Therapeutic Patient Education for Fibromyalgia during Spa Therapy: The FiETT Randomized Controlled Trial
Abstract
:1. Introduction
2. Methods
2.1. Design
2.2. Recruitment
2.3. Participants
2.4. Interventions
2.5. Follow-Up
2.6. Outcomes
2.7. Sample Size
2.8. Randomization
2.9. Statistical Methods
2.10. Ethics and Authorizations
3. Results
3.1. Enrolment and Follow-Up
3.2. Patients’ Characteristics
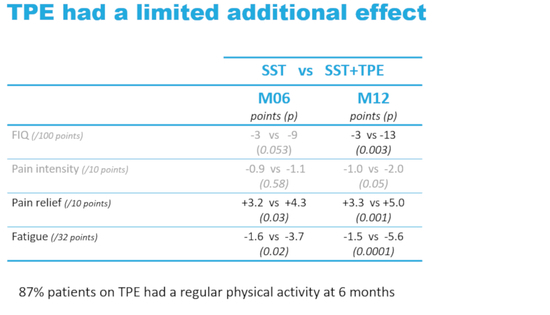
3.3. Fibromyalgia Impact Questionnaire
3.4. Secondary Outcomes
3.5. Adverse Events
3.6. Compliance to Strategies
3.7. Efficacy of Spa Therapy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abreviations
| AFRETh | Association Française de Recherche sur le Thermalisme (French society for thermal spa research) |
| BDI | Beck Depression Inventory |
| CIS | Checklist Individual Strength |
| eCRF | electronic Case Report Form |
| EULAR | European Alliance of Associations for Rheumatology |
| FiETT | Fibromyalgie et Education Thérapeutique en cure Thermale (Fibromyalgia and Therapeutic Education during thermal spa cure) |
| FIQ | Fibromyalgia Impact Questionnaire |
| FIRST | Fibromyalgia Rapid Screening Test |
| GTPS | Graded Tender Point Score |
| HAD | Hospital Anxiety and Depression scale |
| MedDRA | Medical Dictionary for Regulatory Activities |
| mmHg | millimeter of mercury |
| MPQ | McGill Pain Questionnaire |
| PCS | Pain Catastrophizing Scale |
| PSQI | Pittsburgh Sleep Quality Index |
| SE | Standard Error |
| SF-36 | Short Form 36 |
| SOC | System Organ Class |
| SST | Standardized Spa Therapy |
| TSK | Tampa Scale of Kinesiophobia |
| TPE | Therapeutic Patient Education |
| VAS | Visual Analog Scale |
| WOMAC | Western Ontario and McMaster scale |
References
- Davis, F.; Gostine, M.; Roberts, B.; Risko, R.; Cappelleri, J.C.; Sadosky, A. Characterizing classes of fibromyalgia within the continuum of central sensitization syndrome. J. Pain Res. 2018, 11, 2551–2560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gatchel, R.J.; Peng, Y.B.; Peters, M.L.; Fuchs, P.N.; Turk, D.C. The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychol. Bull. 2007, 133, 581–624. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, B.; Baptista, T.M.; Branco, J.C.; Novo, R.F. Fibromyalgia characterization in a psychosocial approach. Psychol. Health Med. 2015, 20, 363–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolfe, F.; Ross, K.; Anderson, J.; Russel, I.J.; Hebert, L. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum. 1995, 38, 19–28. [Google Scholar] [CrossRef]
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.A.; Goldenberg, D.L.; Katz, R.S.; Mease, P.; Russell, A.S.; Russell, I.J. The American college of rheumatology preliminary diagnostic criteria for fibromyalgia and mesuarement of symptom severity. Arthritis Care Res. 2010, 62, 600–610. [Google Scholar] [CrossRef] [Green Version]
- Bondy, B.; Spaeth, M.; Offenbaeher, M.; Glatzeder, K.; Stratz, T.; Schwarz, M.; de Jong, S.; Kruger, M.; Engel, R.R.; Farber, L.; et al. The T102 C polymorphism of the 5-HT2A receptor gene in fibromyalgia. Neurobiol. Dis. 1999, 6, 433–439. [Google Scholar] [CrossRef] [Green Version]
- Buskila, D.; Cohen, H.; Neumann, L.; Ebstein, R.P. An association between fibromyalgia and the dopamine D4 receptor exon III repeat polymorphism and relationship personality traits. Mol. Psychiatry 2004, 9, 730–731. [Google Scholar] [CrossRef]
- Buskila, D.; Abu-Shakra, M.; Neumann, L.; Odes, L.; Shneider, E.; Flusser, D.; Sukenik, S. Balneotherapy for fibromyalgia at the dead sea. Rheumatol. Int. 2001, 20, 105–108. [Google Scholar] [CrossRef]
