Females with Eating Disorders and Urinary Incontinence: A Psychoanalytic Perspective
Abstract
:1. Introduction
2. Psychopathological Processes Underlying EDs
3. Psychoanalytic Perspectives
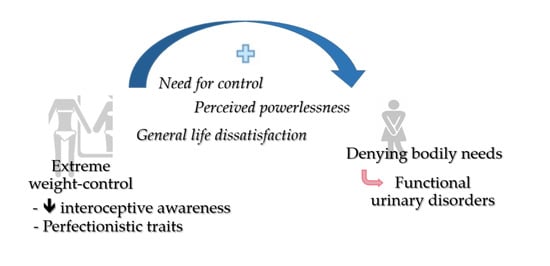
4. Confluence of Personality Traits
5. Association with Functional Urinary Symptoms
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Karwautz, A.F.; Wagner, G.; Waldherr, K.; Nader, I.W.; Fernandez-Aranda, F.; Estivill, X.; Holliday, J.; Collier, D.A.; Treasure, J.L. Gene–environment interaction in anorexia nervosa: Relevance of non-shared environment and the serotonin transporter gene. Mol. Psychiatry 2011, 13, 590–592. [Google Scholar] [CrossRef] [PubMed]
- Nordbø, R.H.; Espeset, E.M.; Gulliksen, K.S.; Skårderud, F.; Geller, J.; Holte, A. Reluctance to recover in anorexia nervosa. Eur. Eat. Disord. Rev. 2012, 13, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Whitney, K.E.; Holtzman, B.; Cook, D.; Bauer, S.; Maffazioli, G.D.; Parziale, A.L.; Ackerman, K.E. Low energy availability and impact sport participation as risk factors for urinary incontinence in female athletes. J. Pediatric Urol. 2021, 17, e1–e290. [Google Scholar] [CrossRef] [PubMed]
- Carvalhais, A.; Araújo, J.; Jorge, R.N.; Bø, K. Urinary incontinence and disordered eating in female elite athletes. J. Sci. Med. Sport 2019, 22, 140–144. [Google Scholar] [CrossRef]
- Araujo, M.P.; Ed, O.; Zucchi, E.V.; Girão, M.J.; Sartori, M.G. The relationship between urinary incontinence and eating disorders in female long-distance runners. Rev. Assoc. Med. Bras. 2008, 54, 146–149. [Google Scholar]
- Linardon, J.; Phillipou, A.; Castle, D.; Newton, R.; Harrison, P.; Cistullo, L.L.; Griffiths, S.; Hindle, A.; Brennan, L. The relative associations of shape and weight over-evaluation, preoccupation, dissatisfaction, and fear of weight gain with measures of psychopathology: An extension study in individuals with anorexia nervosa. Eat. Behav. 2018, 29, 54–58. [Google Scholar] [CrossRef]
- Carter, J.C.; Stewart, D.A.; Fairburn, C.G. Eating disorder examination questionnaire: Norms for young adolescent girls. Behav. Res. Ther. 2001, 39, 625–632. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Shafran, R.; Cooper, Z. A cognitive behavioural theory of anorexia nervosa. Behav. Res. Ther. 1999, 37, 1–13. [Google Scholar] [CrossRef]
- Wetzler, S.; Hackmann, C.; Peryer, G.; Clayman, K.; Friedman, D.; Saffran, K.; Silver, J.; Swarbrick, M.; Magill, E.; van Furth, E.F.; et al. A framework to conceptualize personal recovery from eating disorders: A systematic review and qualitative meta-synthesis of perspectives from individuals with lived experience. Int. J. Eat. Disord. 2020, 53, 1188–1203. [Google Scholar] [CrossRef]
- Espíndola, C.R.; Blay, S.L. Anorexia nervosa treatment from the patient perspective: A metasynthesis of qualitative studies. Ann. Clin. Psychiatry 2009, 13, 38–48. [Google Scholar]
- Patching, J.; Lawler, J. Understanding women’s experiences of developing an eating disorder and recovering: A life-history approach. Nurs. Inq. 2009, 16, 10–21. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, J. Goodbye Ed, Hello Me: Recover from Your Eating Disorder and Fall in Love with Life; McGraw Hill Professional: New York, NY, USA, 2009; p. 167. [Google Scholar]
- MacNeil, L.; Esposito-Smythers, C.; Mehlenbeck, R.; Weismoore, J. The effects of avoidance coping and coping self-efficacy on eating disorder attitudes and behaviors: A stress-diathesis model. Eat. Behav. 2012, 13, 293–296. [Google Scholar] [CrossRef] [PubMed]
