Sleep and Sleepiness Measured by Diaries and Actigraphy among Norwegian and Austrian Helicopter Emergency Medical Service (HEMS) Pilots
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.3.1. Questionnaire
2.3.2. Mission Log
2.3.3. Sleep Diary
2.3.4. Actigraphy
2.3.5. Karolinska Sleepiness Scale
2.4. Data Analyses
2.5. Missing Data
2.6. Ethics
3. Results
3.1. Descriptive Statistics
3.2. Number of Missions and Time Spent on Missions
3.3. Sleep Measured throughout the Workweek
3.3.1. Bedtime and Wake-Up Time
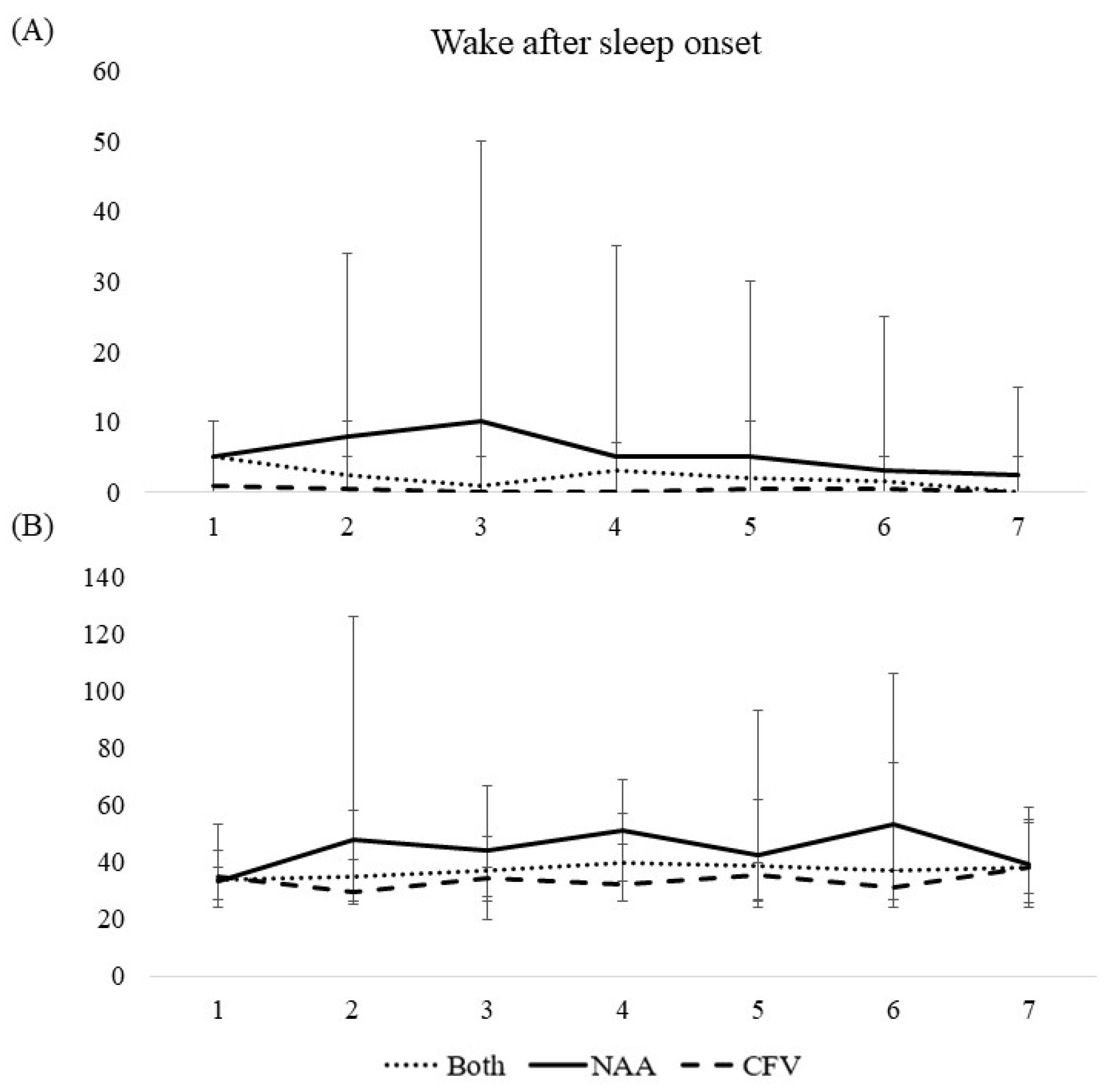
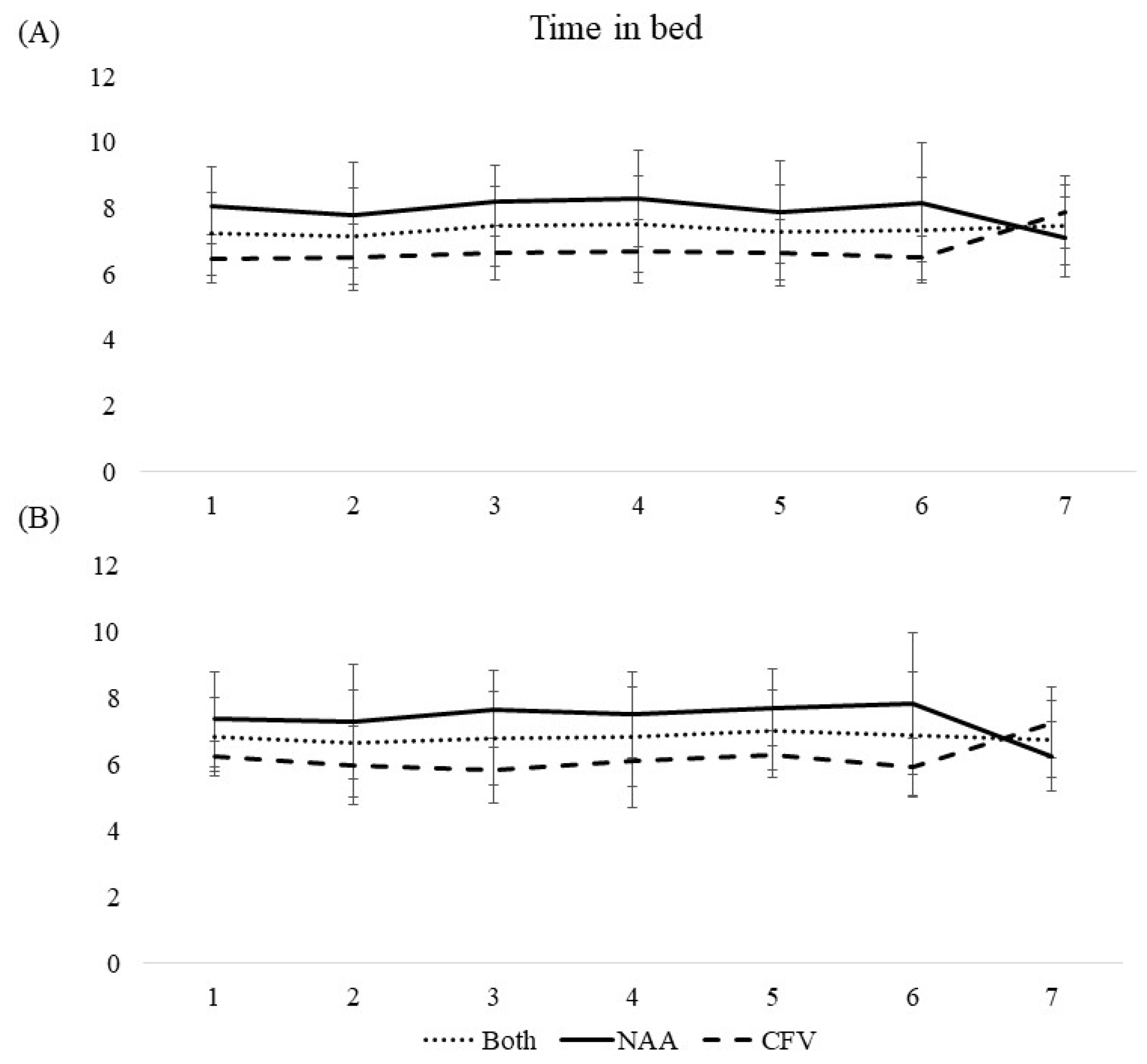
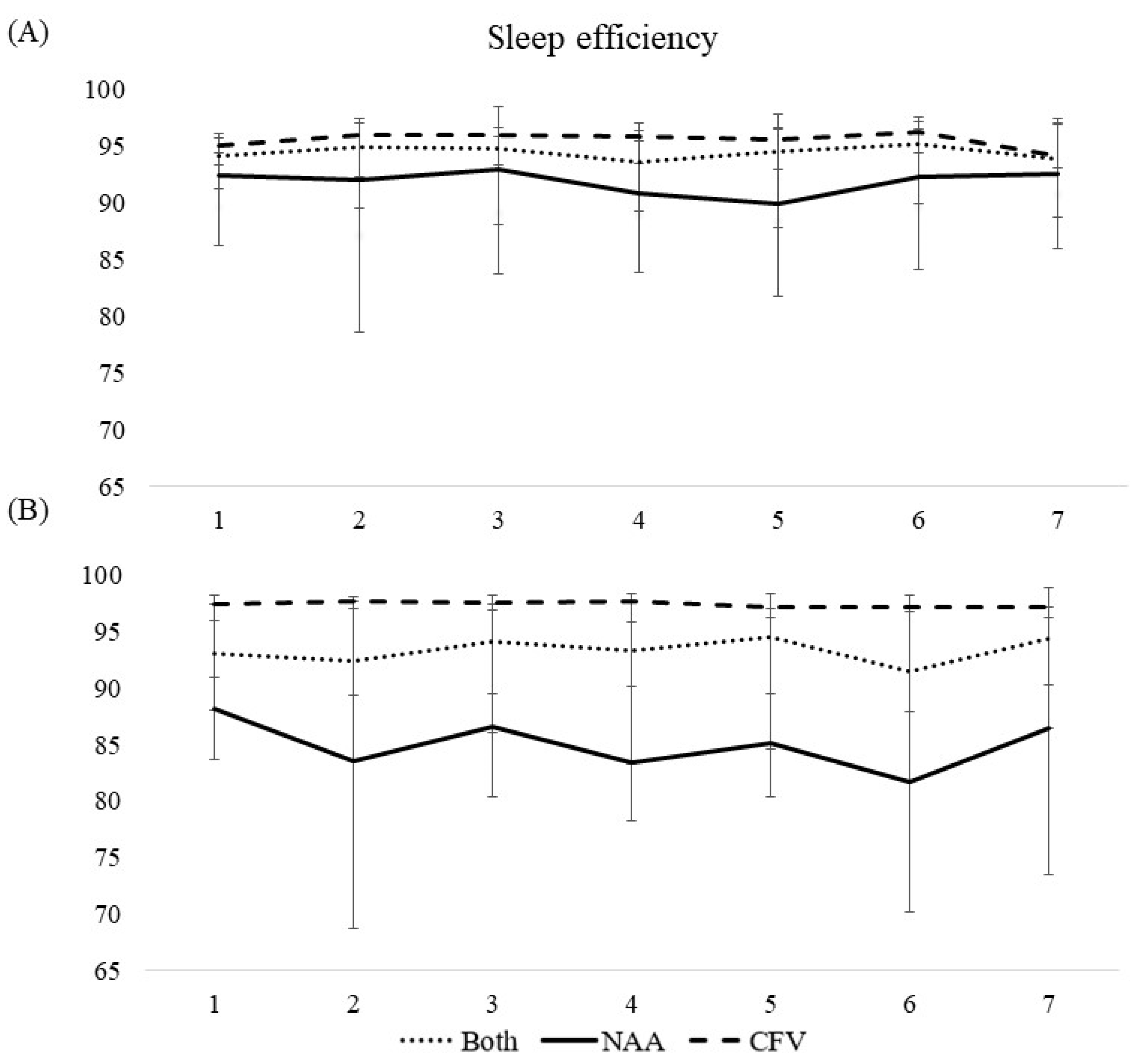
3.3.2. Wake after Sleep Onset, Time in Bed, Total Sleep Time, and Sleep Efficiency
3.4. Sleepiness Measured throughout the Workweek
Karolinska Sleepiness Scale (KSS)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- European Parliament, Council of the European Union. Directive 2003/88/EC of the European parliament and of the council of 4 November 2003 concerning certain aspects of the organisation of working time. Off. J. Eur. Union. 2003, L299, 9–11. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex%3A32003L0088 (accessed on 9 February 2021).
