Working Environment, Personal Protective Equipment, Personal Life Changes, and Well-Being Perceived in Spanish Nurses during COVID-19 Pandemic: A Cross-Sectional Study
Abstract
:1. Introduction
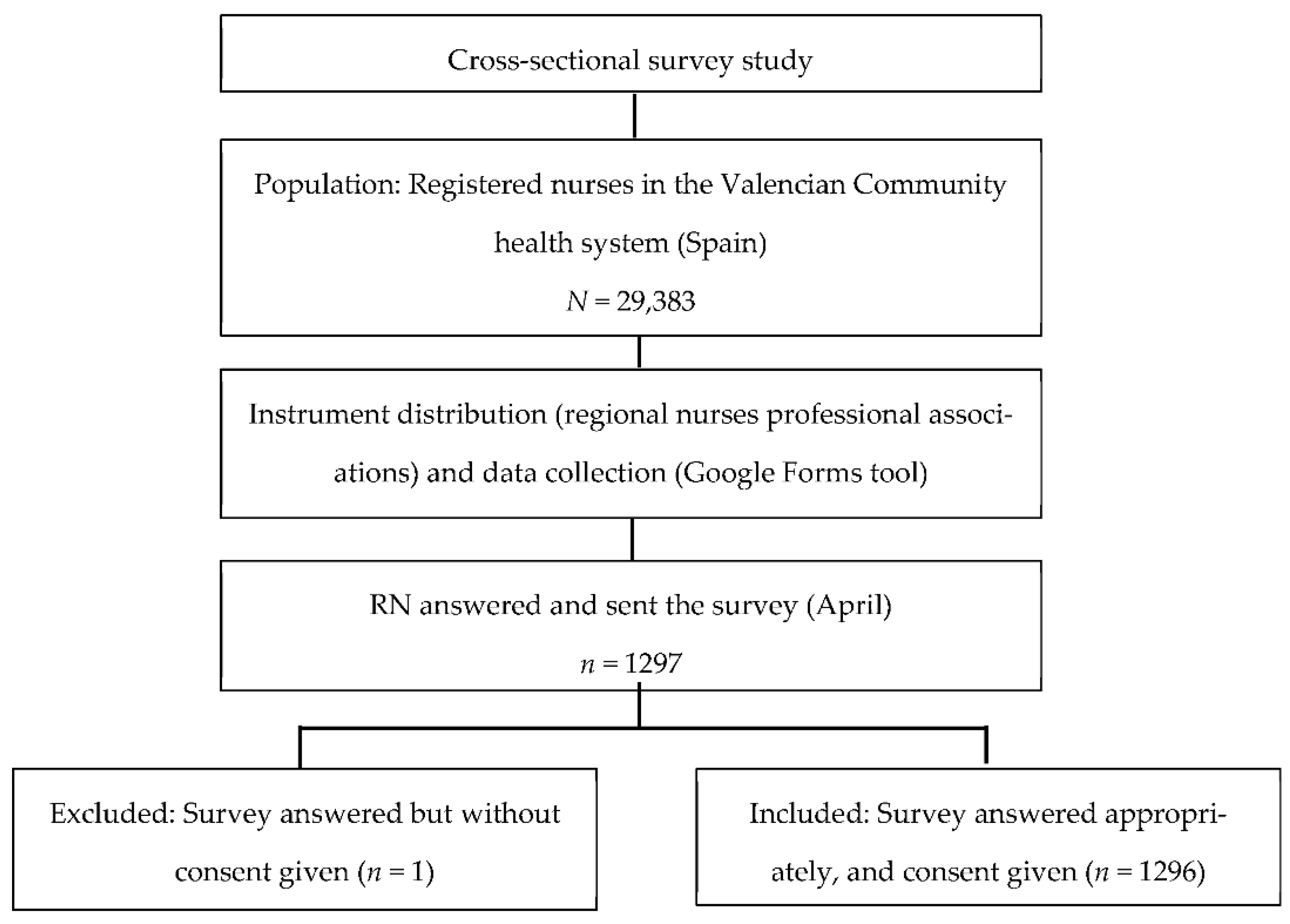
2. Materials and Methods
2.1. Design, Setting and Population
2.2. Instrument and Procedure
2.3. Data Analysis
2.4. Ethical Considerations
2.5. Quality Appraisal
3. Results
3.1. Sample
3.2. Working Environment
3.3. Personal Protective Equipment
3.4. Changes in Nurses’ Personal Lives
3.5. Perceived Well-Being
4. Discussion
4.1. Working Environment
4.2. Personal Protective Equipment
4.3. Changes in Nurses’ Personal Lives
4.4. Perceived Well-Being
4.5. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Atique, S.; Bautista, J.R.; Block, L.J.; Lee, J.J.; Lozada-Perezmitre, E.; Nibber, R.; O’Connor, S.; Peltonen, L.M.; Ronquillo, C.; Tayaben, J.; et al. A Nursing Informatics Response to COVID-19: Perspectives from Five Regions of the World. J. Adv. Nurs. 2020, 76, 2462–2468. [Google Scholar] [CrossRef] [PubMed]
- Ammad Ud Din, M.; Boppana, L.K.T. An Update on the 2019-NCoV Outbreak. Am. J. Infect. Control 2020, 48, 713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- La Moncloa. El Centro Nacional de Microbiología Confirma un Caso de Coronavirus en La Gomera [The National Center for Microbiology Confirms a Case of Coronavirus in La Gomera]. 31 January 2020. Available online: https://www.lamoncloa.gob.es/serviciosdeprensa/notasprensa/sanidad14/Paginas/2020/310120-coronavirus-gomera.aspx (accessed on 24 February 2022).
- Distribución de la Mortalidad por Virus COVID-19 Identificado y Virus no Identificado (Sospechoso), Comunidad y Ciudad Autónoma de Fallecimiento, Sexo y Semana de Fallecimiento [Distribution of Mortality due to COVID-19 Identified Virus and Unidentified (Suspected) Virus, Community and Autonomous City of Death, Sex and Week of Death]. Available online: https://ine.es/jaxi/Tabla.htm?path=/t15/p417/covid/l0/&file=01007.px&L=0 (accessed on 24 February 2022).
- COVID-19 Map—Johns Hopkins Coronavirus Resource Center. Available online: https://coronavirus.jhu.edu/map.html (accessed on 24 February 2022).