- Dingemans, A.E.; Spinhoven, P.; Van Furth, E.F. Maladaptive core beliefs and eating disorder symptoms. Eat. Behav. 2006, 7, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Froreich, F.V.; Vartanian, L.R.; Zawadzki, M.J.; Grisham, J.R.; Touyz, S.W. Psychological need satisfaction, control, and disordered eating. Br. J. Clin. Psychol. 2017, 56, 53–68. [Google Scholar] [CrossRef] [Green Version]
- Ward, A.; Ramsay, R.; Turnbull, S.; Benedettini, M.; Treasure, J. Attachment patterns in eating disorders: Past in the present. Int. J. Eat. Disord. 2000, 28, 370–376. [Google Scholar] [CrossRef]
- Unoka, Z.; Tölgyes, T.; Czobor, P. Early maladaptive schemas and body mass index in subgroups of eating disorders: A differential association. Compr. Psychiatry 2007, 48, 199–204. [Google Scholar] [CrossRef]
- Maher, A.; Cason, L.; Huckstepp, T.; Stallman, H.; Kannis-Dymand, L.; Millear, P.; Mason, J.; Wood, A.; Allen, A. Early maladaptive schemas in eating disorders: A systematic review. Eur. Eat. Disord. Rev. 2022, 30, 3–22. [Google Scholar] [CrossRef]
- Cruzat-Mandich, C.; Díaz-Castrillón, F.; Escobar-Koch, T.; Simpson, S. From eating identity to authentic selfhood: Identity transformation in eating disorder sufferers following psychotherapy. Clin. Psychol. 2017, 21, 227–235. [Google Scholar] [CrossRef]
- Caparrotta, L.; Ghaffari, K. A historical overview of the psychodynamic contributions to the understanding of eating disorders. Psychoanal. Psychother. 2006, 20, 175–196. [Google Scholar] [CrossRef]
- Ebert, A.; Scheuering, S.; Schott, G.; Roesch, W.H. Psychosocial and psychosexual development in childhood and adolescence within the exstrophy-epispadias complex. J. Urol. 2005, 174, 1094–1098. [Google Scholar] [CrossRef]
- Madowitz, J.; Matheson, B.E.; Liang, J. The relationship between eating disorders and sexual trauma. Eat. Weight. Disord.-Stud. Anorex. Bulim. Obes. 2015, 20, 281–293. [Google Scholar] [CrossRef] [PubMed]
- Castellini, G.; Lelli, L.; Ricca, V.; Maggi, M. Sexuality in eating disorders patients: Etiological factors, sexual dysfunction and identity issues. A systematic review. Horm. Mol. Biol. Clin. Investig. 2016, 25, 71–90. [Google Scholar] [CrossRef] [PubMed]
- Fornari, V.; Dancyger, I.F. Psychosexual development and eating disorders. Adolesc. Med. Clin. 2003, 14, 61. [Google Scholar]
- Meyer, B.C.; Weinroth, L.A. Observations on psychological aspects of anorexia nervosa: Report of a case. Psychosom. Med. 1957, 19, 389–398. [Google Scholar] [CrossRef]
- Chassler, L. “In hunger I am king”—Understanding anorexia nervosa from a psychoanalytic perspective: Theoretical and clinical implications. Clin. Soc. Work. J. 1994, 22, 397–415. [Google Scholar] [CrossRef]
- Fassino, S.; Pierò, A.; Gramaglia, C.; Daga, G.A.; Gandione, M.; Rovera, G.G.; Bartocci, G. Clinical, psychological, and personality correlates of asceticism in anorexia nervosa: From saint anorexia to pathologic perfectionism. Transcult. Psychiatry 2006, 43, 600–614. [Google Scholar] [CrossRef] [Green Version]
- Obeid, N.; Valois, D.D.; Bedford, S.; Norris, M.L.; Hammond, N.G.; Spettigue, W. Asceticism, perfectionism and overcontrol in youth with eating disorders. Eat. Weight. Disord.-Stud. Anorex. Bulim. Obes. 2021, 26, 219–225. [Google Scholar] [CrossRef]
- Shafran, R.; Cooper, Z.; Fairburn, C.G. Clinical perfectionism: A cognitive-behavioural analysis. Behav. Res. Ther. 2002, 40, 773–791. [Google Scholar] [CrossRef]
- Ackard, D.M.; Peterson, C.B. Association between puberty and disordered eating, body image, and other psychological variables. Int. J. Eat. Disord. 2001, 29, 187–194. [Google Scholar] [CrossRef]
- Vitousek, K.; Manke, F. Personality variables and disorders in anorexia nervosa and bulimia nervosa. J. Abnorm. Psychol. 1994, 103, 137. [Google Scholar] [CrossRef]
