The Association between Childhood Exposure to Ambient Air Pollution and Obesity: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Methods
2.1. Search Strategy
2.2. Eligibility Criteria and Study Selection
2.3. Data Extraction and Quality Assessment
2.4. Data Synthesis and Statistical Analysis
3. Results
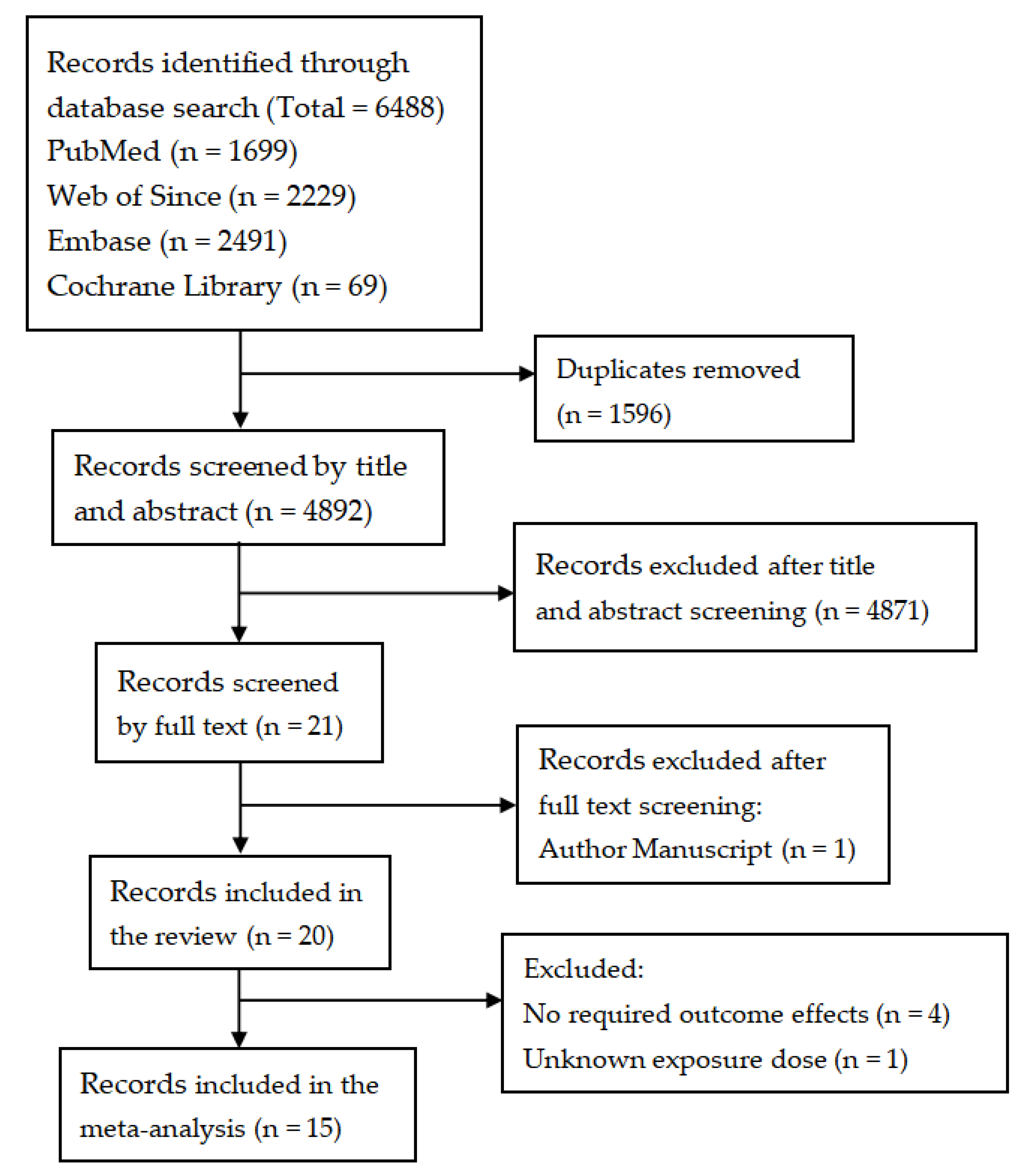
3.1. Study Selection
3.2. Study Characteristics
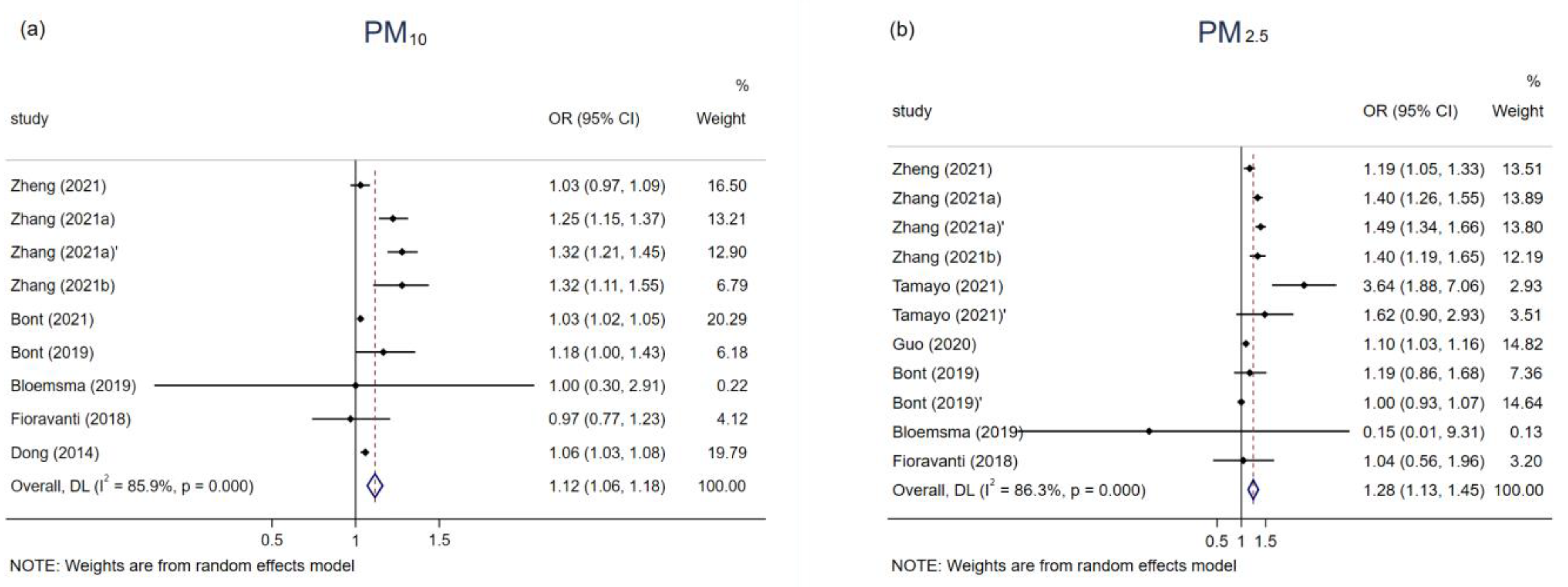
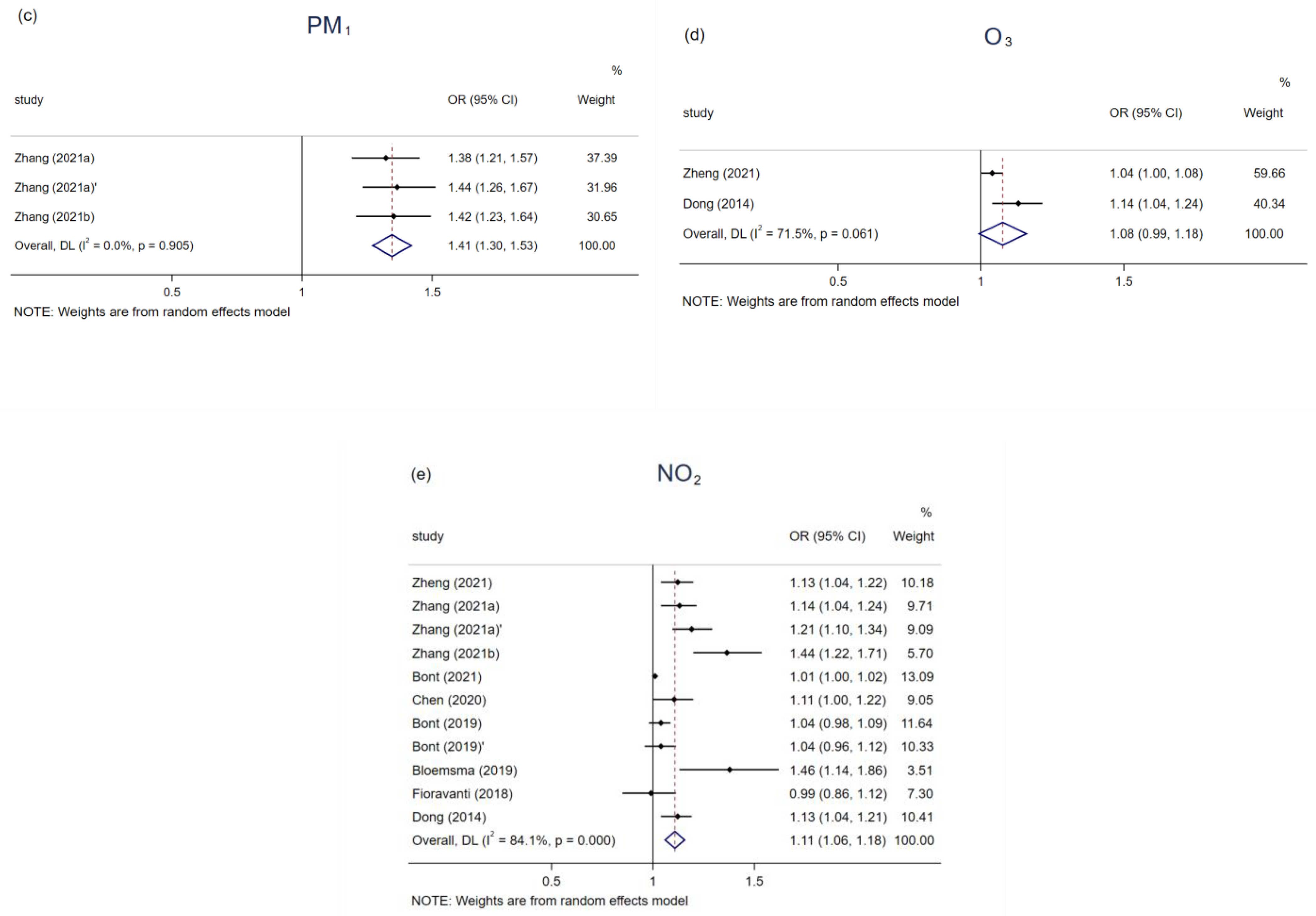
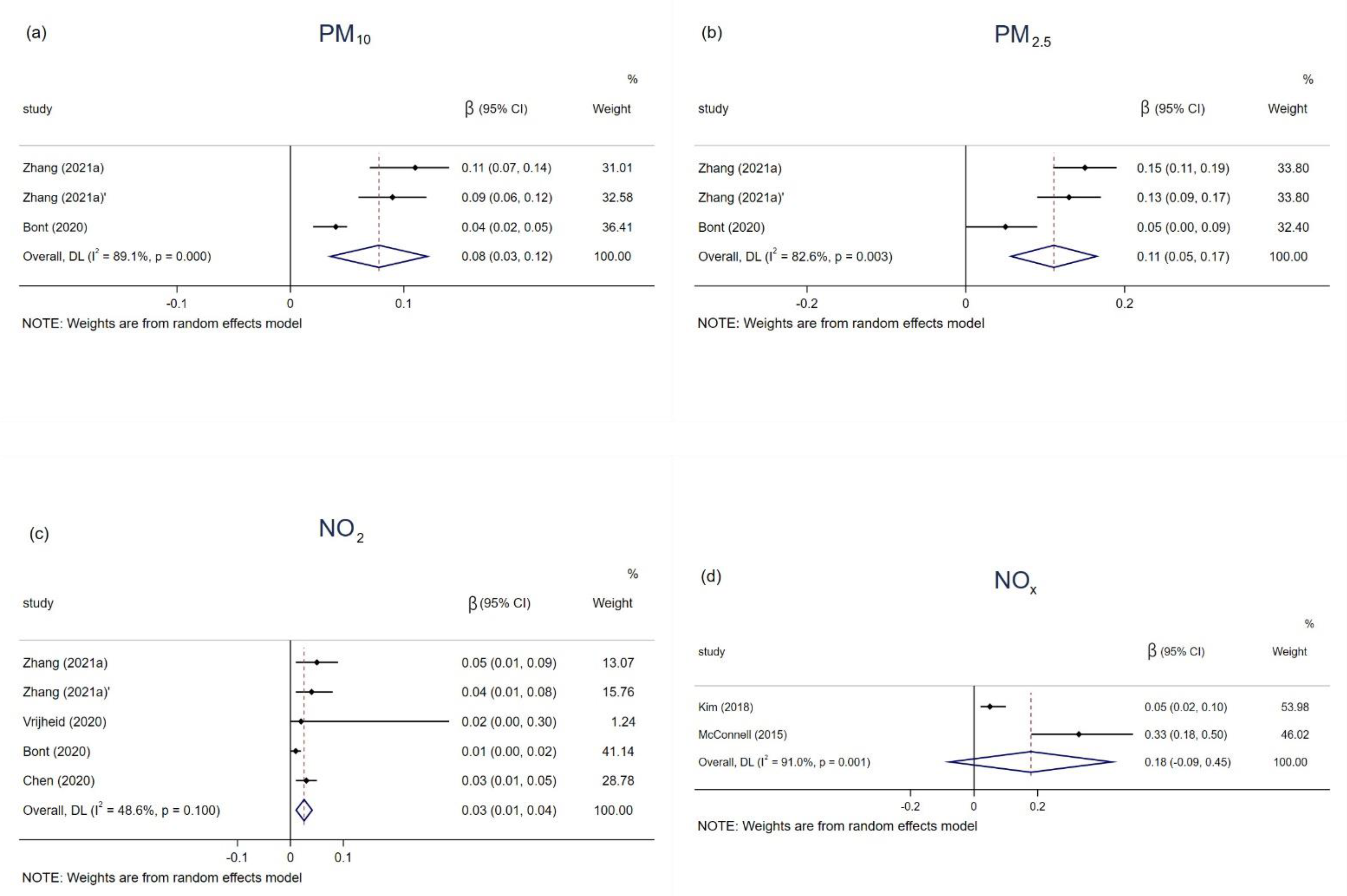
3.3. Air Pollution on Obesity and BMI in Children and Adolescents
3.4. Heterogeneity, Publication Bias, and Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ezzati, M.; Bentham, J.; Di Cesare, M.; Bilano, V.; Bixby, H.; Zhou, B.; Stevens, G.A.; Riley, L.M.; Taddei, C.; Hajifathalian, K.; et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar]
- WHO. Obesity and Overweight; World Health Organizaiton: Geneva, Switzerland, 2020.
