The State of the Evidence about the Family and Community Nurse: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Literature Search Strategy
2.3. Quality Appraisal
2.4. Data Abstraction, Analysis, and Synthesis
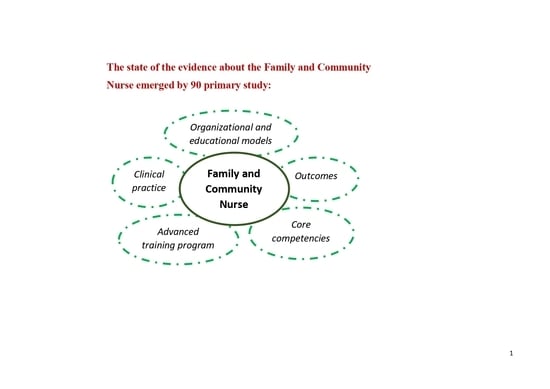
3. Results
- (a)
- Clinical practice
- (b)
- Core competencies
- (c)
- Outcomes
- (d)
- Organisational and educational models
- (e)
- Advanced training program
4. Discussion
4.1. Strengths, Limits, and Further Challenges
4.2. Implications for Clinical Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bloom, D.E.; Luca, D.L. The Global Demography of Aging: Facts, Explanations, Future-Chapter 1. In Handbook of the Economics of Population Aging; Piggott, J., Woodland, A., Eds.; North-Holland: Bonn, Germany, 2016; Volume 1, pp. 3–56. ISBN 978-0-444-53842-0. [Google Scholar]
- Beard, J.R.; Officer, A.; de Carvalho, I.A.; Sadana, R.; Pot, A.M.; Michel, J.-P.; Lloyd-Sherlock, P.; Epping-Jordan, J.E.; Peeters, G.M.E.E.G.; Mahanani, W.R.; et al. The World report on ageing and health: A policy framework for healthy ageing. Lancet 2016, 387, 2145–2154. [Google Scholar] [CrossRef]
- Istituto Nazionale di Statistica (ISTAT). Indicatori Demografici. Anno 2020. Available online: https://www.istat.it/it/files/2021/05/REPORT_INDICATORI-DEMOGRAFICI-2020.pdf (accessed on 22 June 2021).
- Cockerham, W.C.; Hamby, B.W.; Oates, G.R. The Social Determinants of Chronic Disease. Am. J. Prev. Med. 2017, 52, S5–S12. [Google Scholar] [CrossRef] [PubMed]
- Hajat, C.; Stein, E. The global burden of multiple chronic conditions: A narrative review. Prev. Med. Rep. 2018, 12, 284–293. [Google Scholar] [CrossRef] [PubMed]
- Black, D.; O’Loughlin, K.; Kendig, H.; Wilson, L. Cities, environmental stressors, ageing and chronic disease. Australas. J. Ageing 2012, 31, 147–151. [Google Scholar] [CrossRef]
- Graffigna, G.; Barello, S.; Bonanomi, A.; Lozza, E. Measuring patient engagement: Development and psychometric properties of the Patient Health Engagement (PHE) Scale. Front. Psychol. 2015, 6, 274. [Google Scholar] [CrossRef] [PubMed]
- Al Fannah, J.; Al Harthy, H.; Al Salmi, Q. COVID-19 Pandemic: Learning Lessons and a Vision for a Better Health System. Oman Med. J. 2020, 35, e169. [Google Scholar] [CrossRef]
- Boccia, S.; Ricciardi, W.; Ioannidis, J.P.A. What Other Countries Can Learn From Italy During the COVID-19 Pandemic. JAMA Intern. Med. 2020, 180, 927–928. [Google Scholar] [CrossRef]
- Shoss, M.K.; Horan, K.A.; DiStaso, M.; LeNoble, C.A.; Naranjo, A. The Conflicting Impact of COVID-19’s Health and Economic Crises on Helping. Group Organ. Manag. 2021, 46, 3–37. [Google Scholar] [CrossRef]
- World Health Organization. Primary Health Care. Available online: https://www.who.int/news-room/fact-sheets/detail/primary-health-care (accessed on 9 November 2021).
- World Health Organization (WHO). The World Health Report: 1998: Life in the 21st Century, a Vision for All; World Health Organization: Geneva, Switzerland, 1998; ISBN 978-92-4-156189-1. [Google Scholar]
- Da Silva, M.A.; De Medeiros, S.M.; Chaves, A.E.P.; Santos, J.; De Sousa, Y.G.; Rezende, D. Work ability of nurses in Primary Health Care. Int. Arch. Med. 2016, 9, 1–8. [Google Scholar] [CrossRef]
- Marcadelli, S.; Stievano, A.; Rocco, G. Policy proposals for a new welfare: The development of the family and community nurse in Italy as the key to promote social capital and social innovation. Prim. Health Care Res. Dev. 2019, 20. [Google Scholar] [CrossRef]
- Rowe, A.; McClelland, A.; Billingham, K.; Carey, L. Community Health Needs Assessment: An Introductory Guide for the Family Health Nurse in Europe. WHO Reg. Off. Eur. 2001. Available online: https://apps.who.int/iris/handle/10665/108440 (accessed on 20 November 2021).
