A Case Study about Joining Databases for the Assessment of Exposures to Noise and Ototoxic Substances in Occupational Settings
Abstract
:1. Introduction
- SUMER provides the number and proportion of workers exposed to different nuisances for different jobs and/or occupational sectors.
- COLCHIC and SCOLA provide the intensity and/or the duration and/or the frequency of exposure to chemical substances.
- AMELI provides the yearly disease burden: the number and proportion of workers having declared an occupational disease during each calendar year.
2. Materials and Methods
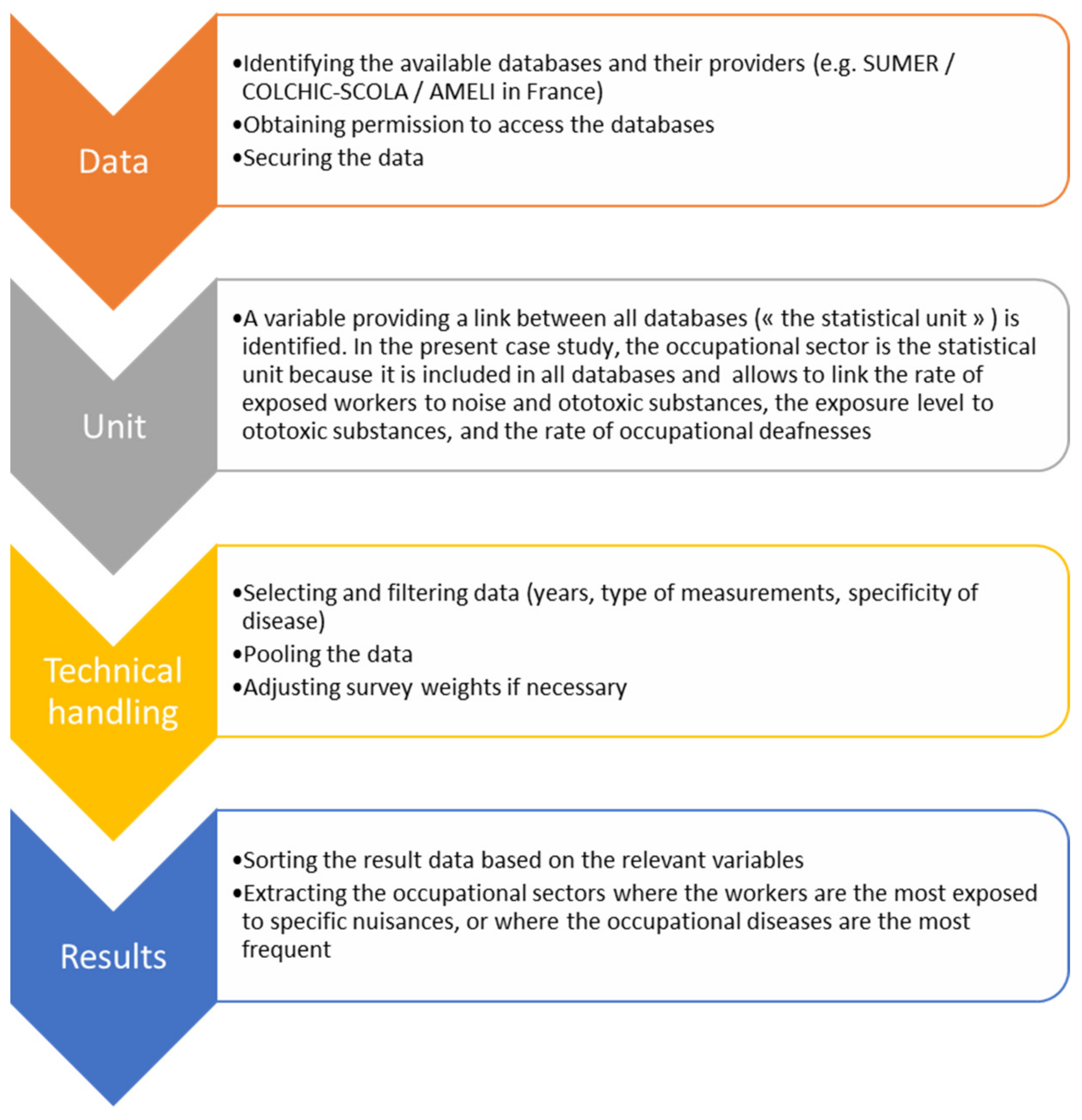
2.1. Overview of the Proposed Methodology and the Choice of Ototoxic Substances
2.2. Step 1: What Are the Prerequisites and the Things to Know and to Do in Order to Obtain Access to Relevant Data?
- SUMER is a survey conducted every 6 or 7 years by the French Ministry of Labor. Occupational physicians collect a vast amount of data regarding workers from all occupations in France. Access to SUMER data has required a partnership. These data allow (among other things) the identification of workers exposed to noise and ototoxic substances per occupational sector. Data from the last three surveys were pooled, adjusted and used. Around 1500 variables were collected. A total of 50,000 individuals were surveyed in 2003, 48,000 in 2010 and 26,000 in 2017. These data are representative of the whole French workforce.
- COLCHIC and SCOLA are national databases hosted by the French National Occupational Health and Safety Institute (INRS), containing about 1,500,000 measurements of chemical substances at the workplace. Among these measurements collected by occupational hygienists from French public health insurance and privately held laboratories in charge of regulatory