- Afshin, A.; Forouzanfar, M.H.; Reitsma, M.B.; Sur, P.; Estep, K.; Lee, A.; Marczak, L.; Mokdad, A.H.; Moradi-Lakeh, M.; Naghavi, M.; et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [PubMed]
- Wormser, D.; Kaptoge, S.; Di Angelantonio, E.; Wood, A.M.; Pennells, L.; Thompson, A.; Sarwar, N.; Kizer, J.R.; Lawlor, D.A.; Nordestgaard, B.G.; et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: Collaborative analysis of 58 prospective studies. Lancet 2011, 377, 1085–1095. [Google Scholar] [PubMed] [Green Version]
- Singh, G.M.; Danaei, G.; Farzadfar, F.; Stevens, G.A.; Woodward, M.; Wormser, D.; Kaptoge, S.; Whitlock, G.; Qiao, Q.; Lewington, S.; et al. The age-specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes: A pooled analysis. PLoS ONE 2013, 8, e65174. [Google Scholar] [CrossRef] [PubMed]
- Simmonds, M.; Llewellyn, A.; Owen, C.G.; Woolacott, N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2016, 17, 95–107. [Google Scholar] [CrossRef] [Green Version]
- Han, J.C.; Lawlor, D.A.; Kimm, S.Y. Childhood obesity. Lancet 2010, 375, 1737–1748. [Google Scholar] [CrossRef]
- Jerrett, M.; McConnell, R.; Wolch, J.; Chang, R.; Lam, C.; Dunton, G.; Gilliland, F.; Lurmann, F.; Islam, T.; Berhane, K. Traffic-related air pollution and obesity formation in children: A longitudinal, multilevel analysis. Environ. Health 2014, 13, 49. [Google Scholar] [CrossRef] [Green Version]
- Cohen, A.J.; Brauer, M.; Burnett, R.; Anderson, H.R.; Frostad, J.; Estep, K.; Balakrishnan, K.; Brunekreef, B.; Dandona, L.; Dandona, R.; et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: An analysis of data from the Global Burden of Diseases Study 2015. Lancet 2017, 389, 1907–1918. [Google Scholar] [CrossRef] [Green Version]
- United States Environmental Protection Agency. Criteria Air Pollutants. EPA; 2017. Available online: https://www.epa.gov/criteria-air-pollutants (accessed on 1 March 2022).
- WHO. Global Urban Ambient Air Pollution Database; WHO: Geneva, Switzerland, 2016.
