Bringing Parent–Child Interaction Therapy to South Africa: Barriers and Facilitators and Overall Feasibility—First Steps to Implementation
Abstract
:1. Introduction
1.1. Parent–Child Interaction Therapy
1.2. Implementation Science: Bringing Evidence-Based Intervention to LMIC
2. Methods
2.1. Design
2.2. Participants
2.2.1. Clinicians
2.2.2. Caregivers
2.3. Contextual Background and Procedures
2.4. Data Generation
2.5. Measures
2.6. Data Analysis
2.7. Ethics
3. Results
3.1. Caregiver Participants Section
3.2. Therapist Fidelity Results
3.3. Therapist Perceptions of Barriers and Facilitators to Implementation
3.4. Next Steps
4. Discussion
4.1. Caregiver Satisfaction and Acceptability
4.2. Therapist Fidelity Ratings
4.3. Therapist Perspectives on Facilitators and Barriers
4.4. Implementation and Stakeholders
4.5. Next Steps for PCIT in South Africa
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Keynejad, R.C.; Dua, T.; Barbui, C.; Thornicroft, G. WHO Mental Health Gap Action Programme (mhGAP) Intervention Guide: A systematic review of evidence from low and middle-income countries Evid. Based Ment. Health 2018, 21, 30–34. [Google Scholar] [CrossRef] [Green Version]
- Keynejad, R.; Spagnolo, J.; Thornicroft, G. WHO mental health gap action programme (mhGAP) intervention guide: Updated systematic review on evidence and impact. Evid. Based Ment. Health 2021, 24, 124–130. [Google Scholar] [CrossRef]
- Bruha, L.; Spyridou, V.; Forth, G.; Ougrin, D. Global child and adolescent mental health: Challenges and advances. Lond. J. Prim. Care 2018, 10, 108–109. [Google Scholar] [CrossRef]
- Olusanya, B.O.; Davis, A.C.; Wertlieb, D.; Boo, N.Y.; Nair, M.; Halpern, R.; Kuper, H.; Breinbauer, C.; de Vries, P.J.; Gladstone, M.; et al. Developmental disabilities among children younger than 5 years in 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Glob. Health 2018, 6, e1100–e1121. [Google Scholar] [CrossRef] [Green Version]
- Zhou, W.; Ouyang, F.; Nergui, O.E.; Bangura, J.B.; Acheampong, K.; Massey, I.Y.; Xiao, S. Child and Adolescent Mental Health Policy in Low- and Middle-Income Countries: Challenges and Lessons for Policy Development and Implementation. Front. Psychiatry 2020, 11, 150. [Google Scholar] [CrossRef]
- Saxena, S.; Thornicroft, G.; Knapp, M.; Whiteford, H. Resources for mental health: Scarcity, inequity, and inefficiency. Lancet 2007, 8, 878–889. [Google Scholar] [CrossRef]
- Alem, A.; Kebede, D.; Fekadu, A.; Shibre, T.; Fekadu, D.; Beyero, T.; Medhin, G.; Negash, A.; Kullgren, G. Clinical course and outcome of schizophrenia in a predominantly treatment-naive cohort in rural Ethiopia. Schizophr. Bull. 2009, 35, 646–654. [Google Scholar] [CrossRef]
- Patel, V.; Maj, M.; Flisher, A.J.; De Silva, M.J.; Koschorke, M.; Prince, M. WPA Zonal and Member Society Representatives. Reducing the treatment gap for mental disorders: A WPA survey. World Psychiatry 2010, 9, 169–176. [Google Scholar] [CrossRef] [Green Version]
- Flisher, A.J.; Dawes, A.; Kafaar, Z.; Lund, C.; Sorsdahl, K.; Myers, B.; Thom, R.; Seedat, S. Child and adolescent mental health in South Africa. J. Child Adolesc. Ment. Health 2012, 24, 149–161. [Google Scholar] [CrossRef]
- Mokitimi, S.; Schneider, M.; de Vries, P.J. A situational analysis of child and adolescent mental health services and systems in the Western Cape Province of South Africa. Child Adolesc. Psychiatry Ment. Health 2022, 16, 6. [Google Scholar] [CrossRef]
- De Vries, P.J. Thinking globally to meet local needs: Autism spectrum disorders in Africa and other low-resource environments. Curr. Opin. Neurol. 2016, 29, 130–136. [Google Scholar] [CrossRef]
- Kleintjes, S.; Flisher, A.J.; Fick, M.; Railoun, A.; Lund, C.; Molteno, C.; Robertson, B.A. The prevalence of mental disorders among children, adolescents and adults in the Western Cape, South Africa. S. Afr. Psychiatry Rev. 2006, 9, 157–160. [Google Scholar] [CrossRef] [Green Version]