controls, the levels of exposure to eight ototoxic substances per occupational sector were extracted. Lead, styrene, toluene, n-hexane, trichloroethylene, arsenic and cobalt were selected because data were available in COLCHIC, SCOLA and SUMER, and because these substances have ototoxic properties demonstrated or suspected in humans.
- AMELI is a website edited by French public health insurance in which the number of cases of occupational hearing loss (among other pathologies) per occupational sector is provided as open data.
- Finally, the French national statistics institute (INSEE) provides the number of workers per occupational sector, also as open data.
2.3. Step 2: Identify or Build a Common Variable, Which Can Be Used to Link All Databases (the “Statistical Unit”)
2.4. Step 4: What Are the Specific Issues for the Technical Handling of the Data (Filtering, Selecting, Adjustment When Considering Survey Data, Pooling)?
2.5. Step 5: The Type of Indicators Used for Communicating the Results Is Easy to Design but Is Difficult to Synthesize
3. Results: A Case Study Assessing the Multiple Exposure to Noise and Ototoxic Substances
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- OECD. Considerations for Assessing the Risks of Combined Exposure to Multiple Chemicals. 2018, p. 296. Available online: http://www.oecd.org/chemicalsafety/risk-assessment/considerations-for-assessing-the-risks-of-combined-exposure-to-multiple-chemicals.pdf (accessed on 2 December 2021).
- ECHA. Guidance on Assessment of Multiple Simultaneous Exposure Routes of PT21 Active Substances. 2013. Available online: https://echa.europa.eu/documents/10162/16908203/pt21_guidance_multiple_simultaneous_exposure_routes_en.pdf/3f2e6f8b-0c02-4c6b-a5f9-67c9f7d17f56 (accessed on 2 December 2021).