- Harrington, J.M. Health effects of shift work and extended hours of work. Occup. Environ. Med. 2001, 58, 68–72. [Google Scholar] [CrossRef] [Green Version]
- Fischer, D.; Lombardi, D.A.; Folkard, S.; Willetts, J.; Christiani, D.C. Updating the “Risk Index”: A systematic review and meta-analysis of occupational injuries and work schedule characteristics. Chronobiol. Int. 2017, 34, 1423–1438. [Google Scholar] [CrossRef] [PubMed]
- Kecklund, G.; Axelsson, J. Health consequences of shift work and insufficient sleep. BMJ 2016, 355, i5210. [Google Scholar] [CrossRef]
- Hankins, D.G. Air medical transport of trauma patients. Prehosp. Emerg. Care 2006, 10, 324–327. [Google Scholar] [CrossRef]
- Sollid, S.J.M.; Rehn, M. The role of the anaesthesiologist in air ambulance medicine. Curr. Opin. Anaesthesiol. 2017, 30, 513–517. [Google Scholar] [CrossRef]
- Blumen, I. UCAN Safety Committee. A Safety Review and Risk Assessment in Air Medical Transport: Supplement to the Air Medical Physician Handbook; Air Medical Physician Association: Salt Lake City, UT, USA, 2002. [Google Scholar]
- Butler, B. Helicopter emergency medical services and weather-related accidents. Air Med. J. 2014, 33, 84–85. [Google Scholar] [CrossRef]
- Radstaak, M.; Geurts, S.A.E.; Beckers, D.G.J.; Brosschot, J.F.; Kompier, M.A.J. Recovery and well-being among Helicopter Emergency Medical Service (HEMS) pilots. Appl. Ergon. 2014, 45, 986–993. [Google Scholar] [CrossRef]
- Zakariassen, E.; Waage, S.; Harris, A.; Gatterbauer-Trischler, P.; Lang, B.; Voelckel, W.; Pallesen, S.; Bjorvatn, B. Causes and management of sleepiness among pilots in a Norwegian and an Austrian air ambulance service—A comparative study. Air Med. J. 2019, 38, 25–29. [Google Scholar] [CrossRef] [Green Version]
- Sallinen, M.; Sihvola, M.; Puttonen, S.; Ketola, K.; Tuori, A.; Härmä, M.; Kecklund, G.; Åkerstedt, T. Sleep, alertness and alertness management among commercial airline pilots on short-haul and long-haul flights. Accid. Anal. Prev. 2017, 98, 320–329. [Google Scholar] [CrossRef]
- Samel, A.; Vejvoda, M.; Maass, H. Sleep deficit and stress hormones in helicopter pilots on 7-day duty for emergency medical services. Aviat. Space Environ. Med. 2004, 75, 935. [Google Scholar] [PubMed]
- Frakes, M.; Kelly, J. Sleep debt and outside employment patterns in helicopter air medical staff working 24-hour shifts. Air Med. J. 2007, 26, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Guyette, F.X.; Morley, J.L.; Weaver, M.D.; Patterson, P.D.; Hostler, D. The effect of shift length on fatigue and cognitive performance in air medical providers. Prehosp. Emerg. Care 2013, 17, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Gregory, K.B.; Winn, W.; Johnson, K.; Rosekind, M.R. Pilot fatigue survey: Exploring fatigue factors in air medical operations. Air Med. J. 2010, 29, 309–319. [Google Scholar] [CrossRef]
- Flaa, T.A.; Bjorvatn, B.; Pallesen, S.; Røislien, J.; Zakariassen, E.; Harris, A.; Waage, S. Subjective and objective sleep among air ambulance personnel. Chronobiol. Int. 2021, 38, 129–139. [Google Scholar] [CrossRef]
- Flaa, T.A.; Harris, A.; Bjorvatn, B.; Gundersen, H.; Zakariassen, E.; Pallesen, S.; Waage, S. Sleepiness among personnel in the Norwegian Air Ambulance Service. Int. Arch. Occup. Environ. Health 2019, 92, 1121–1130. [Google Scholar] [CrossRef] [Green Version]
- CamNTech Ltd. Available online: https://www.camntech.com/ (accessed on 10 December 2021).