- Cohen, H.; Buskila, D.; Neumann, L.; Ebstein, R.P. Confirmation of an association between fibromyalgia and serotonin transporter promoter region (5-HTTLPR) polymorphism, and relationship to anxiety related personality traits. Arthritis Rheum. 2002, 46, 845–847. [Google Scholar] [CrossRef] [Green Version]
- Gursoy, S. Absence of association of the serotonin transporter gene polymorphism with the mentally healthy subset of fibromyalgia patients. Clin. Rheumatol. 2002, 21, 194–197. [Google Scholar] [CrossRef]
- Gursoy, S.; Erdal, E.; Herken, H.; Madenci, E.; Ala, B.; Erdal, N. Significance of catechol-O-methyltransferase gene polymorphism in fibromyalgia syndrome. Rheumatol. Int. 2003, 23, 104–107. [Google Scholar] [CrossRef] [PubMed]
- Offenbaecher, M.; Bondy, B.; de Jong, S.; Glatzeder, K.; Kruger, M.; Schoeps, P.; Ackenheil, M. Possible association of fibromyalgia with a polymorphism in the regulatory region. Arthritis Rheum. 1999, 42, 2482–2488. [Google Scholar] [CrossRef]
- Zubieta, J.K.; Heitzeg, M.M.; Smith, Y.R.; Bueller, J.A.; Xu, K.; Xu, Y.; Koeppe, R.A.; Stohler, C.S.; Goldman, D. COMT val158met genotype affects mu-opioid neurotransmitter responses to a pain stressor. Science 2003, 299, 1240–1243. [Google Scholar] [CrossRef] [PubMed]
- Thieme, K.; Turk, D.C.; Flor, H. Comorbid depression and anxiety in fibromyalgia syndrome: Relationship to somatic and psychosocial variables. Psychosom. Med. 2004, 66, 837–844. [Google Scholar] [CrossRef]
- Perrot, S.; Vicaut, E.; Servant, D.; Ravaud, P. Prevalence of fibromyalgia in France: A multi-step study research combining national screening and clinical confirmation: The DEFI study (Determination of Epidemiology of Fibromyalgia). BMC Musculoskelet. Disord. 2011, 12, 224. [Google Scholar] [CrossRef]
- Branco, J.C.; Bannwarth, B.; Failde, I.; Abello Carbonell, J.; Blotman, F.; Spaeth, M.; Saraiva, F.; Nacci, F.; Thomas, E.; Caubère, J.P.; et al. Prevalence of fibromyalgia: A survey in five European countries. Semin. Arthritis Rheum. 2010, 39, 448–453. [Google Scholar] [CrossRef]
- Katz, R.S.; Wolfe, F.; Michaud, K. Fibromyalgia diagnostic. A comparison of clinical survey and American college of rheumatology criteria. Arthritis Rheum. Off. J. Am. Coll. Rheumatol. 2006, 54, 169–176. [Google Scholar] [CrossRef]
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.A.; Goldenberg, D.L.; Häuser, W.; Katz, R.L.; Mease, P.J.; Russell, A.S.; Russell, I.J.; Walitt, B. Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin. Arthritis Rheum. 2016, 46, 319–329. [Google Scholar] [CrossRef]
- Häuser, W.; Brähler, E.; Ablin, J.; Wolfe, F. Modified 2016 American College of Rheumatology Fibromyalgia Criteria, the Analgesic, Anesthetic, and Addiction Clinical Trial Translations Innovations Opportunities and Networks—American Pain Society Pain Taxonomy, and the Prevalence of Fibromyalgia. Arthritis Care Res. 2021, 73, 617–625. [Google Scholar] [CrossRef]
- Carville, S.F.; Arendt-Nielsen, S.; Bliddal, H.; Blotman, F.; Branco, J.C.; Buskila, D.; Da Silva, J.A.P.; Danneskiold-Samsøe, B.; Dincer, F.; Henriksson, C.; et al. EULAR evidence based recommendations for the management of fibromyalgia syndrome. Ann. Rheum. Dis. 2008, 67, 536–541. [Google Scholar] [CrossRef]
- Kori, S.H.; Miler, R.P.; Todd, D.D. Kinesiophobia: A new view of chronic pain behaviour. Pain Manag. 1990, 3, 35–43. [Google Scholar]
