Translation, Cross-Cultural Adaptation, and Validation of the Malay-Version of the Factors Influencing Community Willingness to Perform Cardiopulmonary Resuscitation and Use an Automated External Defibrillator Questionnaire
Abstract
:1. Introduction
2. Methods
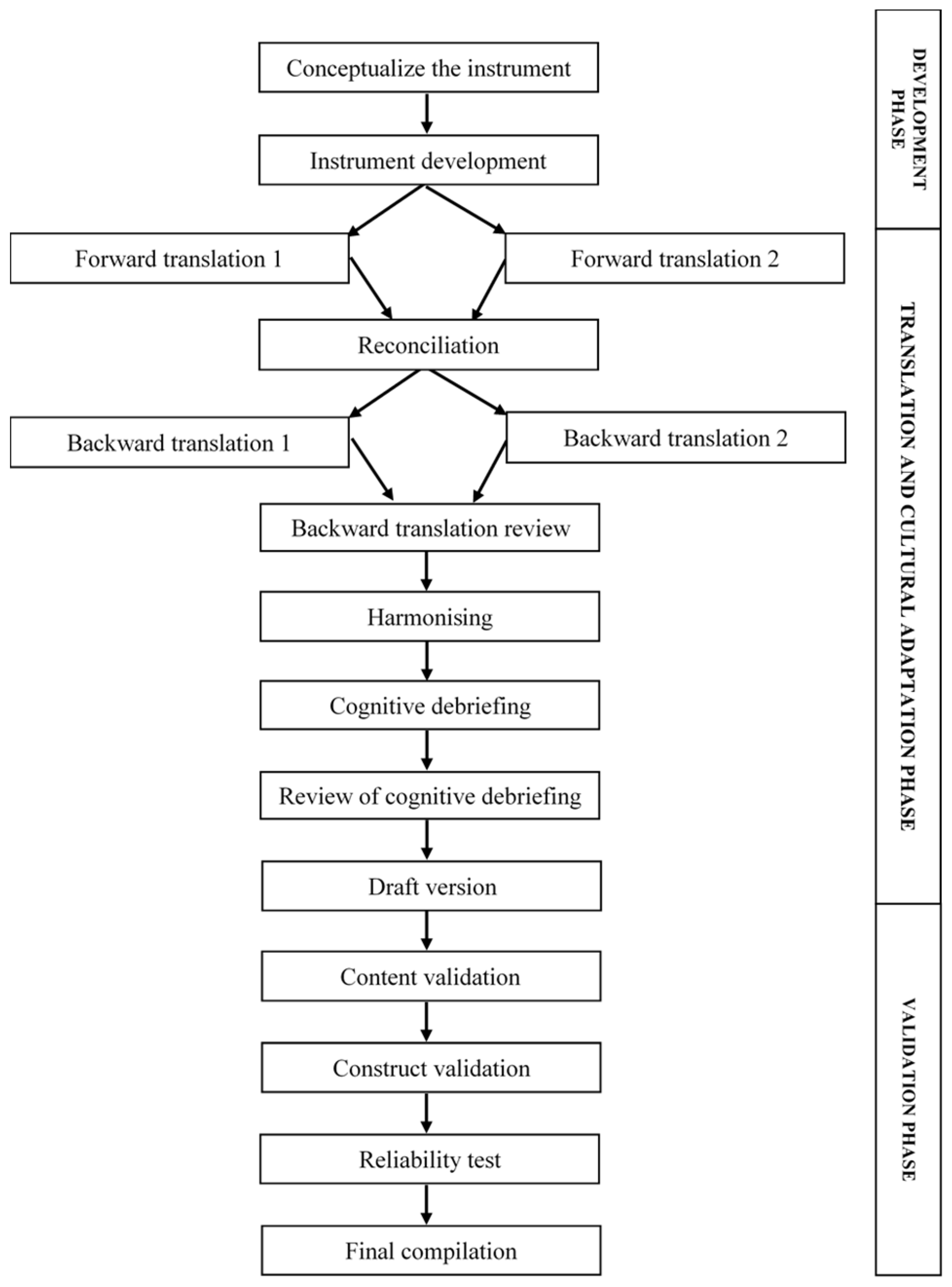
2.1. Phase 1: Development Phase
2.2. Phase 2: Translation and Cultural Adaptation Phase
2.3. Phase 3: Validation Phase
2.3.1. Content Validity
2.3.2. Construct Validity
3. Results
3.1. Sociodemographic Characteristics of the Participants
3.2. Conceptualisation of FIXED
3.3. Content Validity
3.4. Construct Validity
3.5. Reliability Testing
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. World Health Statistics 2019: Monitoring Health for the SDGs, Sustainable Development Goals; WHO: Geneva, Switzerland, 2019.