- Chow, C.M.; Wong, S.N.; Shin, M.; Maddox, R.G.; Feilds, K.-L.; Paxton, K.; Steinbeck, K. Defining the rest interval associated with the main sleep period in actigraph scoring. Nat. Sci. Sleep 2016, 8, 321. [Google Scholar] [CrossRef] [Green Version]
- Akerstedt, T.; Gillberg, M. Subjective and objective sleepiness in the active individual. Int. J. Neurosci. 1990, 52, 29–37. [Google Scholar] [CrossRef]
- Sunde, E.; Mrdalj, J.; Pedersen, T.; Thun, E.; Bjorvatn, B.; Grønli, J.; Harris, A.; Waage, S.; Pallesen, S. Role of nocturnal light intensity on adaptation to three consecutive night shifts: A counterbalanced crossover study. Occup Env. Med 2020, 77, 249–255. [Google Scholar] [CrossRef]
- Worlddata. Sunrise and Sunset in Austria. Available online: https://www.worlddata.info/europe/austria/sunset.php (accessed on 10 December 2021).
- Worlddata. Sunrise and Sunset in Norway. Available online: https://www.worlddata.info/europe/norway/sunset.php (accessed on 10 December 2021).
- Curtis, A.F.; Miller, M.B.; Boissoneault, J.; Robinson, M.; Staud, R.; Berry, R.B.; McCrae, C.S. Discrepancies in sleep diary and actigraphy assessments in adults with fibromyalgia: Associations with opioid dose and age. J. Sleep Res. 2019, 28, e12746. [Google Scholar] [CrossRef]
- Ganesan, S.; Magee, M.; Stone, J.E.; Mulhall, M.D.; Collins, A.; Howard, M.E.; Lockley, S.W.; Rajaratnam, S.M.; Sletten, T.L. The impact of shift work on sleep, alertness and performance in healthcare workers. Sci. Rep. 2019, 9, 4635. [Google Scholar] [CrossRef] [PubMed]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Katz, E.S.; Kheirandish-Gozal, L.; et al. National Sleep Foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Health 2015, 1, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Swanson, L.M.; Arnedt, J.T.; Rosekind, M.R.; Belenky, G.; Balkin, T.J.; Drake, C. Sleep disorders and work performance: Findings from the 2008 National Sleep Foundation Sleep in America poll. J. Sleep Res. 2011, 20, 487–494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sprajcer, M.; Jay, S.M.; Vincent, G.E.; Vakulin, A.; Lack, L.; Ferguson, S.A. How the chance of missing the alarm during an on-call shift affects pre-bed anxiety, sleep and next day cognitive performance. Biol. Psychol. 2018, 137, 133–139. [Google Scholar] [CrossRef]
- Wuyts, J.; De Valck, E.; Vandekerckhove, M.; Pattyn, N.; Exadaktylos, V.; Haex, B.; Maes, J.; Verbraecken, J.; Cluydts, R. Effects of pre-sleep simulated on-call instructions on subsequent sleep. Biol. Psychol. 2012, 91, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Ziebertz, C.M.; Beckers, D.G.; Van Hooff, M.L.; Kompier, M.A.; Geurts, S.A. The effect on sleep of being on-call: An experimental field study. J. Sleep Res. 2017, 26, 809–815. [Google Scholar] [CrossRef]