- Smith, J.P.; Smith, G.C. Long-term economic costs of psychological problems during childhood. Soc. Sci. Med. 2010, 71, 110–115. [Google Scholar] [CrossRef] [Green Version]
- Boylan, K.; Vaillancourt, T.; Boyle, M.; Szatmari, P. Comorbidity of internalizing disorders in children with oppositional defiant disorder. Eur. Child Adolesc. Psychiatry 2007, 16, 484–494. [Google Scholar] [CrossRef]
- Evans, S.C.; Pederson, C.A.; Fite, P.J.; Blossom, J.B.; Cooley, J.L. Teacher-reported irritable and defiant dimensions of oppositional defiant disorder: Social, behavioral, and academic correlates. Sch. Ment. Health A Multidiscip. Res. Pract. J. 2016, 8, 292–304. [Google Scholar] [CrossRef]
- Sari Gokten, E.; Saday Duman, N.; Soylu, N.; Uzun, M.E. Effects of attention-deficit/hyperactivity disorder on child abuse and neglect. Child Abuse. Negl. 2016, 62, 1–9. [Google Scholar] [CrossRef]
- Burke, J.D.; Hipwell, A.E.; Loeber, R. Dimensions of oppositional defiant disorder as predictors of depression and conduct disorder in preadolescent girls. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 484–492. [Google Scholar]
- Burke, J.D.; Stepp, S.D. Adolescent disruptive behavior and borderline personality disorder symptoms in young adult men. J. Abnorm. Child Psychol. 2012, 40, 35–44. [Google Scholar] [CrossRef] [Green Version]
- Herschell, A.D.; Kolko, D.J.; Scudder, A.T.; Taber-Thomas, S.; Schaffner, K.F.; Hiegel, S.A.; Iyengar, S.; Chaffin, M.; Mrozowski, S. Protocol for a state-wide randomised controlled trial to compare three training models for implementing an evidence-based treatment. Implement. Sci. 2015, 10, 133. [Google Scholar] [CrossRef] [Green Version]
- Eyberg, S.M.; Nelson, M.M.; Boggs, S.R. Evidence-based psychosocial treatments for children and adolescents with disruptive behaviour. J. Clin. Child Adolesc. Psychol. 2008, 37, 215–237. [Google Scholar] [CrossRef]
- Cooley, M.E.; Veldorale-Griffin, A.; Petren, R.E.; Mullis, A.K. Parent–Child Interaction Therapy: A Meta-Analysis of Child Behavior Outcomes and Parent Stress. J. Fam. Soc. Work. 2014, 17, 191–208. [Google Scholar] [CrossRef]
- Wagner, S.M.; McNeil, C.B. Parent-child interaction therapy for ADHD: A conceptual overview and critical literature review. Child Fam. Behav. Ther. 2008, 30, 231–256. [Google Scholar] [CrossRef]
- Choate, M.L.; Pincus, D.B.; Eyberg, S.M.; Barlow, D.H. Parent-Child Interaction Therapy for Treatment of Separation Anxiety Disorder in Young Children: A Pilot Study. Cogn. Behav. Pract. 2005, 12, 126–135. [Google Scholar] [CrossRef]
- Chronis-Tuscano, A.; Lewis-Morrarty, E.; Woods, K.E.; O’Brien, K.A.; Mazursky-Horowitz, H.; Thomas, S.R. Parent-child interaction therapy with emotion coaching for preschoolers with attention-deficit/hyperactivity disorder. Cogn. Behav. Pract. 2016, 23, 62–78. [Google Scholar] [CrossRef]
- Danko, C.M.; Garbacz, L.L.; Budd, K.S. Outcomes of Parent–Child Interaction Therapy in an urban community clinic: A comparison of treatment completers and dropouts. Child. Youth Serv. Rev. 2016, 60, 42–51. [Google Scholar] [CrossRef]
- Thomas, R.; Abell, B.; Webb, H.J.; Avdagic, E.; Zimmer-Gembeck, M.J. Parent-Child Interaction Therapy: A Meta-analysis. Pediatrics 2017, 140, e20170352. [Google Scholar] [CrossRef] [Green Version]
- Gross, D.; Belcher, H.M.; Budhathoki, C.; Ofonedu, M.E.; Dutrow, D.; Uveges, M.K.; Slade, E. Reducing preschool behavior problems in an urban mental health clinic: A pragmatic, non-inferiority trial. J. Am. Acad. Child Adolesc. Psychiatry 2019, 58, 572–581. [Google Scholar] [CrossRef] [Green Version]
- Eisenstadt, T.H.; Eyberg, S.; McNeil, C.B.; Newcomb, K.; Funderburk, B. Parent-child interaction therapy with behavior problem children: Relative effectiveness of two stages and overall treatment outcome. J. Clin. Child Psychol. 1993, 22, 42–51. [Google Scholar] [CrossRef]