- An, R.; Ji, M.; Yan, H.; Guan, C. Impact of ambient air pollution on obesity: A systematic review. Int. J. Obes. 2018, 42, 1112–1126. [Google Scholar] [CrossRef]
- Xu, Z.; Xu, X.; Zhong, M.; Hotchkiss, I.P.; Lewandowski, R.P.; Wagner, J.G.; Bramble, L.A.; Yang, Y.; Wang, A.; Harkema, J.R.; et al. Ambient particulate air pollution induces oxidative stress and alterations of mitochondria and gene expression in brown and white adipose tissues. Part. Fibre Toxicol. 2011, 8, 20. [Google Scholar] [CrossRef] [Green Version]
- Sun, Q.; Yue, P.; Deiuliis, J.A.; Lumeng, C.N.; Kampfrath, T.; Mikolaj, M.B.; Cai, Y.; Ostrowski, M.C.; Lu, B.; Parthasarathy, S.; et al. Ambient air pollution exaggerates adipose inflammation and insulin resistance in a mouse model of diet-induced obesity. Circulation 2009, 119, 538–546. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keith, S.W.; Redden, D.T.; Katzmarzyk, P.T.; Boggiano, M.M.; Hanlon, E.C.; Benca, R.M.; Ruden, D.; Pietrobelli, A.; Barger, J.L.; Fontaine, K.R.; et al. Putative contributors to the secular increase in obesity: Exploring the roads less traveled. Int. J. Obes. 2006, 30, 1585–1594. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, L.; Zhu, L.; Xu, Y.; Lyu, J.; Imm, K.; Yang, L. Relationship Between Air Quality and Outdoor Exercise Behavior in China: A Novel Mobile-Based Study. Int. J. Behav. Med. 2017, 24, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Neidell, M. Information, Avoidance Behavior, and Health The Effect of Ozone on Asthma Hospitalizations. J. Hum. Resour. 2009, 44, 450–478. [Google Scholar] [CrossRef] [Green Version]
- Alderete, T.L.; Habre, R.; Toledo-Corral, C.M.; Berhane, K.; Chen, Z.; Lurmann, F.W.; Weigensberg, M.J.; Goran, M.I.; Gilliland, F.D. Longitudinal Associations Between Ambient Air Pollution With Insulin Sensitivity, β-Cell Function, and Adiposity in Los Angeles Latino Children. Diabetes 2017, 66, 1789–1796. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.C.; Chen, P.C.; Hsieh, W.S.; Portnov, B.A.; Chen, Y.A.; Lee, Y.L. Environmental factors associated with overweight and obesity in taiwanese children. Paediatr. Perinat. Epidemiol. 2012, 26, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.; Xu, Z.; Wang, Q.; Ding, Z.; Zhou, L.; Xu, Y.; Su, H.; Li, X.; Zhang, F.; Cheng, J. Long-term exposure to ambient air pollution and obesity in school-aged children and adolescents in Jiangsu province of China. Environ. Res. 2021, 195, 110804. [Google Scholar] [CrossRef]
- Zhang, Z.; Dong, B.; Chen, G.; Song, Y.; Li, S.; Yang, Z.; Dong, Y.; Wang, Z.; Ma, J.; Guo, Y. Ambient air pollution and obesity in school-aged children and adolescents: A multicenter study in China. Sci. Total Environ. 2021, 771, 144583. [Google Scholar] [CrossRef]
- de Bont, J.; Casas, M.; Barrera-Gomez, J.; Cirach, M.; Rivas, I.; Valvi, D.; Alvarez, M.; Dadvand, P.; Sunyer, J.; Vrijheid, M. Ambient air pollution and overweight and obesity in school-aged children in Barcelona, Spain. Environ. Int. 2019, 125, 58–64. [Google Scholar] [CrossRef]
- Fioravanti, S.; Cesaroni, G.; Badaloni, C.; Michelozzi, P.; Forastiere, F.; Porta, D. Traffic-related air pollution and childhood obesity in an Italian birth cohort. Environ. Res. 2018, 160, 479–486. [Google Scholar] [CrossRef]
- Huang, J.V.; Leung, G.M.; Schooling, C.M. The association of air pollution with body mass index: Evidence from Hong Kong’s “Children of 1997” birth cohort. Int. J. Obes. 2018, 43, 62–72. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Zhao, L.; Huang, Q.; Hong, A.; Yu, C.; Xiao, Q.; Zou, B.; Ji, S.; Zhang, L.; Zou, K.; et al. Traffic-related environmental factors and childhood obesity: A systematic review and meta-analysis. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2021, 22, e12995. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, J.S.; Gui, Z.H.; Zou, Z.Y.; Yang, B.Y.; Ma, J.; Jing, J.; Wang, H.J.; Luo, J.Y.; Zhang, X.; Luo, C.Y.; et al. Long-term exposure to ambient air pollution and metabolic syndrome in children and adolescents: A national cross-sectional study in China. Environ. Int. 2021, 148, 106383. [Google Scholar] [CrossRef] [PubMed]
- Seo, M.Y.; Kim, S.-H.; Park, M.J. Air pollution and childhood obesity. Clin. Exp. Pediatrics 2020, 63, 382–388. [Google Scholar] [CrossRef] [Green Version]
- Huang, S.; Zhang, X.; Huang, J.; Lu, X.; Liu, F.; Gu, D. Ambient air pollution and body weight status in adults: A systematic review and meta-analysis. Environ. Pollut. 2020, 265, 114999. [Google Scholar] [CrossRef]
- Parasin, N.; Amnuaylojaroen, T.; Saokaew, S. Effect of Air Pollution on Obesity in Children: A Systematic Review and Meta-Analysis. Children 2021, 8, 327. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Web of Science, Web of Science® Help. 2009. Available online: https://images.webofknowledge.com/WOK50B6/help/WOS/h_advanced_fieldtags.html (accessed on 1 March 2022).
- National Heart, Lung, and Blood Institute, Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. 2014. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tool (accessed on 1 March 2022).