- Wolfe, F.; Walitt, B.T.; Katz, R.S.; Lee, Y.C.; Michaud, K.D.; Häuser, W. Longitudinal patterns of analgesic and central acting drug use and associated effectiveness in fibromyalgia. Eur. J. Pain 2013, 17, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Ablin, J.N.; Häuser, W.; Buskila, D. Spa Treatment (Balneotherapy) for Fibromyalgia—A Qualitative-Narrative Review and a Historical Perspective. Evid. Based Complement. Altern. Med. 2013, 2013, 638050. [Google Scholar] [CrossRef] [PubMed]
- De Andrade, C.S.; Pereira Pessoa de Carvalho, R.F.; Soares, A.S.; de Abreu Freitas, R.P.; de Medeiros Guerra, L.M.; Vilar, M.J. Thalassotherapy for fibromyalgia: A randomized controlled trial comparing aquatic exercises in sea water and water pool. Rheumatol. Int. 2008, 29, 147–152. [Google Scholar] [CrossRef]
- Dönmez, A.; Karagülle, M.Z.; Tercan, N.; Dinler, M.; İşsever, H.; Karagülle, M.; Turan, M. SPA therapy in fibromyalgia: A randomised controlled clinic study. Rheumatol. Int. 2005, 26, 168–172. [Google Scholar] [CrossRef]
- Eröksüz, R.; Erol-Forestier, F.B.; Karaaslan, F.; Forestier, R.; İşsever, H.; Erdoğan, N.; Karagülle, M.Z.; Dönmez, A. Comparison of intermittent and consecutive balneological outpatient treatment (hydrotherapy and peloidotherapy) in fibromyalgia syndrome: A randomized, single-blind, pilot study. Int. J. Biometeorol. 2020, 64, 513–520. [Google Scholar] [CrossRef]
- Evcik, D.; Kizilay, B.; Gökçen, E. The effects of balneotherapy on fibromyalgia patients. Rheumatol. Int. 2002, 22, 56–59. [Google Scholar] [CrossRef]
- Falagas, M.E.; Zarkadoulia, E.; Rafailidis, P.I. The therapeutic effect of balneotherapy: Evaluation of the evidence from randomised controlled trials. Int. J. Clin. Pract. 2009, 63, 1068–1084. [Google Scholar] [CrossRef]
- Fioravanti, A.; Manica, P.; Bortolotti, R.; Cevenini, G.; Tenti, S.; Paolazzi, G. Is balneotherapy effective for fibromyalgia? Results from a 6-month double blind randomized clinical trial. Clin. Rheumatol. 2018, 37, 2203–2212. [Google Scholar] [CrossRef]
- Fioravanti, A.; Perpignano, G.; Tirri, G.; Cardinale, G.; Gianniti, C.; Lanza, C.E.; Loi, A.; Tirri, E.; Sfriso, P.; Cozzi, F. Effects of mud-bath treatment on fibromyalgia patients: A randomized clinical trial. Rheumatol. Int. 2007, 27, 1157–1161. [Google Scholar] [CrossRef]
- Kesiktas, N.; Karagülle, Z.; Erdogan, N.; Yazıcıoglu, K.; Yılmaz, H.; Paker, N. The efficacy of balneotherapy and physical modalities on the pulmonary system of patients with fibromyalgia. J. Back Musculoskelet. Rehabil. 2011, 24, 57–65. [Google Scholar] [CrossRef] [PubMed]
- McVeigh, J.G.; McGaughey, H.; Hall, M.; Kane, P. The effectiveness of hydrotherapy in the management of fibromyalgia syndrome: A systematic review. Rheumatol. Int. 2008, 29, 119–130. [Google Scholar] [CrossRef] [PubMed]
- Neira, R.; Marques, P.; Pérez, P.; Cervantes, F.; Costa, V. Effectiveness of Aquatic Therapy vs Land-based Therapy for Balance and Pain in Women with Fibromyalgia: A study protocol for a randomised controlled trial. BMC Musculoskelet. Disord. 2017, 19, 22. [Google Scholar] [CrossRef]
- Neumann, L.; Sukenik, S.; Bolotin, A.; Abu Shakra, M.; Amir, M.; Flusser, M.; Buskila, D. The effect of balneotherapy at the Dead Sea on the quality of life of patients with fibromyalgia syndrome. Clin. Rheumatol. 2001, 20, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Ozkurt, S.; Dönmez, A.; Zeki Karagülle, M.; Uzunoğlu, E.; Turan, M.; Erdoğan, N. Balneotherapy in fibromyalgia: A single blind randomized controlled clinical study. Rheumatol. Int. 2012, 32, 1949–1954. [Google Scholar] [CrossRef]