- Wong, C.X.; Brown, A.; Lau, D.H.; Chugh, S.S.; Albert, C.M.; Kalman, J.M.; Sanders, P. Epidemiology of Sudden Cardiac Death: Global and Regional Perspectives. Heart Lung Circ. 2019, 28, 6–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fröhlich, G.M.; Lyon, R.M.; Sasson, C.; Crake, T.; Whitbread, M.; Indermuehle, A.; Timmis, A.; Meier, P. Send Orders for Reprints to [email protected] Out-of-Hospital Cardiac Arrest-Optimal Management. Curr. Cardiol. Rev. 2013, 9, 316–324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nurumal, M.S.; Karim, S.S.A. Out of Hospital Cardiac Arrest in Kuala Lumpur: Incidence; Adherence to Protocol; and Issues: A Mixed Method Study. Malays. J. Public Health Med. 2015, 15, 94–103. [Google Scholar]
- Kuramoto, N.; Morimoto, T.; Kubota, Y.; Maeda, Y.; Seki, S.; Takada, K.; Hiraide, A. Public Perception of and Willingness to Perform Bystander CPR in Japan. Resuscitation 2008, 79, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Gräsner, J.T.; Lefering, R.; Koster, R.W.; Masterson, S.; Böttiger, B.W.; Herlitz, J.; Wnent, J.; Tjelmeland, I.B.M.; Ortiz, F.R.; Maurer, H.; et al. EuReCa ONE—27 Nations, ONE Europe, ONE Registry: A Prospective One Month Analysis of out-of-Hospital Cardiac Arrest Outcomes in 27 Countries in Europe. Resuscitation 2016, 105, 188–195. [Google Scholar] [CrossRef] [Green Version]
- Ong, M.E.H.; Do Shin, S.; De Souza, N.N.A.; Tanaka, H.; Nishiuchi, T.; Song, K.J.; Ko, P.C.I.; Leong, B.S.H.; Khunkhlai, N.; Naroo, G.Y.; et al. Outcomes for Out-of-Hospital Cardiac Arrests across 7 Countries in Asia: The Pan Asian Resuscitation Outcomes Study (PAROS). Resuscitation 2015, 96, 100–108. [Google Scholar] [CrossRef] [PubMed]
- American Heart Association. Highlights of the 2020 American Heart Association Guidelines For CPR and ECC; American Heart Association: Dallas, TX, USA, 2020; Volume 53. [Google Scholar]
- Haydon, G.; van der Riet, P.; Maguire, J. Survivors’ Quality of Life after Cardiopulmonary Resuscitation: An Integrative Review of the Literature. Scand. J. Caring Sci. 2017, 31, 6–26. [Google Scholar] [CrossRef]
- Hansen, C.M.; Rosenkranz, S.M.; Folke, F.; Zinckernagel, L.; Tjørnhøj-Thomsen, T.; Torp-Pedersen, C.; Sondergaard, K.B.; Nichol, G.; Rod, M.H. Lay Bystanders’ Perspectives on What Facilitates Cardiopulmonary Resuscitation and Use of Automated External Defibrillators in Real Cardiac Arrests. J. Am. Heart Assoc. 2017, 6, e004572. [Google Scholar] [CrossRef] [Green Version]
- Perkins, G.D.; Jacobs, I.G.; Nadkarni, V.M.; Berg, R.A.; Bhanji, F.; Biarent, D.; Bossaert, L.L.; Brett, S.J.; Chamberlain, D.; De Caen, A.R.; et al. Cardiac Arrest and Cardiopulmonary Resuscitation Outcome Reports: Update of the Utstein Resuscitation Registry Templates for out-of-Hospital Cardiac Arrest: A Statement for Healthcare Professionals from a Task Force of the International Liaison Committee. Circulation 2015, 132, 1286–1300. [Google Scholar] [CrossRef]
- Regard, S.; Rosa, D.; Suppan, M.; Giangaspero, C.; Larribau, R.; Niquille, M.; Sarasin, F.; Suppan, L. Evolution of Bystander Intention to Perform Resuscitation since Last Training: Web-Based Survey. JMIR Form. Res. 2020, 4, e24798. [Google Scholar] [CrossRef]
