Changes in Motor Performance and BMI of Primary School Children over Time–Influence of the COVID-19 Confinement and Social Burden
Abstract
:1. Introduction
2. Materials and Methods
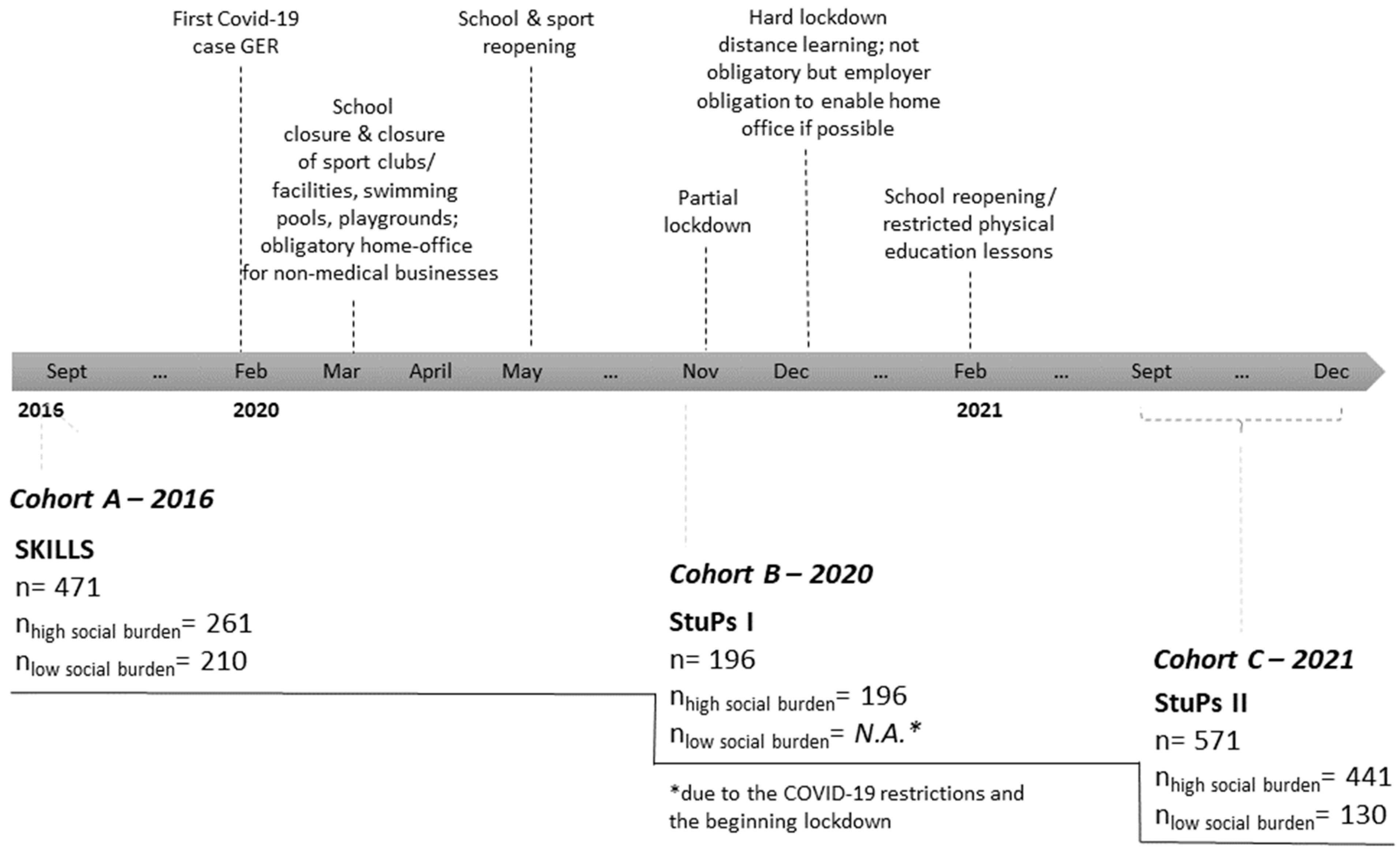
2.1. Study Population
2.2. Analysis Parameter
2.2.1. Anthropometric Data
2.2.2. Motor Test Items: Lateral Jumping, Standing Long Jump, 6-min Run
2.2.3. Socio-Cultural Variable: School-Based Social Index
- ▪
- Children and youth poverty-assessed by the proportion of children living in the vicinity of the primary school with parents receiving governmental financial support for jobseekers (SGB II rate);
- ▪
- The proportion of children in families whose primary language is not German;
- ▪
- The proportion of children who immigrated from abroad;
- ▪
- The proportion of children with special needs in learning, emotional and social development, or language.