- American Nurses Association (ANA). Public Health Nursing. Available online: https://www.nursingworld.org/practice-policy/workforce/public-health-nursing/ (accessed on 21 March 2022).
- Sasso, L.; Bagnasco, A.; Aleo, G.; Zanini, M.; Pozzi, F.; Rodrigues, C.; Alvivo, S.; Musian, D.; Roba, I.; Turunen, H.; et al. Report on Current Family and Community Nurses Working and Occupational Contexts. 2018, 1–76. Available online: https://www.researchgate.net/publication/325046200_Report_on_Current_Family_and_Community_Nurses_Working_and_Occupational_Contexts (accessed on 20 November 2021).
- Flavell, T. An Overview of Eczema Management for Community Nurses. J. Community Nurs. 2015, 29, 83–92. [Google Scholar]
- González, C.G.; Molina, A.H.; Granizo, Y.E.S. Programa de especialización en Enfermería Familiar Comunitaria. Una realidad en Ecuador/Community and Family Nursing specialisation program: A reality in Ecuador. Educ. Médica 2016, 18, 44–48. [Google Scholar] [CrossRef][Green Version]
- Østergaard, B.; Mahrer-Imhof, R.; Shamali, M.; Nørgaard, B.; Jeune, B.; Pedersen, K.S.; Lauridsen, J. Effect of family nursing therapeutic conversations on patients with heart failure and their family members: Secondary outcomes of a randomised multicentre trial. J. Clin. Nurs. 2021, 30, 742–756. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.; Saunders, R.; Stuckhardt, L.; McGinnis, J.M. Engaging Patients, Families, and Communities. In Best Care at Lower Cost: The Path to Continuously Learning Health Care in America; National Academies Press: Washington, DC, USA, 2013; pp. 191–194. ISBN 978-0-309-26073-2. [Google Scholar]
- World Health Organization (WHO). The Family Health Nurse: Context, Conceptual Framework and Curriculum; WHO Regional Office for Europe: Copenhagen, Denmark, 2000; ISBN 978-92-890-1172-3. [Google Scholar]
- Anagnostopoulos, F.; Liolios, E.; Persefonis, G.; Slater, J.; Kafetsios, K.; Niakas, D. Physician Burnout and Patient Satisfaction with Consultation in Primary Health Care Settings: Evidence of Relationships from a one-with-many Design. J. Clin. Psychol. Med. Settings 2012, 19, 401–410. [Google Scholar] [CrossRef]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef]
- Stratton, S.J. Literature Reviews: Methods and Applications. Prehospital Disaster Med. 2019, 34, 347–349. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Tranfield, D.; Denyer, D.; Smart, P. Towards a Methodology for Developing Evidence-Informed Management Knowledge by Means of Systematic Review. Br. J. Manag. 2003, 14, 207–222. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 105906. [Google Scholar] [CrossRef]
- Popay, J.; Rogers, A.; Williams, G. Rationale and Standards for the Systematic Review of Qualitative Literature in Health Services Research. Qual. Health Res. 1998, 8, 341–351. [Google Scholar] [CrossRef]
- Methley, A.M.; Campbell, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv. Res. 2014, 14, 579. [Google Scholar] [CrossRef] [PubMed]
- The Joanna Briggs Institute. The Joanna Briggs Institute Joanna Briggs Institute Reviewers’ Manual: 2014 Edition/Supplement. In The Joanna Briggs Institute Reviewers’ Manual 2014 the Systematic Review of Economic Evaluation Evidence; The Joanna Briggs Institute: Adelaide, Australia, 2014; pp. 1–40. [Google Scholar]
- Porritt, K.; Gomersall, J.; Lockwood, C. JBI’s Systematic Reviews: Study Selection and Critical Appraisal. JBI’s Syst. Rev. 2014, 114, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, T.; Robert, G.; Macfarlane, F.; Bate, P.; Kyriakidou, O.; Peacock, R. Storylines of research in diffusion of innovation: A meta-narrative approach to systematic review. Soc. Sci. Med. 2005, 61, 417–430. [Google Scholar] [CrossRef] [PubMed]
- Papathanasiou, I.; Fradelos, E. Family Community Nursing Curriculum. Available online: https://www.enhance-fcn.eu/wp-content/uploads/2021/05/UTH-FCN-Curriculum_updated_compressed.pdf (accessed on 20 November 2021).