- Eyberg, S.M.; Funderburk, B.W.; Hembree-Kigin, T.L.; McNeil, C.B.; Querido, J.G.; Hood, K.K. Parent-child interaction therapy with behavior problem children: One and two year maintenance of treatment effects in the family. Child Fam. Behav. Ther. 2001, 23, 1–20. [Google Scholar] [CrossRef]
- Nixon, R.D.; Sweeney, L.; Erickson, D.B.; Touyz, S.W. Parent-child interaction therapy: A comparison of standard and abbreviated treatments for oppositional defiant preschoolers. J. Consult. Clin. Psychol. 2003, 71, 251. [Google Scholar] [CrossRef] [Green Version]
- Lieneman, C.C.; Brabson, L.A.; Highlander, A.; Wallace, N.M.; McNeil, C.B. Parent–Child Interaction Therapy: Current Perspectives. Psychol. Res. Behav. Manag. 2017, 10, 239–256. [Google Scholar] [CrossRef] [Green Version]
- McInnis, P.; Kohlhoff, J.; Eapen, V. Real-world outcomes of PCIT for children at risk of autism or developmental delay. J. Child Fam. Stud. 2020, 29, 1701–1711. [Google Scholar] [CrossRef]
- Chase, R.M.; Eyberg, S.M. Clinical presentation and treatment outcome for children with comorbid externalizing and internalizing symptoms. J. Anxiety Disord. 2008, 22, 273–282. [Google Scholar] [CrossRef]
- Floyd, E.M.; Eyberg, S.M. Testing the attachment theory of parent-child interaction therapy. Poster session. In Proceedings of the Annual Meeting of the American Psychological Association, Toronto, Canada, 7–10 August 2003. [Google Scholar]
- Goldfine, M.E.; Wagner, S.M.; Branstetter, S.A.; Mcneil, C.B. Parent-child interaction therapy: An examination of cost-effectiveness. J. Early Intensive Behav. Interv. 2008, 5, 119. [Google Scholar] [CrossRef] [Green Version]
- Herschell, A.D.; Scudder, A.B.; Schaffner, K.F.; Slagel, L.A. Feasibility and Effectiveness of Parent Child Interaction Therapy with Victims of Domestic Violence: A Pilot Study. J. Child Fam. Stud. 2017, 26, 271–283. [Google Scholar] [CrossRef]
- Jackson, C.B.; Herschell, A.D.; Schaffner, K.F.; Turiano, N.A.; McNeil, C.B. Training community-based clinicians in parent-child interaction therapy: The interaction between expert consultation and caseload. Prof. Psychol. Res. Pract. 2017, 48, 481–489. [Google Scholar] [CrossRef]
- Niec, L.N.; Hemme, J.M.; Yopp, J.M.; Brestan, E.V. Parent-child interaction therapy: The rewards and challenges of a group format. Cogn. Behav. Pract. 2005, 12, 113–125. [Google Scholar] [CrossRef]
- Ware, L.M.; McNeil, C.B.; Masse, J.; Stevens, S. Efficacy of in-home parent-child interaction therapy. Child Fam. Behav. Ther. 2008, 30, 99–126. [Google Scholar] [CrossRef] [Green Version]
- Graziano, P.A.; Bagner, D.M.; Slavec, J.; Hungerford, G.; Kent, K.; Babinski, D.; Pasalich, D. Feasibility of intensive parent-child interaction therapy (I-PCIT): Results from an open trial. J. Psychopathol. Behav. Assess. 2015, 37, 38–49. [Google Scholar] [CrossRef] [Green Version]
- Abrahamse, M.; Egan, R.; Coelman, F.; Heiner, W. Transporting PCIT around the world. In Handbook of Parent-Child Interaction Therapy; Springer: Cham, Switzerland, 2008; pp. 269–281. [Google Scholar]
- Abrahamse, M.E.; Junger, M.; van Wouwe, M.A.; Boer, F.; Lindauer, R.J. Treating child disruptive behavior in high-risk families: A comparative effectiveness trial from a community-based implementation. J. Child Fam. Stud. 2016, 25, 1605–1622. [Google Scholar] [CrossRef] [Green Version]
- Bjørseth, Å.; Wichstrøm, L. Effectiveness of parent-child interaction therapy (PCIT) in the treatment of young children’s behavior problems. A randomized controlled study. PLoS ONE 2016, 11, e0159845. [Google Scholar] [CrossRef] [Green Version]
