The Effectiveness of Learning to Use HMD-Based VR Technologies on Nursing Students: Chemoport Insertion Surgery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Participants
2.3. Tools
2.3.1. Knowledge
2.3.2. Learning Attitude
2.3.3. Satisfaction with Self-Practice
2.3.4. Learning Motivation
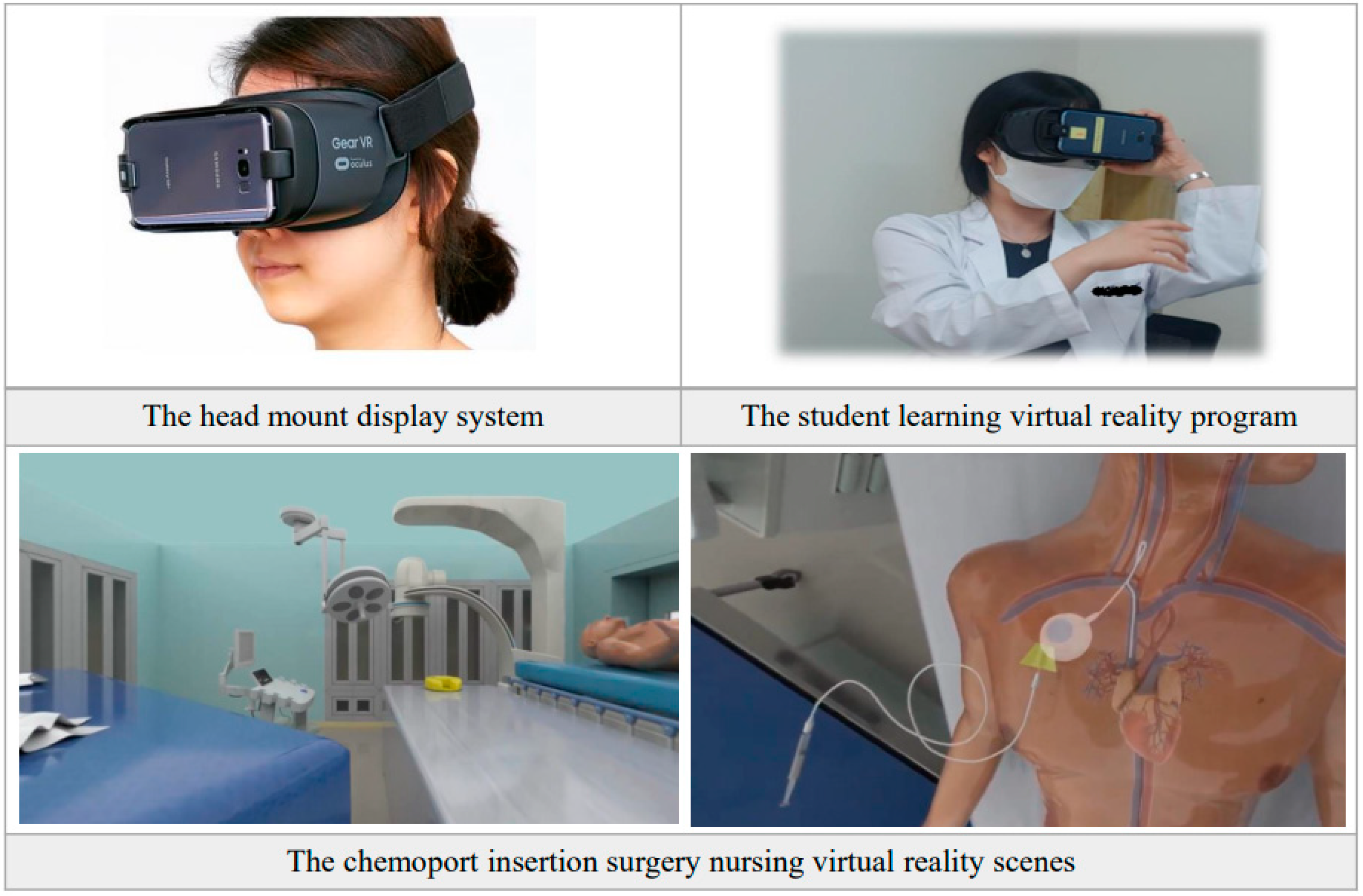
2.4. Intervention
2.4.1. Intervention Development Process
- Step 1: First, the overall scenario was constructed through a literature review for content development. Second, one surgeon and one surgical nurse with extensive experience in Chemoport insertion surgery were interviewed for information on Chemoport insertion surgery indications, surgical procedures, necessary supplies and equipment, essential knowledge, and precautions. Third, the angiography room and surgical equipment, instruments, and items were observed. The surgery was observed several times to complete the scenario.