- Daly, B.; Smith, K. Promoting good dental health in older people: Role of the community nurse. Br. J. Community Nurs. 2015, 20, 431–436. [Google Scholar] [CrossRef]
- Holdoway, A.; Anderson, L. What more can community nurses do to manage adult malnutrition. Br. J. Community Nurs. 2019, 24, S6–S10. [Google Scholar] [CrossRef]
- Lumbers, M. Osteomyelitis, diabetic foot ulcers and the role of the community nurse. Br. J. Community Nurs. 2021, 26, S6–S9. [Google Scholar] [CrossRef]
- Bidone, S.; Pagano, B.; Garlasco, J. Evaluation of self-perceived competence among Family and Community Nurses who attained the Master’s Degree at the University of Eastern Piedmont (2013–2019): An exploratory survey. Assist. Inferm. Ric. 2021, 40, 30–38. [Google Scholar] [CrossRef]
- Courtenay, M. Community Nurse Prescribing. J. Community Nurs. 2018, 32, 18–20. [Google Scholar]
- Dening, K.H.; Hibberd, P. Exploring the community nurse role in family-centred care for patients with dementia. Br. J. Community Nurs. 2016, 21, 198–202. [Google Scholar] [CrossRef]
- Lee, G.; Pickstone, N.; Facultad, J.; Titchener, K. The future of community nursing: Hospital in the Home. Br. J. Community Nurs. 2017, 22, 174–180. [Google Scholar] [CrossRef]
- Terracciano, E.; Gentili, S.; Madaro, O.; Curti, E.; Inzerilli, M.C.; Albanese, L.; Accarino, N.; Tardi, A.; Orlando, S.; Riccardi, F.; et al. The effect of community nurse on mortality and hospitalization in a group of over-75 older adults: A nested case-control study. Ann. Ig. 2021, 33, 487–498. [Google Scholar] [PubMed]
- Balestra, M.L. Family Nurse Practitioner Scope of Practice Issues When Treating Patients With Mental Health Issues. J. Nurse Pract. 2019, 15, 479–482. [Google Scholar] [CrossRef]
- Bright, T.; Burdett, T. Smoking Cessation and the Health Promotion Role of Community Nurses. J. Community Nurs. 2019, 33, 56–60. [Google Scholar]
- Chater, A.; Courtenay, M. Community nursing and antibiotic stewardship: The importance of communication and training. Br. J. Community Nurs. 2019, 24, 338–342. [Google Scholar] [CrossRef]
- Clare, C.S. The Role of Community Nurses in Stroke Prevention. J. Community Nurs. 2017, 31, 54–58. [Google Scholar]
- Connolly, M.; Charnley, K.; Collins, R.; Barry, C.; McIlfatrick, S.; Larkin, P.; Brenner, M.; Johnston, B. Evaluating an educational programme for dignity care intervention with community nurses in Ireland. Int. J. Palliat. Nurs. 2018, 24, 474–481. [Google Scholar] [CrossRef]
- Ma, W.; Meng, X.; Wei, Y.; Li, J. Roles and activities of community nurses in China: A descriptive study. J. Nurs. Manag. 2018, 27, 433–441. [Google Scholar] [CrossRef]
- Phillips, A. Supporting smoking cessation in older patients: A continuing challenge for community nurses. Br. J. Community Nurs. 2016, 21, 457–461. [Google Scholar] [CrossRef][Green Version]
- Martínez-Riera, J.R.; Rodríguez, F.J.C. Family and Community Nursing, Chronology of a Specialty. Enferm. Clín. 2019, 29, 352–356. [Google Scholar] [CrossRef]
- Kent, S.; Dowling, M.; Byrne, G. Community nurses’ child protection role: Views of public health nurses in Ireland. Community Pract. J. Community Pract. Health Visit. Assoc. 2011, 84, 33–36. [Google Scholar]
- World Health Organization (WHO). Primary Health Care. Available online: https://www.who.int/westernpacific/health-topics/primary-health-care (accessed on 10 November 2021).