- Zamunér, A.R.; Andrade, C.P.; Arca, E.A.; Avila, M.A. Impact of water therapy on pain management in patients with fibromyalgia: Current perspectives. J. Pain Res. 2019, 12, 1971–2007. [Google Scholar] [CrossRef] [Green Version]
- Ardiç, F.; Ozgen, M.; Aybek, H.; Rota, S.; Cubukçu, D.; Gökgöz, A. Effects of balneotherapy on serum IL-1, PGE2 and LTB4 levels in fibromyalgia patients. Rheumatol. Int. 2007, 27, 441–446. [Google Scholar] [CrossRef]
- Zijlstra, T.R.; Van de Laar, M.A.; Bernelot Moens, H.J. Spa treatment for primary fibromyalgia syndrome: A combination of thalassotherapy, exercise and patient education improves symptoms and quality of life. Rheumatology 2005, 44, 539–546. [Google Scholar] [CrossRef] [Green Version]
- Silva, A.; Queiroz, S.S.; Andersen, M.L.; Mônico-Neto, M.; Campos, R.M.; Roizenblatt, S.; Tufik, S.; Mello, M.T. Passive body heating improves sleep patterns in female patients with fibromyalgia. Clinics 2013, 68, 135–140. [Google Scholar] [CrossRef]
- Bidonde, J.; Busch, A.J.; Webber, S.C.; Schachter, C.L.; Danyliw, A.; Overend, T.J.; Richards, R.S.; Rader, T. Aquatic exercise training for fibromyalgia. Cochrane Database Syst. Rev. 2014, 10, 10–28. [Google Scholar] [CrossRef]
- Cao, C.F.; Ma, K.L.; Li, Q.L.; Luan, F.J.; Wang, Q.B.; Zhang, M.H.; Viswanath, O.; Myrcik, D.; Varrassi, G.; Wang, H.Q. Balneotherapy for Fibromyalgia Syndrome: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 1493. [Google Scholar] [CrossRef] [PubMed]
- Fraioli, A.; Grassi, M.; Mennuni, G.; Geraci, A.; Petraccia, L.; Fontana, M.; Conte, S.; Serio, A. Clinical researches on the efficacy of spa therapy in fibromyalgia. A systematic review. Ann. Dell’istituto Super. Sanità 2013, 49, 219–229. [Google Scholar]
- Giacomelli, C.; Sernissi, F.; Sarzi-Putini, P.; Di Franco, M.; Atzeni, F.; Bazzichi, L. Fibromyalgia: A critical digest of the recent literature. Clin. Exp. Rheumatol. 2013, 31, S153–S157. [Google Scholar] [PubMed]
- Giannotti, E.; Koutsikos, K.; Pigatto, M.; Rampudda, M.E.; Doria, A.; Masiero, S. Medium-/long-term effects of a specific exercise protocol combined with patient education on spine mobility, chronic fatigue, pain, aerobic fitness and level of disability in fibromyalgia. Biomed. Res. Int. 2014, 2014, 474029. [Google Scholar] [CrossRef]
- Guidelli, G.M.; Tenti, S.; De Nobili, E.; Fioravanti, A. Fibromyalgia syndrome and spa therapy: Myth or reality? Clin. Med. Insights Arthritis Musculoskelet. Disord. 2012, 5, 19–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Langhorst, J.; Musai, F.; Klose, P.; Haüser, W. Efficacy of hydrotherapy in fibromyalgia syndrome—A meta-analysis of randomized controlled trials. Rheumatology 2009, 48, 1155–1159. [Google Scholar] [CrossRef] [Green Version]
- Naumann, J.; Sadaghiani, C. Therapeutic benefit of balneotherapy and hydrotherapy in the management of fibromyalgia syndrome: A qualitative systematic review and meta-analysis of randomized controlled trials. Arthritis Res. Ther. 2014, 16, R141. [Google Scholar] [CrossRef] [Green Version]
- Roques, C.F.; Queneau, P. Spa therapy for pain of patients with chronic low back pain, knee osteoarthritis and fibromyalgia. Bull. L’academie Natl. Med. 2016, 200, 575–587. [Google Scholar]
- World Health Organization; Regional Office for Europe, Slama-Chaudhry, Anbreen & Golay, Alain. Patient education and self-management support for chronic disease: Methodology for implementing patient-tailored therapeutic programmes. Public Health Panor. 2019, 5, 357–361. [Google Scholar]