- Step 2: After creating a storyboard and scenario for Chemoport insertion, the contents were reviewed by the surgeon and operating nurse for revision.
- Step 3: Resource 3D modeling (using Autodesk 3DS Max for 3D modeling and rendering, and Pixologic ZBrush for sculpting and 3D modeling) and voice scripts were developed.
- Step 4: Each scene was created with 3D animation (3DS Max).
- Step 5: VR rendering (using the Arnold renderer in 3DS Max) was conducted for each scene.
- Step 6: After organizing the scenes in an appropriate order, the audio script and video were matched (using Adobe After Effects for video and effect production).
- Step 7: After checking the development contents, usability was verified by three operating nurses working in tertiary general hospitals with more than 10 years of experience. Ease of use and student satisfaction were evaluated, and the final revision of the contents was conducted based on the feedback.
- Step 8: The HMD-based VRP was applied to nursing students and evaluated. It proceeded in stages of pre-briefing, learning, debriefing, and pre-post survey.
2.4.2. Intervention Application and Data Collection
2.5. Ethical Considerations
2.6. Data Analysis
3. Results
3.1. Participant Characteristics and Baseline Test of Homogeneity
3.2. HMD-Based VRP Effect Evaluation
3.2.1. Knowledge
3.2.2. Learning Attitude
3.2.3. Satisfaction with Self-Practice
3.2.4. Learning Motivation
3.3. The Instructor-Led Debriefing
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shin, S.; Park, J.H.; Kim, J.H. Effectiveness of patient simulation in nursing education: Meta-analysis. Nurse Educ. Today 2015, 35, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Taylor, C. Problem solving in clinical nursing practice. J. Adv. Nurs. 1997, 26, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.B.; Williams, B.A.; Fang, J.B.; Ye, Q.H. A systematic review of selected evidence on improving knowledge and skills through high-fidelity simulation. Nurse Educ. Today 2012, 32, 294–298. [Google Scholar] [CrossRef] [PubMed]
- Dubovi, I.; Levy, S.T.; Dagan, E. Now I know how! The learning process of medication administration among nursing students with non-immersive desktop virtual reality simulation. Comput. Educ. 2017, 113, 16–27. [Google Scholar] [CrossRef]
- Lim, K.C. Directions of simulation-based learning in nursing practice education: A systematic review. J. Korean Acad. Soc. Nurs. Educ. 2011, 17, 246–256. [Google Scholar] [CrossRef] [Green Version]
- Blum, C.A.; Borglund, S.; Parcells, D. High-fidelity nursing simulation: Impact on student self-confidence and clinical competence. Int. J. Nurs. Educ. Sch. 2010, 7, 18. [Google Scholar] [CrossRef] [PubMed]
- Cooper, J.B.; Taqueti, V.R. A brief history of the development of mannequin simulators for clinical education and training. Qual Saf. Health Care 2004, 13 (Suppl. S1), i11–i18. [Google Scholar] [CrossRef] [PubMed]
- Prensky, M. Digital natives, digital Immigrants. Horizon 2001, 9. [Google Scholar] [CrossRef] [Green Version]