- Stuart, E. Nutrition and Wound Care: What Community Nurses Should Know. J. Community Nurs. 2020, 34, 58–62. [Google Scholar]
- Green, S.M.; James, E.P.; Latter, S.; Sutcliffe, M.; Fader, M.J. Barriers and facilitators to screening for malnutrition by community nurses: A qualitative study. J. Hum. Nutr. Diet. 2014, 27, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Simonetti, V.; Comparcini, D.; Tomietto, M.; Pavone, D.; Flacco, M.E.; Cicolini, G. Effectiveness of a family nurse-led programme on accuracy of blood pressure self-measurement: A randomised controlled trial. J. Clin. Nurs. 2021, 30, 2409–2419. [Google Scholar] [CrossRef] [PubMed]
- Jongudomkarn, D.; MacDuff, C. Development of a family nursing model for prevention of cancer and other noncommunicable diseases through an appreciative inquiry. Asian Pac. J. Cancer Prev. 2015, 15, 10367–10374. [Google Scholar] [CrossRef]
- Phelan, A. Elder abuse and the community nurse: Supporting the patient. Br. J. Community Nurs. 2010, 15, 472–478. [Google Scholar] [CrossRef]
- Howerton, C.R.; Ellington, B.J.; Henley, C. Breast Augmentation: Motives and the Role of the Family Nurse Practitioner. Plast. Surg. Nurs. 2011, 31, 95–99. [Google Scholar] [CrossRef]
- Mnisi, S.D.; Peu, D.; Meyer, S.M. Role of community nurses in the prevention of tuberculosis in the Tshwane Health District of Gauteng. Curationis 2012, 35, 9. [Google Scholar] [CrossRef]
- Roden, J.; Jarvis, L.; Campbell-Crofts, S.; Whitehead, D. Australian rural, remote and urban community nurses’ health promotion role and function. Health Promot. Int. 2015, 31, 704–714. [Google Scholar] [CrossRef]
- Savini, S.; Iovino, P.; Monaco, D.; Marchini, R.; Di Giovanni, T.; Donato, G.; Pulimeno, A.; Matera, C.; Quintavalle, G.; Turci, C. A family nurse-led intervention for reducing health services’ utilization in individuals with chronic diseases: The ADVICE pilot study. Int. J. Nurs. Sci. 2021, 8, 264–270. [Google Scholar] [CrossRef]
- Skingley, A. Older people, isolation and loneliness: Implications for community nursing. Br. J. Community Nurs. 2013, 18, 84–90. [Google Scholar] [CrossRef]
- Slevin, E. Learning disabilities: A survey of community nurses for people with prevalence of challenging behaviour and contact demands. J. Clin. Nurs. 2004, 13, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Nissanholtz–Gannot, R.; Shapiro, E. Community nurses and chronic disease in Israel: Professional dominance as a social justice issue. Nurs. Inq. 2021, 28, 12376. [Google Scholar] [CrossRef] [PubMed]
- Adderley, U.J.; Thompson, C. Community nurses & rsquo; judgement for the management of venous leg ulceration: A judgement analysis. Int. J. Nurs. Stud. 2015, 52, 345–354. [Google Scholar] [CrossRef]
- Aldridge, A. The role of the community nurse in psoriatic comorbidities interventions. Br. J. Community Nurs. 2014, 19, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Andrews, N.J.; Phillips, A.J. Community nurses’ support for patients with fibromyalgia who use cannabis to manage pain. Br. J. Community Nurs. 2021, 26, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, V. Patients with inflammatory arthritis: An opportunity for community nurses. Br. J. Community Nurs. 2011, 16, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Oliver, S. Understanding the needs of older people with rheumatoid arthritis: The role of the community nurse. Nurs. Older People 2009, 21, 30–37. [Google Scholar] [CrossRef]
- Ogston-Tuck, S. A silent epidemic: Community nursing and effective pain management. Br. J. Community Nurs. 2012, 17, 512–518. [Google Scholar] [CrossRef]
- Gregg, S.R.; Brown, A.; Pasvogel, A. Try-It-On: Preparing family nurse practitioners to use holistic integrative interventions to reduce opioid prescriptions in chronic pain management. J. Am. Assoc. Nurse Pract. 2020, 32, 37–44. [Google Scholar] [CrossRef]
- Weber, S. A Stigma Identification Framework for Family Nurses Working With Parents Who Are Lesbian, Gay, Bisexual, or Transgendered and Their Families. J. Fam. Nurs. 2010, 16, 378–393. [Google Scholar] [CrossRef]