- Ministerio de Sanidad, Consumo y Bienestar Social—Profesionales—Nueva Enfermedad por Coronavirus, COVID-19 [Ministry of Health, Consumption and Social Welfare—Professional—New Coronavirus Disease, COVID-19]. Available online: https://www.mscbs.gob.es/en/profesionales/saludPublica/ccayes/alertasActual/nCov/home.htm (accessed on 24 February 2022).
- Bambi, S.; Iozzo, P.; Lucchini, A. New Issues in Nursing Management During the COVID-19 Pandemic in Italy. Am. J. Crit. Care 2020, 29, e92–e93. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Tong, Z.; Guan, X.; Du, B.; Qiu, H.; Slutsky, A.S. Critical Care Crisis and Some Recommendations during the COVID-19 Epidemic in China. Intensive Care Med. 2020, 46, 837–840. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Binkley, C.E.; Kemp, D.S. Ethical Rationing of Personal Protective Equipment to Minimize Moral Residue During the COVID-19 Pandemic. J. Am. Coll. Surg. 2020, 230, 1111. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, J.; Jackson, D.; Usher, K. The Potential for COVID-19 to Contribute to Compassion Fatigue in Critical Care Nurses. J. Clin. Nurs. 2020, 29, 2762–2764. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.Z.; Han, M.F.; Luo, T.D.; Ren, A.K.; Zhou, X.P. Mental Health Survey of Medical Staff in a Tertiary Infectious Disease Hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2020, 38, 192–195. [Google Scholar] [CrossRef] [PubMed]
- Williamson, V.; Murphy, D.; Greenberg, N. COVID-19 and Experiences of Moral Injury in Front-Line Key Workers. Occup. Med. 2020, 70, 317–319. [Google Scholar] [CrossRef] [Green Version]
- Mira, J.J.; Carrillo, I.; Guilabert, M.; Mula, A.; Martin-Delgado, J.; Pérez-Jover, M.V.; Vicente, M.A.; Fernández, C. Acute Stress of the Healthcare Workforce during the COVID-19 Pandemic Evolution: A Cross-Sectional Study in Spain. BMJ Open 2020, 10, e042555. [Google Scholar] [CrossRef]
- Zhao, F.; Ahmed, F.; Faraz, N.A. Caring for the Caregiver during COVID-19 Outbreak: Does Inclusive Leadership Improve Psychological Safety and Curb Psychological Distress? A Cross-Sectional Study. Int. J. Nurs. Stud. 2020, 110, 103725. [Google Scholar] [CrossRef]
- Da Silva, F.C.T.; Neto, M.L.R. Psychiatric Symptomatology Associated with Depression, Anxiety, Distress, and Insomnia in Health Professionals Working in Patients Affected by COVID-19: A Systematic Review with Meta-Analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 104, 110057. [Google Scholar] [CrossRef] [PubMed]