2.3. Data Analysis
3. Results
3.1. Anthropometric Data–Descriptive Presentation
3.1.1. Cohort Comparisons of BMI and BMI z Score (High Social Burden)
3.1.2. Cohort Comparison of BMI and BMI z Score Considering Social Index (Cohorts A and C)
3.2. Motor Performance
3.2.1. Lateral Jumping–Descriptive Presentation
Cohort Comparisons of Lateral Jumping (High Social Burden)
Cohort Comparison of Lateral Jumping Considering Social Index (Cohorts A and C)
3.2.2. Standing Long Jump–Descriptive Presentation
Cohort Comparisons of Standing Long Jump (High Social Burden)
Cohort Comparison of Standing Long Jump Considering Social Index (Cohorts A and C)
6-min Run–Descriptive Presentation
Cohort Comparisons of 6-min Run (High Social Burden)
Cohort Comparison of 6-min Run Considering Social Index (Cohorts A and C)
4. Discussion
Strengths and Weaknesses
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Variable | Type | Definition | Cohort A | Cohort B | Cohort C |
|---|---|---|---|---|---|
| 2016 | 2020 | 2021 | |||
| Age | Metric | Participants’ age in years at the measurement point | √ | √ | √ |
| Sex | Dichotomous | Participants‘ sex, 0 = girl, 1 = boy | √ | √ | √ |
| Height | Metric | Participants’ body height in cm | √ | √ | √ |
| Weight | Metric | Participants’ body weight in kg | √ | √ | √ |
| BMI | Metric | Participants’ body mass index (measure of weight adjusted for height) in kg/m2 | √ | √ | √ |
| BMI z score | Metric | Participants’ BMI standard deviation score | √ | √ | √ |
| BMI percentile | Categorial | Participants’ BMI category 1 = underweight, 2 = normal weight, 3 = overweight, 4 = obesity | √ | √ | √ |
| Lateral jumps | Metric | Participants‘ number of jumps during 2 × 15 s, to assess agility and coordination | √ | √ | √ |
| Standing long jump | Metric | Participants’ best of two tries (in cm), to assess the rapid strength of the lower extremities | √ | √ | √ |
| 6-min run | Metric | Distance (in meters) run by a participant in 6 min, aerobic endurance capacity | √ | N.A. * | √ |
| Social index | Metric | Social index of each participant’s school, from 1 = very low burden to 9 = very high burden; numbers were clustered as dummy variables into 0 = low social burden (numbers 1 to 5), 1 = high social burden (numbers 6 to 9) | √ | √ | √ |
| Pandemic Situation | Categorial | Participants were screened during COVID-19 pandemic situations in 2020 or 2021; 0 = no, 1 = yes | √ | √ | √ |
| Tests of Between-Subjects Effects | Pairwise Comparisons | ||||||
|---|---|---|---|---|---|---|---|
| Corrected Model | BMI | Age | Sex | Cohort B-A | Cohort C-A | Cohort C-B | |
| p-Value (Adjusted R2) | p-Value (np2) | p-Value (np2) | p-Value (np2) | ΔMW (SD), % Change, p-Value (np2) | ΔMW (SD), % Change, p-Value (np2) | ΔMW (SD), % Change, p-Value (np2) | |