- Cotrim, T.; Carvalhais, J.; Neto, C.; Teles, J.; Noriega, P.; Rebelo, F. Determinants of sleepiness at work among railway control workers. Appl. Ergon. 2017, 58, 293–300. [Google Scholar] [CrossRef]
- Mullins, H.M.; Cortina, J.M.; Drake, C.L.; Dalal, R.S. Sleepiness at work: A review and framework of how the physiology of sleepiness impacts the workplace. J. Appl. Psychol. 2014, 99, 1096. [Google Scholar] [CrossRef]
- Honn, K.A.; Satterfield, B.C.; McCauley, P.; Caldwell, J.L.; Van Dongen, H.P.A. Fatiguing effect of multiple take-offs and landings in regional airline operations. Accid. Anal. Prev. 2016, 86, 199–208. [Google Scholar] [CrossRef] [Green Version]
- Borbély, A.A.; Daan, S.; Wirz-Justice, A.; Deboer, T. The two-process model of sleep regulation: A reappraisal. J. Sleep Res. 2016, 25, 131–143. [Google Scholar] [CrossRef]
- Bendak, S.; Rashid, H.S.J. Fatigue in aviation: A systematic review of the literature. Int. J. Ind. Ergon. 2020, 76, 102928. [Google Scholar] [CrossRef]
- Matthews, K.A.; Patel, S.R.; Pantesco, E.J.; Buysse, D.J.; Kamarck, T.W.; Lee, L.; Hall, M.H. Similarities and differences in estimates of sleep duration by polysomnography, actigraphy, diary, and self-reported habitual sleep in a community sample. Sleep Health 2018, 4, 96–103. [Google Scholar] [CrossRef] [PubMed]
- Carskadon, M.A. Guidelines for the multiple sleep latency test (MSLT): A standard measure of sleepiness. Sleep 1986, 9, 519–524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stampi, C.; Stone, P.; Michimori, A. A new quantitative method for assessing sleepiness: The Alpha Attenuation Test. Work Stress 1995, 9, 368–376. [Google Scholar] [CrossRef]
- Rosekind, M.R.; Gregory, K.B.; Mallis, M.M. Alertness management in aviation operations: Enhancing performance and sleep. Aviat. Space Environ. Med. 2006, 77, 1256–1265. [Google Scholar] [PubMed]



| NAA | CFV | NAA | CFV | NAA | CFV | |||
|---|---|---|---|---|---|---|---|---|
| n (%) | Mean (SD) | Median (IQR) | Statistic | p-Value | ||||
| Years in position (n = 47) | 5 (3.5–7) | 10.5 (5–15) | −2.18 a | 0.029 b | ||||
| Caffeine intake at work (n = 45) | 4.58 (0.42) | 3.05 (0.36) | 2.73 c | 0.009 d | ||||
| 0 cups | 1 (4.0) | 3 (13.6) | ||||||
| 1–2 cups | 2 (8.0) | 3 (13.6) | ||||||
| 3–4 cups | 7 (28.0) | 11 (50.0) | ||||||
| 5–6 cups | 10 (40.0) | 4 (18.2) | ||||||
| >7 cups | 5 (20.0) | 1 (4.6) | ||||||
| Sleep need § (n = 44) | 07:01 (00:40) | 07:16 (00:38) | −1.23 c | 0.225 d | ||||
| Sleep problems related to work schedule (n = 45) | 0.231 e | |||||||
| Yes | 7 (28.0) | 11 (50.0) | ||||||
| No | 18 (72.0) | 11 (50.0) | ||||||
| Sleep Diary | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bedtime | Wake-Up Time | Wake after Sleep Onset | Time in Bed | Total Sleep Time | Sleep Efficiency | |||||||||||||