- Yoo, S.Y. Development and effects of a simulation-based education program for newborn emergency care. J. Korean Acad. Nurs. 2013, 43, 468. [Google Scholar] [CrossRef]
- Lee, M.-J.; Jung, D. The impact of a simulation-based education program for emergency airway management on self-efficacy and clinical performance among nurses. Sŏngin Kanho Hakhoe Chi 2014, 26, 1. [Google Scholar] [CrossRef]
- Choi, E.H.; Kwon, K.N.; Lee, E.J. Achievements of nursing students among simulation and traditional education of bleeding patients. J. Korean Acad. Soc. Nurs. Educ. 2013, 19, 52–59. [Google Scholar] [CrossRef] [Green Version]
- Cant, R.P.; Cooper, S.J. Simulation in the internet age: The place of web-based simulation in nursing education. An integrative review. Nurse Educ. Today 2014, 34, 1435–1442. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.J. Development and evaluation of a simulation-based education course for nursing students. Korean J. Adult Nurs. 2008, 20, 548–560. [Google Scholar]
- Montemurro, N.; Condino, S.; Cattari, N.; D’Amato, R.; Ferrari, V.; Cutolo, F. Augmented reality-assisted craniotomy for parasagittal and convexity en Plaque Meningiomas and Custom-Made Cranio-Plasty: A preliminary laboratory report. Int. J. Environ. Res. Public Health 2021, 18, 9955. [Google Scholar] [CrossRef] [PubMed]
- Serino, S.; Pedroli, E.; Keizer, A.; Triberti, S.; Dakanalis, A.; Pallavicini, F.; Chirico, A.; Riva, G. Virtual reality body swapping: A tool for modifying the allocentric memory of the body. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Liaw, S.Y.; Chan, S.W.C.; Chen, F.G.; Hooi, S.C.; Siau, C. Comparison of virtual patient simulation with mannequin-based simulation for improving clinical performances in assessing and managing clinical deterioration: Randomized controlled trial. J. Med. Internet Res. 2014, 16, e214. [Google Scholar] [CrossRef] [Green Version]
- Jeffries, P. Simulation in Nursing Education: From Conceptualization to Evaluation; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2020. [Google Scholar]
- Choi, J.H. The future of education and culture industry through virtual reality. Future Horiz. 2016, 29, 20–23. [Google Scholar]
- Jenson, C.E.; Forsyth, D.M. Virtual reality simulation: Using three-dimensional technology to teach nursing students. Comput Inform. Nurs. 2012, 30, 312–318. [Google Scholar] [CrossRef] [Green Version]
- Kang, S.; Kim, C.; Lee, H.S.; Nam, J.W.; Park, M.S. Integrative review on nursing education: Adopting virtual reality convergence simulation. J. Converg. Inf. Technol. 2020, 10, 60–74. [Google Scholar] [CrossRef]
- Kang, K.H. The Effect of Appraisal Effectiveness on the Organizational Performance of Perioperative Nursing Department. Unpublished Ph.D. Thesis, Seoul National University, Seoul, Korea, 2012. [Google Scholar]
- Cho, M.J. A study on the job-satisfaction and its depressive factors in human relation among operation room nurses. Korean Nurse 1993, 32, 48–60. [Google Scholar]