- Hammond, A.; Freeman, K. Community patient education and exercise for people with fibromyalgia: A parallel group randomized controlled trial. Clin. Rehabil. 2006, 20, 835–846. [Google Scholar] [CrossRef]
- Ittersum van, M.W.; Wilgen van, C.P.; der Schans van, C.P.; Lambrecht, L.; Groothoff, J.W.; Nijs, J. Written pain neuroscience education in fibromyalgia: A multicenter randomized controlled trial. Pain Pract. 2014, 14, 689–700. [Google Scholar] [CrossRef] [PubMed]
- Karper, W.B. Effects of exercise, patient education, and resource support on women with fibromyalgia: An extended long-term study. J. Women Aging 2016, 28, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Nam, S.; Tin, D.; Bain, L.; Thorne, J.C.; Ginsburg, L. Clinical utility of the Hospital Anxiety and Depression Scale (HADS) for an outpatient fibromyalgia education program. Clin. Rheumatol. 2014, 33, 685–692. [Google Scholar] [CrossRef] [PubMed]
- Oh, T.H.; Hoskin, T.L.; Luedtke, C.A.; Weingarten, T.N.; Vincent, A.; Kim, C.H.; Thompson, J.M. Predictors of clinical outcome in fibromyalgia after a brief interdisciplinary fibromyalgia treatment program: Single center experience. PM&R 2012, 4, 257–263. [Google Scholar]
- Bagdatli, A.O.; Donmez, A.; Eröksüz, R.; Bahad1r, G.; Turan, M.; Erdogan, N. Does addition of ‘mud-pack and hot pool treatment’ to patient education make a difference in fibromyalgia patients? A randomized controlled single blind study. Int. J. Biometeorol. 2015, 59, 1905–1911. [Google Scholar] [CrossRef]
- Koçyigit, B.F.; Gür, A.; Altindag, O.; Akyol, A.; Gursoy, S. Comparison of education and balneotherapy efficacy in patients with fibromyalgia syndrome: A randomized, controlled clinical study. Agri 2016, 28, 72–78. [Google Scholar] [CrossRef]
- Camerini, L.; Camerini, A.L.; Schulz, P.J. Do participation and personalization matter? A model-driven evaluation of an Internet-based patient education intervention for fibromyalgia patients. Patient Educ. Couns. 2013, 92, 229–234. [Google Scholar] [CrossRef]
- Perrot, S.; Bouhassira, D.; Fermanian, J.; Cercle d’Etude de la Douleur en Rhumatologie. Development and validation of the Fibromyalgia Rapid Screening tool (FiRST). Pain 2010, 150, 250–256. [Google Scholar] [CrossRef]
- Gendreau, R.M.; Arnold, L.; Clauw, D.J.; Gendreau, J.; Daugherty, B.; Lederman, S. Novel Composite Responder Endpoints for Fibromyalgia Therapy Assessment. Arthritis Rheumatol. 2016, 68 (Suppl. 10). [Google Scholar]
- Mease, P.J.; Clauw, D.J.; Christensen, R.; Crofford, L.J.; Gendreau, R.M.; Martin, S.A.; Simon, L.S.; Strand, V.; Williams, D.A.; Arnold, L.M.; et al. Toward development of a fibromyalgia responder index and disease activity score: OMERACT module update. J. Rheumatol. 2011, 38, 1487–1495. [Google Scholar] [CrossRef] [Green Version]
- Burckhardt, C.S.; Clark, S.R.; Bennett, R.M. The Fibromyalgia Impact Questionnaire: Development and validation. J. Rheumatol. 1991, 18, 728–733. [Google Scholar] [PubMed]
- Perrot, S.; Dumont, D.; Guillemin, F.; Pouchot, J.; Coste, J.; For the French Group of Quality of Life Research. Quality of life in women with fibromyalgia syndrome: Validation of the QIF, the French version of the fibromyalgia impact questionnaire. J. Rheumatol. 2003, 30, 1054–1059. [Google Scholar] [PubMed]
- Huskisson, E.C. Measurement of pain. Lancet 1974, 2, 1127–1131. [Google Scholar] [CrossRef]
- Price, D.D.; McGrath, P.A.; Rafii, A.; Buckingham, B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 1983, 17, 45–56. [Google Scholar] [CrossRef]
