Association between Wood and Other Biomass Fuels and Risk of Low Birthweight in Uganda: A Cross-Sectional Analysis of 2016 Uganda Demographic and Health Survey Data
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Setting, and Data Source
2.2. Study Population
2.3. Modifications to the Wealth Index
2.4. Exposure Variables
2.5. Outcome Variables
2.6. Covariates
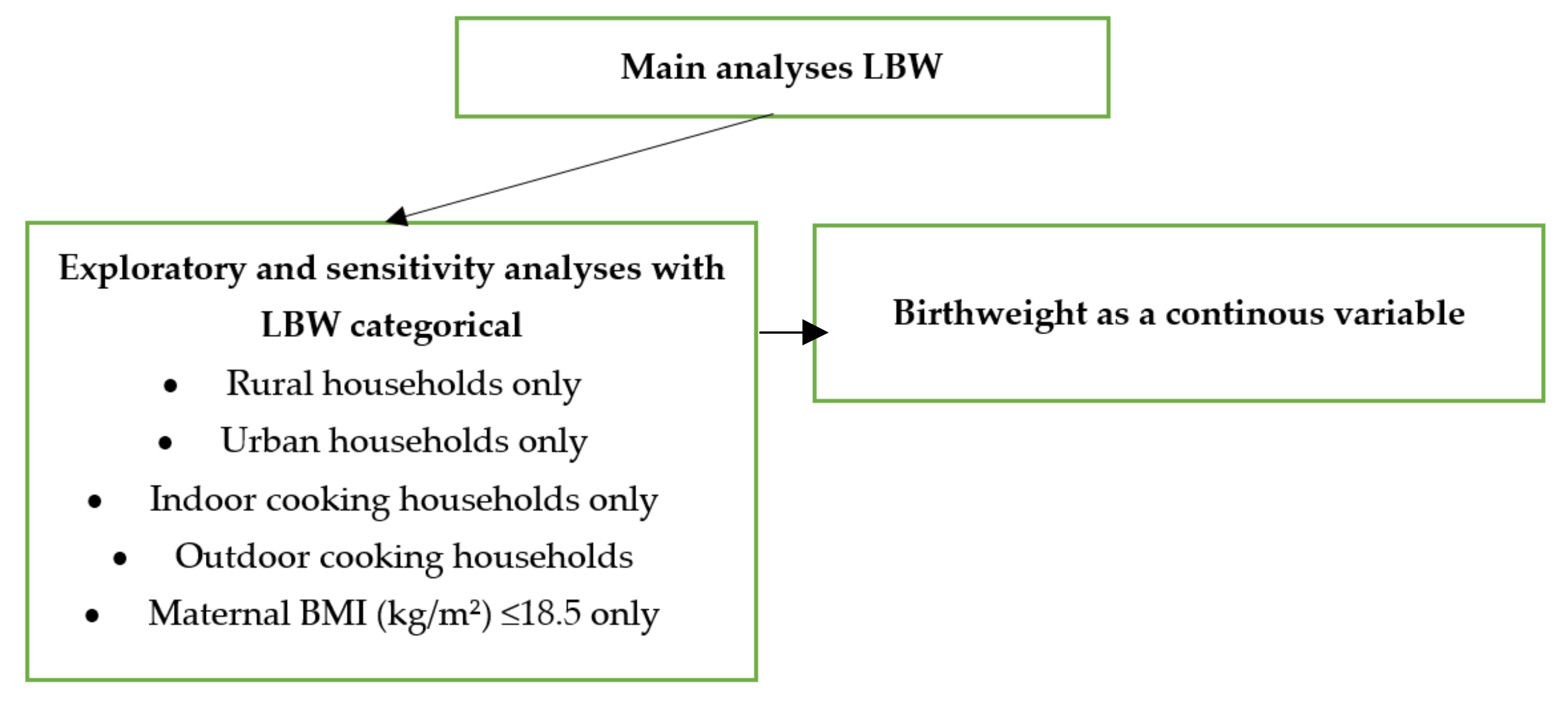
2.7. Data Analysis
2.8. Ethical Approval and Authorisation
3. Results
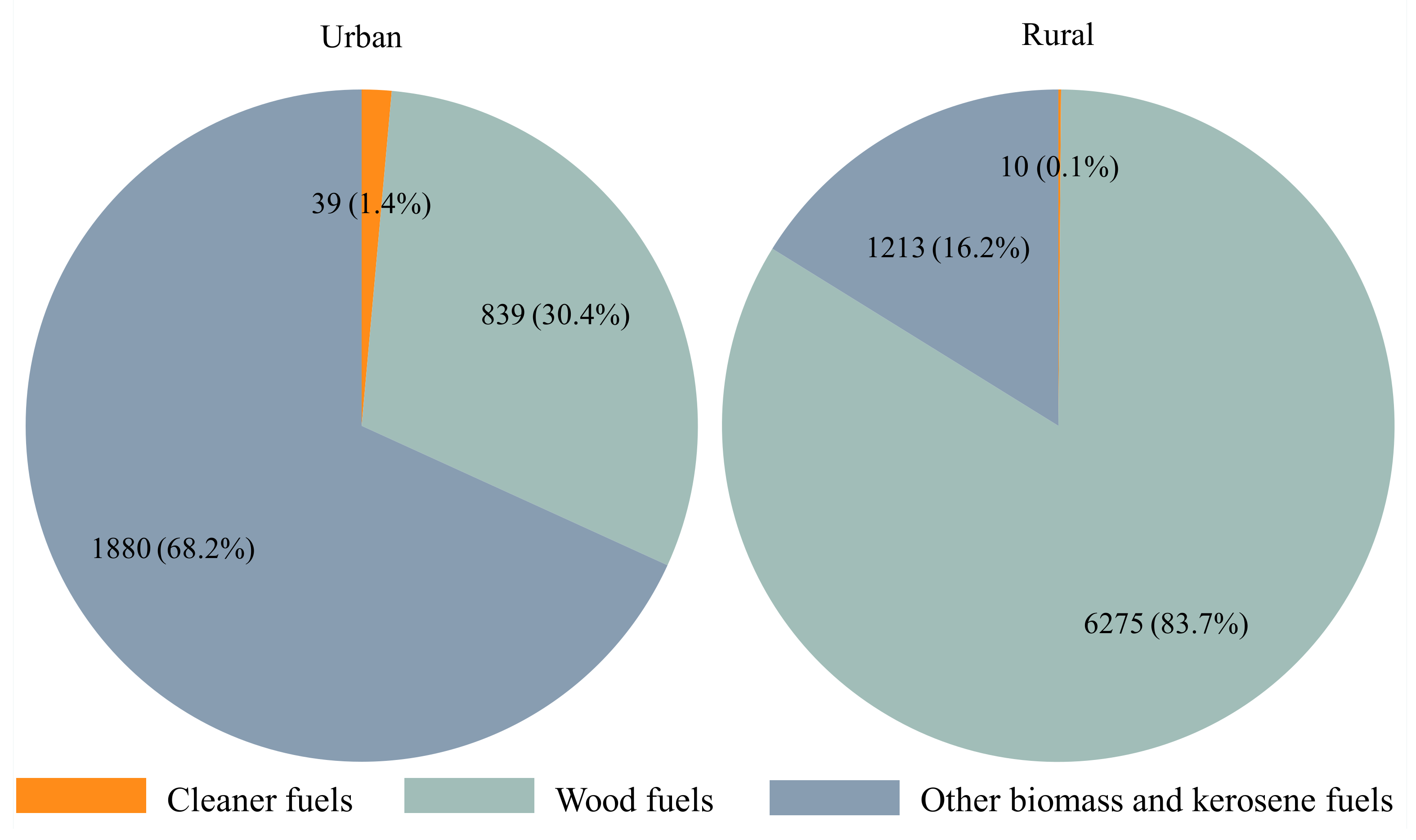
3.1. Descriptive Statistics
3.2. Association between Type of Biomass Cooking Fuels with LBW
3.3. Sensitivity Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stoner, O.; Lewis, J.; Martínez, I.L.; Gumy, S.; Economou, T.; Adair-Rohani, H. Household cooking fuel estimates at global and country level for 1990 to 2030. Nat. Commun. 2021, 12, 5793. [Google Scholar] [CrossRef] [PubMed]
- WHO. Particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. In WHO Global Air Quality Guidelines; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Smith, K.R.; Bruce, N.; Balakrishnan, K.; Adair-Rohani, H.; Balmes, J.; Chafe, Z.; Dherani, M.; Hosgood, H.D.; Mehta, S.; Pope, D. Millions dead: How do we know and what does it mean? Methods used in the comparative risk assessment of household air pollution. Annu. Rev. Public Health 2014, 35, 185–206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, K.K.; Bing, R.; Kiang, J.; Bashir, S.; Spath, N.; Stelzle, D.; Mortimer, K.; Bularga, A.; Doudesis, D.; Joshi, S.S. Adverse health effects associated with household air pollution: A systematic review, meta-analysis, and burden estimation study. Lancet Glob. Health 2020, 8, e1427–e1434. [Google Scholar] [CrossRef]
- Avis, W.M.S.; Singh, A. Air Pollution Exposure in Low Income Households in Kampala. ASAP East Africa Vulnerability Scoping Study No. 6. University of Birmingham: Birmingham, UK, 2018. Available online: https://assets.publishing.service.gov.uk (accessed on 11 February 2022).