- Firew, T.; Sano, E.D.; Lee, J.W.; Flores, S.; Lang, K.; Salman, K.; Greene, M.C.; Chang, B.P. Protecting the Front Line: A Cross-Sectional Survey Analysis of the Occupational Factors Contributing to Healthcare Workers’ Infection and Psychological Distress during the COVID-19 Pandemic in the USA. BMJ Open 2020, 10, e042752. [Google Scholar] [CrossRef]
- Shaukat, N.; Ali, D.M.; Razzak, J. Physical and Mental Health Impacts of COVID-19 on Healthcare Workers: A Scoping Review. Int. J. Emerg. Med. 2020, 13, 40. [Google Scholar] [CrossRef] [PubMed]
- INEbase/Society/Health/Statistics of Collegiate Health Professionals/Latest Data. Available online: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176781&menu=ultiDatos&idp=1254735573175 (accessed on 24 February 2022).
- Choi, K.R.; Skrine Jeffers, K.; Cynthia Logsdon, M. Nursing and the Novel Coronavirus: Risks and Responsibilities in a Global Outbreak. J. Adv. Nurs. 2020, 76, 1486–1487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tran, K.; Cimon, K.; Severn, M.; Pessoa-Silva, C.L.; Conly, J. Aerosol Generating Procedures and Risk of Transmission of Acute Respiratory Infections to Healthcare Workers: A Systematic Review. PLoS ONE 2012, 7, 35797. [Google Scholar] [CrossRef] [Green Version]
- Widiasih, R.; Ermiati; Emaliyawati, E.; Hendrawati, S.; Susanti, R.D.; Sutini, T.; Sari, C.W.M. Nurses’ Actions to Protect Their Families from COVID-19: A Descriptive Qualitative Study. Glob. Qual. Nurs. Res. 2021, 8. [Google Scholar] [CrossRef] [PubMed]
- Melnyk, B.M.; Hsieh, A.P.; Tan, A.; Teall, A.M.; Weberg, D.; Jun, J.; Gawlik, K.; Hoying, J. Associations Among Nurses’ Mental/Physical Health, Lifestyle Behaviors, Shift Length, and Workplace Wellness Support During COVID-19: Important Implications for Health Care Systems. Nurs. Adm. Q. 2022, 46, 5. [Google Scholar] [CrossRef]
- Boynton, P.M.; Greenhalgh, T. Selecting, Designing, and Developing Your Questionnaire. BMJ Br. Med. J. 2004, 328, 1312. [Google Scholar] [CrossRef] [Green Version]
- Ministerio de Sanidad, Consumo y Bienestar Social—Profesionales—Documentos Técnicos para Profesionales [Ministry of Health, Consumption and Social Welfare—Professionals—Technical Documents for Professionals—Coronavirus]. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos.htm (accessed on 24 February 2022).