- Yang, B.Y.; Qian, Z.; Howard, S.W.; Vaughn, M.G.; Fan, S.J.; Liu, K.K.; Dong, G.H. Global association between ambient air pollution and blood pressure: A systematic review and meta-analysis. Environ. Pollut. 2018, 235, 576–588. [Google Scholar] [CrossRef]
- Tamayo-Ortiz, M.; Téllez-Rojo, M.M.; Rothenberg, S.J.; Gutiérrez-Avila, I.; Just, A.C.; Kloog, I.; Texcalac-Sangrador, J.L.; Romero-Martinez, M.; Bautista-Arredondo, L.F.; Schwartz, J.; et al. Exposure to pm2.5 and obesity prevalence in the greater mexico city area. Int. J. Environ. Res. Public Health 2021, 18, 2301. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ong, H.; Holstius, D.; Li, Y.; Seto, E.; Wang, M. Air pollution and child obesity: Assessing the feasibility of measuring personal PM2.5 exposures and behaviours related to BMI in preschool-aged children in China. Obes. Med. 2019, 16, 100149. [Google Scholar] [CrossRef]
- Nikolic, M.; Stankovic, A.; Jovic, S.; Kocic, B.; Bogdanovic, D. Effects of air pollution on growth in schoolchildren. Coll. Antropol. 2014, 38, 493–497. [Google Scholar] [PubMed]
- Kim, E.; Park, H.; Park, E.A.; Hong, Y.-C.; Ha, M.; Kim, H.-C.; Ha, E.-H. Particulate matter and early childhood body weight. Environ. Int. 2016, 94, 591–599. [Google Scholar] [CrossRef]
- de Bont, J.; Hughes, R.; Tilling, K.; Diaz, Y.; de Castro, M.; Cirach, M.; Fossati, S.; Nieuwenhuijsen, M.; Duarte-Salles, T.; Vrijheid, M. Early life exposure to air pollution, green spaces and built environment, and body mass index growth trajectories during the first 5 years of life: A large longitudinal study. Environ. Pollut. 2020, 266, 115266. [Google Scholar] [CrossRef]
- Chen, X.; Liao, J.; Xu, S.; Zhang, B.; Wang, W.; Cao, Z.; Mahai, G.; Yang, X.; Zhang, Y.; Liang, S.; et al. Associations of exposure to nitrogen dioxide and major roadways with growth trajectories and obesity at 2 years old: A prospective cohort study. Atmos. Environ. 2020, 232, 117574. [Google Scholar] [CrossRef]
- Bloemsma, L.D.; Wijga, A.H.; Klompmaker, J.O.; Janssen, N.A.H.; Smit, H.A.; Koppelman, G.H.; Brunekreef, B.; Lebret, E.; Hoek, G.; Gehring, U. The associations of air pollution, traffic noise and green space with overweight throughout childhood: The PIAMA birth cohort study. Environ. Res. 2019, 169, 348–356. [Google Scholar] [CrossRef]
- de Bont, J.; Díaz, Y.; de Castro, M.; Cirach, M.; Basagaña, X.; Nieuwenhuijsen, M.; Duarte-Salles, T.; Vrijheid, M. Ambient air pollution and the development of overweight and obesity in children: A large longitudinal study. Int. J. Obes. 2021, 45, 1124–1132. [Google Scholar] [CrossRef]
- Dong, G.-H.; Qian, Z.; Liu, M.-M.; Wang, D.; Ren, W.-H.; Flick, L.H.; Fu, J.; Wang, J.; Chen, W.; Simckes, M.; et al. Ambient Air Pollution and the Prevalence of Obesity in Chinese Children: The Seven Northeastern Cities Study. Obesity 2014, 22, 795–800. [Google Scholar] [CrossRef] [Green Version]
- Guo, Q.; Xue, T.; Jia, C.; Wang, B.; Cao, S.; Zhao, X.; Zhang, Q.; Zhao, L.; Zhang, J.; Duan, X. Association between exposure to fine particulate matter and obesity in children: A national representative cross-sectional study in China. Environ. Int. 2020, 143, 105950. [Google Scholar] [CrossRef]
- Kim, J.S.; Alderete, T.L.; Chen, Z.; Lurmann, F.; Rappaport, E.; Habre, R.; Berhane, K.; Gilliland, F.D. Longitudinal associations of in utero and early life near-roadway air pollution with trajectories of childhood body mass index. Environ. Health 2018, 17, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McConnell, R.; Shen, E.; Gilliland, F.D.; Jerrett, M.; Wolch, J.; Chang, C.-C.; Lurmann, F.; Berhane, K. A Longitudinal Cohort Study of Body Mass Index and Childhood Exposure to Secondhand Tobacco Smoke and Air Pollution: The Southern California Children’s Health Study. Environ. Health Perspect. 2015, 123, 360–366. [Google Scholar] [CrossRef] [Green Version]
- Vrijheid, M.; Fossati, S.; Maitre, L.; Marquez, S.; Roumeliotaki, T.; Agier, L.; Andrusaityte, S.; Cadiou, S.; Casas, M.; de Castro, M.; et al. Early—Life Environmental Exposures and Childhood Obesity: An Exposome-Wide Approach. Environ. Health Perspect. 2020, 128, 067009. [Google Scholar] [CrossRef] [PubMed]
- Skinner, A.C.; Ravanbakht, S.N.; Skelton, J.A.; Perrin, E.M.; Armstrong, S.C. Prevalence of Obesity and Severe Obesity in US Children, 1999–2016. Pediatrics 2018, 141, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spinelli, A.; Buoncristiano, M.; Kovacs, V.A.; Yngve, A.; Spiroski, I.; Obreja, G.; Starc, G.; Pérez, N.; Rito, A.I.; Kunešová, M.; et al. Prevalence of Severe Obesity among Primary School Children in 21 European Countries. Obes. Facts 2019, 12, 244–258. [Google Scholar] [CrossRef]
- Aiello, A.M.; Marques de Mello, L.; Souza Nunes, M.; Soares da Silva, A.; Nunes, A. Prevalence of Obesity in Children and Adolescents in Brazil: A Meta-analysis of Cross-sectional Studies. Curr. Pediatr. Rev. 2015, 11, 36–42. [Google Scholar] [CrossRef]
- Greenstone, M.; Hanna, R. Environmental Regulations, Air and Water Pollution, and Infant Mortality in India. Am. Econ. Rev. 2014, 104, 3038–3072. [Google Scholar] [CrossRef] [Green Version]