- Nguyen, T.-H.-Y.; Bertin, M.; Bodin, J.; Fouquet, N.; Bonvallot, N.; Roquelaure, Y. Multiple Exposures and Coexposures to Occupational Hazards Among Agricultural Workers: A Systematic Review of Observational Studies. Saf. Health Work 2018, 9, 239–248. [Google Scholar] [CrossRef] [PubMed]
- Bertin, M.; Nguyen, T.-H.-Y.; Bonvallot, N.; Bodin, J.; Roquelaure, Y. Occupational co-exposure to biomechanical factors and neurotoxic chemicals in a representative sample of French employees. J. Occup. Health 2020, 62, e12090. [Google Scholar] [CrossRef] [PubMed]
- Févotte, J.; Dananché, B.; Delabre, L.; Ducamp, S.; Garras, L.; Houot, M.; Luce, D.; Orlowski, E.; Pilorget, C.; Lacourt, A.; et al. Matgéné: A program to develop job-exposure matrices in the general population in France. Ann. Occup. Hyg. 2011, 55, 865–878. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonneterre, V.; Mathern, G.; Pelen, O.; Balthazard, A.-L.; Delafosse, P.; Mitton, N.; Colonna, M. Cancer incidence in a chlorochemical plant in Isère, France: An occupational cohort study, 1979–2002. Am. J. Ind. Med. 2012, 55, 756–767. [Google Scholar] [CrossRef] [PubMed]
- Bertrais, S.; André, N.; Bèque, M.; Chastang, J.-F.; Niedhammer, I. Associations between multiple occupational exposures and sleep problems: Results from the national French Working Conditions survey. J. Sleep Res. 2021, 30, e13101. [Google Scholar] [CrossRef]
- Gardner, R. Overview and Characteristics of Some Occupational Exposures and Health Risks on Offshore Oil and Gas Installations. Ann. Occup. Hyg. 2003, 47, 201–210. [Google Scholar] [CrossRef] [Green Version]
- Labrèche, F.; Kim, J.; Song, C.; Pahwa, M.; Ge, C.B.; Arrandale, V.H.; McLeod, C.B.; Peters, C.E.; Lavoué, J.; Davies, H.W.; et al. The current burden of cancer attributable to occupational exposures in Canada. Prev. Med. 2019, 122, 128–139. [Google Scholar] [CrossRef]
- Stamm, R. MEGA-Database: One million data since 1972. Appl. Occup. Environ. Hyg. 2000, 16, 159–163. [Google Scholar] [CrossRef]
- Lavoué, J.; Friesen, M.C.; Burstyn, I. Workplace Measurements by the US Occupational Safety and Health Administration since 1979: Descriptive Analysis and Potential Uses for Exposure Assessment. Ann. Occup. Hyg. 2013, 57, 77–97. [Google Scholar]
- Mater, G.; Paris, C.; Lavoué, J. Descriptive analysis and comparison of two French occupational exposure databases: COLCHIC and SCOLA. Am. J. Ind. Med. 2016, 59, 379–391. [Google Scholar] [CrossRef] [Green Version]
- ISPESL. Vibration Database—PAF—Physical Agents Portal. Available online: https://www.portaleagentifisici.it/index.php?lg=EN (accessed on 26 July 2021).
- SUVA. Liste des Tableaux de Niveaux Sonores. 2020. Available online: https://www.suva.ch/fr-ch/prevention/themes-specialises/bruit-et-vibrations#uxlibrary-material=8d7ca881a1cb4564ba03758db23fcd3f&uxlibrary-material-filter=materialGroup:all&uxlibrary-open=/fr-CH?atomid=8d7ca881a1cb4564ba03758db23fcd3f%26showContainer=1 (accessed on 20 January 2021).
- Sanli, O.; Dobruch, J.; Knowles, M.A.; Burger, M.; Alemozaffar, M.; Nielsen, M.E.; Lotan, Y. Bladder cancer. Nat. Rev. Dis. Primers 2017, 3, 17022. [Google Scholar] [CrossRef] [PubMed]
- Alpert, N.; van Gerwen, M.; Taioli, E. Epidemiology of mesothelioma in the 21st century in Europe and the United States, 40 years after restricted/banned asbestos use. Transl. Lung Cancer Res. 2020, 9, S28–S38. [Google Scholar] [CrossRef] [PubMed]
- Raulf, M. Allergen component analysis as a tool in the diagnosis and management of occupational allergy. Mol. Immunol. 2018, 100, 21–27. [Google Scholar] [CrossRef]
- Patel, S.; Zhou, C.; Rattan, S.; Flaws, J.A. Effects of Endocrine-Disrupting Chemicals on the Ovary. Biol. Reprod. 2015, 93, 20. [Google Scholar] [CrossRef] [PubMed]
- Campo, P.; Morata, T.C.; Hong, O. Chemical exposure and hearing loss. Dis. Mon. 2013, 59, 119–138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Occupational Safety and Health Administration. Preventing Hearing Loss Caused by Chemical (Ototoxicity) and Noise Exposure. Available online: https://www.osha.gov/publications/shib030818 (accessed on 28 September 2021).