- Koçyigit, B.F.; Okyay, R.A. The relationship between body mass index and pain, disease activity, depression and anxiety in women with fibromyalgia. PeerJ 2018, 6, e4917. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vlaeyen, J.W.S.; Kole-Snijders, A.M.J.; Rotteveel, A.M.; Rueslink, R.; Heuts, P.H.T.G. The rôle of fear of mouvement/(re)injury in pain disability. J. Occup. Rehabil. 1995, 5, 235–252. [Google Scholar] [CrossRef]
- Vlaeyen, J.W.S.; Kole-Snijders, A.M.J.; Boeren, R.G.B.; Ruesink, R.; Van Eek, H. Fear of mouvement/(re)injury in chronic low back problem and its relations to behavioral performance. Pain 1995, 62, 363–372. [Google Scholar] [CrossRef]
- Sullivan, M.J.L.; Bishop, S.R.; Pivik, J. The pain catastrophizing scale: Development and validation. Psychol. Assess. 1995, 7, 524–532. [Google Scholar] [CrossRef]
- Bellamy, N.; Buchanan, W.W.; Goldsmith, C.H.; Campbell, J.; Stitt, L.W.J. Validation of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J. Rheumatol. 1995, 15, 1833–1840. [Google Scholar]
- Pichot, P.; Brun, J.P. Brief self-evaluation questionnaire for depressive, asthenic and anxious dimensions [in French]. Ann. Med. Psychol. 1984, 142, 862–865. [Google Scholar]
- Johns, M.W. A new method for measuring day time sleepiness: The Epworth Sleepiness Scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Macfarlane, G.J.; Kronisch, C.; Dean, L.E.; Atzeni, F.; Häuser, W.; Fluß, E.; Choy, E.; Kosek, E.; Amris, K.; Branco, J.; et al. Eular revisited recommendations for the management of fibromyalgia. Ann. Rheum. Dis. 2017, 76, 318–328. [Google Scholar] [CrossRef] [PubMed]
- Bennett, R.M.; Bushmakin, A.G.; Cappelleri, J.C.; Zlateva, G.; Sadosky, A.B. Minimal clinically important difference in the fibromyalgia impact questionnaire. J. Rheumatol. 2009, 36, 1304–1311. [Google Scholar] [CrossRef] [PubMed]
- Maindet, C.; Maire, A.; Vermorel, C.; Cracowski, C.; Rolland, C.; Forestier, R.; Comte, A.; Roques, C.F.; Serra, E.; Bosson, J.L. Spa Therapy for the Treatment of Fibromyalgia: An Open, Randomized Multicenter Trial. J. Pain 2021, 22, 940–951. [Google Scholar] [CrossRef]
- Hanh, T.; Serog, P.; Fauconnier, J.; Batailler, P.; Mercier, F.; Roques, C.F.; Blin, P. One-year effectiveness of a 3-week balneotherapy program for the treatment of overweight or obesity. Evid. Based Complement. Altern. Med. 2012, 2012, 150839. [Google Scholar] [CrossRef]
- Schnebelen-Berthier, C.; Negro, N.; Jaruga, A.; Roques, C.F.; Lecerf, J.M. Long term effect of spa therapy combined with patient education program on subjects with overweight and obesity—A controlled study. Obes. Res. Clin. Pract. 2019, 13, 492–498. [Google Scholar] [CrossRef]
- Kundakci, B.; Kaur, J.; Shim, S.R.; Hall, M.; Doherty, M.; Zhang, W.; Abhishek, A. THU0461 The comparative efficacy of non-pharmacological interventions for fibromyalgia: A systematic review with bayesian network meta-analysis. Ann. Rheum. Dis. 2020, 79, 467–468. [Google Scholar] [CrossRef]
- Carrera, B.G.; Segura-Jiménez, V.; Acosta-Manzano, P.; Estevez-Lopez, F.; Cosic, M.B.; Aparicio, V.A.; Carbonell-Baeza, A.; Delgado-Fernández, M. OP0101 Comparative effectiveness of land and water-based exercise on quality of life of patients with fibromyalgia: Preliminary findings from the al-ándalus randomised controlled trial. Ann. Rheum. Dis. 2018, 76, 318–328. [Google Scholar]
- Rivas Neira, S.; Pasqual Marques, A.; Vivas Costa, J. AB0957 Is aquatic therapy more effective than land-based therapy in reducing pain of women with fibromyalgia? Ann. Rheum. Dis. 2020, 79, 1775–1776. [Google Scholar] [CrossRef]