- Leung, C.; Tsang, S.; Heung, K.; Yiu, I. Effectiveness of Parent-Child interaction therapy (PCIT) among Chinese families. Res. Soc. Work. Pract. 2009, 19, 304–313. [Google Scholar] [CrossRef] [Green Version]
- Phillips, J.; Morgan, S.; Cawthorne, K.; Barnett, B. Pilot evaluation of Parent-Child Interaction Therapy (PCIT) delivered in an Australian community early childhood clinic setting. Aust. N. Z. J. Psychiatry 2008, 42, 712–719. [Google Scholar] [CrossRef] [PubMed]
- Woodfield, M.J.; Cargo, T.; Merry, S.N.; Hetrick, S.E. Barriers to Clinician Implementation of Parent-Child Interaction Therapy (PCIT) in New Zealand and Australia: What Role for Time-Out? Int. J. Environ. Res. Public Health 2021, 18, 13116. [Google Scholar] [CrossRef] [PubMed]
- Heymann, P.; Heflin, B.H.; Bagner, D.M. Parent-Child Interaction Therapy: Theory and Research to Practice. In Selected Topics in Child and Adolescent Mental Health; Stones, S., Glazzard, J., Muzio, M.R., Eds.; IntechOpen: Vienna, Austria, 2020. [Google Scholar] [CrossRef] [Green Version]
- Schlebusch, L.; Chambers, N.J.; Dawson-Squibb, J.J.; Harty, M.; Franz, L.; de Vries, P.J. Challenges and opportunities of implementing early interventions for autism spectrum disorders in resource-limited settings: A South African example. In Starting At the Beginning; Academic Press: Cambridge, MA, USA, 2020; pp. 99–132. [Google Scholar]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 2009, 4, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Bammer, G. Integration and implementation sciences: Building a new specialization. Ecol. Soc. 2003, 10, 95–107. [Google Scholar] [CrossRef]
- Proctor, E.; Silmere, H.; Raghavan, R.; Hovmand, P.; Aarons, G.; Bunger, A.; Griffey, R.; Hensley, M. Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Adm. Policy Ment. Health 2011, 38, 65–76. [Google Scholar] [CrossRef] [Green Version]
- Funderburk, B.W.; Ware, L.M.; Altshuler, E.; Chaffin, M. Use and feasibility of telemedicine technology in the dissemination of parent-child interaction therapy. Child Maltreatment 2008, 13, 377–382. [Google Scholar] [CrossRef]
- Kumm, A.J.; Viljoen, M.; de Vries, P.J. The Digital Divide in Technologies for Autism: Feasibility Considerations for Low- and Middle-Income Countries. J. Autism. Dev. Disord. 2021, 13, 1–14. [Google Scholar] [CrossRef]
- Karsh, B.T. Beyond usability: Designing effective technology implementation systems to promote patient safety. Qual. Saf. Health Care 2004, 13, 388–394. [Google Scholar] [CrossRef] [Green Version]
- Aarons, G.A.; Sklar, M.; Mustanski, B.; Benbow, N.; Brown, C.H. “Scaling-out” evidence-based interventions to new populations or new health care delivery systems. Implement. Sci. 2017, 12, 111. [Google Scholar] [CrossRef] [PubMed]
- Means, A.R.; Kemp, C.G.; Gwayi-Chore, M.C.; Gimbel, S.; Soi, C.; Sherr, K.; Weiner, B.J. Evaluating and optimizing the consolidated framework for implementation research (CFIR) for use in low-and middle-income countries: A systematic review. Implement. Sci. 2020, 15, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Vivanti, G.; Kasari, C.; Green, J.; Mandell, D.; Maye, M.; Hudry, K. Implementing and evaluating early intervention for children with autism: Where are the gaps and what should we do? Autism Res. 2018, 11, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Chambers, N.J.; de Vries, P.J.; Delehanty, A.D.; Wetherby, A.M. Feasibility of utilizing autism navigator® for primary care in South Africa. Autism Res. 2018, 11, 1511–1521. [Google Scholar] [CrossRef]
- Makombe, C.B.T.; Shabalala, N.; Viljoen, M.; Seris, N.; de Vries, P.J.; Franz, L. Sustainable implementation of early intervention for autism spectrum disorder through caregiver coaching: South African perspectives on barriers and facilitators. Pediatric Med. 2019, 2, 39. [Google Scholar] [CrossRef]
- StatsSA. Available online: https://statssa.gov.za (accessed on 5 March 2022).