| BMI (kg/m2) | <0.001 (0.058) | N.A. | <0.001 (0.044) | 0.362 (0.001) | Δ 0.8 (0.3) +4.9% 0.020 | Δ 0.9 (0.3) +5.4% <0.001 | Δ 0.1 (0.3) +0.5% 1.0 |
| BMI z score | 0.005 (0.010) | N.A. | N.A. | N.A. | Δ 0.2 (0.1) +48.1% 0.070 | Δ 0.3 (0.1) +71.5% <0.001 | Δ 0.1 (0.1) +15.8% 0.333 |
| lateral jumps (counts) * | <0.001 (0.358) | <0.001 (0.037) | <0.001 (0.324) | 0.227 (0.002) | Δ −3.8 (1.3) −7.6% 0.012 | Δ −6.1 (1.1) −12.3% <0.001 | Δ −2.4 (1.2) −5.1% 0.141 |
| standing long jump (cm) * | <0.001 (0.269) | <0.001 (0.094) | <0.001 (0.206) | <0.001 (0.038) | Δ 5.8 (1.9) +5.4% 0.008 | Δ 2.3 (1.6) +2.1% 0.497 | Δ −3.6 (1.7) +3.1% 0.124 |
| 6-min run (m) * | <0.001 (0.366) | <0.001 (0.159) | <0.001 (0.117) | <0.001 (0.035) | N.A. | Δ −97.4 (8.8) −11.3% <0.001 | N.A. |
| Dependent Variable | Factors | Covariates | |
|---|---|---|---|
| Model 1 | BMI | cohort, social index | age, sex |
| Model 2 | BMI z score | cohort, social index | |
| Model 3 | lateral jumps | cohort, social index | BMI, age, sex |
| Model 4 | standing long jumps | cohort, social index | BMI, age, sex |
| Model 5 | 6-min run | cohort, social index | BMI, age, sex |
| Tests of Between-Subjects Effects | Pairwise Comparisons | |||||||
|---|---|---|---|---|---|---|---|---|
| Corrected Model | Cohort | Social Index | High-Low Burden | Cohort A: High-Low Burden | Cohort C: High-Low Burden | High Burden: Cohort C-A | Low Burden: Cohort C-A | |
| p-Value (Adjusted R2) | p-Value (np2) | p-Value (np2) | ΔMW (SD), % Change, p-Value (np2) | ΔMW (SD), % Change, p-Value (np2) | ΔMW (SD), % Change, p-Value (np2) | ΔMW (SD), % Change, p-Value (np2) | ΔMW (SD), % Change, p-Value (np2) | |
| Model 1 | <0.001 (0.084) | 0.040 (0.004) * | Δ 1.1 (0.2) +6.4% <0.001 (0.027) | Δ 0.7 (0.3) +3.9% 0.017 (0.006) | Δ 1.5 (0.3) +8.8% <0.001 (0.024) | Δ 0.9 (0.2) +5.3% <0.001 (0.015) | Δ 0.1 (0.3) +0.6% 0.769 (0) | |
| Model 2 | <0.001 (0.041) | 0.016 (0.006) | <0.001 (0.024) | Δ 0.4 (0.1) <0.001 (0.024) | Δ 0.2 (0.1) 0.013 (0.006) | Δ 0.5 (0.1) <0.001 (0.020) | Δ 0.3 (0.1) <0.001 (0.012) | Δ 0.1 (0.1) 0.657 (0) |
| Model 3 | <0.001 (0.390) | <0.001 (0.035) | <0.001 (0.021) | Δ −4.5 (1.0) −9.6% <0.001 (0.021) | Δ −4.3 (1.3) −7.8% <0.001 (0.010) | Δ −4.8 (1.4) −9.8% <0.001 (0.011) | Δ −6.0 (1.1) −11.9% <0.001 (0.028) | Δ −5.4 (1.6) −10,0% <0.001 (0.012) |
| Model 4 | <0.001 (0.304) | 0.022 (0.005) * | Δ −8.9 (1.4) −7.4% <0.001 (0.040) | Δ −12.1 (1.9) −10.0% <0.001 (0.040) | Δ −5.7 (2.1) −4.8% 0.006 (0.008) | Δ −2.6 (1.6) +2.4% 0.108 (0.003) | Δ −3.8 (2.3) −3.1% 0.096 (0.003) | |
| Model 5 | <0.001 (0.426) | 0.009 (0.007) * | Δ −71.7 (7.6) −8.0% <0.001 (0.080) | Δ−52.0 (10.2) −5.6% <0.001 (0.025) | Δ −91.4 (11.1) −10.6% <0.001 (0.062) | Δ −96.8 (8.7) −11.1% <0.001 (0.108) | Δ −57.5 (12.2) −6.2% <0.001 (0.021) | |
References
- Janssen, I.; Leblanc, A.G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 40. [Google Scholar] [CrossRef] [Green Version]