- Johnson, A.C.; Morata, T.C.; The Nordic Expert Group for Criteria Documentation of Health Risks from Chemicals. 142. Occupational Exposure to Chemicals and Hearing Impairment; Arbete och Hälsa, University of Gothenburg: Gothenburg, Sweden, 2010; Volume 44, p. 177. [Google Scholar]
- Venet, T.; Campo, P.; Thomas, A.; Cour, C.; Rieger, B.; Cosnier, F. The tonotopicity of styrene-induced hearing loss depends on the associated noise spectrum. Neurotoxicol. Teratol. 2015, 48, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Sliwińska-Kowalska, M.; Bilski, B.; Zamysłowska-Szmytke, E.; Kotyło, P.; Fiszer, M.; Wesołowski, W.; Pawlaczyk-Łuszczyńska, M.; Kucharska, M.; Dudarewicz, A. Hearing impairment in the plastics industry workers exposed to styrene and noise. Med. Pr. 2001, 52, 297–303. [Google Scholar]
- Coates-Verley, L.; Wathier, L.; Pouyatos, B. Ototoxicité des métaux. Ref. Sante Trav. 2021, 165, 13–31. [Google Scholar]
- Sécurité Sociale Rapport de la Comission Instituée par L’article L. 176-2 du Code de la Sécurité Sociale 2014. Available online: https://www.securite-sociale.fr/files/live/sites/SSFR/files/medias/DSS/2017/RAPPORT/DSS-2017-RAPPORT-RAPPORT_SUR_LA_SOUS_DECLARATION_DES_AT-MP.pdf (accessed on 2 December 2021).
- Cheng, W.; Roberts, B.; Mukherjee, B.; Neitzel, R.L. Meta-analysis of job-exposure matrix data from multiple sources. J. Expo. Sci. Environ. Epidemiol. 2018, 28, 259–274. [Google Scholar] [CrossRef]
- Van Tongeren, M.; Jimenez, A.S.; Hutchings, S.J.; MacCalman, L.; Rushton, L.; Cherrie, J.W. Occupational cancer in Britain. Exposure assessment methodology. Br. J. Cancer 2012, 107, S18–S26. [Google Scholar] [CrossRef] [Green Version]
- Hai, R.; Quix, C.; Jarke, M. Data lake concept and systems: A survey. arXiv 2021, arXiv:2106.09592. [Google Scholar]
| SUMER | COLCHIC/SCOLA | CNAM | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Occupational Sector | Number of Workers in the Occ. Sect. | % of Workers Exposed to Noise and Ototoxic Substances | % of Workers Exposed to Ototoxic Substances Only | % of Workers Oxposed to Noise Only | % of Workers Neither Exposed to Noise nor Ototoxic Substances | Number of Measurements of Ototoxic Substances Available | % of Measurements of Ototoxic Substances above OELV | Number of Occup. Hearing loss for 100,000 Workers | Number of Occ. Hearing Loss in the Occ. Sect. Divided by nb of Overall Hearing Loss (per 100,000 Workers) |
| Manufacture of products of wood, cork, straw and plaiting materials | 45,500 | 1.2% | 1.7% | 64.9% | 33.4% | 290 | 32% | 13.9 | 4.4 |
| Demolition and site preparation | 85,200 | 1.2% | 1.5% | 63.8% | 34.7% | 223 | 32% | 13.1 | 4.2 |
| Forging, pressing, stamping and roll-forming of metal: powder metallurgy | 38,900 | 5.6% | 7.4% | 59.9% | 32.7% | 199 | 38% | 23.3 | 7.4 |
| Construction of utility projects | 61,900 | 1.4% | 1.4% | 55.1% | 43.5% | 37 | 28% | 23.1 | 7.4 |
| Other specialised construction activities | 334,600 | 5.6% | 7.1% | 54.4% | 38.5% | 230 | 53% | 10.8 | 3.4 |
| Repair of fabricated metal products, machinery and equipment | 74,200 | 3.7% | 6.5% | 52.8% | 40.6% | 133 | 13% | 23.6 | 7.5 |
| Construction of residential and non-residential buildings | 130,300 | 1.6% | 2.1% | 48.0% | 49.8% | 85 | 29% | 14.8 | 4.7 |