- Peterson, E.R.; Barron, K.A. How to get focus groups talking: New ideas that will Stick. Int. J. Qual. Methods 2007, 6, 140–144. [Google Scholar] [CrossRef]
- Brestan, E.V.; Jacobs, J.R.; Rayfield, A.D.; Eyberg, S.M. A consumer satisfaction measure for parent-child treatments and its relation to measures of child behavior change. Behav. Ther. 1999, 30, 17–30. [Google Scholar] [CrossRef]
- Funderburk, B.W.; Eyberg, S. Parent-child interaction therapy. In History of Psychotherapy: Continuity and Change; Norcross, J.C., VandenBos, G.R., Freedheim, D.K., Eds.; American Psychological Association: Washington, DC, USA, 2011; pp. 415–420. [Google Scholar] [CrossRef]
- Ritchie, J.; Spencer, L. Qualitative data analysis for applied policy research. In Analysing Qualitative Data; Bryman, B., Burgess, R., Eds.; Routledge: London, UK; New York, NY, USA, 1994; pp. 173–194. [Google Scholar]
- Parkinson, S.; Eatough, V.; Holmes, J.; Stapley, E.; Midgley, N. Framework analysis: A worked example of a study exploring young people’s experiences of depression. Qual. Res. Psychol. 2016, 13, 109–129. [Google Scholar] [CrossRef] [Green Version]
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 2013, 13, 117. [Google Scholar] [CrossRef] [Green Version]
- Keith, R.E.; Crosson, J.C.; O’Malley, A.S.; Cromp, D.; Taylor, E.F. Using the Consolidated Framework for Implementation Research (CFIR) to produce actionable findings: A rapid-cycle evaluation approach to improving implementation. Implement. Sci. 2017, 12, 15. [Google Scholar] [CrossRef] [Green Version]
- Chaffin, M.; Silovsky, J.F.; Funderburk, B.; Valle, L.A.; Brestan, E.V.; Balachova, T.; Bonner, B.L. Parent-child interaction therapy with physically abusive parents: Efficacy for reducing future abuse reports. J. Consult. Clin. Psychol. 2004, 72, 500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masse, J.J.; McNeil, C.B.; Wagner, S.; Quetsch, L.B. Examining the efficacy of parent-child interaction therapy with children on the autism spectrum. J. Child Fam. Stud. 2016, 25, 2508–2525. [Google Scholar] [CrossRef]
- Carroll, C.; Patterson, M.; Wood, S.; Booth, A.; Rick, J.; Balain, S. A conceptual framework for implementation fidelity. Implement. Sci. 2007, 2, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Breitenstein, S.M.; Gross, D.; Garvey, C.A.; Hill, C.; Fogg, L.; Resnick, B. Implementation fidelity in community-based interventions. Res. Nurs. Health 2010, 33, 164–173. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, M.A.; Eyberg, S.M. Predicting treatment and follow-up attrition in parent-child interaction therapy. J. Abnorm. Child Psychol. 2009, 37, 431–441. [Google Scholar] [CrossRef]
- Fernandez, M.A.; Butler, A.M.; Eyberg, S.M. Treatment outcome for low socioeconomic status African American families in parent-child interaction therapy: A pilot study. Child Fam. Behav. Ther. 2011, 33, 32–48. [Google Scholar] [CrossRef]
- Timmer, S.G.; Urquiza, A.J.; Zebell, N.M.; McGrath, J.M. Parent-child interaction therapy: Application to maltreating parent-child dyads. Child Abus. Negl. 2005, 29, 825–842. [Google Scholar] [CrossRef]
- Agazzi, H.; Tan, S.Y.; Ogg, J.; Armstrong, K.; Kirby, R.S. Does parent-child interaction therapy reduce maternal stress, anxiety, and depression among mothers of children with autism spectrum disorder? Child Fam. Behav. Ther. 2017, 39, 283–303. [Google Scholar] [CrossRef]
- McNeil, C.B.; Hembree-Kigin, T.L. Home-based PCIT: From the lab to the living room. In Parent-Child Interaction Therapy; Springer: Boston, MA, USA, 2010; pp. 413–419. [Google Scholar]
- Gurwitch, R.; PCIT: Parent-Child Interaction Therapy Fact Sheet. National Child Traumatic Stress Network. 2019. Available online: https://www.nctsn.org/sites/default/files/interventions/pcit_general_031419.pdf (accessed on 1 February 2022).