- Ortega, F.B.; Ruiz, J.R.; Castillo, M.J.; Sjöström, M. Physical fitness in childhood and adolescence: A powerful marker of health. Int. J. Obes. 2008, 32, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Finger, J.D.; Varnaccia, G.; Borrmann, A.; Lange, C.; Mensink, G. Körperliche Aktivität von Kindern und Jugendlichen in Deutschland–Querschnittergebnisse aus KiGGS Welle 2 und Trends. J. Health Monit. 2018, 3, 24–31. [Google Scholar] [CrossRef]
- Eberhardt, T.; Niessner, C.; Oriwol, D.; Buchal, L.; Worth, A.; Bös, K. Secular Trends in Physical Fitness of Children and Adolescents: A Review of Large-Scale Epidemiological Studies Published after 2006. Int. J. Environ. Res. Public Health 2020, 17, 5671. [Google Scholar] [CrossRef]
- Schlag, E.; Ferrari, N.; Koch, B.; Dordel, S.; Joisten, C. Secular trends in motor performance of children and adolescents between 2010 and 2020. Transl. Sports Med. 2021, 4, 882–891. [Google Scholar] [CrossRef]
- Schienkiewitz, A.; Brettschneider, A.K.; Damerow, S.; Schaffrath Rosario, A. Übergewicht und Adipositas im Kindes- und Jugendalter in Deutschland—Querschnittergebnisse aus KiGGS Welle 2 und Trends. J. Health Monit. 2018, 3, 16–23. [Google Scholar] [CrossRef]
- Adamakis, M. Resurgence of physical education and physical activity in the COVID-19 era: Policy inconsistencies, implications and future considerations. IJoPE 2021, 58, 29–40. [Google Scholar] [CrossRef]
- Wunsch, K.; Kienberger, K.; Niessner, C. Changes in Physical Activity Patterns Due to the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 2250. [Google Scholar] [CrossRef]
- Rossi, L.; Behme, N.; Breuer, C. Physical Activity of Children and Adolescents during the COVID-19 Pandemic-A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 11440. [Google Scholar] [CrossRef]
- Schmidt, S.C.E.; Anedda, B.; Burchartz, A.; Eichsteller, A.; Kolb, S.; Nigg, C.; Niessner, C.; Oriwol, D.; Worth, A.; Woll, A. Physical activity and screen time of children and adolescents before and during the COVID-19 lockdown in Germany: A natural experiment. Sci. Rep. 2020, 10, 21780. [Google Scholar] [CrossRef]
- Schmidt, S.C.E.; Burchartz, A.; Kolb, S.; Niessner, C.; Oriwol, D.; Woll, A. Influence of socioeconomic variables on physical activity and screen time of children and adolescents during the COVID-19 lockdown in Germany: The MoMo study. Ger. J. Exerc. Sport Res. 2021, 1–12. [Google Scholar] [CrossRef]
- Schmidt, S.C.E.; Burchartz, A.; Kolb, S.; Niessner, C.; Oriwol, D. Zur Situation der Körperlichsportlichen Aktivität von Kindern und Jugendlichen Während der COVID-19 Pandemie in Deutschland: Die Motorik-Modul Studie (MoMo) No. 165, KIT Scientific Working Papers. 2021. Available online: https://www.sport.kit.edu/rd_download/1.%20Startseite/Aktuelles/Schmidt%20et%20al%20MoMo%20Corona%202%20SR%202021.pdf (accessed on 24 March 2022).