- Okello, G.; Devereux, G.; Semple, S. Women and girls in resource poor countries experience much greater exposure to household air pollutants than men: Results from Uganda and Ethiopia. Environ. Int. 2018, 119, 429–437. [Google Scholar] [CrossRef] [PubMed]
- Amegah, A.K.; Quansah, R.; Jaakkola, J.J. Household air pollution from solid fuel use and risk of adverse pregnancy outcomes: A systematic review and meta-analysis of the empirical evidence. PLoS ONE 2014, 9, e113920. [Google Scholar] [CrossRef]
- Younger, A.; Alkon, A.; Harknett, K.; Louis, R.J.; Thompson, L.M. Adverse birth outcomes associated with household air pollution from unclean cooking fuels in low-and middle-income countries: A systematic review. Environ. Res. 2021, 204, 112274. [Google Scholar] [CrossRef] [PubMed]
- Oza, S.; Lawn, J.E.; Hogan, D.R.; Mathers, C.; Cousens, S.N. Neonatal cause-of-death estimates for the early and late neonatal periods for 194 countries: 2000–2013. Bull. World Health Organ. 2014, 93, 19–28. [Google Scholar] [CrossRef]
- Blencowe, H.; Krasevec, J.; De Onis, M.; Black, R.E.; An, X.; Stevens, G.A.; Borghi, E.; Hayashi, C.; Estevez, D.; Cegolon, L. National, regional, and worldwide estimates of low birthweight in 2015, with trends from 2000: A systematic analysis. Lancet Glob. Health 2019, 7, e849–e860. [Google Scholar] [CrossRef] [Green Version]
- Misra, P.; Srivastava, R.; Krishnan, A.; Sreenivaas, V.; Pandav, C.S. Indoor air pollution-related acute lower respiratory infections and low birthweight: A systematic review. J. Trop. Pediatrics 2012, 58, 457–466. [Google Scholar] [CrossRef] [Green Version]
- Pope, D.P.; Mishra, V.; Thompson, L.; Siddiqui, A.R.; Rehfuess, E.A.; Weber, M.; Bruce, N.G. Risk of low birth weight and stillbirth associated with indoor air pollution from solid fuel use in developing countries. Epidemiol. Rev. Environ. Health Perspect. 2010, 32, 70–81. [Google Scholar] [CrossRef] [Green Version]
- Amegah, A.K.; Jaakkola, J.J.; Quansah, R.; Norgbe, G.K.; Dzodzomenyo, M. Cooking fuel choices and garbage burning practices as determinants of birth weight: A cross-sectional study in Accra, Ghana. J. Environ. Health 2012, 11, 78. [Google Scholar] [CrossRef] [Green Version]
- Adeyemi, R.A.; Zewotir, T.; Ramroop, S. Semiparametric multinomial ordinal model to analyze spatial patterns of child birth weight in Nigeria. Int. J. Environ. Res. Public Health 2016, 13, 1145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alexander, D.A.; Northcross, A.; Karrison, T.; Morhasson-Bello, O.; Wilson, N.; Atalabi, O.M.; Dutta, A.; Adu, D.; Ibigbami, T.; Olamijulo, J. Pregnancy outcomes and ethanol cook stove intervention: A randomized-controlled trial in Ibadan, Nigeria. Environ. Int. 2018, 111, 152–163. [Google Scholar] [CrossRef]
- Arinola, G.O.; Dutta, A.; Oluwole, O.; Olopade, C.O. Household air pollution, levels of micronutrients and heavy metals in cord and maternal blood, and pregnancy outcomes. Int. J. Environ. Res. Public Health Engl. 2018, 15, 2891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roberman, J.; Emeto, T.I.; Adegboye, O.A. Adverse birth outcomes due to exposure to household air pollution from unclean cooking fuel among women of reproductive age in Nigeria. Int. J. Environ. Res. Public Health 2021, 18, 634. [Google Scholar] [CrossRef] [PubMed]
- Milanzi, E.B.; Namacha, N.M. Maternal biomass smoke exposure and birth weight in Malawi: Analysis of data from the 2010 Malawi Demographic and Health Survey. Malawi Med. J. 2017, 29, 160–165. [Google Scholar] [CrossRef] [Green Version]
- Admasie, A.; Kumie, A.; Worku, A. Association of household fuel type, kitchen characteristics and house structure with child size at birth in Wolaita Sodo, Southern Ethiopia. Open Public Health J. 2018, 11, 298–308. [Google Scholar] [CrossRef]
- Kanno, G.G.; Anbesse, A.T.; Shaka, M.F.; Legesse, M.T.; Andarge, S.D. Investigating the effect of biomass fuel use and kitchen location on maternal report of birth size: A Cross-Sectional Analysis of 2016 Ethiopian Demographic Health Survey data. Public Health Pract. 2021, 2, 100211. [Google Scholar] [CrossRef]