- Peters, D.H.; Bhuiya, A.; Ghaffar, A. Engaging stakeholders in implementation research: Lessons from the Future Health Systems Research Programme experience. Health Res. Policy Syst. 2017, 15, 1–3. [Google Scholar] [CrossRef] [Green Version]
- Chambers, D.A.; Norton, W.E. The adaptome: Advancing the science of intervention adaptation. Am. J. Prev. Med. 2016, 51, S124–S131. [Google Scholar] [CrossRef] [Green Version]
- Fleming, G.E.; Kohlhoff, J.; Morgan, S.; Turnell, A.; Maiuolo, M.; Kimonis, E.R. An effectiveness open trial of internet-delivered parent training for young children with conduct problems living in regional and rural Australia. Behav. Ther. 2021, 52, 110–123. [Google Scholar] [CrossRef] [PubMed]
- Comer, J.S.; Furr, J.M.; Cooper-Vince, C.; Madigan, R.J.; Chow, C.; Chan, P.T.; Eyberg, S.M. Rationale and considerations for the internet-based delivery of parent-child interaction therapy. Cogn. Behav. Pract. 2015, 22, 302–316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gurwitch, R.H.; Salem, H.; Nelson, M.M.; Comer, J.S. Leveraging parent-child interaction therapy and telehealth capacities to address the unique needs of young children during the COVID-19 public health crisis. Psychol. Trauma Theory Pract. Policy 2020, 12, S82. [Google Scholar] [CrossRef] [PubMed]
- Matos, M.; Torres, R.; Santiago, R.; Jurado, M.; Rodríguez, I. Adaptation of parent-child interaction therapy for Puerto Rican families: A preliminary study. Fam. Process. 2006, 45, 205–222. [Google Scholar] [CrossRef] [PubMed]
- Pincus, D.B.; Eyberg, S.M.; Choate, M.L. Adapting parent-child interaction therapy for young children with separation anxiety disorder. Educ. Treat. Child. 2005, 28, 163–181. [Google Scholar]
- Briegel, W. Tailoring parent-child interaction therapy (PCIT) for older children: A case study. Z. Für Kinder-Und Jugendpsychiatrie Und Psychother. 2017, 46, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Petrenko, C.L.; Alto, M.E. Interventions in fetal alcohol spectrum disorders: An international perspective. Eur. J. Med. Genet. 2017, 60, 79–91. [Google Scholar] [CrossRef] [Green Version]
- Gardner, F.; Montgomery, P.; Knerr, W. Transporting evidence-based parenting programs for child problem behavior (age 3–10) between countries: Systematic review and meta-analysis. J. Clin. Child Adolesc. Psychol. 2016, 45, 749–762. [Google Scholar] [CrossRef] [Green Version]
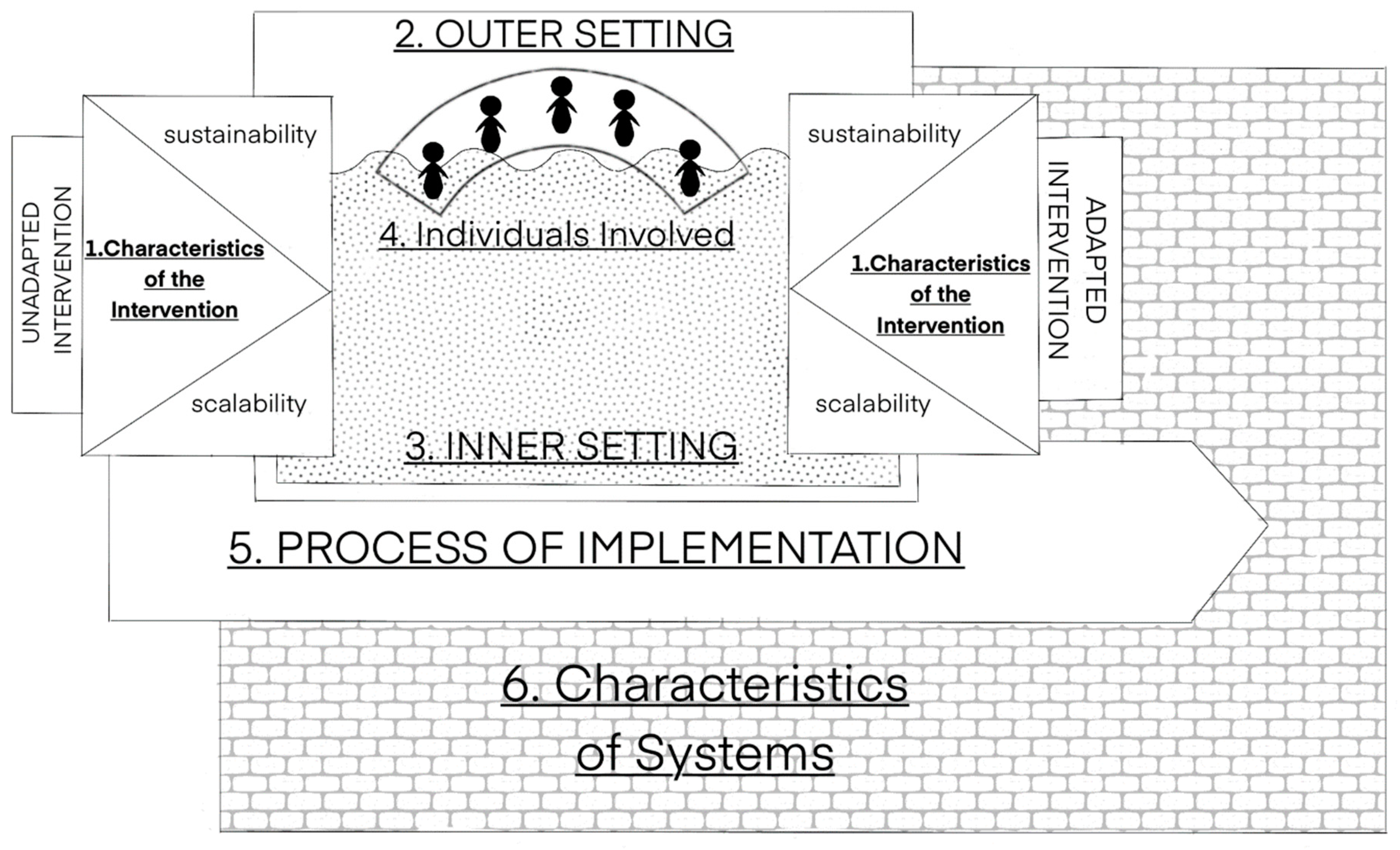

| Construct | Definition | Reference |
|---|---|---|
| Overall Feasibility | The extent to which a new intervention can be used successfully within a given setting, including elements of implementation (e.g., acceptability, fidelity). | Karsh [54] |
| Acceptability | The perceived fit, relevance, or compatibility of an intervention to a particular user, provider, community or setting | Proctor et al. [51] |
| Fidelity | The extent to which an intervention was implemented as it was prescribed in the original protocol or as it was intended by the developers of the programme | Proctor et al. [51] |
| Scalability | The ability of an intervention (shown to be efficacious on a small scale and/or under controlled conditions) to be expanded to reach a greater proportion of the eligible population, while retaining effectiveness in real world conditions | Aarons et al. [55] |