- Son, J.W.; Ryoo, H.W.; Moon, S.; Kim, J.; Ahn, J.Y.; Park, J.B.; Seo, K.S.; Kim, J.K.; Kim, Y.J. Association between Public Cardiopulmonary Resuscitation Education and the Willingness to Perform Bystander Cardiopulmonary Resuscitation: A Metropolitan Citywide Survey. Clin. Exp. Emerg. Med. 2017, 4, 80–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohamad Marzuki, M.F.; Yaacob, N.A.; Yaacob, N.M. Translation, Cross-Cultural Adaptation, and Validation of the Malay Version of the System Usability Scale Questionnaire for the Assessment of Mobile Apps. JMIR Hum. Factors 2018, 5, e10308. [Google Scholar] [CrossRef] [PubMed]
- Wild, D.; Grove, A.; Martin, M.; Eremenco, S.; Mcelroy, S.; Verjee-Lorenz, A.; Erikson, P. Principles of Good Practice for the translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: Report of the iSPOR task Force for translation and Cultural Adaptation. Value Health 2005, 8, 94–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Panchal, A.R.; Fishman, J.; Camp-Rogers, T.; Starodub, R.; Merchant, R.M. An “Intention-Focused” Paradigm for Improving Bystander CPR Performance. Resuscitation 2015, 88, 48–51. [Google Scholar] [CrossRef] [Green Version]
- Ajzen, I. The Theory of Planned Behavior: Frequently Asked Questions. Hum. Behav. Emerg. Technol. 2020, 2, 314–324. [Google Scholar] [CrossRef]
- Fan, K.L.; Leung, L.P.; Poon, H.T.; Chiu, H.Y.; Liu, H.L.; Tang, W.Y. Public Knowledge of How to Use an Automatic External Defibrillator in Out-of-Hospital Cardiac Arrest in Hong Kong. Hong Kong Med. J. 2016, 22, 582–588. [Google Scholar] [CrossRef] [Green Version]
- Karuthan, S.R.; Firdaus, P.J.F.B.; Angampun, A.D.A.G.; Chai, X.J.; Sagan, C.D.; Ramachandran, M.; Perumal, S.; Karuthan, M.; Manikam, R.; Chinna, K. Knowledge of and Willingness to Perform Hands-Only Cardiopulmonary Resuscitation among College Students in Malaysia. Medicine 2019, 98, e18466. [Google Scholar] [CrossRef]
- Chew, K.S.; Liaw, S.Y.; Ahmad Zahedi, A.Z.; Wong, S.S.L.; Singmamae, N.; Kaushal, D.N.; Chan, H.C. Development, Validation and Translation of Cardiopulmonary Resuscitation and Automated External Defibrillator Training and Placement Bilingual Questionnaire. BMC Res. Notes 2019, 12, 670. [Google Scholar] [CrossRef] [Green Version]
- Cohen, J. A Coefficient of Agreement for Nominal Scales. Educ. Psychol. Meas. 1960, 20, 37–46. [Google Scholar] [CrossRef]
- Lynn, M.R. Determination and Quantification of Content Validity. Nurs. Res. 1986, 35, 382–386. [Google Scholar] [CrossRef]
- McHugh, M.L. Interrater Reliability: The Kappa Statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Yusoff, M.S.B. ABC of Content Validation and Content Validity Index Calculation. Educ. Med. J. 2019, 11, 49–54. [Google Scholar] [CrossRef]
- Polit, D.F.; Beck, C.T. The Content Validity Index: Are You Sure You Know What’s Being Reported? Critique and Recommendations. Res. Nurs. Health 2006, 29, 489–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abdollahpour, I.; Nedjat, S.; Noroozian, M.; Majdzadeh, R. The Process of Content Validity in Instrument Development. Iran. Epidemiol. 2011, 64, 66–74. [Google Scholar]
- Wynd, C.A.; Schmidt, B.; Schaefer, M.A. Two Quantitative Approaches for Estimating Content Validity. West. J. Nurs. Res. 2003, 25, 508–518. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [Green Version]
- Bonett, D.G. Sample Size Requirements for Testing and Estimating Coefficient Alpha. J. Educ. Behav. Stat. 2002, 27, 335–340. [Google Scholar] [CrossRef]