- McCrae, N.; Bynoe, S. The role of community nurses in preventing female genital mutilation. Prim. Health Care 2015, 25, 30–33. [Google Scholar] [CrossRef]
- Jin, L.; Pan, R.; Huang, L.; Zhang, H.; Jiang, M.; Zhao, H. Family nursing with the assistance of network improves clinical outcome and life quality in patients underwent coronary artery bypass grafting: A Consolidated Standards of Reporting Trials-Compliant Randomized Controlled Trial. Medicine 2020, 99, e23488. [Google Scholar] [CrossRef]
- Davis, W.; Lewin, G.; Davis, T.; Bruce, D. Determinants and costs of community nursing in patients with type 2 diabetes from a community-based observational study: The Fremantle Diabetes Study. Int. J. Nurs. Stud. 2013, 50, 1166–1171. [Google Scholar] [CrossRef] [PubMed]
- Kwok, T.; Lee, J.; Woo, J.; Lee, D.T.; Griffith, S. A randomized controlled trial of a community nurse-supported hospital discharge programme in older patients with chronic heart failure. J. Clin. Nurs. 2007, 17, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Yates, A. Basic Continence Assessment: What Community Nurses Should Know. J. Community Nurs. 2019, 33, 52–55. [Google Scholar]
- Duncan, D. Role of the community nurse in Parkinson’s disease and lower urinary disorders. Br. J. Community Nurs. 2021, 26, 251–254. [Google Scholar] [CrossRef] [PubMed]
- Reid, J. Managing Urinary Incontinence: Guidelines for Community Nurses. J. Community Nurs. 2014, 28, 20–26. [Google Scholar]
- Nazarko, L. Cognitive assessment: A guide for community nurses. Br. J. Community Nurs. 2013, 18, 550–553. [Google Scholar] [CrossRef]
- Nazarko, L. Considering the difficulties with dysphagia: An overview for community nurses. Br. J. Community Nurs. 2016, 21, 226–230. [Google Scholar] [CrossRef]
- McKenzie, H.; Boughton, M.; Hayes, L.; Forsyth, S.; Davies, M.; Underwood, E.; McVey, P. A sense of security for cancer patients at home: The role of community nurses. Health Soc. Care Community 2007, 15, 352–359. [Google Scholar] [CrossRef]
- Kelly, A.M. What can community nurses do for older adults who experience faecal incontinence? Br. J. Community Nurs. 2019, 24, 28–31. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A. Analysing the role played by district and community nurses in bereavement support. Br. J. Community Nurs. 2015, 20, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A. Role of district and community nurses in bereavement care: A qualitative study. Br. J. Community Nurs. 2015, 20, 494–501. [Google Scholar] [CrossRef] [PubMed]
- Adamson, E.; Cruickshank, S. A “good Death” at Home: Community Nurses Helping to Make It Possible. Br. J. Community Nurs. 2013, 18, 40–42. [Google Scholar] [CrossRef] [PubMed]
- Husband, J. The evolving role of the community nurse specialist in palliative care. Br. J. Community Nurs. 2008, 13, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Mendes, A. A community nurse’s role in supporting a “good” experience of grief. Br. J. Community Nurs. 2017, 22, 566–567. [Google Scholar] [CrossRef]
- Pickstock, S. Breathlessness at End of Life: What Community Nurses Should Know. J. Community Nurs. 2017, 31, 74–77. [Google Scholar]
- Caruso, R.; Fida, R.; Sili, A.; Arrigoni, C. Towards an integrated model of nursing competence: An overview of the literature reviews and concept analysis. Prof. Inferm. 2016, 69, 35–43. [Google Scholar] [CrossRef]
- Bagnasco, A.; Zanini, M.; Pozzi, F.; Aleo, G.; Catania, G.; Sasso, L. Uno Studio Europeo E-Delphi per Identificare Le Competenze Fondamentali per La Definizione Del Percorso Formativo Dell’Infermiere Di Famiglia e Di Comunità. L’infermiere 2020, 57, 75–93. [Google Scholar]
- International Family Nursing Association (IFNA). IFNA Position Statement on Planetary Health and Family Health. Available online: https://internationalfamilynursing.org/2020/04/18/ifna-position-statement-on-planetary-health-and-family-health/ (accessed on 8 October 2021).
- Pisano González, M.M.; González Pisano, A.C.; Bassols, A.A. Community and Family Nurse: Present Keys, Future Challenges. Enferm. Clin. 2019, 29, 365–369. [Google Scholar] [CrossRef]