- Zenic, N.; Taiar, R.; Gilic, B.; Blazevic, M.; Maric, D.; Pojskic, H.; Sekulic, D. Levels and Changes of Physical Activity in Adolescents during the COVID-19 Pandemic: Contextualizing Urban vs. Rural Living Environment. Appl. Sci. 2020, 10, 3997. [Google Scholar] [CrossRef]
- Ostermeier, E.; Tucker, P.; Clark, A.; Seabrook, J.A.; Gilliland, J. Parents’ Report of Canadian Elementary School Children’s Physical Activity and Screen Time during the COVID-19 Pandemic: A Longitudinal Study. Int. J. Environ. Res. Public Health 2021, 18, 12352. [Google Scholar] [CrossRef]
- Rundle, A.G.; Park, Y.; Herbstman, J.B.; Kinsey, E.W.; Wang, Y.C. COVID-19-Related School Closings and Risk of Weight Gain Among Children. Obesity (Silver Spring) 2020, 28, 1008–1009. [Google Scholar] [CrossRef] [Green Version]
- Perez, D.; Thalken, J.K.; Ughelu, N.E.; Knight, C.J.; Massey, W.V. Nowhere to Go: Parents’ Descriptions of Children’s Physical Activity During a Global Pandemic. Front. Public Health 2021, 9, 642932. [Google Scholar] [CrossRef]
- ten Velde, G.; Lubrecht, J.; Arayess, L.; van Loo, C.; Hesselink, M.; Reijnders, D.; Vreugdenhil, A. Physical activity behaviour and screen time in Dutch children during the COVID-19 pandemic: Pre-, during- and post-school closures. Pediatr. Obes. 2021, 16, e12779. [Google Scholar] [CrossRef]
- Xiang, M.; Zhang, Z.; Kuwahara, K. Impact of COVID-19 pandemic on children and adolescents’ lifestyle behavior larger than expected. Prog. Cardiovasc. Dis. 2020, 63, 531–532. [Google Scholar] [CrossRef]
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obesity (Silver Spring) 2020, 28, 1382–1385. [Google Scholar] [CrossRef]
- Carson, V.; Hunter, S.; Kuzik, N.; Gray, C.E.; Poitras, V.J.; Chaput, J.-P.; Saunders, T.J.; Katzmarzyk, P.T.; Okely, A.D.; Connor Gorber, S.; et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: An update. Appl. Physiol. Nutr. Metab. 2016, 41, S240–S265. [Google Scholar] [CrossRef]
- Tandon, P.S.; Zhou, C.; Johnson, A.M.; Gonzalez, E.S.; Kroshus, E. Association of Children’s Physical Activity and Screen Time with Mental Health During the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e2127892. [Google Scholar] [CrossRef]
- Leblanc, A.G.; Gunnell, K.E.; Prince, S.A.; Saunders, T.J.; Barnes, J.D.; Chaput, J.-P. The Ubiquity of the Screen: An Overview of the Risks and Benefits of Screen Time in Our Modern World. Transl. J. Am. Coll. Sports Med. 2017, 2, 104. [Google Scholar] [CrossRef]
- Chambonnière, C.; Fearnbach, N.; Pelissier, L.; Genin, P.; Fillon, A.; Boscaro, A.; Bonjean, L.; Bailly, M.; Siroux, J.; Guirado, T.; et al. Adverse Collateral Effects of COVID-19 Public Health Restrictions on Physical Fitness and Cognitive Performance in Primary School Children. Int. J. Environ. Res. Public Health 2021, 18, 11099. [Google Scholar] [CrossRef]
- Jarnig, G.; Jaunig, J.; van Poppel, M.N.M. Association of COVID-19 Mitigation Measures with Changes in Cardiorespiratory Fitness and Body Mass Index Among Children Aged 7 to 10 Years in Austria. JAMA Netw. Open 2021, 4, e2121675. [Google Scholar] [CrossRef]