- Demelash, H.; Motbainor, A.; Nigatu, D.; Gashaw, K.; Melese, A. Risk factors for low birth weight in Bale zone hospitals, South-East Ethiopia: A case–control study. BMC Pregnancy Childbirth 2015, 15, 264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mishra, V.; Dai, X.; Smith, K.R.; Mika, L. Maternal exposure to biomass smoke and reduced birth weight in Zimbabwe. Ann. Epidemiol. 2004, 14, 740–747. [Google Scholar] [CrossRef]
- Weber, E.; Adu-Bonsaffoh, K.; Vermeulen, R.; Klipstein-Grobusch, K.; Grobbee, D.E.; Browne, J.L.; Downward, G.S. Household fuel use and adverse pregnancy outcomes in a Ghanaian cohort study. J. Reprod. Health 2020, 17, 29. [Google Scholar] [CrossRef] [PubMed]
- Woolley, K.E.; Bagambe, T.; Singh, A.; Avis, W.R.; Kabera, T.; Weldetinsae, A.; Mariga, S.T.; Kirenga, B.; Pope, F.D.; Thomas, G.N. Investigating the association between wood and charcoal domestic cooking, respiratory symptoms and acute respiratory infections among children aged under 5 Years in Uganda: A Cross-sectional analysis of the 2016 Demographic and Health Survey. Int. J. Environ. Res. Public Health 2020, 17, 3974. [Google Scholar] [CrossRef]
- Coker, E.; Katamba, A.; Kizito, S.; Eskenazi, B.; Davis, J.L. Household air pollution profiles associated with persistent childhood cough in urban Uganda. Environ. Int. 2020, 136, 105471. [Google Scholar] [CrossRef] [PubMed]
- Van Gemert, F.; Chavannes, N.; Nabadda, N.; Luzige, S.; Kirenga, B.; Eggermont, C.; de Jong, C.; van der Molen, T. Impact of chronic respiratory symptoms in a rural area of sub-Saharan Africa: An in-depth qualitative study in the Masindi district of Uganda. Prim. Care Respir. J. 2013, 22, 300–305. [Google Scholar] [CrossRef] [PubMed]
- The World Bank Group. Uganda | Data. Available online: https://data.worldbank.org/country/uganda (accessed on 8 March 2021).
- Uganda Bureau of Statistics (UBOS); ICF. Uganda Demographic and Health Survey 2016; UBOS: Kampala, Uganda; ICF: Rockville, MD, USA, 2018.
- Uganda Human Development Reports. Available online: http://hdr.undp.org/sites/all/themes/hdr_theme/country-notes/UGA.pdf (accessed on 1 September 2021).
- Ministry of Energy and Mineral Development. The Renewable Energy Policy for Uganda. 2007. Available online: https://www.era.go.ug/index.php/download-repo/doc_details/209-era-ceo-s-keynote-speech-at-the-era-getfit-uganda-solar-pv-award-event?tmpl=component (accessed on 1 September 2021).
- Vohr, B.R.; Tyson, J.E.; Wright, L.L.; Perritt, R.L.; Li, L.; Poole, W.K.; Network, N.N.R. Maternal age, multiple birth, and extremely low birth weight infants. J. Pediatrics 2009, 154, 498–503.e492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rutstein, S.O.; Johnson, K. The DHS Wealth Index; DHS Comparative Reports No. 6.; ORC Macro: Calverton, MD, USA, 2004. [Google Scholar]
- Rutstein, S.O. Steps to Constructing the New DHS Wealth Index; ICF International: Rockville, MA, USA, 2015. [Google Scholar]
- Corp, I.S. IBM SPSS Statistics for Windows. Version 27.0; IBM: Armonk, NY, USA, 2020. [Google Scholar]
- Tusting, L.S.; Bottomley, C.; Gibson, H.; Kleinschmidt, I.; Tatem, A.J.; Lindsay, S.W.; Gething, P.W. Housing improvements and malaria risk in sub-Saharan Africa: A multi-country analysis of survey data. PLoS Med. 2017, 14, e1002234. [Google Scholar] [CrossRef] [Green Version]
- Manyeh, A.K.; Kukula, V.; Odonkor, G.; Ekey, R.A.; Adjei, A.; Narh-Bana, S.; Akpakli, D.E.; Gyapongi, M. Socioeconomic and demographic determinants of birth weight in southern rural Ghana: Evidence from Dodowa Health and Demographic Surveillance System. BMC Pregnancy Childbirth 2016, 16, 160. [Google Scholar] [CrossRef] [Green Version]
- Dahlui, M.; Azahar, N.; Oche, O.M.; Aziz, N.A. Risk factors for low birth weight in Nigeria: Evidence from the 2013 Nigeria Demographic and Health Survey. Glob. Health Action 2016, 9, 28822. [Google Scholar] [CrossRef]
- Ahammed, B.; Maniruzzaman, M.; Ferdausi, F.; Abedin, M.M.; Hossain, M.T. Socioeconomic and demographic factors associated with low birth weight in Nepal: Data from 2016 Nepal demographic and health survey. Soc. Health Behav. 2020, 3, 158. [Google Scholar] [CrossRef]
- Poverty Maps of Uganda-Uganda Bureau of Statistics. Available online: https://www.ubos.org/wp-content/uploads/publications/02_2020Poverty_Map_report__Oct_2019.pdf (accessed on 1 September 2021).
