vertical Changes | Tooth Disturbances | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | p | Yes | No | p | Yes | No | p | Yes | No | p | |
| Median (25–75) percentile values) | Median (25–75) percentile values) | Median (25–75) percentile values) | Median (25–75) percentile values) | Median (25–75) percentile values) | Median (25–75) percentile values) | Median (25–75) percentile values) | Median (25–75) percentile values) | |||||
| Age at the beginning (mo) | 33 (22–62) | 33 (18.5–48.5) | 0.4655 | 29.5 (17–52) | 33 (22–54) | 0.5450 | 31 (1–79) | 33 (20–53) | 0.7868 | 57 (28–80) | 30.5 (17–39) | 0.0198 |
| Length of disease (mo) | 13 (5–25) | 21 (10–26) | 0.2866 | 21.5 (6–26) | 20 (6–25) | 0.4839 | 24 (5–28) | 20 (6–25) | 0.7043 | 20 (13–26) | 20.5 (6–25) | 0.8342 |
| RTX of head (yes) | 3/23 * | 8/52 | 1.00 | 4/22 | 7/53 | 0.7213 | 0/3 | 11/72 | 1.00 | 2/17 | 9/58 | 1.00 |
| Relapse (yes) | 2/23 | 6/52 | 1.00 | 4/22 | 4/52 | 0.2271 | 0/3 | 8/72 | 1.00 | 2/16 | 6/58 | 1.00 |
| TBI (yes) | 0/23 | 1/52 | 1.00 | 0/22 | 1/53 | 1.00 | 0/3 | 1/72 | 1.00 | 0/17 | 1/58 | 1.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Proc, P.; Szczepanska, J.; Herud, A.; Zubowska, M.; Fendler, W.; Lukomska-Szymanska, M.; Mlynarski, W. Comparative Study of Malocclusions between Cancer Patients and Healthy Peers. Int. J. Environ. Res. Public Health 2022, 19, 4045. https://doi.org/10.3390/ijerph19074045
Proc P, Szczepanska J, Herud A, Zubowska M, Fendler W, Lukomska-Szymanska M, Mlynarski W. Comparative Study of Malocclusions between Cancer Patients and Healthy Peers. International Journal of Environmental Research and Public Health. 2022; 19(7):4045. https://doi.org/10.3390/ijerph19074045
Chicago/Turabian StyleProc, Patrycja, Joanna Szczepanska, Anna Herud, Malgorzata Zubowska, Wojciech Fendler, Monika Lukomska-Szymanska, and Wojciech Mlynarski. 2022. "Comparative Study of Malocclusions between Cancer Patients and Healthy Peers" International Journal of Environmental Research and Public Health 19, no. 7: 4045. https://doi.org/10.3390/ijerph19074045