- Van Huy, N.; Bang, K.; Xuan, H.T.A.; Thang, C.D.; Van Thanh, N.; Hoan, L.T.; Tak, S.; Yu, S.-Y.; Yi, J.; Son, D.T.; et al. The roles of, activities of, and competencies for, community nursing services in rural Vietnam: Implications for policy decisions. Int. J. Health Plan. Manag. 2018, 33, e1147–e1159. [Google Scholar] [CrossRef]
- Wacharasin, C.; Theinpichet, S. Family Nursing Practice, Education, and Research: What Is Happening in Thailand? J. Fam. Nurs. 2008, 14, 429–435. [Google Scholar] [CrossRef]
- Wilkes, L.; Cioffi, J.; Cummings, J.; Warne, B.; Harrison, K. Clients with chronic conditions: Community nurse role in a multidisciplinary team. J. Clin. Nurs. 2013, 23, 844–855. [Google Scholar] [CrossRef] [PubMed]
- Miguélez-Chamorro, A.; Ferrer-Arnedo, C. The family and community nurse: Health agent and model for the chronic patient within the community. Enferm. Clin. 2014, 24, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Widyarani, D.; Susanto, T.; Wahyuni, D.; Pham, H.T.T. Identifying Community/Public Health Nursing Competencies in Indonesia: A Modified Delphi Method. Nurse Media J. Nurs. 2020, 10, 350–360. [Google Scholar] [CrossRef]
- Norman, K.M. The image of community nursing: Implications for future student nurse recruitment. Br. J. Community Nurs. 2015, 20, 12–18. [Google Scholar] [CrossRef]
- Mendes, A. Personal beliefs, culture and religion in community nursing care. Br. J. Community Nurs. 2018, 23, 46–47. [Google Scholar] [CrossRef]
- Falavigna, G.; Ippoliti, R. The socio-economic planning of a community nurses programme in mountain areas: A Directional Distance Function approach. Socio-Econ. Plan. Sci. 2020, 71, 100770. [Google Scholar] [CrossRef]
- Omeri, A.; Malcolm, P. Cultural diversity: A challenge for community nurses. Contemp. Nurse 2004, 17, 183–191. [Google Scholar] [CrossRef]
- Wood-Baker, R.; Reid, D.; Robinson, A.; Walters, E.H. Clinical trial of community nurse mentoring to improve self-management in patients with chronic obstructive pulmonary disease. Int. J. Chronic Obstr. Pulm. Dis. 2012, 7, 407. [Google Scholar] [CrossRef]
- Cramm, J.M.; Nieboer, A.P. Self-management abilities and quality of life among frail community-dwelling individuals: The role of community nurses in the Netherlands. Health Soc. Care Community 2016, 25, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Broekema, S.; Paans, W.; Roodbol, P.F.; Luttik, M.L.A. Effects of family nursing conversations on families in home health care: A controlled before-and-after study. J. Adv. Nurs. 2021, 77, 231–243. [Google Scholar] [CrossRef] [PubMed]
- Ippoliti, R.; Allievi, I.; Falavigna, G.; Giuliano, P.; Montani, F.; Obbia, P.; Rizzi, S.; Moda, G. The sustainability of a community nurses programme aimed at supporting active ageing in mountain areas. Int. J. Health Plan. Manag. 2018, 33, e1100–e1111. [Google Scholar] [CrossRef]
- Zimansky, M.; Stasielowicz, L.; Franke, I.; Remmers, H.; Friedel, H.; Atzpodien, J. Effects of Implementing a Brief Family Nursing Intervention With Hospitalized Oncology Patients and Their Families in Germany: A Quasi-Experimental Study. J. Fam. Nurs. 2020, 26, 346–357. [Google Scholar] [CrossRef] [PubMed]
- Nissanholtz-Gannot, R.; The Community Nursing Study Group; Rosen, B.; Hirschfeld, M. The changing roles of community nurses: The case of health plan nurses in Israel. Isr. J. Health Policy Res. 2017, 6, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Morin, D.; Aubin, M.; Vezina, L.; Gagnon, J.; Racine, S.; Reinharz, D.; Paradis, M.; Dallaire, C.; Aubin, K. From Hospital to Home After Cardiac Surgery: Evaluation of a Community Nursing Care Management Model. Prof. Case Manag. 2009, 14, 167–175. [Google Scholar] [CrossRef]
- Vogel, R.G.M.; Bours, G.J.J.W.; Rooijackers, T.H.; Metzelthin, S.F.; Erkens, P.M.G.; van Rossum, E.; Zwakhalen, S.M.G. Process evaluation of a programme to empower community nurse leadership. BMC Nurs. 2021, 20, 127. [Google Scholar] [CrossRef]
- Macdonald, J.M. Combination Model of Care for community nurse practitioners. Br. J. Nurs. 2005, 14, 1144–1148. [Google Scholar] [CrossRef]