- Hwang, S.Y. Effects of Problem-Based Learning on the Knowledge Achievement, Critical Thinking Ability, Attitude and Motivation toward Learning of Nursing Students. Ph.D. Thesis, Chonnam National University, Gwangju, Korea, 2003. [Google Scholar]
- Park, E.H.; Hwang, S.Y. Effects of a web-based learning contents in operating room nursing for nursing students. J. Korea Contents Assoc. 2011, 11, 384–394. [Google Scholar] [CrossRef]
- Yoo, M.S. The effectiveness of standardized patient managed instruction for a fundamental nursing course. J. Korean Acad. Soc. Nurs. Educ. 2001, 7, 94–112. [Google Scholar]
- Keller, J.M. Motivational design of instruction. In Instructional Design Theories and Models; Reigeluth, C.M., Ed.; Routledge: London, UK, 1983. [Google Scholar]
- Jang, H.J. The Development and Effectiveness of Courseware for Injection. Unpublished Ph.D. Dissertation, Ewha University, Seoul, Korea, 1996. [Google Scholar]
- Hauze, S.; Marshall, J. Validation of the instructional materials motivation survey: Measuring student motivation to learn via mixed reality nursing education simulation. IJEL 2020, 19, 49–64. [Google Scholar]
- Leem, E.; Woo, T. Exploratory research on virtual reality contents design methods based on Head Mounted Device. J. Korean Soc. Media Arts 2016, 14, 91–106. [Google Scholar] [CrossRef]
- Brockmyer, J.H.; Fox, C.M.; Curtiss, K.A.; McBroom, E.; Burkhart, K.M.; Pidruzny, J.N. The development of the game engagement questionnaire: A measure of engagement in video game-playing. J. Exp. Soc. Psychol. 2009, 45, 624–634. [Google Scholar] [CrossRef]
- Peden, R.G.; Mercer, R.; Tatham, A.J. The use of head-mounted display eyeglasses for teaching surgical skills: A prospective randomised study. Int. J. Surg. 2016, 34, 169–173. [Google Scholar] [CrossRef]
- Han, K.S.; Cho, J.H. The effect of presence and engagement in HMD virtual reality advertising on attitude and memory. J. Korea Converg. Soc. 2019, 10, 139–146. [Google Scholar] [CrossRef]
- Tsai, S.-L.; Chai, S.-K.; Hsieh, L.-F.; Lin, S.; Taur, F.-M.; Sung, W.-H.; Doong, J.-L. The use of virtual reality computer simulation in learning Port-A Cath Injection. Adv. Health Sci. Educ. Theory Pract. 2006, 13, 71–87. [Google Scholar] [CrossRef]
- Samosorn, A.B.; Gilbert, G.E.; Bauman, E.B.; Khine, J.; McGonigle, D. Teaching airway insertion skills to nursing faculty and students using virtual reality: A pilot study. Clin. Simul. Nurs. 2020, 39, 18–26. [Google Scholar] [CrossRef]
- Kang, K.-A.; Kim, S.-J.; Lee, M.-N.; Kim, M.; Kim, S. Comparison of learning effects of virtual reality simulation on nursing students caring for children with asthma. Int. J. Environ. Res. Public Health 2020, 17, 8417. [Google Scholar] [CrossRef]
- Chen, F.Q.; Leng, Y.F.; Ge, J.F.; Wang, D.W.; Li, C.; Chen, B.; Sun, Z.L. Effectiveness of virtual reality in nursing education: Meta-analysis. J. Med. Internet Res. 2020, 22, e18290. [Google Scholar] [CrossRef] [PubMed]