- Basterfield, L.; Burn, N.L.; Galna, B.; Batten, H.; Goffe, L.; Karoblyte, G.; Lawn, M.; Weston, K.L. Changes in children’s physical fitness, BMI and health-related quality of life after the first 2020 COVID-19 lockdown in England: A longitudinal study. J. Sports Sci. 2022, 1–9. [Google Scholar] [CrossRef]
- Tsoukos, A.; Bogdanis, G.C. The Effects of a Five-Month Lockdown Due to COVID-19 on Physical Fitness Parameters in Adolescent Students: A Comparison between Cohorts. Int. J. Environ. Res. Public Health 2021, 19, 326. [Google Scholar] [CrossRef]
- Chang, T.-H.; Chen, Y.-C.; Chen, W.-Y.; Chen, C.-Y.; Hsu, W.-Y.; Chou, Y.; Chang, Y.-H. Weight Gain Associated with COVID-19 Lockdown in Children and Adolescents: A Systematic Review and Meta-Analysis. Nutrients 2021, 13, 3668. [Google Scholar] [CrossRef]
- Woolford, S.J.; Sidell, M.; Li, X.; Else, V.; Young, D.R.; Resnicow, K.; Koebnick, C. Changes in Body Mass Index Among Children and Adolescents During the COVID-19 Pandemic. JAMA 2021, 326, 1434–1436. [Google Scholar] [CrossRef]
- Ehlen, S.; Dreiskämper, D.; Utesch, T.; Rehaag, R. Integrierte Gesamtansätze kommunaler Gesundheitsförderung für Kinder. Präv Gesundh. 2018, 13, 254–260. [Google Scholar] [CrossRef]
- Wessely, S.; Starke, D.; Weyers, S.; Joisten, C. Closing the gap between practice and science in school- and community-based participatory physical literacy promotion: Study protocol of the StuPs project. BMC Public Health 2021, 21, 642. [Google Scholar] [CrossRef]
- Stolzenberg, H.; Kahl, H.; Bergmann, K.E. Körpermaße bei Kindern und Jugendlichen in Deutschland. Bundesgesundheitsblatt Gesundh. Gesundh. 2007, 50, 659–669. [Google Scholar] [CrossRef] [Green Version]
- Kromeyer-Hauschild, K.; Moss, A.; Wabitsch, M. Referenzwerte für den Body-Mass-Index für Kinder, Jugendliche und Erwachsene in Deutschland. Adipositas-Ursachen Folgeerkrankungen Ther. 2015, 9, 123–127. [Google Scholar] [CrossRef]
- Lier, L.M.; Breuer, C.; Ferrari, N.; Friesen, D.; Maisonave, F.; Schmidt, N.; Graf, C. Cost-effectiveness of a family-based multicomponent outpatient intervention program for children with obesity in Germany. Public Health 2020, 186, 185–192. [Google Scholar] [CrossRef]
- Kromeyer-Hauschild, K.; Wabitsch, M.; Kunze, D.; Geller, F.; Geiß, H.-C.; Hesse, V.; von Hippel, A.; Jaeger, U.; Johnsen, D.; Korte, W. Perzentile für den Body-mass-Index für das Kindes-und Jugendalter unter Heranziehung verschiedener deutscher Stichproben. Mon. Kinderheilkd. 2001, 149, 807–818. [Google Scholar] [CrossRef] [Green Version]
- Schräpler, J.P.; Jeworutzki, S. Konstruktion des Sozialindex für Schulen in Nordrhein-Westfalen, ZEFIR-Materialien. Band 15; Zentrum für interdisziplinäre Regionalforschung (ZEFIR): Bochum, Germany, 2021. [Google Scholar]
- Stadt Köln. Integriertes Handlungskonzept Starke Veedel—Starkes Köln. Available online: https://www.stadt-koeln.de/mediaasset/content/pdf15/starke-veedel/integriertes_handlungskonzept_nach_schlusszeichnung_ob.pdf (accessed on 24 June 2021).