- Cordero, A.; Santos García-Gallego, C.; Bertomeu-González, V.; Fácila, L.; Rodríguez-Mañero, M.; Escribano, D.; Castellano, J.M.; Zuazola, P.; Núñez, J.; Badimón, J.J.; et al. Mortality Associated with Cardiovascular Disease in Patients with COVID-19. REC CardioClinics 2021, 56, 30–38. [Google Scholar] [CrossRef]
- Kremer, H.J.; Thurner, W. Age Dependence in COVID-19 Mortality in Germany. Dtsch. Arztebl. Int. 2020, 117, 432–433. [Google Scholar] [CrossRef]
- Ejaz, H.; Alsrhani, A.; Zafar, A.; Javed, H.; Junaid, K.; Abdalla, A.E.; Abosalif, K.O.A.; Ahmed, Z.; Younas, S. COVID-19 and Comorbidities: Deleterious Impact on Infected Patients. J. Infect. Public Health 2020, 13, 1833. [Google Scholar] [CrossRef] [PubMed]
- Abtahi, M.; Gholamnia, R.; Bagheri, A.; Jabbari, M.; Koolivand, A.; Dobaradaran, S.; Jorfi, S.; Vaziri, M.H.; Khoshkerdar, M.; Rastegari, P.; et al. An Innovative Index for Assessing Vulnerability of Employees of Different Occupations from the COVID-19 Pandemic in Iran. Environ. Res. 2021, 197, 111039. [Google Scholar] [CrossRef] [PubMed]
- Cruz Lendínez, A.J.; Grande Gascón, M.L.; García Fernández, F.P.; Hueso Montoro, C.; Ruiz López, M.; García Ramiro, P.A.; Tamajón Flores, F.; Calero García, M.J.; Morales Asenjo, J.M.; García Alumbreros, M.J. Analysis of the Situation of Nurses, Midwives, and Physiotherapists in Spanish Health Centres, 1st ed.; Cruz Lendínez, A.J., García Alumbreros, M.J., Eds.; Sindicato de Enfermería—Satse: Madrid, Spain, 2019. [Google Scholar]
- Cebrián-Cuenca, A.; Mira, J.J.; Caride-Miana, E.; Fernández-Jiménez, A.; Orozco-Beltrán, D. Sources of Psychological Distress among Primary Care Physicians during the COVID-19 Pandemic’s First Wave in Spain: A Cross-Sectional Study. Prim. Health Care Res. Dev. 2021, 22, e55. [Google Scholar] [CrossRef]
- Martin-Delgado, J.; Viteri, E.; Mula, A.; Serpa, P.; Pacheco, G.; Prada, D.; de Andrade Lourenção, D.C.; Baptista, P.C.P.; Ramirez, G.; Mira, J.J. Availability of Personal Protective Equipment and Diagnostic and Treatment Facilities for Healthcare Workers Involved in COVID-19 Care: A Cross-Sectional Study in Brazil, Colombia, and Ecuador. PLoS ONE 2020, 15, e0242185. [Google Scholar] [CrossRef] [PubMed]
- Tabah, A.; Ramanan, M.; Laupland, K.B.; Buetti, N.; Cortegiani, A.; Mellinghoff, J.; Morris, A.C.; Camporota, L.; Zappella, N.; Elhadi, M.; et al. Personal Protective Equipment and Intensive Care Unit Healthcare Worker Safety in the COVID-19 Era (PPE-SAFE): An International Survey. J. Crit. Care 2020, 59, 70. [Google Scholar] [CrossRef] [PubMed]
- Aranaz Andrés, J.M.; Gea Velázquez de Castro, M.T.; Vicente-Guijarro, J.; Beltrán Peribáñez, J.; García Haro, M.; Valencia-Martín, J.L.; Bischofberger Valdés, C.; María Aranaz Andrés, J.; Bolúmar Montrull, F.; Lorenzo Valencia Martín, J.; et al. Masks as Personal Protective Equipment in the COVID-19 Pandemic: How, When and Which Should Be Used. J. Healthc. Qual. Res. 2020, 35, 245. [Google Scholar] [CrossRef] [PubMed]
- UNE-EN. 14683:2019+AC:2019. Medical Face Masks—Requirements and Test Methods. Available online: https://tienda.aenor.com/norma-une-en-14683-2019-ac-2019-n0062987 (accessed on 24 February 2022).
