Mental Health Outcomes in Australian Healthcare and Aged-Care Workers during the Second Year of the COVID-19 Pandemic
Abstract
:1. Introduction
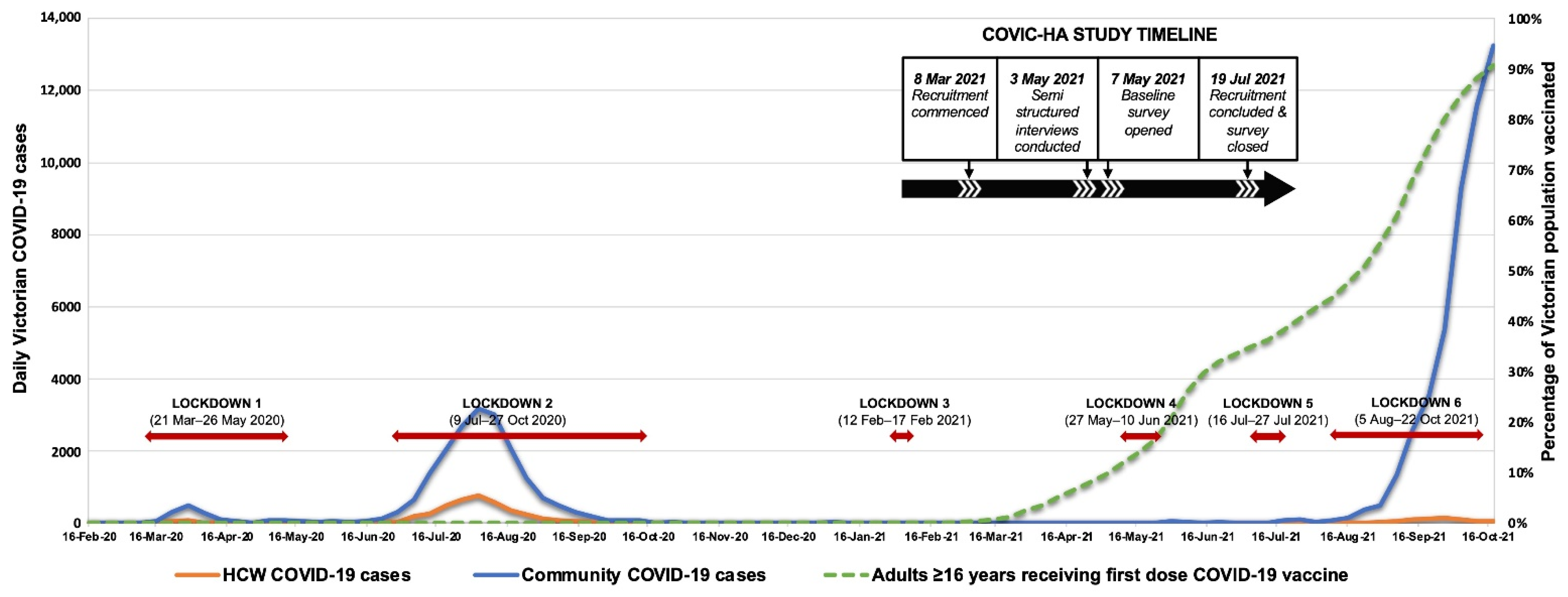
2. Materials and Methods
Data Collection and Analysis
3. Results
3.1. Mental Health and Wellbeing
3.2. Work Home and Lives
3.3. Perspectives on Vaccination and Workplace Supports
3.4. HCW Experiences
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pearce, N.; Lawlor, D.A.; Brickley, E.B. Comparisons between countries are essential for the control of COVID-19. Int. J. Epidemiol. 2020, 49, 1059–1062. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Regional Population. ABS; 2019-20 [Updated 30 March 2021]. Available online: https://www.abs.gov.au/statistics/people/population/regional-population/2019-20#media-releases (accessed on 5 October 2021).
- Victorian Department of Health COVID-19 Writing Group. Population-based analysis of the epidemiological features of COVID-19 epidemics in Victoria, Australia, January 2020–March 2021, and their suppression through comprehensive control strategies. Lancet Reg. Health West Pac. 2021, 17, 100297. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Weekly Operational Update on COVID-19—29 December 2020. Geneva: World Health Organization. 2020. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update---29-december-2020 (accessed on 21 March 2022).