- Paterson, D.C.; Ramage, K.; Moore, S.A.; Riazi, N.; Tremblay, M.S.; Faulkner, G. Exploring the impact of COVID-19 on the movement behaviors of children and youth: A scoping review of evidence after the first year. J. Sport Health Sci. 2021, 10, 675–689. [Google Scholar] [CrossRef]
- Poulain, T.; Meigen, C.; Sobek, C.; Ober, P.; Igel, U.; Körner, A.; Kiess, W.; Vogel, M. Loss of childcare and classroom teaching during the Covid-19-related lockdown in spring 2020: A longitudinal study on consequences on leisure behavior and schoolwork at home. PLoS ONE 2021, 16, e0247949. [Google Scholar] [CrossRef]
- Kelso, A.; Reimers, A.K.; Abu-Omar, K.; Wunsch, K.; Niessner, C.; Wäsche, H.; Demetriou, Y. Locations of Physical Activity: Where Are Children, Adolescents, and Adults Physically Active? A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 1240. [Google Scholar] [CrossRef]
- Tomkinson, G.R.; Carver, K.D.; Atkinson, F.; Daniell, N.D.; Lewis, L.K.; Fitzgerald, J.S.; Lang, J.J.; Ortega, F.B. European normative values for physical fitness in children and adolescents aged 9–17 years: Results from 2 779 165 Eurofit performances representing 30 countries. Br. J. Sports Med. 2018, 52, 1445–14563. [Google Scholar] [CrossRef] [Green Version]
- Škrkar, S.; Madić, D.; Petrović, M. Differences in the motor competence of younger school age children. FU Phys. Ed. Sport 2020, 18, 295–303. [Google Scholar] [CrossRef]
- Cena, H.; Fiechtner, L.; Vincenti, A.; Magenes, V.C.; de Giuseppe, R.; Manuelli, M.; Zuccotti, G.V.; Calcaterra, V. COVID-19 Pandemic as Risk Factors for Excessive Weight Gain in Pediatrics: The Role of Changes in Nutrition Behavior. A Narrative Review. Nutrients 2021, 13, 4255. [Google Scholar] [CrossRef]
- Lampert, T.; Müters, S.; Stolzenberg, H.; Kroll, L.E. Messung des sozioökonomischen Status in der KiGGS-Studie: Erste Folgebefragung (KiGGS Welle 1). Bundesgesundheitsblatt Gesundh. Gesundh. 2014, 57, 762–770. [Google Scholar] [CrossRef]
- Watkins, C.S.; Howard, M.O. Educational success among elementary school children from low socioeconomic status families: A systematic review of research assessing parenting factors. J. Child. Poverty 2015, 21, 17–46. [Google Scholar] [CrossRef]
- Medrano, M.; Cadenas-Sanchez, C.; Oses, M.; Arenaza, L.; Amasene, M.; Labayen, I. Changes in lifestyle behaviours during the COVID-19 confinement in Spanish children: A longitudinal analysis from the MUGI project. Pediatr. Obes. 2021, 16, e12731. [Google Scholar] [CrossRef] [PubMed]





| Total | Cohort A 2016 Pre-Pandemic | Cohort B 2020 Peri-Pandemic | Cohort C 2021 Peri-Pandemic | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| High Burden | Low Burden | High Burden | High Burden | Low Burden | ||||||||
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| N | 1238 | 261 | 210 | 196 | 441 | 130 | ||||||
| female sex % | 599 | 48.4% | 117 | 44.8% | 107 | 51.0% | 100 | 51.0% | 216 | 49.0% | 59 | 45.4% |