| Building completion and finishing | 331,200 | 4.3% | 7.0% | 47.0% | 46.0% | 369 | 35% | 7.3 | 2.3 |
| Treatment and coating of metals: machining | 107,900 | 9.2% | 12.2% | 46.7% | 41.1% | 552 | 23% | 18.7 | 6.0 |
| Electrical, plumbing and other construction installation activities | 374,700 | 5.2% | 6.5% | 38.3% | 55.2% | 71 | 31% | 25.4 | 8.1 |
| SUMER | COLCHIC/SCOLA | CNAM | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Occupational Sector | Number of Workers in the Occ. Sect. | % of Workers Exposed to Noise and Ototoxic Substances | % of Workers Exposed to Ototoxic Substances Only | % of Workers Oxposed to Noise Only | % of Workers Neither Exposed to Noise nor Ototoxic Substances | Number of Measurements of Ototoxic Substances Available | % of Measurements of Ototoxic Substances above OELV | Number of Occup. Hearing Loss for 100,000 Workers | Nb of Occ. Hearing Loss in the Occ. Sect. Divided by nb of Overall Hearing Loss (per 100,000 Workers) |
| Manufacture of medical and dental instruments and supplies | 45,800 | 8.4% | 23.3% | 4.8% | 71.9% | 547 | 31.6% | 2.2 | 0.7 |
| Maintenance and repair of motor vehicles | 118,500 | 11.1% | 15.4% | 30.0% | 54.6% | 497 | 52.3% | 8.3 | 2.6 |
| Manufacture of other chemical products | 23,900 | 8.3% | 15.1% | 20.2% | 64.7% | 379 | 18.0% | 7.0 | 2.2 |
| Manufacture of basic chemicals, fertilisers and nitrogen compounds, plastics and synthetic rubber in primary forms | 48,400 | 7.8% | 12.3% | 29.7% | 58.0% | 555 | 13.4% | 9.6 | 3.1 |
| Treatment and coating of metals: machining | 107,900 | 9.2% | 12.2% | 46.7% | 41.1% | 552 | 22.8% | 18.7 | 6.0 |
| Manufacture of electronic components and boards | 47,600 | 2.7% | 11.2% | 10.1% | 78.7% | 131 | 13.0% | 1.1 | 0.3 |
| Sale of motor vehicle parts and accessories | 67,000 | 5.3% | 11.0% | 21.1% | 67.9% | 54 | 45.0% | 3.7 | 1.2 |
| Sale of motor vehicles | 176,300 | 8.2% | 10.9% | 21.0% | 68.1% | 154 | 28.6% | 5.2 | 1.7 |
| Other specialised construction activities | 334,600 | 5.6% | 7.1% | 54.4% | 38.5% | 230 | 53.2% | 10.8 | 3.4 |
| Building completion and finishing | 331,200 | 4.3% | 7.0% | 47.0% | 46.0% | 369 | 34.7% | 7.3 | 2.3 |
| Occupational Sector | Number of Workers in the Occ. Sect. | % of Workers Exposed to Noise and Ototoxic Substances | % of Workers Exposed to Ototoxic Substances Only | % of Workers Oxposed to Noise Only | % of Workers Neither Exposed to Noise nor Ototoxic Substances | Number of Measurements of Ototoxic Substances Available | % of Measurements of Ototoxic Substances above OELV | Number of Occup. Hearing Loss for 100,000 Workers | Nb of Occ. Hearing Loss in the Occ. Sect. Divided by nb of Overall Hearing Loss (per 100,000 Workers) |
|---|---|---|---|---|---|---|---|---|---|
| Maintenance and repair of motor vehicles | 118,500 | 11.1% | 15.4% | 30.0% | 54.6% | 497 | 52.3% | 8.3 | 2.6 |
| Treatment and coating of metals: machining | 107,900 | 9.2% | 12.2% | 46.7% | 41.1% | 552 | 22.8% | 18.7 | 6.0 |
| Manufacture of medical and dental instruments and supplies | 45,800 | 8.4% | 23.3% | 4.8% | 71.9% | 547 | 31.6% | 2.2 | 0.7 |
| Manufacture of other chemical products | 23,900 | 8.3% | 15.1% | 20.2% | 64.7% | 379 | 18.0% | 7.0 | 2.2 |
| Sale of motor vehicles | 176,300 | 8.2% | 10.9% | 21.0% | 68.1% | 154 | 28.6% | 5.2 | 1.7 |