| Both | NAA | CFV | Both | NAA | CFV | Both | NAA | CFV | Both | NAA | CFV | Both | NAA | CFV | Both | NAA | CFV | |
| Day | ||||||||||||||||||
| 1 § | ||||||||||||||||||
| 2 | 0.043 | 0.115 | −0.056 | −0.021 | −0.092 | −0.008 | 0.170 | 0.365 | 0.007 | −0.086 | −0.238 | 0.054 | −0.255 | −0.707 | 0.126 | −2.18 | −6.50 | 1.31 |
| 3 | −0.267 | −0.412 | −0.149 | −0.002 | −0.077 | −0.021 | 0.065 | 0.177 | 0.001 | 0.273 | 0.322 | 0.187 | 0.215 | 0.099 | 0.201 | −0.471 | −2.65 | 0.383 |
| 4 | −0.036 | 0.087 | −0.188 | 0.218 | 0.352 | 0.049 | 0.049 | 0.134 | −0.021 | 0.288 | 0.317 | 0.255 | 0.257 | 0.122 | 0.369 | 0.109 | −2.11 | 1.93 |
| 5 | 0.196 | 0.467 | −0.118 | 0.223 | 0.328 | 0.025 | 0.024 | 0.084 | 0.010 | 0.049 | −0.101 | 0.174 | −0.032 | −0.364 | 0.196 | −1.06 | −3.42 | 0.126 |
| 6 | 0.347 | 0.464 | 0.142 | 0.451 | 0.673 | 0.168 | 0.099 | 0.238 | −0.006 | 0.113 | 0.253 | 0.027 | 0.084 | 0.032 | 0.154 | 0.261 | −2.20 | 2.06 |
| 7 | 0.524 * | 0.364 | 0.638 * | 0.644 ** | −0.519 | 1.80 *** | −0.094 | −0.154 | −0.001 | 0.232 | −0.875 * | 1.40 *** | 0.213 | −0.858 * | 1.31 *** | −0.900 | −2.55 | 0.115 |
| Actigraphy | ||||||||||||||||||
| Bedtime | Wake-up time | Wake after sleep onset | Time in bed | Total sleep time | Sleep efficiency | |||||||||||||
| Both | NAA | CFV | Both | NAA | CFV | Both | NAA | CFV | Both | NAA | CFV | Both | NAA | CFV | Both | NAA | CFV | |
| Day | ||||||||||||||||||
| 1 § | ||||||||||||||||||
| 2 | 0.287 | 0.304 | 0.288 | 0.135 | 0.246 | 0.036 | 0.211 | 0.361 | 0.075 | −0.148 | −0.032 | −0.255 | −0.249 | −0.352 | −0.183 | −1.78 | −3.94 | 0.264 |
| 3 | −0.089 | −0.429 | 0.311 | −0.110 | −0.092 | −0.098 | 0.032 | 0.080 | 0.024 | −0.010 | 0.363 | −0.409 | 0.038 | 0.276 | −0.319 | 0.485 | 0.100 | 0.331 |
| 4 | 0.084 | 0.215 | −0.050 | 0.148 | 0.435 | −0.145 | 0.132 | 0.210 | 0.034 | 0.069 | 0.244 | −0.097 | 0.007 | 0.073 | −0.034 | −0.888 | −1.84 | 0.246 |
| 5 | 0.257 | 0.583 * | −0.052 | 0.522 | 1.01 ** | 0.022 | 0.086 | 0.141 | 0.057 | 0.274 | 0.457 | 0.073 | 0.322 | 0.443 | 0.110 | 0.802 | 0.954 | 0.193 |
| 6 | 0.564 ** | 0.801 ** | 0.307 | 0.685 * | 1.36 ** | −0.001 | 0.219 | 0.397 | −0.014 | 0.132 | 0.627 | −0.314 | −0.012 | 0.281 | −0.182 | −1.30 | −2.38 | 0.467 |
| 7 | 0.555 ** | 0.098 | 1.02 *** | 0.539 * | −0.960 * | 2.05 *** | −0.020 | −0.197 | 0.142 * | −0.011 | −1.02 * | 1.03 *** | 0.051 | −0.861 * | 1.00 ** | −0.428 | −0.717 | 0.084 |
| Sleep Diary | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bedtime | Wake-Up Time | Wake after Sleep Onset | Time in Bed | Total Sleep Time | Sleep Efficiency | |||||||
| NAA | CFV | NAA | CFV | NAA | CFV | NAA | CFV | NAA | CFV | NAA | CFV | |
| Number § | −0.061 | −0.052 | −0.126 | 0.006 | 0.073 | 0.002 | −0.048 | 0.023 | −0.158 | 0.062 | −1.26 | 0.540 |