| male sex % | 639 | 51.6% | 144 | 55.2% | 103 | 49.0% | 96 | 49.0% | 225 | 51.0% | 71 | 54.6% |
| age (years) | 1238 | 8.1 (1.2) | 261 | 8.3 (1.1) | 210 | 8.1 (1.1) | 196 | 8.3 (1.2) | 441 | 8.0 (1.3) | 130 | 8.3 (1.3) |
| height (cm) | 1238 | 130.9 (9.1) | 261 | 131.3 (8.6) | 210 | 132.2 (8.9) | 196 | 132.3 (9.2) | 441 | 128.9 /9.2) | 130 | 132.1 (8.9) |
| body weight (kg) | 1238 | 30.6 (8.3) | 261 | 30.3 (7.5) | 210 | 29.5 (6.9) | 196 | 32.5 (9.5) | 441 | 30.7 (9.1) | 130 | 29.7 (6.7) |
| BMI (kg/m2) | 1238 | 17.6 (3.2) | 261 | 17.4 (2.8) | 210 | 16.7 (2.4) | 196 | 18.3 (3.6) | 441 | 18.2 (3.6) | 130 | 16.9 (2.3) |
| BMI z score | 1238 | 0.5 (1.1) | 261 | 0.4 (1.0) | 210 | 0.2 (0.9) | 196 | 0.6 (1.3) | 441 | 0.7 (1.2) | 130 | 0.2 (0.9) |
| percentile % | 261 | 210 | 441 | 130 | ||||||||
| underweight | 51 | 4.1% | 9 | 3.4% | 7 | 3.3% | 7 | 3.6% | 19 | 4.3% | 9 | 6.9% |
| normal weight | 883 | 71.3% | 193 | 73.9% | 180 | 85.7% | 130 | 66.3% | 280 | 63.5% | 100 | 76.9% |
| overweight | 162 | 13.1% | 31 | 11.9% | 11 | 5.2% | 34 | 17.3% | 71 | 16.1% | 15 | 11.5% |
| obese | 142 | 11.5% | 28 | 10.7% | 12 | 5.7% | 25 | 12.8% | 71 | 16.1% | 6 | 4.6% |
| social index (level) | 1238 | 5.0 (2.1) | 261 | 5.5 (0.5) | 210 | 2.5 (1.5) | 196 | 6.5 (0.5) | 441 | 6.5 (0.5) | 130 | 1.0 (0.0) |
| motor performance | ||||||||||||
| lateral jumping (counts) | 1232 | 48.1 (17.3) | 261 | 51.3 (17.0) | 209 | 55.4 (0.9) | 196 | 47.1 (14.4) | 437 | 42.3 (17.5) | 129 | 51.2 (17.0) |
| standing long jump (cm) | 1144 | 114.2 (23.5) | 230 | 111.1 (22.0) | 209 | 123.3 (22.0) | 182 | 115.2 (23.0) | 413 | 109.2 (22.9) | 124 | 121.2 (25.1) |
| 6-min run (m) | 1038 | 840.1 (143.8) | 261 | 879.3 (111.0) | 208 | 936.4 (113.6) | N.A. | 439 | 757.9 (133.2) | 130 | 884.3 (132.3) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wessely, S.; Ferrari, N.; Friesen, D.; Grauduszus, M.; Klaudius, M.; Joisten, C. Changes in Motor Performance and BMI of Primary School Children over Time–Influence of the COVID-19 Confinement and Social Burden. Int. J. Environ. Res. Public Health 2022, 19, 4565. https://doi.org/10.3390/ijerph19084565
Wessely S, Ferrari N, Friesen D, Grauduszus M, Klaudius M, Joisten C. Changes in Motor Performance and BMI of Primary School Children over Time–Influence of the COVID-19 Confinement and Social Burden. International Journal of Environmental Research and Public Health. 2022; 19(8):4565. https://doi.org/10.3390/ijerph19084565
Chicago/Turabian StyleWessely, Stefanie, Nina Ferrari, David Friesen, Martin Grauduszus, Marlen Klaudius, and Christine Joisten. 2022. "Changes in Motor Performance and BMI of Primary School Children over Time–Influence of the COVID-19 Confinement and Social Burden" International Journal of Environmental Research and Public Health 19, no. 8: 4565. https://doi.org/10.3390/ijerph19084565