| Caregiver | Age | Gender | Self-Identified Race/Ethnicity | Education | Graduation/Completion |
|---|---|---|---|---|---|
| Participant 1 | 42 | Female | White | Bachelors | Y |
| Participant 2 | 38 | Male | White | Diploma | Y |
| Participant 3 | 39 | Female | Coloured | Less than high school graduation | Y |
| Participant 4 | 39 | Male | Coloured | Less than high school graduation | Y |
| Participant 5 | 41 | Female | White | Bachelors | Y |
| Participant 6 | 45 | Male | White | Bachelors | N |
| Participant 7 | 38 | Female | Coloured | Diploma | Y |
| Participant 8 | 40 | Male | Coloured | Diploma | Y |
| Participant 9 | 36 | Female | Black | Bachelors | N |
| Participant 10 | 56 | Male | White | High school | N |
| Participant 11 | 36 | Female | White | Bachelors | N |
| Participant 12 | 40 | Male | White | Bachelors | N |
| Participant 13 | 37 | Female | White | Bachelors | Y |
| Participant 14 | 40 | Male | White | Diploma | N |
| Domains and Constructs | Therapist Consensus Reflections |
|---|---|
| Domain 1: Characteristics of the Intervention (relating to the quality and features of the intervention) | |
| Evidence Strength and Quality: Perception of the quality and validity of evidence supporting the belief that the intervention will have desired outcomes |
|
| Relative Advantage: Perception of the advantage of implementing the intervention versus an alternative solution |
|
| Adaptability: Degree to which an intervention can be tailored to meet the needs of an organization |
|
| Complexity: Perceived difficulty of implementation |
|
| Perceived scalability |
|
| Perceived sustainability |
|
| Domain 2: Outer Setting (referring to the economic, political and social contexts where the tertiary level hospital resides) | |
| Patient Needs and Resources: Extent to which patient needs are accurately known and prioritized by the organization |
|
| Cosmopolitanism: Level of connectedness and networks with other organizations |
|
| Domain 3: Inner Setting (refers to the structural, political and cultural contexts where the implementation will take place, e.g., the hospital, department group of people) |
|
| Domain 4: Individuals involved in implementation (referring to those involved in implementing the intervention) | |
| Knowledge and Beliefs about Intervention: Individual staff knowledge and attitude towards the intervention |
|
| Domain 5: Process of implementation (referring, though not limited to, the planning around implementation and execution of that plan) |
|
| Domain 6: Characteristics of systems (referring to the relationship between key systems characteristics and implementation) |
|
| Domains and Constructs | Therapist Consensus Reflections |
|---|---|
| Domain 1 Characteristics of the Intervention (relating to the quality and features of the intervention) | |
| Evidence Strength and Quality: Perception of the quality and validity of evidence supporting the belief that the intervention will have desired outcomes |
|
| Relative Advantage: Perception of the advantage of implementing the intervention versus an alternative solution |