- Bonett, D.; Wright, T. Cronbach’s Alpha Reliability: Interval Estimation, Hypothesis Testing, and Sample Size Planning. J. Organ. Behav. 2014, 36, 3–15. [Google Scholar] [CrossRef]
- Cattell, R.B. The Scree Test for the Number of Factors. Multivar. Behav. Res. 1966, 1, 245–276. [Google Scholar] [CrossRef]
- Hershberger, S.L. Encyclopedia of Statistics in Behavioral Science; Everitt, B.S., Howell, D.C., Eds.; John Wiley and Sons Inc.: New York, NY, USA, 2005. [Google Scholar]
- Kaiser, H.F. An Index of Factorial Simplicity. Psychometrika 1974, 39, 31–36. [Google Scholar] [CrossRef]
- Velicer, W.F.; Fava, J.L. Effects of Variable and Subject Sampling on Factor Pattern Recovery. Psychol. Methods 1998, 3, 231. [Google Scholar] [CrossRef]
- Williams, B.; Onsman, A.; Brown, T. Exploratory Factor Analysis: A Five-Step Guide for Novices EDUCATION Exploratory Factor Analysis: A Five-Step Guide for Novices. Australas. J. Paramed. 2012, 8, 1–13. [Google Scholar]
- Osborne, J.W.; Costello, A.B.; Kellow, J.T. Best Practices in Exploratory Factor Analysis: Four recommendations for getting the most from your analysis. Pract. Assess. Res. Eval. 2011, 10, 7. [Google Scholar] [CrossRef]
- Hair, J.F.; Anderson, R.E.; Tatham, R.L.; Black, W.C. Multivariate Data Analysis; Prentice-Hall: Englewood Cliffs, NJ, USA, 1995. [Google Scholar]
- Samuels, P. Advice on Exploratory Factor Analysis Electronic Multiple Choice Assessment in Mathematics (ELMUCHAS). View Project Reliability Analysis and Factor Analysis View Project Advice on Exploratory Factor Analysis; Birmingham City University: Birmingham, UK, 2017. [Google Scholar]
- Tsang, S.; Royse, C.F.; Terkawi, A.S. Guidelines for Developing, Translating, and Validating a Questionnaire in Perioperative and Pain Medicine. Saudi J. Anaesth. 2017, 11, S80–S89. [Google Scholar] [CrossRef] [PubMed]
- Cronbach, L.J. Coefficient Alpha and the Internal Structure of Tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef] [Green Version]
- Tavakol, M.; Dennick, R. Making Sense of Cronbach’s Alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef]
- DeVellis, R.F. Scale Development: Theory and Applications, 2nd ed.; SAGE Publications Inc.: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 4th ed.; SAGE Publications Inc.: Thousand Oaks, CA, USA, 2013. [Google Scholar]
- Hinton, P.R.; Brownlow, C.; Mcmurray, I.; Cozens, B. SPSS Explained; Routledge Inc.: East Sussex, UK, 2004. [Google Scholar]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice; Prentice Hall: Hoboken, NJ, USA, 2000. [Google Scholar]
- Hair, J.F.; Black, W.C.; Black, B.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis: A Global Perspective, 7th ed.; Pearson Education: Upper Saddle River, NJ, USA, 2014. [Google Scholar]
- Straub, D.; Gefen, D. Validation Guidelines for IS Positivist Research. Commun. Assoc. Inf. Syst. 2004, 13, 24. [Google Scholar] [CrossRef]
- Strömsöe, A.; Svensson, L.; Axelsson, Å.B.; Claesson, A.; Göransson, K.E.; Nordberg, P.; Herlitz, J. Improved Outcome in Sweden after Out-of-Hospital Cardiac Arrest and Possible Association with Improvements in Every Link in the Chain of Survival. Eur. Heart J. 2015, 36, 863–871. [Google Scholar] [CrossRef]
- Wissenberg, M.; Lippert, F.K.; Folke, F.; Weeke, P.; Hansen, C.M.; Christensen, E.F.; Jans, H.; Hansen, P.A.; Lang-Jensen, T.; Olesen, J.B.; et al. Association of National Initiatives to Improve Cardiac Arrest Management with Rates of Bystander Intervention and Patient Survival after Out-of-Hospital Cardiac Arrest. J. Am. Med. Assoc. 2013, 310, 1377–1384. [Google Scholar] [CrossRef] [Green Version]