- World Health Organization. Report of a WHO Technical Consultation on Birth Spacing: Geneva, Switzerland 13–15 June 2005; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- World Health Organization. Global Nutrition Targets 2025: Low Birth Weight Policy Brief; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Mahumud, R.A.; Sultana, M.; Sarker, A.R. Distribution and determinants of low birth weight in developing countries. J. Prev. Med. Public Health 2017, 50, 18. [Google Scholar] [CrossRef] [Green Version]
- McDonald, S.D.; Han, Z.; Mulla, S.; Beyene, J. Overweight and obesity in mothers and risk of preterm birth and low birth weight infants: Systematic review and meta-analyses. BMJ 2010, 341, c3428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- StataCorp. Stata Statistical Software: Release 16; StataCorp LLC.: College Station, TX, USA, 2019. [Google Scholar]
- The Demographic and Health Survey Program (DHS) The DHS Program US-AID. Available online: https://dhsprogram.com/ (accessed on 20 December 2021).
- Khan, M.N.; Islam, M.M.; Islam, M.R.; Rahman, M.M. Household air pollution from cooking and risk of adverse health and birth outcomes in Bangladesh: A nationwide population-based study. Environ. Health Perspect. 2017, 16, 57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sreeramareddy, C.T.; Shidhaye, R.R.; Sathiakumar, N. Association between biomass fuel use and maternal report of child size at birth-an analysis of 2005–06 India Demographic Health Survey data. BMC Public Health 2011, 11, 403. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Odo, D.B.; Yang, I.A.; Knibbs, L.D. A systematic review and appraisal of epidemiological studies on household fuel use and its health effects using demographic and health surveys. Int. J. Environ. Res. Public Health 2021, 18, 1411. [Google Scholar] [CrossRef] [PubMed]
- Fullerton, D.G.; Bruce, N.; Gordon, S.B. Indoor air pollution from biomass fuel smoke is a major health concern in the developing world. Trans. R. Soc. Trop. Med. Hyg. 2008, 102, 843–851. [Google Scholar] [CrossRef] [Green Version]
- Boy, E.; Bruce, N.; Delgado, H. Birth weight and exposure to kitchen wood smoke during pregnancy in rural Guatemala. Environ. Health Perspect. 2002, 110, 109–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amegah, A.K.; Jaakkola, J.J. Household air pollution and the sustainable development goals. Bull. World Health Organ. 2016, 94, 215. [Google Scholar] [CrossRef] [PubMed]
- Woolley, K.E.; Dickinson-Craig, E.; Bartington, S.E.; Oludotun, T.; Kirenga, B.; Mariga, S.T.; Kabera, T.; Coombe, A.; Pope, F.D.; Singh, A. Effectiveness of interventions to reduce household air pollution from solid biomass fuels and improve maternal and child health outcomes in low-and middle-income countries: A systematic review protocol. Syst. Rev. 2021, 10, 73–90. [Google Scholar] [CrossRef]
- Barnes, B.R. Behavioural change, indoor air pollution and child respiratory health in developing countries: A review. Int. J. Environ. Res. Public Health Engl. 2014, 11, 4607–4618. [Google Scholar] [CrossRef] [Green Version]