| Duration ∫ | 0.003 *** | 0.002 * | 0.003 ** | 0.001 | −0.001 * | −0.000 | −0.000 | −0.001 | 0.002 | −0.001 | 0.023 ** | −0.005 |
| Actigraphy | ||||||||||||
| Bedtime | Wake-up time | Wake after sleep onset | Time in bed | Total sleep time | Sleep efficiency | |||||||
| NAA | CFV | NAA | CFV | NAA | CFV | NAA | CFV | NAA | CFV | NAA | CFV | |
| Number § | 0.017 | −0.050 | −0.010 | −0.032 | 0.093 | −0.019 | −0.020 | 0.017 | −0.154 | 0.083 | −1.03 | 0.187 * |
| Duration ∫ | 0.002 ** | 0.002 ** | 0.002 | 0.002 * | −0.001 | −0.000 | −0.001 | −0.001 | 0.001 | −0.001 | 0.008 | −0.001 |
| Both | NAA | CFV | |
|---|---|---|---|
| Day | |||
| 1 § | |||
| 2 | −0.452 *** | −0.732 *** | −0.126 |
| 3 | −0.313 * | −0.435 | −0.177 |
| 4 | −0.374 | −0.683 * | 0.018 |
| 5 | −0.459 | −0.757 | −0.103 |
| 6 | −0.474 | −0.690 | −0.093 |
| 7 | −0.439 | −0.634 | −0.143 |
| Time | |||
| 08 § | |||
| 10 | −0.274 * | −0.662 *** | −0.213 |
| 12 | −0.369 ** | −0.943*** | −0.159 |
| 14 | −0.166 | −0.885 *** | 0.195 |
| 16 | 0.094 | −0.656 *** | 0.485 *** |
| 18 | 0.221 * | −0.399 * | 0.469 *** |
| 20 | 0.350 ** | −0.581 ** | 0.943 *** |
| 22 | 1.18 *** | 0.006 | 2.11 *** |
| 00 | 2.08 *** | 1.16 *** | 3.35 *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flaa, T.A.; Bjorvatn, B.; Pallesen, S.; Zakariassen, E.; Harris, A.; Gatterbauer-Trischler, P.; Waage, S. Sleep and Sleepiness Measured by Diaries and Actigraphy among Norwegian and Austrian Helicopter Emergency Medical Service (HEMS) Pilots. Int. J. Environ. Res. Public Health 2022, 19, 4311. https://doi.org/10.3390/ijerph19074311
Flaa TA, Bjorvatn B, Pallesen S, Zakariassen E, Harris A, Gatterbauer-Trischler P, Waage S. Sleep and Sleepiness Measured by Diaries and Actigraphy among Norwegian and Austrian Helicopter Emergency Medical Service (HEMS) Pilots. International Journal of Environmental Research and Public Health. 2022; 19(7):4311. https://doi.org/10.3390/ijerph19074311
Chicago/Turabian StyleFlaa, Tine Almenning, Bjørn Bjorvatn, Ståle Pallesen, Erik Zakariassen, Anette Harris, Pia Gatterbauer-Trischler, and Siri Waage. 2022. "Sleep and Sleepiness Measured by Diaries and Actigraphy among Norwegian and Austrian Helicopter Emergency Medical Service (HEMS) Pilots" International Journal of Environmental Research and Public Health 19, no. 7: 4311. https://doi.org/10.3390/ijerph19074311
APA StyleFlaa, T. A., Bjorvatn, B., Pallesen, S., Zakariassen, E., Harris, A., Gatterbauer-Trischler, P., & Waage, S. (2022). Sleep and Sleepiness Measured by Diaries and Actigraphy among Norwegian and Austrian Helicopter Emergency Medical Service (HEMS) Pilots. International Journal of Environmental Research and Public Health, 19(7), 4311. https://doi.org/10.3390/ijerph19074311