| Manufacture of basic chemicals, fertilisers and nitrogen compounds, plastics and synthetic rubber in primary forms | 48,400 | 7.8% | 12.3% | 29.7% | 58.0% | 555 | 13.4% | 9.6 | 3.1 |
| Printing and service activities related to printing | 68,900 | 7.7% | 10.2% | 20.5% | 69.4% | 474 | 23.1% | 6.0 | 1.9 |
| Other specialised construction activities | 334,600 | 5.6% | 7.1% | 54.4% | 38.5% | 230 | 53.2% | 10.8 | 3.4 |
| Sale of motor vehicle parts and accessories | 67,000 | 5.3% | 11.0% | 21.1% | 67.9% | 54 | 45.0% | 3.7 | 1.2 |
| Electrical, plumbing and other construction installation activities | 374,700 | 5.2% | 6.5% | 38.3% | 55.2% | 71 | 31.3% | 4.5 | 1.4 |
| SUMER | COLCHIC/SCOLA | CNAM | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Occupational Sector | Number of Workers in the Occ. Sect. | % of Workers Exposed to Noise and Ototoxic Substances | % of Workers Exposed to Ototoxic Substances Only | % of Workers Oxposed to Noise Only | % of Workers Neither Exposed to Noise nor Ototoxic Substances | Number of Measurements of Ototoxic Substances Available | % of Measurements of Ototoxic Substances above OELV | Number of Occup. Hearing Loss for 100,000 Workers | Nb of Occ. Hearing Loss in the Occ. Sect. Divided by nb of Overall Hearing Loss (per 100,000 Workers) |
| Residential nursing care activities | 112,000 | 0.0% | 0.0% | 0.0% | 100% | 0 | - | 0.4 | 0.1 |
| Monetary intermediation | 315,400 | 0.0% | 0.0% | 0.2% | 100% | 0 | - | 0.0 | - |
| Accounting, bookkeeping and auditing activities: tax consultancy | 310,100 | 0.1% | 0.2% | 0.4% | 99% | 8 | - | 0.0 | - |
| Hotels and similar accommodation | 135,900 | 0.1% | 0.1% | 0.6% | 99% | 0 | - | 0.2 | 0.1 |
| Management consultancy activities | 152,900 | 0.1% | 0.3% | 0.5% | 99% | 8 | - | 0.1 | - |
| Insurance, reinsurance and pension funding, except compulsory social security | 656,300 | 0.0% | 0.3% | 0.9% | 99% | 2 | - | 0.1 | - |
| Social work activities without accommodation for the elderly and disabled | 245,600 | 0.0% | 0.1% | 1.4% | 99% | 0 | - | 0.4 | 0.1 |
| Other human health activities | 169,400 | 0.1% | 0.5% | 1.7% | 98% | 9 | - | 0.0 | - |
| Hospital activities | 523,100 | 0.2% | 0.7% | 1.5% | 98% | 9 | - | 0.3 | 0.1 |
| Other social work activities without accommodation | 556,300 | 0.0% | 0.1% | 2.6% | 97% | 0 | - | 0.2 | 0.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clerc, F.; Pouyatos, B. A Case Study about Joining Databases for the Assessment of Exposures to Noise and Ototoxic Substances in Occupational Settings. Int. J. Environ. Res. Public Health 2022, 19, 4455. https://doi.org/10.3390/ijerph19084455
Clerc F, Pouyatos B. A Case Study about Joining Databases for the Assessment of Exposures to Noise and Ototoxic Substances in Occupational Settings. International Journal of Environmental Research and Public Health. 2022; 19(8):4455. https://doi.org/10.3390/ijerph19084455
Chicago/Turabian StyleClerc, Frédéric, and Benoit Pouyatos. 2022. "A Case Study about Joining Databases for the Assessment of Exposures to Noise and Ototoxic Substances in Occupational Settings" International Journal of Environmental Research and Public Health 19, no. 8: 4455. https://doi.org/10.3390/ijerph19084455