- Cohen, H.; Neumann, L.; Alhosshle, A.; Kotler, M.; Abu-Shakra, M.; Buskila, D. Abnormal sympathovagal balance in men with fibromyalgia. J. Rheumatol. 2001, 28, 581–589. [Google Scholar] [PubMed]
- Giske, L.; Vøllestad, N.K.; Mengshoel, A.M.; Jensen, J.; Knardahl, S.; Røe, C. Attenuated adrenergic responses to exercise in women with fibromyalgia—A controlled study. Eur. J. Pain 2008, 12, 351–360. [Google Scholar] [CrossRef] [PubMed]
- Naschitz, J.E.; Rozenbaum, M.; Fields, M.C.; Enis, S.; Manor, H.; Dreyfuss, D.; Peck, S.; Peck, E.R.; Babich, J.P.; Mintz, E.P.; et al. Cardiovascular reactivity in fibromyalgia: Evidence for pathogenic heterogeneity. J. Rheumatol. 2005, 32, 335–339. [Google Scholar] [PubMed]
- Bruehl, S.; Chung, O.Y.; Jirjis, J.N.; Biridepalli, S. Prevalence of clinical hypertension in patients with chronic pain compared to nonpain general medical patients. Clin. J. Pain 2005, 21, 147–153. [Google Scholar] [CrossRef]
- Olsen, R.B.; Bruehl, S.; Nielsen, C.S.; Rosseland, L.A.; Eggen, A.E.; Stubhaug, A. Hypertension prevalence, and diminished blood pressure-related hypoalgesia in individuals reporting chronic pain in a general population: The Tromso study. Pain 2013, 154, 257–262. [Google Scholar] [CrossRef]
- Zamunér, A.R.; Porta, A.; Pieroni Andrade, C.; Marchi, A.; Forti, M.; Furlan, R.; Barbic, F.; Catai, A.M.; Silva, E. Cardiovascular control in women with fibromyalgia syndrome: Do causal methods provide nonredundant information compared with more traditional approaches? Am. J. Physiol. Regul. Integr. Comp. Physiol. 2015, 309, R79–R84. [Google Scholar] [CrossRef] [Green Version]
- Ducher, M.; Fauvel, J.P.; Cerutti, C. Risk profile in hypertension genesis: A five-year follow-up study. Am. J. Hypertens. 2006, 19, 775–780. [Google Scholar] [CrossRef]
- Jackson, T.; Thomas, S.; Stabile, V.; Han, X.; Shotwell, M.; McQueen, K. Prevalence of chronic pain in low-income and middle-income countries: A systematic review and meta-analysis. Lancet 2015, 385, S10. [Google Scholar] [CrossRef] [Green Version]
- Kang, J.H.; Park, D.J.; Kim, S.H.; Nah, S.S.; Lee, J.H.; Kim, S.K.; Lee, Y.A.; Hong, S.J.; Kim, H.S.; Lee, H.S.; et al. Severity of fibromyalgia symptoms is associated with socioeconomic status and not obesity in Korean patients. Clin. Exp. Rheumatol. 2016, 34, S83. [Google Scholar]
- Correa-Rodríguez, M.; El Mansouri-Yachou, J.; Casas-Barragán Molina, F.; Rueda-Medina, B.; Aguilar-Ferrándiz, M.E. The Association of Body Mass Index and Body Composition with Pain, Disease Activity, Fatigue, Sleep and Anxiety in Women with Fibromyalgia. Nutrients 2019, 11, 1193. [Google Scholar] [CrossRef] [Green Version]
- Rusu, C.; Gee, M.E.; Lagace, C.; Parlor, M. Chronic fatigue syndrome and fibromyalgia in Canada: Prevalence and associations with six health status indicators. Health Promot. Chronic Dis. Prev. Can. 2015, 35, 3–11. [Google Scholar] [CrossRef] [PubMed]

| Randomized Strategy | ||||
|---|---|---|---|---|
| SST N = 78 | SST + TPE N = 79 | |||
| Gender | # (%) | Female | 73 (94) | 76 (96) |
| Age (years) | # (%) | [25–40] [40–60] [60–65] | 5 (6) 60 (77) 13 (17) | 6 (10) 54 (68) 19 (24) |
| Monthly net taxable income at baseline (€) * | # (%) | Unknown <1000 1000–1999 ≥2000 | 23 (29) 26 (33) 29 (37) | 5 (6) 18 (23) 29 (37) 27 (34) |
| Socio-professional category | # (%) | Craftsperson, merchant, entrepreneur High-level executive, intellectual professional Employee Retired Other | 11 (14) 10 (13) 38 (49) 6 (8) 13 (17) | 2 (3) 11 (14) 40 (51) 8 (10) 18 (23) |