- UNE-EN. 149:2001+A1:2010. Respiratory Protective Devices—Filtering Half Masks to Protect against Particles—Requirements, Testing, Marking. Available online: https://www.une.org/encuentra-tu-norma/busca-tu-norma/norma?c=N0044643 (accessed on 24 February 2022).
- World Health Organization. Rational Use of Personal Protective Equipment for Coronavirus Disease (COVID-19 and Considerations during Severe Shortages Interim Guidance). April 2020. Available online: https://apps.who.int/iris/handle/10665/331695 (accessed on 24 February 2022).
- Kampf, G.; Scheithauer, S.; Lemmen, S.; Saliou, P.; Suchomel, M. COVID-19-Associated Shortage of Alcohol-Based Hand Rubs, Face Masks, Medical Gloves, and Gowns: Proposal for a Risk-Adapted Approach to Ensure Patient and Healthcare Worker Safety. J. Hosp. Infect. 2020, 105, 424–427. [Google Scholar] [CrossRef]
- Avis SF2H du 14 Mars 2020, Prolongation du Port ou Réutilisation des Masques [SF2H Notice of March 14, 2020, Extension of Wearing or Reuse of Masks]. Available online: https://www.sf2h.net/avis-du-14-mars-2020-prolongation-utilisation-des-masques (accessed on 24 February 2022).
- Ranney, M.L.; Griffeth, V.; Jha, A.K. Critical Supply Shortages—The Need for Ventilators and Personal Protective Equipment during the COVID-19 Pandemic. N. Engl. J. Med. 2020, 382, e41. [Google Scholar] [CrossRef]
- Burdorf, A.; Porru, F.; Rugulies, R. The COVID-19 (Coronavirus) Pandemic: Consequences for Occupational Health. Scand. J. Work. Environ. Health 2020, 46, 229–230. [Google Scholar] [CrossRef]
- Chandler-Jeanville, S.; Nohra, R.G.; Loizeau, V.; Lartigue-Malgouyres, C.; Zintchem, R.; Naudin, D.; Rothan-Tondeur, M. Perceptions and Experiences of the COVID-19 Pandemic amongst Frontline Nurses and Their Relatives in France in Six Paradoxes: A Qualitative Study. Int. J. Environ. Res. Public Health 2021, 18, 6977. [Google Scholar] [CrossRef]
- Huang, L.; Lei, W.; Liu, H.; Hang, R.; Tao, X.; Zhan, Y. Nurses’ Sleep Quality of “Fangcang” Hospital in China during the COVID-19 Pandemic. Int. J. Ment. Health Addict. 2020, 20, 789–799. [Google Scholar] [CrossRef] [PubMed]
- Bellanti, F.; Lo Buglio, A.; Capuano, E.; Dobrakowski, M.; Kasperczyk, A.; Kasperczyk, S.; Ventriglio, A.; Vendemiale, G. Factors Related to Nurses’ Burnout during the First Wave of Coronavirus Disease-19 in a University Hospital in Italy. Int. J. Environ. Res. Public Health 2021, 18, 5051. [Google Scholar] [CrossRef] [PubMed]

| n | % | |
|---|---|---|
| Gender | ||
| Female | 1131 | 87.3 |
| Male | 165 | 12.7 |
| Age | ||
| 22–29 | 205 | 15.8 |
| 30–39 | 423 | 32.6 |
| 40–49 | 408 | 31.5 |
| 50–59 | 207 | 16 |
| ≤60 | 53 | 4.1 |
| Years as nurses | ||
| 0–5 | 252 | 19.4 |
| 6–10 | 168 | 13.0 |
| 11–15 | 378 | 29.2 |
| 16–20 | 240 | 18.5 |
| More than 20 | 258 | 19.9 |
| Type of institution | ||
| Public institutions | 1128 | 87 |
| Private institutions | 168 | 13 |
| Nursing professional group | ||
| General nursing (without specialty) | 1144 | 88.4 |
| Pediatric Nurse Specialist | 65 | 5.1 |