- Lalani, M.; Fernandes, J.; Fradgley, R.; Ogunsola, C.; Marshall, M. Transforming community nursing services in the UK; lessons from a participatory evaluation of the implementation of a new community nursing model in East London based on the principles of the Dutch Buurtzorg model. BMC Health Serv. Res. 2019, 19, 945. [Google Scholar] [CrossRef]
- Cavada, L.; Siller, M.; Quircio, S.; Groeber, G.; Fink, I.; Preusse-Bleuler, B.; Battisti, E. L’esperienza dell’introduzione dell’infermiere di famiglia in un comune della Provincia di Bolzano. Assist. Inferm. E Ric. 2021, 40, 158–162. [Google Scholar] [CrossRef]
- Looman, W.S. Teaching Systems Thinking for Advanced Family Nursing Practice: A Theory-Based Tool. J. Fam. Nurs. 2019, 26, 5–14. [Google Scholar] [CrossRef]
- Schober, M.; Affara, F.A. International Council of Nurses: Advanced Nursing Practice; Blackwell Pub.: Oxford, UK; Malden, MA, USA, 2006; ISBN 978-1-4051-2533-8. [Google Scholar]
- Randall, D.; Collins, E. Community nursing: Will new standards be a panacea? Br. J. Nurs. 2021, 30, 880. [Google Scholar] [CrossRef]
- Dlamini, C.P.; Khumalo, T.; Nkwanyana, N.; Mathunjwa-Dlamini, T.R.; Macera, L.; Nsibandze, B.S.; Kaplan, L.; Stuart-Shor, E.M. Developing and Implementing the Family Nurse Practitioner Role in Eswatini: Implications for Education, Practice, and Policy. Ann. Glob. Health 2020, 86, 50. [Google Scholar] [CrossRef] [PubMed]
- Fu, W.; Bao, J.; Meng, J. Development of community nursing in Zhejiang Province, China: A report of the driving measures. Int. Nurs. Rev. 2010, 57, 265–268. [Google Scholar] [CrossRef] [PubMed]
- Yingling, C.T.; Cotler, K.; Hughes, T. Building nurses’ capacity to address health inequities: Incorporating lesbian, gay, bisexual and transgender health content in a family nurse practitioner programme. J. Clin. Nurs. 2017, 26, 2807–2817. [Google Scholar] [CrossRef] [PubMed]
- World Cancer Research Fund (WCRF). American Institute for Cancer Research (AICR) Recommendations and Public Health and Policy Implications. Contin. Update Proj. Expert Rep. 2018, 2018, 1–92. [Google Scholar]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Longhini, J.; Saiani, L.; Palese, A. La complessità della ricerca infermieristica nelle cure primarie: Appunti di metodo. Assist. Inferm. Ric. 2021, 40, 175–182. [Google Scholar] [CrossRef]
- Conti, A.; Albanesi, B.; Brusca, E.; Martini, L.; Costa, C.; Campagna, S. L’infermiere di famiglia e comunità: Panoramica sull’esercizio della professione in Europa. Assist. Inferm. Ric. 2021, 40, 131–136. [Google Scholar] [CrossRef]
- Moorhead, S.; Swanson, E.; Johnson, M.; Maas, M.L. Nursing Outcomes Classification (NOC): Measurement of Health Outcomes, 6th ed.; Elsevier: St. Louis, MI, USA, 2018; ISBN 978-0-323-49764-0. [Google Scholar]
- Werley, H.H.; Devine, E.C.; Zorn, C.R.; Ryan, P.; Westra, B.L. The Nursing Minimum Data Set: Abstraction tool for standardized, comparable, essential data. Am. J. Public Health 1991, 81, 421–426. [Google Scholar] [CrossRef][Green Version]
- Morris, R.; Matthews, A.; Scott, A.P. Validity, reliability and utility of the Irish Nursing Minimum Data Set for General Nursing in investigating the effectiveness of nursing interventions in a general nursing setting: A repeated measures design. Int. J. Nurs. Stud. 2014, 51, 562–571. [Google Scholar] [CrossRef] [PubMed]
- Emre, I.E.; Erol, N.; Ayhan, Y.I.; Özkan, Y.; Erol, Ç. The analysis of the effects of acute rheumatic fever in childhood on cardiac disease with data mining. Int. J. Med. Inform. 2019, 123, 68–75. [Google Scholar] [CrossRef] [PubMed]

| First Author | Year | Clinical Practice | Core Competencies | Outcomes | Organizational and Educational Models | Advanced Training Program |
|---|---|---|---|---|---|---|
| Adamson E. | 2013 | X | ||||
| Adderley J. | 2015 | X | ||||
| Aldridge A. | 2014 | X | X | |||
| Andrews N. | 2021 | X | ||||
| Bagnasco A. | 2020 | X | ||||
| Balestra M. | 2019 | X | ||||
| Bidone S. | 2021 | X | X | X | ||
| Bright T. | 2019 | X | X | |||
| Broekema S. | 2020 | X | ||||