- Bobrow, B.J.; Spaite, D.W.; Berg, R.A.; Stolz, U.; Sanders, A.B.; Kern, K.B.; Vadeboncoeur, T.F.; Clark, L.L.; Gallagher, J.V.; Stapczynski, J.S.; et al. Chest Compression-Only CPR by Lay Rescuers and Survival from out-of-Hospital Cardiac Arrest. J. Am. Med. Assoc. 2010, 304, 1447–1454. [Google Scholar] [CrossRef] [Green Version]
- Rodrigues, I.B.; Adachi, J.D.; Beattie, K.A.; MacDermid, J.C. Development and Validation of a New Tool to Measure the Facilitators, Barriers and Preferences to Exercise in People with Osteoporosis. BMC Musculoskelet. Disord. 2017, 18, 540. [Google Scholar] [CrossRef] [Green Version]
- Kraemer, H.C.; Periyakoil, V.S.; Noda, A. Kappa Coefficients in Medical Research. Stat. Med. 2002, 21, 2109–2129. [Google Scholar] [CrossRef]
- Vach, W. The Dependence of Cohen’s Kappa on the Prevalence Does Not Matter. J. Clin. Epidemiol. 2005, 58, 655–661. [Google Scholar] [CrossRef]
- Darroch, J.N.; McCloud, P.I. Category Distinguishability and Observer Agreement. Aust. J. Stat. 1986, 28, 371–388. [Google Scholar] [CrossRef]
- Beavers, A.S.; Lounsbury, J.W.; Richards, J.K.; Huck, S.W.; Skolits, G.J.; Esquivel, S.L. Practical Considerations for Using Exploratory Factor Analysis in Educational Research. Pract. Assess. Res. Eval. 2013, 18, 6. [Google Scholar]


| Characteristic | Frequency (n) | Percentage (%) |
|---|---|---|
| Gender | ||
| (a) Male | 51 | 51 |
| (b) Female | 49 | 49 |
| Age (years) | ||
| (a) below 40 | 80 | 80 |
| (b) 40 and above | 20 | 20 |
| Ethnicity | ||
| (a) Malay | 77 | 77 |
| (b) Chinese | 15 | 15 |
| (c) Indian | 6 | 6 |
| (d) Others | 2 1 | 2 |
| Level of education | ||
| (a) Secondary education | 15 | 15 |
| (b) Higher (Certificate/Diploma/Degree) | 85 | 85 |
| Marital Status | ||
| (a) Single | 44 | 44 |
| (b) Married | 53 | 53 |
| (c) Widow/Widower | 3 | 3 |
| Residential area | ||
| (a) City | 61 | 61 |
| (b) Rural | 39 | 39 |
| Employment Status | ||
| (a) Health workers | 42 | 42 |
| (b) Employers | 28 | 28 |
| (c) Self-employed | 8 | 8 |
| (d) Students | 15 | 15 |
| (e) Pensions | 5 | 5 |
| (f) Housewives | 1 | 1 |
| (g) Not working | 1 | 1 |
| Total household income (RM per month) | ||
| (a) B40 (below RM 4850) 2 | 59 | 59 |
| (b) Not B40 (RM 4850 and above) | 41 | 41 |
| Medical history of chronic illness | ||
| (a) Yes | 3 | 3 |
| (b) No | 97 | 97 |
| Medical history of family members living together with chronic illnesses | ||
| (a) Yes | 34 | 34 |
| (b) No | 66 | 66 |
| Experience of witnessing the incidence of cardiac arrest | ||
| (a) Ever | 38 | 38 |
| (b) Never | 62 | 62 |
| Have performed CPR on a victim who suffered a cardiac arrest | ||
| (a) Ever | 35 | 35 |
| (b) Never | 65 | 65 |
| Item | Construct | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
| S-CVI/Ave | 1.0 | 1.0 | 1.0 | 0.88 | 0.95 | 1.0 | 1.0 | 1.0 | 1.0 |
| S-CVI/UA | 1.0 | 1.0 | 1.0 | 0.38 | 0.75 | 1.0 | 1.0 | 1.0 | 1.0 |
| Average proportion of items | 1.0 | 1.0 | 1.0 | 0.88 | 0.95 | 1.0 | 1.0 | 1.0 | 1.0 |
| Construct FIXED | Kaiser–Meyer–Olkin Measure of Sampling Adequacy | Bartlett’s Test of Sphericity | ||
|---|---|---|---|---|
| Approx. Chi-Square | df | Sig. | ||
| FIXED Instrument | 0.777 | 3345.614 | 946 | <0.001 |
| Perception | 0.802 | 493.299 | 45 | <0.001 |