- Rosenthal, J.; Quinn, A.; Grieshop, A.P.; Pillarisetti, A.; Glass, R.I. Clean cooking and the SDGs: Integrated analytical approaches to guide energy interventions for health and environment goals. J. Energy Sustain. Dev. 2018, 42, 152–159. [Google Scholar] [CrossRef]
- Woolley, K.E.; Dickinson-Craig, E.; Lawson, H.L.; Sheikh, J.; Day, R.; Pope, F.D.; Greenfield, S.M.; Bartington, S.E.; Warburton, D.; Manaseki-Holland, S. Effectiveness of interventions to reduce household air pollution from solid biomass fuels and improve maternal and child health outcomes in low-and middle-income countries: A systematic review and meta-analysis. Indoor Air 2022, 32, e12958. [Google Scholar] [PubMed]
- Vakalopoulos, A.; Dharmage, S.C.; Dharmaratne, S.; Jayasinghe, P.; Lall, O.; Ambrose, I.; Weerasooriya, R.; Bui, D.S.; Yasaratne, D.; Heyworth, J. Household air pollution from biomass fuel for cooking and adverse fetal growth outcomes in rural Sri Lanka. Int. J. Environ. Res. Public Health 2021, 18, 1878. [Google Scholar] [CrossRef] [PubMed]
| Birthweight < 2500 g N (%) | Birthweight ≥ 2500 g N (%) | ||
|---|---|---|---|
| N = 986 | N = 9281 | p-Value | |
| Cooking fuel | 0.062 | ||
| Wood | 720 (73.3) | 6393 (69.3) | |
| Other polluting fuels | 262 (26.7) | 2831 (30.7) | |
| Missing (%) | 4 (0.4) | 56 (0.6) | |
| Cooking location | 0.942 | ||
| In the house | 100 (10.2) | 967 (10.4) | |
| In a separate building | 622 (63.1) | 5774 (62.3) | |
| Outdoors | 264 (26.8) | 2521 (27.2) | |
| Missing (%) | 264 (26.8) | 0 (0.0) | |
| Household smoking | 0.863 | ||
| Yes | 862 (87.5) | 8137 (87.7) | |
| No | 124 (12.5) | 1144 (12.3) | |
| Type of place of residence | 0.293 | ||
| Urban | 247 (25.0) | 2522 (27.2) | |
| Rural | 739 (75.0) | 6759 (72.8) | |
| Region | 0.096 | ||
| Central | 277 (28.1) | 2719 (29.3) | |
| East | 250 (25.3) | 2354 (25.4) | |
| North | 259 (26.3) | 2071 (22.3) | |
| West | 200 (20.3) | 2137 (23.0) | |
| Electricity | 0.011 | ||
| Yes | 700 (74.3) | 6169 (69.0) | |
| No | 243 (25.7) | 2772 (31.0) | |
| Missing (%) | 43 (4.4) | 339 (3.7) | |
| Number of household members (listed) | 0.568 | ||
| Median (IQR) | 6.0 (4.0, 8.0) | 5.0 (4.0, 7.0) | |
| Combined wealth index | 0.003 | ||
| Low | 248 (25.1) | 1851 (19.9) | |
| Second | 193 (19.6) | 1662 (17.9) | |
| Middle | 182 (18.4) | 1632 (17.6) | |
| Fourth | 158 (16.1) | 1804 (19.4) | |
| Highest | 205 (20.8) | 2332 (25.1) | |
| Maternal characteristics | |||
| Respondent’s current age | <0.001 | ||
| Median (IQR) | 26.0 (22.0, 32.0) | 27.0 (23.0, 32.0) | |
| Mother’s education | 0.010 | ||
| No education/Primary | 697 (70.7) | 6072 (65.4) | |
| Secondary/higher | 289 (29.3) | 3208 (34.6) | |
| Mother’s BMI (kg/m2) | 0.223 | ||
| <18.5 | 19 (6.2) | 253 (8.3) | |
| ≥18.5 | 296 (93.8) | 2795 (91.7) | |
| Missing (%) | 670 (68.0) | 6233 (67.2) | |
| Variable | Birthweight < 2500 g N (%) | Birthweight ≥ 2500 g N (%) | |
|---|---|---|---|
| N = 986 | N = 9281 | p-Value | |
| Parity | 0.327 | ||
| Once | 170 (17.2) | 1466 (15.8) | |
| More than once | 816 (82.8) | 7814 (84.2) | |
| Birth order number | |||
| Median (IQR) | 2.0 (1.0, 5.0) | 3.0 (2.0, 5.0) | |
| Sex of child | <0.001 | ||
| Male | 438 (44.4) | 4761 (51.3) | |
| Female | 548 (55.6) | 4520 (48.7) | |
| Birth Interval | 0.576 | ||
| ≤24 months | 824 (83.5) | 7681 (82.8) | |