|
| Adaptability: Degree to which an intervention can be tailored to meet the needs of an organization |
|
| Complexity: Perceived difficulty of implementation |
|
| Cost: Cost of the intervention and costs associated with implementing the intervention |
|
| Perceived scalability |
|
| Perceived sustainability |
|
| Domain 2: Outer Setting (referring to the economic, political and social contexts where the tertiary level hospital resides) | |
| Cosmopolitanism: Level of connectedness and networks with other organizations |
|
| Domain 3: Inner Setting (refers to the structural, political and cultural contexts where the implementation will take place, e.g., the hospital, department, group of people) | |
| Implementation climate: Relative priority of implementing the current intervention versus other competing priorities |
|
| Readiness for Implementation: Access to resources, knowledge, and information about the intervention |
|
| Domain 4: Individuals involved in implementation (referring to those involved in implementing the intervention) | |
| Self-efficacy: An individual’s belief in their capabilities to execute the implementation |
|
| Domain 5: Process of implementation (referring, though not limited to, the planning around implementation and execution of that plan) |
|
| Domain 6: Characteristics of systems (referring to the relationship between key systems characteristics and implementation) |
|
| Adaptations |
| Creation of a “PCIT hub” |
| Expansion of PCIT in South Africa |
| Increase access |
| Increase awareness |
| Research |
| Sustainable funding |
| Training (trainers and universities) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dawson-Squibb, J.-J.; Davids, E.L.; Chase, R.; Puffer, E.; Rasmussen, J.D.M.; Franz, L.; de Vries, P.J. Bringing Parent–Child Interaction Therapy to South Africa: Barriers and Facilitators and Overall Feasibility—First Steps to Implementation. Int. J. Environ. Res. Public Health 2022, 19, 4450. https://doi.org/10.3390/ijerph19084450
Dawson-Squibb J-J, Davids EL, Chase R, Puffer E, Rasmussen JDM, Franz L, de Vries PJ. Bringing Parent–Child Interaction Therapy to South Africa: Barriers and Facilitators and Overall Feasibility—First Steps to Implementation. International Journal of Environmental Research and Public Health. 2022; 19(8):4450. https://doi.org/10.3390/ijerph19084450
Chicago/Turabian StyleDawson-Squibb, John-Joe, Eugene Lee Davids, Rhea Chase, Eve Puffer, Justin D. M. Rasmussen, Lauren Franz, and Petrus J. de Vries. 2022. "Bringing Parent–Child Interaction Therapy to South Africa: Barriers and Facilitators and Overall Feasibility—First Steps to Implementation" International Journal of Environmental Research and Public Health 19, no. 8: 4450. https://doi.org/10.3390/ijerph19084450
APA StyleDawson-Squibb, J.-J., Davids, E. L., Chase, R., Puffer, E., Rasmussen, J. D. M., Franz, L., & de Vries, P. J. (2022). Bringing Parent–Child Interaction Therapy to South Africa: Barriers and Facilitators and Overall Feasibility—First Steps to Implementation. International Journal of Environmental Research and Public Health, 19(8), 4450. https://doi.org/10.3390/ijerph19084450