| Attitude | 0.643 | 203.192 | 28 | <0.001 |
| Perceived norms | 0.582 | 48.267 | 6 | <0.001 |
| Self-efficacy | 0.786 | 200.929 | 10 | <0.001 |
| Intention | 0.854 | 370.516 | 15 | <0.001 |
| Behaviour | 0.818 | 407.524 | 6 | <0.001 |
| Barriers | 0.812 | 504.038 | 21 | <0.001 |
| Item No | Item | Factor Loading | ||||||
|---|---|---|---|---|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Factor 6 | Factor 7 | ||
| Perception | ||||||||
| Implementation Strategies of the AED | ||||||||
| 2 | The signage that shows the location of the AED is clear | 0.922 | ||||||
| 3 | The AED is located in a location that is easily accessible at all times (including after office hours) | 0.908 | ||||||
| 4 | The steps in the AED instructional poster on how to use the AED are easy to follow | 0.853 | ||||||
| 1 | The AED is clearly visible | 0.813 | ||||||
| 5 | The AED is located at a secure site | 0.776 | ||||||
| Community’s perception on the importance of CPR and AED | ||||||||
| 6 | CPR and AED are important in saving life | 0.869 | ||||||
| 7 | It is important for an AED to be available in the place where I work. | 0.851 | ||||||
| 8 | Using an AED is important on any unresponsive victims | 0.457 | ||||||
| Community’s perception on the AED handling training | ||||||||
| 9 | Person who handles an AED requires formal training. | 0.840 | ||||||
| 10 | AED practice drills should be performed on a regular basis | 0.817 | ||||||
| Attitude | ||||||||
| Fearful of CPR and AED | ||||||||
| 15 | Not being afraid of worsening the victim’s condition | 0.805 | ||||||
| 16 | Not being afraid of legal action | 0.771 | ||||||
| 14 | Not being afraid of hurting the victim by performing CPR | 0.768 | ||||||
| 13 | Not being afraid of disease transmission | 0.682 | ||||||
| Courage for CPR and AED | ||||||||
| 18 | Belief that knowing CPR is important for the society | 0.871 | ||||||
| 11 | Thinking that performing resuscitation could save a life | 0.811 | ||||||
| 17 | Being proud of performing resuscitation successfully | 0.744 | ||||||
| Importance of CPR and AED | ||||||||
| 12 | Knowing the importance of starting a resuscitation before EMS arrival | 0.956 | ||||||
| Perceived norms | ||||||||
| Relatives | ||||||||
| 20 | Belief that relatives want the subject to resuscitate them if needed | 0.842 | ||||||
| 21 | Knowing that relatives are the most likely victim | 0.774 | ||||||
| 19 | Belief that relatives would be proud if the participant performed resuscitation | 0.661 | ||||||
| Community | ||||||||
| 22 | Diffusion of responsibility | 0.924 | ||||||
| Self-efficacy | ||||||||
| Intrinsic | ||||||||
| 24 | Feeling able to resuscitate | 0.904 | ||||||
| 25 | Feeling able to recognise a cardiac arrest | 0.896 | ||||||
| 27 | Knowing how to perform a resuscitation | 0.880 | ||||||
| Extrinsic | ||||||||
| 26 | Not believing that only health care professionals can adequately perform resuscitation | 0.787 | ||||||
| 23 | Knowledge of the emergency number | 0.667 | ||||||
| Intention | ||||||||
| 31 | Perform CPR on an elderly person | 0.901 | ||||||
| 32 | Perform CPR on a relative or family member | 0.882 | ||||||
| 28 | Perform CPR on a stranger | 0.869 | ||||||
| 30 | Perform CPR on a child | 0.864 | ||||||
| 33 | Using an AED | 0.692 | ||||||
| 29 | Perform CPR on a victim of trauma | 0.593 | ||||||
| Behaviour | ||||||||