| Cavada L. | 2021 | X | ||||
| Chamberlain V. | 2016 | X | ||||
| Chamorro A. | 2014 | X | ||||
| Chater A. | 2019 | X | X | |||
| Clare C.S. | 2017 | X | ||||
| Connolly M. | 2018 | X | ||||
| Courtenay M. | 2018 | X | X | |||
| Cramm J.M. | 2017 | X | ||||
| Daly B. | 2015 | X | ||||
| Davis W.A. | 2013 | X | X | |||
| Dening H.K. | 2016 | X | ||||
| Dlamini C.P. | 2020 | X | ||||
| Duncan D. | 2021 | X | ||||
| Falavigna G. | 2020 | X | X | |||
| Flavell T. | 2015 | X | ||||
| Fu W. | 2010 | X | ||||
| Gafas González C. | 2017 | X | X | |||
| Green S.M. | 2014 | X | ||||
| Gregg S.R. | 2019 | X | X | |||
| Holdoway A. | 2019 | X | ||||
| Howerton C.R. | 2011 | X | X | |||
| Husband J. | 2008 | X | ||||
| International Family Nursing Association (INFA) | 2020 | X | X | |||
| Ippoliti R. | 2018 | X | X | |||
| Jin L. | 2020 | X | X | |||
| Johnson A. | 2015 | X | X | |||
| Johnson A. | 2015 | X | X | |||
| Jongudomkarn D. | 2014 | X | X | X | ||
| Kelly A.M. | 2019 | X | X | |||
| Kent S. | 2011 | X | ||||
| Kwok T. | 2008 | X | X | |||
| Lalani M. | 2019 | X | ||||
| Lee G. | 2017 | X | ||||
| Looman W.S. | 2020 | X | X | |||
| Lumbers M. | 2021 | X | ||||
| Ma W. | 2018 | X | ||||
| MacDonald J.M. | 2005 | X | ||||
| Marcadelli S. | 2019 | X | X | |||
| Martinez-Riera J.R. | 2019 | X | ||||
| McCrae N. | 2014 | X | ||||
| McKenzie J.E. | 2007 | X | ||||
| Mendes A. | 2018 | X | ||||
| Mendes A. | 2017 | X | ||||
| Mnisi S.D. | 2012 | X | ||||
| Morin D. | 2009 | X | ||||
| Nazarko L. | 2013 | X | ||||
| Nazarko L. | 2016 | X | ||||
| Nissanholtz-Gannot R. | 2020 | X | ||||
| Nissanholtz-Gannot R. | 2017 | X | ||||
| Norman K.M. | 2015 | X | ||||
| Ogston-Tuck S.A. | 2018 | X | ||||
| Oliver S. | 2009 | X | ||||
| Omeri A. | 2004 | X | ||||
| Østergaard B. | 2021 | X | ||||
| Papadopoulou C. | 2021 | X | ||||
| Papathanasiou I. | 2020 | X | ||||
| Phelan A. | 2010 | X | ||||
| Phillips A. | 2016 | X | X | |||
| Pickstock S. | 2017 | X | ||||
| Pisano González M.M. | 2019 | X | X | |||
| Randall D. | 2021 | X | ||||
| Reid J. | 2014 | X | ||||
| Roden J. | 2016 | X | X | |||
| Sasso L. | 2018 | X | ||||
| Savini S. | 2021 | X | X | |||
| Simonetti V. | 2021 | X | X | |||
| Skingley A. | 2016 | X | ||||
| Slevin E. | 2003 | X | ||||
| Stuart E. | 2020 | X | ||||
| Terracciano E. | 2020 | X | ||||
| Huy N.V. | 2018 | X | ||||
| Vogel R.G. | 2021 | X | ||||
| Wacharasin C. | 2008 | X | ||||
| Wang S. | 2019 | X | X | |||
| Weber S. | 2010 | X | ||||
| Widyarani D. | 2020 | X | ||||
| Wilkes L. | 2014 | X | ||||
| Wood-Baker R. | 2012 | X | ||||
| Yates A. | 2019 | X | ||||
| Yingling C.T. | 2017 | X | ||||
| Zimansky M. | 2020 | X | ||||
| Total number of studies | 90 | 54 | 20 | 21 | 9 | 14 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dellafiore, F.; Caruso, R.; Cossu, M.; Russo, S.; Baroni, I.; Barello, S.; Vangone, I.; Acampora, M.; Conte, G.; Magon, A.; et al. The State of the Evidence about the Family and Community Nurse: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 4382. https://doi.org/10.3390/ijerph19074382
Dellafiore F, Caruso R, Cossu M, Russo S, Baroni I, Barello S, Vangone I, Acampora M, Conte G, Magon A, et al. The State of the Evidence about the Family and Community Nurse: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(7):4382. https://doi.org/10.3390/ijerph19074382
Chicago/Turabian StyleDellafiore, Federica, Rosario Caruso, Michela Cossu, Sara Russo, Irene Baroni, Serena Barello, Ida Vangone, Marta Acampora, Gianluca Conte, Arianna Magon, and et al. 2022. "The State of the Evidence about the Family and Community Nurse: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 7: 4382. https://doi.org/10.3390/ijerph19074382
APA StyleDellafiore, F., Caruso, R., Cossu, M., Russo, S., Baroni, I., Barello, S., Vangone, I., Acampora, M., Conte, G., Magon, A., Stievano, A., & Arrigoni, C. (2022). The State of the Evidence about the Family and Community Nurse: A Systematic Review. International Journal of Environmental Research and Public Health, 19(7), 4382. https://doi.org/10.3390/ijerph19074382