| Body mass index (kg/m2) | # (%) | [17–25] [25–30] [30–42] | 38 (49) 24 (31) 16 (21) | 42 (53) 18 (23) 19 (24) |
| Blood pressure | Mean (SE) | Systolic Diastolic | 125 (1) 71 (1) | 124 (1) 70 (1) |
| Patients with history medical event per MedDRA System Organ Class | # (%) | Musculoskeletal and connective Surgery tissue disorders Others | 16 (21) 25 (32) | 14 (18) 22 (28) |
| Gastrointestinal disorders Appendectomy Others | 10 (13) 16 (21) | 12 (15) 11 (14) | ||
| Vascular disorders | 13 (17) | 11 (14) | ||
| Nervous system disorders | 11 (14) | 11 (14) | ||
| Reproductive system and breast disorders | 10 (13) | 7 (9) | ||
| Endocrine disorders Thyroid Diabetes | 8 (10) 2 (3) | 11 (14) 3 (4) | ||
| Psychiatric disorders Depression Others | 16 (15) 1 (1) | 6 (8) | ||
| Others | 32 (41) | 30 (38) | ||
| None declared | 20 (26) | 27 (34) | ||
| Fibromyalgia Rapid Screening Tool | # (%) | 5 6 | 14 (18) 64 (82) | 10 (13) 69 (87) |
| Fibromyalgia Impact Questionnaire (%) | # (%) | Missing [0–45] [45–55] [55–65] [65–75] [75–100] | 4 (5) 12 (15) 10 (13) 29 (37) 15 (4) 8 (2) | 17 (22) 10 (13) 18 (23) 22 (6) 12 (3) |
| Fibromyalgia Impact Questionnaire | Mean (SE) | 60 (13) | 60 (16) | |
| Pain intensity (Visual Analog Scale) | Mean (SE) | 7 (0) | 7 (0) | |
| Kinesiophobia (Tampa Scale) | Mean (SE) | 36 (1) | 35 (1) | |
| Pain Catastrophizing (Pain Catastrophizing Scale) | Mean (SE) | 27 (1) | 25 (2) | |
| Rumination | Mean (SE) | 9 (0) | 8 (0) | |
| Magnification | Mean (SE) | 5 (0) | 5 (0) | |
| Helplessness | Mean (SE) | 14 (1) | 12 (1) | |
| Functional limitation due to arthritis (WOMAC scale) | Mean (SE) | 36 (1) | 36 (1) | |
| Fatigue (Pichot scale) | Mean (SE) | 23 (1) | 24 (1) | |
| Sleepiness (Epworth scale) | Mean (SE) | 12 (1) | 12 (1) | |
| Anxiety (Hospital Anxiety and Depression scale) | Mean (SE) | 12 (1) | 13 (0) | |
| Depression (Hospital Anxiety and Depression scale) | Mean (SE) | 10 (1) | 8 (1) | |
| Patients with non-pharmaceutical treatment for fibromyalgia compliant with EULAR 2016 | # (%) | None declared Recommended only At least one discouraged | 16 (21) 5 (6) 57 (73) | 25 (32) 7 (9) 47 (59) |
| Patients with drugs for fibromyalgia compliant with EULAR 2016 | # (%) | None declared Recommended only At least one discouraged | 13 (17) 51 (65) 14 (18) | 14 (18) 51 (65) 14 (18) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ducamp, P.; Sichère, P.; Gayum, H.; Dubourg, K.; Roques, C.-F.; Journot, V. Therapeutic Patient Education for Fibromyalgia during Spa Therapy: The FiETT Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 4613. https://doi.org/10.3390/ijerph19084613
Ducamp P, Sichère P, Gayum H, Dubourg K, Roques C-F, Journot V. Therapeutic Patient Education for Fibromyalgia during Spa Therapy: The FiETT Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2022; 19(8):4613. https://doi.org/10.3390/ijerph19084613
Chicago/Turabian StyleDucamp, Philippe, Patrick Sichère, Hermine Gayum, Karine Dubourg, Christian-François Roques, and Valérie Journot. 2022. "Therapeutic Patient Education for Fibromyalgia during Spa Therapy: The FiETT Randomized Controlled Trial" International Journal of Environmental Research and Public Health 19, no. 8: 4613. https://doi.org/10.3390/ijerph19084613
APA StyleDucamp, P., Sichère, P., Gayum, H., Dubourg, K., Roques, C.-F., & Journot, V. (2022). Therapeutic Patient Education for Fibromyalgia during Spa Therapy: The FiETT Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 19(8), 4613. https://doi.org/10.3390/ijerph19084613