| 37 | Confident to use an AED on an unresponsive victim | 0.942 | ||||||
| 34 | Confident to perform CPR | 0.938 | ||||||
| 35 | Confident to use an AED | 0.937 | ||||||
| 36 | Confident in recognising victim with no signs of life | 0.897 | ||||||
| Barriers | ||||||||
| 43 | Concerned that I might be sued if I perform emergency CPR inappropriately | 0.857 | ||||||
| 39 | Concerned in injuring the victim when performing CPR | 0.846 | ||||||
| 44 | Concerned that I might be sued if I used an AED inappropriately | 0.828 | ||||||
| 41 | Concerned in injuring the victim if I use an AED device during CPR | 0.819 | ||||||
| 40 | Concerned in injuring myself when performing CPR | 0.771 | ||||||
| 42 | Concerned in injuring myself if I use an AED device during CPR | 0.748 | ||||||
| 38 | Concerned in getting infection from the victim when performing CPR | 0.699 | ||||||
| Construct and Sub-Construct | Item | Corrected Item-Total Correlation | Cronbach’s Alpha before Deleting (44 Items) | Cronbach’s Alpha after Deleting (40 Items) |
|---|---|---|---|---|
| Perception (Implementation Strategies of the AED) | The signage that shows the location of the AED is clear | 0.855 | 0.915 | 0.915 |
| The AED is located in a location that is easily accessible at all times (including after office hours) | 0.835 | |||
| The steps in the AED instructional poster on how to use the AED are easy to follow | 0.790 | |||
| The AED is clearly visible | 0.713 | |||
| The AED is located at a secure site | 0.748 | |||
| Perception (Community’s perception on the importance of CPR and AED) | CPR & AED are important in saving life | 0.482 | 0.637 | 0.637 |
| It is important for an AED to be available in the place where I work. | 0.567 | |||
| Using an AED is important on any unresponsive victims | 0.378 | |||
| Perception (Community’s perception on the AED handling training) | Person who handles an AED requires formal training. | 0.462 | 0.632 | 0.632 |
| AED practice drills should be performed on a regular basis | 0.462 | |||
| Attitude (Fearful of CPR and AED) | Not being afraid of worsening the victim’s condition | 0.617 | 0.755 | 0.755 |
| Not being afraid of legal action | 0.568 | |||
| Not being afraid of hurting the victim by performing CPR | 0.589 | |||
| Not being afraid of disease transmission | 0.443 | |||
| Attitude (Courage for CPR and AED) | Belief that knowing CPR is important for the society | 0.634 | 0.693 | 0.693 |
| Thinking that performing resuscitation could save a life | 0.546 | |||
| Being proud of performing resuscitation successfully | 0.483 | |||
| Attitude (Importance of CPR and AED) | Knowing the importance of starting a resuscitation before EMS arrival | Component eliminated (one item) | ||
| Perceived norms (Relatives) | Belief that relatives want the subject to resuscitate them if needed | 0.575 | 0.633 | 0.633 |
| Knowing that relatives are the most likely victim | 0.395 | |||
| Belief that relatives would be proud if the participant performed resuscitation | 0.379 | |||
| Perceived norms (Community) | Diffusion of responsibility | Component eliminated (one item) | ||
| Self-efficacy (Intrinsic) | Feeling able to resuscitate | 0.812 | 0.895 | 0.895 |
| Feeling able to recognise a cardiac arrest | 0.799 | |||
| Knowing how to perform a resuscitation | 0.778 | |||
| Self-efficacy (Extrinsic) | Not believing that only health care professionals can adequately perform resuscitation | 0.067 | 0.111 | Component eliminated (two item) |