| >24 months | 162 (16.5) | 1599 (17.2) | |
| Duration of pregnancy | <0.001 | ||
| Pre-term | 274 (27.8) | 1184 (12.8) | |
| Term | 711 (72.2) | 8097 (87.2) | |
| Timing of first ANC visits | 0.066 | ||
| <5 months gestation | 387 (65.1) | 3896 (60.8) | |
| ≥5 months gestation | 207 (34.9) | 2509 (39.2) | |
| Missing (%) | 391 (39.7) | 2875 (31.0) | |
| Number of ANC visits | 0.003 | ||
| <4 | 252 (41.4) | 2206 (34.3) | |
| ≥4 | 357 (58.6) | 4225 (65.7) | |
| Missing (%) | 377 (38.3) | 2849 (30.7) | |
| Place of delivery | 0.131 | ||
| Health facility | 906 (92.5) | 8655 (93.9) | |
| Home | 73 (7.5) | 561 (6.1) | |
| Missing (%) | 7 (0.7) | 64 (0.7) | |
| Delivery by caesarean section | 0.763 | ||
| No | 895 (91.4) | 8479 (91.8) | |
| Yes | 84 (8.6) | 760 (8.2) | |
| Missing (%) | 7 (0.7) | 42 (0.4) | |
| Iron supplementation | 0.131 | ||
| No | 66 (10.8) | 562 (8.7) | |
| Yes | 545 (89.2) | 5906 (91.3) | |
| Missing (%) | 375 (38.0) | 2812 (30.3) | |
| Sulphadoxine-pyrimethamine | 0.014 | ||
| Yes | 467 (76.8) | 5251 (81.4) | |
| No | 141 (23.2) | 1199 (18.6) | |
| Missing (%) | 378 (38.4) | 2831 (30.5) | |
| Deworming | 0.021 | ||
| Yes | 364 (59.7) | 4179 (65.2) | |
| No | 246 (40.3) | 2226 (34.8) | |
| Missing (%) | 376 (38.1) | 2876 (31.0) | |
| Unadjusted Analysis | Adjusted Analysis (N = 9863) | |||||
|---|---|---|---|---|---|---|
| UOR | 95% CI | p-Value | AOR | 95% CI | p-Value | |
| Household Characteristics | ||||||
| Cooking fuel | ||||||
| Wood | Ref. | Ref. | ||||
| Other polluting fuels | 0.82 | (0.67, 1.00) | 0.053 | 0.94 | (0.72, 1.22) | 0.646 |
| Cooking location | ||||||
| In the house | Ref. | Ref. | ||||
| In a separate building | 1.04 | (0.75, 1.43) | 0.818 | 0.99 | (0.71, 1.36) | 0.928 |
| Outdoors | 1.01 | (0.71, 1.43) | 0.959 | 0.94 | (0.67, 1.30) | 0.691 |
| Household smoking | ||||||
| Yes | Ref. | Ref. | ||||
| No | 1.02 | (0.82, 1.27) | 0.863 | 0.92 | (0.73, 1.15) | 0.470 |
| Type of place of residence | ||||||
| Urban | Ref. | |||||
| Rural | 1.12 | (0.91, 1.37) | 0.294 | 0.90 | (0.70, 1.15) | 0.400 |
| Region | ||||||
| Central | Ref. | Ref. | ||||
| East | 1.04 | (0.83, 1.30) | 0.726 | 0.76 | (0.59, 0.98) | 0.035 |
| North | 1.23 | (0.98, 1.54) | 0.076 | 0.75 | (0.57, 0.99) | 0.042 |
| West | 0.92 | (0.71, 1.19) | 0.525 | 0.82 | (0.62, 1.06) | 0.134 |
| Electricity | ||||||
| Yes | Ref. | Ref. | ||||
| No | 1.30 | (1.06, 1.58) | 0.011 | 0.94 | (0.73, 1.22) | 0.655 |
| Number of household members (listed) | ||||||
| 1.01 | (0.99, 1.04) | 0.418 | 1.03 | (1.00, 1.07) | 0.027 | |
| Combined wealth index | ||||||
| Low | Ref. | Ref. | ||||
| Second | 0.87 | (0.70, 1.08) | 0.214 | 0.92 | (0.71, 1.18) | 0.500 |
| Middle | 0.83 | (0.66, 1.04) | 0.108 | 0.89 | (0.67, 1.19) | 0.435 |
| Fourth | 0.66 | (0.51, 0.84) | 0.001 | 0.69 | (0.50, 0.96) | 0.027 |
| Highest | 0.66 | (0.50, 0.85) | 0.002 | 0.73 | (0.50, 1.08) | 0.120 |
| Maternal characteristics | ||||||
| Respondent’s current age | ||||||
| 0.98 | (0.97, 0.99) | 0.001 | 0.99 | (0.97, 1.01) | 0.403 | |
| Mother’s education | ||||||
| No education/Primary only | Ref. | Ref. | ||||
| Secondary only/higher | 0.78 | (0.65, 0.94) | 0.010 | 0.80 | (0.64, 1.00) | 0.050 |