- Woon, A.P.N.; Mok, W.Q.; Chieng, Y.J.S.; Zhang, H.M.; Ramos, P.; Mustadi, H.B.; Lau, Y. Effectiveness of virtual reality training in improving knowledge among nursing students: A systematic review, meta-analysis and meta-regression. Nurse Educ. Today 2021, 98, 104655. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Yang, M.; Ku, B.; Mann, J.S. Effects of virtual reality simulation program regarding high-risk neonatal infection control on nursing students. Asian Nurs. Res. 2021, 15, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-R.; Choi, E.-J. Development of a scenario and evaluation for SimBaby simulation learning of care for children with fever in emergency units. J. Korea Contents Assoc. 2011, 11, 279–288. [Google Scholar] [CrossRef] [Green Version]
- Hjelle, B.A.F.; Eriksen, J.H. Virtual Reality Based Learning Tool to Increase Nursing Student’s Motivation in Medication Management Education. Master’s Thesis, University of Agder, Kristiansund, Norway, 2021. [Google Scholar]
- Mao, R.Q.; Lan, L.; Kay, J.; Lohre, R.; Ayeni, O.R.; Goel, D.P.; Sa, D. Immersive virtual reality for surgical training: A systematic review. J. Surg. Res. 2021, 268, 40–58. [Google Scholar] [CrossRef]
- Natalia Campos, S.; Magdalena Ramos, N.-P.; Antonio José Moreno, G. Virtual reality and motivation in the educational context: Bibliometric study of the last twenty years from Scopus. Alteridad Cuenca Ecuad. 2020, 15, 47. [Google Scholar] [CrossRef] [Green Version]
- Park, J.T.; Kim, J.H.; Lee, J.H. Development of educational content for dental extraction skill training using virtual reality technology. J. Korea Contents Assoc. 2018, 18, 218–228. [Google Scholar] [CrossRef]
- Dalgarno, B.; Lee, M.J.W. What are the learning affordances of 3-D virtual environments? Br. J. Educ. Technol. 2010, 41, 10–32. [Google Scholar] [CrossRef]
- Shorey, S.; Ng, E.D. The use of virtual reality simulation among nursing students and registered nurses: A systematic review. Nurse Educ. Today 2021, 98, 104662. [Google Scholar] [CrossRef]
- Bak, S.-H.; Yun, G.-Y.; Choi, T.-J.; You, H.-B.; Bae, J.-H. Design of immersive experience training system with virtual reality technology (VR). J. Digit. Contents Soc. 2018, 19, 2289–2295. [Google Scholar] [CrossRef]
- Decker, S.; Fey, M.; Sideras, S.; Caballero, S.; Boese, T.; Franklin, A.E.; Borum, J.C. Standards of best practice: Simulation standard VI: The debriefing process. Clin. Simul. Nurs. 2013, 9, S26–S29. [Google Scholar] [CrossRef]
- Paige, J.T.; Arora, S.; Fernandez, G.; Seymour, N. Debriefing 101: Training faculty to promote learning in simulation-based training. Am. J. Surg. 2015, 209, 126–131. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Categories | Total (N = 60) | Exp. (N = 30) | Cont. (N = 30) | χ2 or t | p |
|---|---|---|---|---|---|---|
| N (%) or Mean ± SD | ||||||
| Gender | Male | 10 (16.7) | 4 (13.3) | 6 (20.0) | 0.49 | 0.731 |
| Female | 50 (83.3) | 26 (86.7) | 24 (80.0) | |||
| Age | 25.2 ± 6.45 | 23.10 ± 2.76 | 27.3 ± 8.25 | 21.79 | 0.150 | |
| Grades | 4.0–4.5 | 11 (18.3) | 5 (16.7) | 6 (20.0) | 2.33 | 0.507 |
| 3.5–4.0 | 27 (45.0) | 14 (46.7) | 13 (43.3) | |||
| 3.0–3.5 | 20 (33.3) | 9 (30.0) | 11 (36.7) | |||
| 2.5–3.0 | 2 (3.3) | 2 (6.7) | 0 | |||
| Satisfaction of major in nursing | Very high | 32 (53.3) | 16 (53.3) | 16 (53.3) | 0.62 | 0.733 |