- North, C.M.; Rice, M.B.; Ferkol, T.; Gozal, D.; Hui, C.; Jung, S.H.; Kuribayashi, K.; McCormack, M.C.; Mishima, M.; Morimoto, Y.; et al. Air pollution in the Asia-Pacific Region: A Joint Asian Pacific Society of Respirology/American Thoracic Society perspective (Republication). Respirology 2019, 24, 484–491. [Google Scholar] [CrossRef] [Green Version]
- Klompmaker, J.O.; Hoek, G.; Bloemsma, L.D.; Wijga, A.H.; van den Brink, C.; Brunekreef, B.; Lebret, E.; Gehring, U.; Janssen, N.A.H. Associations of combined exposures to surrounding green, air pollution and traffic noise on mental health. Environ. Int. 2019, 129, 525–537. [Google Scholar] [CrossRef]
- Li, N.; Georas, S.; Alexis, N.; Fritz, P.; Xia, T.; Williams, M.A.; Horner, E.; Nel, A. A work group report on ultrafine particles (American Academy of Allergy, Asthma & Immunology): Why ambient ultrafine and engineered nanoparticles should receive special attention for possible adverse health outcomes in human subjects. J. Allergy Clin. Immunol. 2016, 138, 386–396. [Google Scholar]
- Ustulin, M.; Keum, C.; Woo, J.; Woo, J.T.; Rhee, S.Y. Effects of climatic variables on weight loss: A global analysis. Sci. Rep. 2017, 7, 40708. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Zhang, J.J.; Li, Z.; Gow, A.; Chung, K.F.; Hu, M.; Sun, Z.; Zeng, L.; Zhu, T.; Jia, G.; et al. Chronic exposure to air pollution particles increases the risk of obesity and metabolic syndrome: Findings from a natural experiment in Beijing. FASEB J. 2016, 30, 2115–2122. [Google Scholar] [CrossRef] [PubMed]
- Toledo-Corral, C.M.; Alderete, T.L.; Habre, R.; Berhane, K.; Lurmann, F.W.; Weigensberg, M.J.; Goran, M.I.; Gilliland, F.D. Effects of air pollution exposure on glucose metabolism in Los Angeles minority children. Pediatr. Obes. 2018, 13, 54–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, Y.L.; Liu, W.T.; Lee, K.Y.; Chuang, H.C.; Chen, H.W.; Chuang, K.J.; Billings, M.E.; Gold, D.; Szpiro, A.; Aaron, C.P.; et al. Association of PM(2.5) with sleep-disordered breathing from a population-based study in Northern Taiwan urban areas. Environ. Pollut. 2018, 233, 109–113. [Google Scholar] [CrossRef]
- Billings, M.E.; Gold, D.; Szpiro, A.; Aaron, C.P.; Jorgensen, N.; Gassett, A.; Leary, P.J.; Kaufman, J.D.; Redline, S.R. The Association of Ambient Air Pollution with Sleep Apnea: The Multi-Ethnic Study of Atherosclerosis. Ann. Am. Thorac. Soc. 2019, 16, 363–370. [Google Scholar] [CrossRef]
- Chen, Z.; Herting, M.M.; Chatzi, L.; Belcher, B.R.; Alderete, T.L.; McConnell, R.; Gilliland, F.D. Regional and traffic-related air pollutants are associated with higher consumption of fast food and trans fat among adolescents. Am. J. Clin. Nutr. 2019, 109, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, R.; Jadotte, Y.; Zha, P.; Porter, S.A.; Holly, C.; Salmond, S.; Watkins, E.A. The association between prenatal exposure to environmental tobacco smoke and childhood obesity: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2018, 16, 1643–1662. [Google Scholar] [CrossRef]
- Reilly, J.J.; Armstrong, J.; Dorosty, A.R.; Emmett, P.M.; Ness, A.; Rogers, I.; Steer, C.; Sherriff, A. Early life risk factors for obesity in childhood: Cohort study. BMJ 2005, 330, 1357. [Google Scholar] [CrossRef] [Green Version]
| Study ID | Author (Year) | Country | Study Design | Study Period | Sample Size (Boy %) | Age | Quality a |
|---|---|---|---|---|---|---|---|
| 1 | Zheng et al. (2021) | China | Cross-sectional | 2019 | 36,456 (52.1) | 9–17 | 13 |
| 2 | Zhang et al. (2021a) | China | Cross-sectional | 2013–2014 | 44,718 (50.5) | 7–18 | 13 |
| 3 | Zhang et al. (2021b) | China | Cross-sectional | 2013–2014 | 9897 (50.3) | 10–18 | 13 |
| 4 | Tamayo et al. (2021) | Mexico | Cross-sectional | 2006 and 2012 | 4306 (51.5) | 2–18 | 11 |
| 5 | Bont et al. (2021) | Spain | Cohort | 2006–2018 | 416,955 (51.4) | 2–15 | 12 |
| 6 | Vrijheid et al. (2020) | UK | Cross-sectional | 2013–2016 | 1301 (54.7) | 6–11 | 11 |
| 7 | Guo et al. (2020) | China | Cross-sectional | 2013–2014 | 40,953 (48.3) | 6–17 | 13 |
| 8 | Bont et al. (2020) | Spain | Cohort | 2011–2016 | 79,992 (51.0) | 0–5 | 13 |
| 9 | Chen et al. (2020) | China | Cohort | 2012–2014 | 5752 (52.5) | 0–2 | 12 |
| 10 | Bont et al. (2019) | Spain | Cross-sectional | 2012 | 2660 (51.1) | 7–10 | 13 |
| 11 | Bloemsma et al. (2019) | Netherlands | Cohort | 1996–2014 | 3680 (51.9) | 3–17 | 12 |
| 12 | Kim et al. (2018) | US | Cohort | 2002–2003 | 2318 (50.6) | 6.5 ± 0.7 | 13 |
| 13 | Fioravanti et al. (2018) | Italy | Cohort | 2003–2004 | 719 (50.6) | 4–8 | 12 |
| 14 | McConnell et al. (2015) | US | Cohort | 2003–2014 | 3318 (49.6) | 10.1 ± 0.59 | 13 |
| 15 | Dong et al. (2014) | China | Cross-sectional | 2009 | 30,056 (50.4) | 2–14 | 11 |
| Study ID | Author (Year) | Exposure | Duration | Exposure Assessment | Outcome Definition | Statistical Model | Adjusted Covariates |
|---|---|---|---|---|---|---|---|