| Mother’s BMI (Kg/m2) | ||||||
| <18.5 | Ref. | |||||
| ≥18.5 | 1.37 | (0.82, 2.29) | 0.225 | |||
| Birth characteristics | ||||||
| Parity | ||||||
| Once | Ref. | Ref. | ||||
| More than once | 0.90 | (0.73, 1.11) | 0.327 | 1.18 | (0.89, 1.55) | 0.249 |
| Birth order number | ||||||
| 0.95 | (0.92, 0.99) | 0.008 | 0.96 | (0.90, 1.02) | 0.164 | |
| Sex of child | ||||||
| Male | Ref. | Ref. | ||||
| Female | 1.32 | (1.13, 1.53) | <0.001 | 1.32 | (1.13, 1.55) | 0.001 |
| Birth Interval | ||||||
| ≤24 months | Ref. | Ref. | ||||
| >24 months | 0.95 | (0.78, 1.15) | 0.576 | 0.95 | (0.77, 1.16) | 0.597 |
| Duration of pregnancy | ||||||
| Pre-term | Ref. | Ref. | ||||
| term | 0.38 | (0.31, 0.46) | <0.001 | 0.39 | (0.31, 0.49) | <0.001 |
| Timing of first ANC visits | ||||||
| <5 months gestation | Ref. | |||||
| ≥5 months gestation | 0.83 | (0.68, 1.01) | 0.066 | |||
| Number of ANC visits | ||||||
| <4 times | Ref. | |||||
| ≥4 times | 0.74 | (0.61, 0.90) | 0.003 | |||
| Place of delivery | ||||||
| Health facility | Ref. | Ref. | ||||
| Home | 1.25 | (0.94, 1.67) | 0.131 | 1.21 | (0.90, 1.62) | 0.211 |
| Delivery by caesarean section | ||||||
| No | Ref. | Ref. | ||||
| Yes | 1.05 | (0.78, 1.41) | 0.763 | 1.16 | (0.87, 1.56) | 0.313 |
| Iron supplementation | ||||||
| No | Ref. | |||||
| Yes | 0.78 | (0.57, 1.08) | 0.132 | |||
| Sulphadoxine-pyrimethamine | ||||||
| Yes | Ref. | |||||
| No | 1.32 | (1.06, 1.65) | 0.014 | |||
| Deworming | ||||||
| Yes | Ref. | |||||
| No | 1.27 | (1.04, 1.55) | 0.021 | |||
| AOR | 95% CI | p-Value | |
|---|---|---|---|
| Place of residence | |||
| Urban (N = 2274) | 1.09 | (0.65, 1.83) | 0.745 |
| Rural (N = 7589) | 0.85 | (0.61, 1.18) | 0.322 |
| Cooking location | |||
| Indoor (N = 7190) | 1.04 | (0.77, 1.42) | 0.786 |
| Outdoor (N = 2682) | 0.77 | (0.49, 1.19) | 0.235 |
| Adjusting for normal maternal BMI | |||
| BMI ≤ 18 (N = 2655) | 0.92 | (0.59, 1.44) | 0.726 |
| Adjusting for all confounders | |||
| N = 2167 | 0.78 | (0.46, 1.31) | 0.348 |
| Birthweight as a continuous variable | |||
| N = 9863 | 29.43 | (−38.15, 97.01) | 0.393 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Epuitai, J.; Woolley, K.E.; Bartington, S.E.; Thomas, G.N. Association between Wood and Other Biomass Fuels and Risk of Low Birthweight in Uganda: A Cross-Sectional Analysis of 2016 Uganda Demographic and Health Survey Data. Int. J. Environ. Res. Public Health 2022, 19, 4377. https://doi.org/10.3390/ijerph19074377
Epuitai J, Woolley KE, Bartington SE, Thomas GN. Association between Wood and Other Biomass Fuels and Risk of Low Birthweight in Uganda: A Cross-Sectional Analysis of 2016 Uganda Demographic and Health Survey Data. International Journal of Environmental Research and Public Health. 2022; 19(7):4377. https://doi.org/10.3390/ijerph19074377
Chicago/Turabian StyleEpuitai, Joshua, Katherine E. Woolley, Suzanne E. Bartington, and G. Neil Thomas. 2022. "Association between Wood and Other Biomass Fuels and Risk of Low Birthweight in Uganda: A Cross-Sectional Analysis of 2016 Uganda Demographic and Health Survey Data" International Journal of Environmental Research and Public Health 19, no. 7: 4377. https://doi.org/10.3390/ijerph19074377