| Midwifery | 42 | 3.2 |
| Family and Community Nurse Specialist | 16 | 1.2 |
| Mental Health Nurse Specialist | 11 | 0.8 |
| Occupational Health Specialist Nurse | 11 | 0.8 |
| Geriatrics Nurse Specialist | 7 | 0.5 |
| Working area | ||
| Hospital ward | 428 | 33 |
| Primary care | 209 | 16.1 |
| Intermediate or Intensive Care Unit | 181 | 14 |
| Other hospital units | 125 | 9.6 |
| Emergencies | 123 | 9.5 |
| Operating rooms | 80 | 6.2 |
| Outpatients’ departments | 53 | 4.1 |
| Other workplaces | 31 | 2.4 |
| Delivery rooms | 22 | 1.7 |
| Socio-health community centers | 28 | 2.2 |
| Home hospitalization unit | 16 | 1.2 |
| What Has Happened to Your Job? | n | % | ||
|---|---|---|---|---|
| I am still in the same job | 953 | 73.5 | ||
| I have been relocated | 217 | 16.7 | ||
| I have been hired to reinforce | 126 | 9.7 | ||
| What has happened to the nurse–patient ratio in your service? | ||||
| The nursing staff has been increased | 524 | 40.4 | ||
| It keeps the same nursing staff | 524 | 40.4 | ||
| The nursing staff has been decreased | 210 | 16.2 | ||
| If you are vulnerable personnel, have you changed your position or role? Have you been redeployed? | n | % | Valid percentage 1 | |
| Pregnancy | Yes 2 | 5 | 0.4 | 33.33 |
| Not yet | 4 | 0.3 | 26.66 | |
| Sick leave approved | 6 | 0.5 | 40 | |
| I do not meet the criteria | 1281 | 98.8 | - | |
| Immunosuppression disorder | Yes | 12 | 0.9 | 42.86 |
| Not yet | 8 | 0.6 | 28.57 | |
| Sick leave approved | 8 | 0.6 | 28.57 | |
| I do not meet the criteria | 1268 | 97.8 | - | |
| Cardiovascular disease | Yes | 19 | 1.4 | 31.15 |
| Not yet | 35 | 2.7 | 57.38 | |
| Sick leave approved | 7 | 0.5 | 11.47 | |
| I do not meet the criteria | 1235 | 95.3 | - | |
| Diabetes | Yes | 11 | 0.8 | 55 |
| Not yet | 7 | 0.5 | 35 | |
| Sick leave approved | 2 | 0.2 | 10 | |
| I do not meet the criteria | 1276 | 98.5 | - | |
| Chronic lung disease | Yes | 9 | 0.7 | 23 |
| Not yet | 21 | 1.6 | 54 | |
| Sick leave approved | 9 | 0.7 | 23 | |
| I do not meet the criteria | 1257 | 97 | - | |
| Cancer in active treatment | Yes | 5 | 0.4 | 41.67 |
| Not yet | 5 | 0.4 | 41.67 | |
| Sick leave approved | 2 | 0.2 | 16.66 | |
| I do not meet the criteria | 1284 | 99.1 | - | |
| Over 60 years | Yes | 17 | 1.3 | 32.7 |
| Not yet | 30 | 2.3 | 57.7 | |
| Sick leave approved | 5 | 0.4 | 9.6 | |
| I do not meet the criteria | 1244 | 96 | - | |
| Frequency of Replacement | Reuse | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Once Per Shift n (%) | Once per Week n (%) | After Contact with COVID-19 +/Possible COVID-19 Patient n (%) | Only when It Deteriorates n (%) | Never n (%) | Other n (%) | Yes n (%) | No n (%) | I Have Never Had n (%) | |
| Surgical mask | 802 | 108 | 274 | 57 | 3 | 52 | 806 | 466 | 24 |
| (61.9) | (8.3) | (21.1) | (4.4) | (0.2) | (4) | (62.2) | (36) | (1.8) | |
| FPP2 mask | 303 | 191 | 366 | 178 | 163 | 95 | 908 | 208 | 180 |
| (23.4) | (14.7) | (28.2) | (13.7) | (12.6) | (7.3) | (70.1) | (16) | (13.9) | |