| Knowledge of the emergency number | 0.067 | |||
| Intention | Perform CPR on an elderly person | 0.815 | 0.878 | 0.878 |
| Perform CPR on a relative or family member | 0.785 | |||
| Perform CPR on a stranger | 0.772 | |||
| Perform CPR on a child | 0.761 | |||
| Using an AED | 0.586 | |||
| Perform CPR on a victim of trauma | 0.491 | |||
| Behaviour | Confident to use an AED on an unresponsive victim | 0.897 | 0.945 | 0.945 |
| Confident to perform CPR | 0.885 | |||
| Confident to use an AED | 0.887 | |||
| Confident in recognising victim with no signs of life | 0.818 | |||
| Barriers | Concerned that I might be sued if I perform emergency CPR inappropriately | 0.786 | 0.903 | 0.903 |
| Concerned in injuring the victim when performing CPR | 0.775 | |||
| Concerned that I might be sued if I used an AED inappropriately | 0.750 | |||
| Concerned in injuring the victim if I use an AED device during CPR | 0.735 | |||
| Concerned in injuring myself when performing CPR | 0.688 | |||
| Concerned in injuring myself if I use an AED device during CPR | 0.662 | |||
| Concerned in getting infection from the victim when performing CPR | 0.604 |
| Construct Dan Sub-Construct | ICC and 95% Confidence Interval | Cronbach’s Alpha | ||
|---|---|---|---|---|
| Construct | Overall | Construct | Construct | |
| Perception (Implementation Strategies of the AED) | 0.932 (0.898–0.958) | 0.723 (0.614–0.819) | 0.915 | 0.849 |
| Perception (Community’s perception on the importance ofCPR and AED) | 0.643 (0.457–0.782) | 0.637 | ||
| Perception (Community’s perception on the AED handling training) | 0.502 (0.216–0.702) | 0.632 | ||
| Attitude (Fearful of CPR and AED) | 0.729 (0.585–0.835) | 0.755 | ||
| Attitude (Courage for CPR and AED) | 0.746 (0.608–0.846) | 0.693 | ||
| Perceived norms (Relatives) | 0.760 (0.635–0.854) | 0.633 | ||
| Self-efficacy(Intrinsic) | 0.911 (0.863–0.946) | 0.895 | ||
| Intention | 0.875 (0.813–0.922) | 0.878 | ||
| Behaviour | 0.922 (0.881–0.952) | 0.945 | ||
| Barriers | 0.896 (0.845–0.935) | 0.903 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Daud, A.; Mohammed Nawi, A.; Aizuddin, A.N.; Yahya, M.F. Translation, Cross-Cultural Adaptation, and Validation of the Malay-Version of the Factors Influencing Community Willingness to Perform Cardiopulmonary Resuscitation and Use an Automated External Defibrillator Questionnaire. Int. J. Environ. Res. Public Health 2022, 19, 4882. https://doi.org/10.3390/ijerph19084882
Daud A, Mohammed Nawi A, Aizuddin AN, Yahya MF. Translation, Cross-Cultural Adaptation, and Validation of the Malay-Version of the Factors Influencing Community Willingness to Perform Cardiopulmonary Resuscitation and Use an Automated External Defibrillator Questionnaire. International Journal of Environmental Research and Public Health. 2022; 19(8):4882. https://doi.org/10.3390/ijerph19084882
Chicago/Turabian StyleDaud, Amsyar, Azmawati Mohammed Nawi, Azimatun Noor Aizuddin, and Mohammad Fadhly Yahya. 2022. "Translation, Cross-Cultural Adaptation, and Validation of the Malay-Version of the Factors Influencing Community Willingness to Perform Cardiopulmonary Resuscitation and Use an Automated External Defibrillator Questionnaire" International Journal of Environmental Research and Public Health 19, no. 8: 4882. https://doi.org/10.3390/ijerph19084882