- Merwin, R.M.; Zucker, N.L.; Lacy, J.L.; Elliott, C.A. Interoceptive awareness in eating disorders: Distinguishing lack of clarity from non-acceptance of internal experience. Cogn. Emot. 2010, 24, 892–902. [Google Scholar] [CrossRef]
- Leue, C.; Kruimel, J.; Vrijens, D.; Masclee, A.; Van Os, J.; Van Koeveringe, G. Functional urological disorders: A sensitized defence response in the bladder-gut-brain axis. Nat. Rev. Urol. 2017, 14, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Kanbur, N.; Pinhas, L.; Lorenzo, A.; Farhat, W.; Licht, C.; Katzman, D.K. Nocturnal enuresis in adolescents with anorexia nervosa: Prevalence, potential causes, and pathophysiology. Int. J. Eat. Disord. 2011, 44, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Aoki, Y.; Brown, H.W.; Brubaker, L.; Cornu, J.N.; Daly, J.O.; Cartwright, R. Urinary incontinence in women. Nat. Rev. Dis. Primers 2017, 3, 17042. [Google Scholar] [CrossRef] [Green Version]
- Goldstick, O.; Constantini, N. Urinary incontinence in physically active women and female athletes. Br. J. Sports Med. 2014, 48, 296–298. [Google Scholar] [CrossRef]
- Bodner-Adler, B.; Bodner, K.; Kimberger, O.; Halpern, K.; Rieken, M.; Koelbl, H.; Umek, W. Role of serum steroid hormones in women with stress urinary incontinence: A case–control study. BJU Int. 2017, 120, 416–421. [Google Scholar] [CrossRef] [Green Version]
- Movig, K.L.; Leufkens, H.G.; Belitser, S.V.; Lenderink, A.W.; Egberts, A.C. Selective serotonin reuptake inhibitor-induced urinary incontinence. Pharmacoepidemiol. Drug Saf. 2002, 11, 271–279. [Google Scholar] [CrossRef]
- Arasteh, A.; Mostafavi, S.; Vahed, S.Z.; Montazeri, S.S. An association between incontinence and antipsychotic drugs: A systematic review. Biomed. Pharmacother. 2021, 142, 112027. [Google Scholar] [CrossRef]
- Tsakiris, P.; Oelke, M.; Michel, M.C. Drug-induced urinary incontinence. Drugs Aging 2008, 25, 541–549. [Google Scholar] [CrossRef]
- Ng, Q.X.; Lim, Y.L.; Loke, W.; Yeo, W.S.; Chee, K.T. Obsessive-Compulsive Disorders and Functional Urinary Disorders: A Fortuitous Association? Behav. Sci. 2021, 11, 89. [Google Scholar] [CrossRef]
- Vanderlinden, J.; Dalle Grave, R.; Fernandez, F.; Vandereycken, W.; Pieters, G.; Noorduin, C. Which factors do provoke binge eating? An exploratory study in eating disorder patients. Eat. Weight. Disord.-Stud. Anorex. Bulim. Obes. 2004, 9, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Winters, J.C.; Dmochowski, R.R.; Goldman, H.B.; Herndon, C.A.; Kobashi, K.C.; Kraus, S.R.; Lemack, G.E.; Nitti, V.W.; Rovner, E.S.; Wein, A.J. Urodynamic studies in adults: AUA/SUFU guideline. J. Urol. 2012, 188, 2464–2472. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ng, Q.X.; Lim, Y.L.; Loke, W.; Chee, K.T.; Lim, D.Y. Females with Eating Disorders and Urinary Incontinence: A Psychoanalytic Perspective. Int. J. Environ. Res. Public Health 2022, 19, 4874. https://doi.org/10.3390/ijerph19084874
Ng QX, Lim YL, Loke W, Chee KT, Lim DY. Females with Eating Disorders and Urinary Incontinence: A Psychoanalytic Perspective. International Journal of Environmental Research and Public Health. 2022; 19(8):4874. https://doi.org/10.3390/ijerph19084874
Chicago/Turabian StyleNg, Qin Xiang, Yu Liang Lim, Wayren Loke, Kuan Tsee Chee, and Donovan Yutong Lim. 2022. "Females with Eating Disorders and Urinary Incontinence: A Psychoanalytic Perspective" International Journal of Environmental Research and Public Health 19, no. 8: 4874. https://doi.org/10.3390/ijerph19084874
APA StyleNg, Q. X., Lim, Y. L., Loke, W., Chee, K. T., & Lim, D. Y. (2022). Females with Eating Disorders and Urinary Incontinence: A Psychoanalytic Perspective. International Journal of Environmental Research and Public Health, 19(8), 4874. https://doi.org/10.3390/ijerph19084874