| 1 | Zheng et al. (2021) | PM10, PM2.5, O3, NO2 | Long-term | Monitoring stations | Age-and-sex specific BMI cut-offs (Chinese national standard) | Multivariate regression model | Sex, age, paternal, sugar-sweetened beverage consumption, sweetened food consumption, frequency of having breakfast, fried food consumption, physical activity duration |
| 2 | Zhang et al. (2021a) | PM10, PM2.5, PM1, NO2 | Long-term | Satellite-based spatial-temporal model | Age-and-sex specific BMI cut-offs (Chinese national standard) | Mixed-effects linear and logistic regression models | Age, physical activity, fruit & vegetable intake, parental smoking, parental education, north or south, urban residency, regional GDP per capita |
| 3 | Zhang et al. (2021b) | PM10, PM2.5,PM1, NO2 | Long-term | Satellite-based spatial-temporal model | Waist circumference (Chinese national standard) | Generalized linear mixed-effects models | Age, sex, weight status, temperature, relative humidity, parental education level achieved, parental smoking status, parental alcohol consumption, family history of type 2 diabetes, hypertension, obesity, or cerebrovascular disease, outdoor physical activity time, diet of high fat, SSBs intake. |
| 4 | Tamayo et al. (2021) | PM2.5 | Long-term | Hybrid spatio-temporal model | Age-specific BMI (WHO standard) | Logistic regression models | Age, sex, SES, and smoking status |
| 5 | Bont et al. (2021) | PM10, PM2.5, NO2 | Long-term | Land use regression model | Age-and-sex specific BMI (WHO standard) | Cox proportional hazards models | Sex, deprivation index, nationality, deprivation index, and had age (1-year categories) in the strata statement. |
| 6 | Vrijheid et al. (2020) | NO2 | Long-term | Land use regression model | Age-and-sex specific BMI (WHO standard) | Linear regression models, and logistic regression models | Sex, maternal BMI, maternal education, maternal age at conception, parity, parental country of origin, breastfeeding, and birth weight |
| 7 | Guo et al. (2020) | PM2.5 | Long-term | Machine-learning model | Age-and-sex specific BMI cut-offs (Chinese national standard) | Logistic regression models | Sex, age, urbanity, boarding school or not, economic level, maternal occupation, maternal education, vegetable intake, fruit intake, beverages intake, activity times, ventilation, cooking fuel type, household heating fuel type, school heating fuel type, and secondhand smoke duration |
| 8 | Bont et al. (2020) | PM10, PM2.5, NO2 | Long-term | Land use regression model | BMI z-scores (WHO standard) | Linear spline multilevel model | Sex, age, deprivation index, nationality |
| 9 | Chen et al. (2020) | NO2 | Long-term | Land use regression model | Age- and sex-specific z scores for BMI (WHO standard) | Generalized estimating equation models, Distributed lag nonlinear models | Maternal age, maternal education, annual household income and residence area |
| 10 | Bont et al. (2019) | PM10, PM2.5, NO2 | Long-term | Land use regression model | Age- and sex-specific z scores for BMI (WHO standard) | Multilevel mixed linear and ordered logistic models | Maternal and paternal education, maternal and paternal country of birth, paternal employment status, number of siblings, household status and maternal smoking during pregnancy |
| 11 | Bloemsma et al. (2019) | PM10, PM2.5, NO2 | Long-term | Land use regression model | Age-and-sex specific BMI (International Obesity Task Force cut-offs) | Generalized linear mixed models | Age, sex maternal level of education, paternal level of education, maternal smoking during pregnancy, parental smoking in child’s home and neighborhood socioeconomic status and region |
| 12 | Kim et al. (2018) | NOx | Long-term | California line-source dispersion model | BMI (US CDC criteria) | Linear mixed effects models | Age, sex, race/ethnicity, parental education, and Spanish baseline questionnaire |
| 13 | Fioravanti et al. (2018) | PM10, PM2.5, NO2 | Long-term | Land use regression model | Age- and sex-specific z scores for BMI (WHO standard) | Logistic regression models, Generalized Estimating Equation models and linear regression models | Maternal and paternal education, maternal pre-pregnancy BMI, maternal smoking during pregnancy, gestational diabetes, maternal age at delivery, gestational age, childbirth weight, breastfeeding duration, age at weaning and inversely weighted for the probability of participation at baseline and at the two follow-ups, respectively |
| 14 | McConnell et al. (2015) | NOx | Long-term | California line-source dispersion model | Age-and-sex specific BMI (US CDC criteria) | Multilevel linear model | Sex, ethnicity, community, year of enrollment, and age |
| 15 | Dong et al. (2014) | PM10, NO2, SO2, O3 | Long-term | Monitoring stations | Age-and-sex specific BMI standards (Chinese CDC criteria) | Logistic regression | Age, gender, parental education, breastfeeding, low birth weight, area of residence per person, house decorations, home coal use, ventilation device in kitchen, air exchange in winter, passive smoking exposure, and districts |