| High | 18 (30.0) | 8 (26.7) | 10 (33.3) | |||
| Moderate | 10 (16.7) | 6 (20.0) | 4 (13.3) | |||
| Interesting of practice | Very high | 32 (53.3) | 17 (56.7) | 15 (50.0) | 1.97 | 0.374 |
| High | 23 (38.3) | 12 (40.0) | 11 (36.7) | |||
| Moderate | 5 (8.3) | 1 (3.3) | 4 (13.3) | |||
| Knowledge | 5.25 ± 1.36 | 5.37 ± 1.13 | 5.13 ± 1.57 | 5.83 | 0.443 | |
| Learning attitude | 54.03 ± 6.15 | 55.03 ± 5.48 | 53.03 ± 6.70 | 28.64 | 0.155 | |
| Satisfaction | 67.58 ± 12.33 | 69.70 ± 11.99 | 65.47 ± 12.50 | 24.67 | 0.646 | |
| Learning motivation | 105.47 ± 18.86 | 111.37 ± 18.21 | 99.57 ± 17.89 | 43.00 | 0.386 | |
| Variables | Group | Pre Mean ± SD | Post Mean ± SD | t(a) | p(a) | t(b) | p(b) | |
|---|---|---|---|---|---|---|---|---|
| Knowledge | Exp. | 5.37 ± 1.13 | 6.97 ± 1.35 | 6.87 | 0.001 * | 4.01 | 0.001 | |
| Cont. | 5.13 ± 1.57 | 4.80 ± 1.65 | −0.79 | 0.878 | ||||
| Attitude | Exp. | 55.03 ± 5.48 | 60.00 ± 6.94 | 3.83 | 0.001 * | 3.25 | 0.002 | |
| Cont. | 53.03 ± 6.70 | 50.87 ± 8.03 | −1.22 | 0.231 | ||||
| Satisfaction | Exp. | 69.70 ± 11.99 | 75.00 ± 10.49 | 2.75 | 0.010 * | 2.46 | 0.017 | |
| Cont. | 65.47 ± 12.50 | 64.17 ± 14.31 | −0.69 | 0.493 | ||||
| Motivation | Exp. | 111.37 ± 18.21 | 118.37 ± 16.86 | 3.12 | 0.004 * | 1.59 | 0.118 | |
| Cont. | 99.57 ± 17.89 | 100.30 ± 23.51 | 0.23 | 0.823 | ||||
| Sub-domain | Attention | Exp. | 40.53 ± 6.76 | 43.90 ± 7.24 | 4.34 | 0.000 * | 2.51 | 0.016 |
| Cont. | 37.77 ± 6.14 | 37.17 ± 8.37 | −0.44 | 0.666 | ||||
| Relevance | Exp. | 30.57 ± 5.93 | 33.47 ± 5.61 | 2.95 | 0.006 * | 2.10 | 0.040 | |
| Cont. | 25.97 ± 5.98 | 25.87 ± 7.52 | −0.10 | 0.924 | ||||
| Confidence | Exp. | 22.33 ± 4.19 | 22.57 ± 2.79 | 0.39 | 0.698 | −0.75 | 0.456 | |
| Cont. | 20.93 ± 4.43 | 21.90 ± 5.35 | 1.24 | 0.223 | ||||
| Satisfaction | Exp. | 17.93 ± 3.40 | 18.63 ± 3.14 | 0.94 | 0.354 | 0.04 | 0.971 | |
| Cont. | 14.90 ± 3.59 | 15.37 ± 4.29 | 0.64 | 0.527 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, A.-R.; Park, E.-A. The Effectiveness of Learning to Use HMD-Based VR Technologies on Nursing Students: Chemoport Insertion Surgery. Int. J. Environ. Res. Public Health 2022, 19, 4823. https://doi.org/10.3390/ijerph19084823
Jung A-R, Park E-A. The Effectiveness of Learning to Use HMD-Based VR Technologies on Nursing Students: Chemoport Insertion Surgery. International Journal of Environmental Research and Public Health. 2022; 19(8):4823. https://doi.org/10.3390/ijerph19084823
Chicago/Turabian StyleJung, Ae-Ri, and Eun-A Park. 2022. "The Effectiveness of Learning to Use HMD-Based VR Technologies on Nursing Students: Chemoport Insertion Surgery" International Journal of Environmental Research and Public Health 19, no. 8: 4823. https://doi.org/10.3390/ijerph19084823
APA StyleJung, A.-R., & Park, E.-A. (2022). The Effectiveness of Learning to Use HMD-Based VR Technologies on Nursing Students: Chemoport Insertion Surgery. International Journal of Environmental Research and Public Health, 19(8), 4823. https://doi.org/10.3390/ijerph19084823