| FPP3 mask | 65 | 63 | 214 | 60 | 767 | 127 | 287 | 173 | 836 |
| (5) | (4.9) | (16.5) | (4.6) | (59.2) | (9.8) | (22.1) | (13.3) | (64.6) | |
| Safety glasses | 185 | 35 | 663 | 91 | 200 | 122 | 873 | 177 | 246 |
| (14.3) | (2.7) | (51.2) | (7) | (15.4) | (9.4) | (67.4) | (13.6) | (19) | |
| Face shield | 242 | 42 | 580 | 139 | 150 | 143 | 938 | 206 | 152 |
| (18.7) | (3.2) | (44.8) | (10.7) | (11.6) | (11) | (72.4) | (15.9) | (11.7) | |
| Waterproof gown | 232 | 36 | 607 | 66 | 216 | 139 | 566 | 468 | 262 |
| (17.9) | (2.8) | (46.8) | (5.1) | (16.7) | (10.7) | (43.7) | (36.1) | (20.2) | |
| Surgical gown | 375 | 54 | 479 | 58 | 134 | 196 | 490 | 643 | 163 |
| (28.9) | (4.2) | (37) | (4.5) | (10.3) | (15.1) | (37.8) | (49.6) | (12.6) | |
| Full-body isolation suit | 113 | 38 | 398 | 38 | 549 | 160 | 233 | 379 | 684 |
| (8.7) | (2.9) | (30.7) | (2.9) | (42.4) | (12.3) | (18) | (29.2) | (52.8) | |
| Have You Left Your Home to Avoid Infecting Your Family? (n = 1296) | n | % |
|---|---|---|
| Yes | 145 | 11.2 |
| No | 1151 | 88.8 |
| After leaving your usual home, where have you stayed? (n = 145) | ||
| Second residence or empty family home | 127 | 87.6 |
| I have paid for a hotel/flat/apartment | 14 | 9.6 |
| In hotel/flat/apartment made available altruistically by a company | 4 | 2.8 |
| If you have children, who has overseen them while you were working? (n = 802) | ||
| Father/mother/my partner | 494 | 61.6 |
| They stay alone (by age) | 153 | 19.1 |
| Grandparents | 93 | 11.6 |
| Other family and friends | 31 | 3.9 |
| Paid staff | 21 | 2.6 |
| In turn, both parents are healthcare professionals | 10 | 1.2 |
| If you are the primary caregiver of a dependent person, have you stopped doing this to avoid contagion? (n = 228) | ||
| Yes | 114 | 50 |
| No | 114 | 50 |
| Have they facilitated shift changes for family conciliation in your job? (n = 689) | ||
| Yes | 219 | 31.8 |
| No | 445 | 64.6 |
| I had to request an extension of reduced working hours | 25 | 3.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiménez-García, S.; de Juan Pérez, A.; Pérez-Cañaveras, R.M.; Vizcaya-Moreno, F. Working Environment, Personal Protective Equipment, Personal Life Changes, and Well-Being Perceived in Spanish Nurses during COVID-19 Pandemic: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 4856. https://doi.org/10.3390/ijerph19084856
Jiménez-García S, de Juan Pérez A, Pérez-Cañaveras RM, Vizcaya-Moreno F. Working Environment, Personal Protective Equipment, Personal Life Changes, and Well-Being Perceived in Spanish Nurses during COVID-19 Pandemic: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(8):4856. https://doi.org/10.3390/ijerph19084856
Chicago/Turabian StyleJiménez-García, Segundo, Alba de Juan Pérez, Rosa M. Pérez-Cañaveras, and Flores Vizcaya-Moreno. 2022. "Working Environment, Personal Protective Equipment, Personal Life Changes, and Well-Being Perceived in Spanish Nurses during COVID-19 Pandemic: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 8: 4856. https://doi.org/10.3390/ijerph19084856