| Pollution Type | Author (Year) | Group | Sample Size | Incremental Scale | Original Effect | Transformed OR/β |
|---|---|---|---|---|---|---|
| obesity | ||||||
| PM10 | Zheng (2021) | Total | 36,456 | 10 μg/m3 | 1.03 (0.97, 1.09) | - |
| Zhang (2021a) | Boy | 22,573 | 10 μg/m3 | 1.25 (1.15, 1.37) | - | |
| Zhang (2021a)’ | Girl | 22,145 | 10 μg/m3 | 1.32 (1.21, 1.45) | - | |
| Zhang (2021b) | Total | 44,718 | 10 μg/m3 | 1.32 (1.11, 1.55) | - | |
| Bont (2021) | Total | 416,955 | 6.4 μg/m3 | 1.02 (1.02, 1.03) | 1.03 (1.02, 1.05) | |
| Bont (2019) | Home | 2660 | 5.6 μg/m3 | 1.10 (1.00, 1.22) | 1.18 (1.00, 1.43) | |
| Bloemsma (2019) | Total | 3680 | 1.06 μg/m3 | 1.00 (0.88, 1.12) | 1.00 (0.30, 2.91) | |
| Fioravanti (2018) | Total | 719 | 10 μg/m3 | 0.97 (0.77, 1.23) | - | |
| Dong (2014) | Total | 30,056 | 31 µg/m3 | 1.19 (1.11, 1.26) | 1.06 (1.03, 1.08) | |
| PM2.5 | Zheng (2021) | Total | 36,456 | 10 μg/m3 | 1.19 (1.05, 1.33) | - |
| Zhang (2021a) | Boy | 22,573 | 10 μg/m3 | 1.40 (1.26, 1.55) | - | |
| Zhang (2021a)’ | Girl | 22,145 | 10 μg/m3 | 1.49 (1.34, 1.66) | - | |
| Zhang (2021b) | Total | 44,718 | 10 μg/m3 | 1.40 (1.19, 1.65) | - | |
| Tamayo (2021) | Children | 1370 | 10 μg/m3 | 3.64 (1.88, 7.06) | - | |
| Tamayo (2021)’ | Adolescence | 1519 | 10 μg/m3 | 1.62 (0.90, 2.93) | - | |
| Guo (2020) | Total | 40,953 | 10 μg/m3 | 1.10 (1.03, 1.16) | - | |
| Bont (2019) | Home | 2660 | 2.7 μg/m3 | 1.05 (0.96, 1.15) | 1.19 (0.86, 1.68) | |
| Bont (2019)’ | School | 2660 | 10.7 μg/m3 | 1.00 (0.93, 1.08) | 1.00 (0.93, 1.07) | |
| Bloemsma (2019) | Total | 3680 | 1.17 μg/m3 | 0.80 (0.59 1.09) | 0.15 (0.01, 9.31) | |
| Fioravanti (2018) | Total | 719 | 5 μg/m3 | 1.02 (0.75, 1.40) | 1.04 (0.56, 1.96) | |
| PM1 | Zhang (2021a) | Boy | 22,573 | 10 μg/m3 | 1.38 (1.21, 1.57) | - |
| Zhang (2021a)’ | Girl | 22,145 | 10 μg/m3 | 1.44 (1.25, 1.67) | - | |
| Zhang (2021b) | Total | 44,718 | 10 μg/m3 | 1.42 (1.23, 1.64) | - | |
| O3 | Zheng (2021) | Total | 36,456 | 10 μg/m3 | 1.04 (1.00, 1.08) | - |
| Dong (2014) | Total | 30,056 | 11.3 ppb | 1.14 (1.04, 1.24) | 1.06 (1.02, 1.09) | |
| NO2 | Zheng (2021) | Total | 36,456 | 10 μg/m3 | 1.13 (1.04, 1.22) | - |
| Zhang (2021a) | Boy | 22,573 | 10 μg/m3 | 1.14 (1.04, 1.24) | - | |
| Zhang (2021a)’ | Girl | 22,145 | 10 μg/m3 | 1.21 (1.10, 1.34) | - | |
| Zhang (2021b) | Total | 44,718 | 10 μg/m3 | 1.44 (1.22, 1.71) | - | |
| Bont (2021) | Total | 416,955 | 21.8 μg/m3 | 1.03 (1.02, 1.04) | 1.01 (1.00, 1.02) | |
| Chen (2020) | Total | 5752 | 10 μg/m3 | 1.11 (1.00, 1.22) | - | |
| Bont (2019) | Home | 2660 | 13.7 μg/m3 | 1.05 (0.97, 1.13) | 1.04 (0.98, 1.09) | |
| Bont (2019)’ | School | 2660 | 22.3 μg/m3 | 1.09 (0.92, 1.28) | 1.04 (0.96, 1.12) | |
| Bloemsma (2019) | Total | 3680 | 8.9 μg/m3 | 1.40 (1.12, 1.74) | 1.46 (1.14, 1.86) | |
| Fioravanti (2018) | Total | 719 | 10 μg/m3 | 0.99 (0.86, 1.12) | - | |
| Dong (2014) | Total | 300,56 | 5.3 ppb | 1.13 (1.04, 1.22) | 1.13 (1.04, 1.21) | |
| BMI | ||||||
| PM10 | Zhang (2021a) | Boy | 22,573 | 10 μg/m3 | 0.11 (0.07, 0.14) | - |
| Zhang (2021a)’ | Girl | 22,145 | 10 μg/m3 | 0.09 (0.06, 0.12) | - | |
| Bont (2020) | Total | 79,992 | 6.3 μg/m3 | 0.02 (0.01, 0.03) | 0.04 (0.02, 0.05) | |
| PM2.5 | Zhang (2021a) | Boy | 22,573 | 10 μg/m3 | 0.15 (0.11, 0.19) | - |
| Zhang (2021a)’ | Girl | 22,145 | 10 μg/m3 | 0.13 (0.09, 0.17) | - | |
| Bont (2020) | Total | 79,992 | 1.5 μg/m3 | 0.01 (0.00, 0.01) | 0.05 (0.00, 0.09) | |
| NO2 | Zhang (2021a) | Boy | 22,573 | 10 μg/m3 | 0.05 (0.01, 0.09) | - |
| Zhang (2021a)’ | Girl | 22,145 | 10 μg/m3 | 0.04 (0.01, 0.08) | - | |
| Vrijheid (2020) | Total | 1301 | 92.8 μg/m3 | 0.15 (0.01, 0.28) | 0.02 (0.00, 0.30) | |
| Bont (2020) | Total | 79,992 | 21.3 μg/m3 | 0.02 (0.01, 0.03) | 0.01 (0.00, 0.02) | |
| Chen (2020) | Total | 5752 | 10 μg/m3 | 0.03 (0.01, 0.05) | - | |
| NOx | Kim (2018) | Total | 2318 | 9.4 ppb | 0.10 (0.03, 0.20) | 0.05 (0.02, 0.10) |
| McConnell (2015) | Total | 2994 | 16.8 ppb | 1.13 (0.61, 1.65) | 0.33 (0.18, 0.50) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, C.; Li, C.; Zhao, F.; Zhu, J.; Wang, S.; Sun, G. The Association between Childhood Exposure to Ambient Air Pollution and Obesity: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 4491. https://doi.org/10.3390/ijerph19084491
Huang C, Li C, Zhao F, Zhu J, Wang S, Sun G. The Association between Childhood Exposure to Ambient Air Pollution and Obesity: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(8):4491. https://doi.org/10.3390/ijerph19084491
Chicago/Turabian StyleHuang, Chao, Cheng Li, Fengyi Zhao, Jing Zhu, Shaokang Wang, and Guiju Sun. 2022. "The Association between Childhood Exposure to Ambient Air Pollution and Obesity: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 8: 4491. https://doi.org/10.3390/ijerph19084491
APA StyleHuang, C., Li, C., Zhao, F., Zhu, J., Wang, S., & Sun, G. (2022). The Association between Childhood Exposure to Ambient Air Pollution and Obesity: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(8), 4491. https://doi.org/10.3390/ijerph19084491