- De Foo, C.; Grépin, K.A.; Cook, A.R.; Hsu, L.Y.; Bartos, M.; Singh, S.; Asgari, N.; Teo, Y.Y.; Heymann, D.L.; Legido-Quigley, H. Navigating from SARS-CoV-2 elimination to endemicity in Australia, Hong Kong, New Zealand, and Singapore. Lancet 2021, 398, 1547–1551. [Google Scholar] [CrossRef]
- Fisher, J.; Tran, T.; Hammarberg, K.; Nguyen, H.; Stocker, R.; Rowe, H.; Sastri, J.; Popplestone, S.; Kirkman, M. Quantifying the mental health burden of the most severe covid-19 restrictions: A natural experiment. J. Affect. Disord. 2021, 293, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, D.; Sheehan, L.; Petrie, D.; van Vreden, C.; Whiteford, P.; Collie, A. The health impacts of a 4-month long community-wide COVID-19 lockdown: Findings from a prospective longitudinal study in the state of Victoria, Australia. PLoS ONE 2022, 17, e0266650. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.H.; Drew, D.A.; Graham, M.S.; Joshi, A.D.; Guo, C.-G.; Ma, W.; Mehta, R.S.; Warner, E.T.; Sikavi, D.R.; Lo, C.-H.; et al. Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health 2020, 5, e475–e483. [Google Scholar] [CrossRef]
- Sahebi, A.; Nejati, B.; Moayedi, S.; Yousefi, K.; Torres, M.; Golitaleb, M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: An umbrella review of meta-analyses. Prog. Neuro Psychopharmacol. Biol. Psychiatry 2021, 107, 110247. [Google Scholar] [CrossRef]
- Saragih, I.D.; Tonapa, S.I.; Saragih, I.S.; Advani, S.; Batubara, S.O.; Suarilah, I.; Lin, C.J. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2021, 121, 104002. [Google Scholar] [CrossRef]
- Marvaldi, M.; Mallet, J.; Dubertret, C.; Moro, M.R.; Guessoum, S.B. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2021, 126, 252–264. [Google Scholar] [CrossRef]
- Denning, M.; Goh, E.T.; Tan, B.; Kanneganti, A.; Almonte, M.; Scott, A.; Martin, G.; Clarke, J.; Sounderajah, V.; Markar, S.; et al. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the Covid-19 pandemic: A multinational cross-sectional study. PLoS ONE 2021, 16, e0238666. [Google Scholar] [CrossRef]
- Khasne, R.W.; Dhakulkar, B.S.; Mahajan, H.C. Burnout among Healthcare Workers during COVID-19 Pandemic in India: Results of a Questionnaire-based Survey. Indian J. Crit. Care Med. 2020, 24, 664–671. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.C.; Quiban, C.; Sloan, C.; Montejano, A. Predictors of poor mental health among nurses during COVID-19 pandemic. Nurs. Open 2020, 8, 900–907. [Google Scholar] [CrossRef] [PubMed]
- Chou, R.; Dana, T.; Buckley, D.I.; Selph, S.; Fu, R.; Totten, A.M. Epidemiology of and Risk Factors for Coronavirus Infection in Health Care Workers: A living rapid review. Ann. Intern. Med. 2020, 173, 120–136. [Google Scholar] [CrossRef] [PubMed]
- Dobson, H.; Malpas, C.B.; Burrell, A.J.; Gurvich, C.; Chen, L.; Kulkarni, J.; Winton-Brown, T. Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Australas. Psychiatry 2020, 29, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Smallwood, N.; Karimi, L.; Bismark, M.; Putland, M.; Johnson, D.; Dharmage, S.C.; Barson, E.; Atkin, N.; Long, C.; Ng, I.; et al. High levels of psychosocial distress among Australian frontline healthcare workers during the COVID-19 pandemic: A cross-sectional survey. Gen. Psychiatry 2021, 34, e100577. [Google Scholar] [CrossRef] [PubMed]
- Ananda-Rajah, M.; Veness, B.; Berkovic, D.; Parker, C.; Kelly, G.; Ayton, D. Hearing the voices of Australian healthcare workers during the COVID-19 pandemic. BMJ Lead. 2020, 5, 31–35. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [Green Version]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [Green Version]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2010, 16, 606–613. [Google Scholar] [CrossRef]
- Thoresen, S.; Tambs, K.; Hussain, A.; Heir, T.; Johansen, V.A.; Bisson, J.I. Brief measure of posttraumatic stress reactions: Impact of Event Scale-6. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 45, 405–412. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P.; Maslach, C.; Jackson, S.E.; Leiter, M.P. Maslach Burnout Inventory. In Evaluating Stress: A Book of Resources, 3rd ed.; Zalaquett, C.P., Wood, R.J., Eds.; Evaluating Stress: Lanham, MD, USA, 1997; pp. 191–218. [Google Scholar]
- International Wellbeing Group. Personal Wellbeing Index, 5th ed.; Australian Centre on Quality of Life, Deakin University: Melbourne, Australia, 2013; Available online: http://www.acqol.com.au/uploads/pwi-a/pwi-a-english.pdf (accessed on 15 October 2021).
- Vaishnavi, S.; Connor, K.; Davidson, J.R. An abbreviated version of the Connor-Davidson Resilience Scale (CD-RISC), the CD-RISC2: Psychometric properties and applications in psychopharmacological trials. Psychiatry Res. 2007, 152, 293–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fisher, J.R.; Tran, T.D.; Hammarberg, K.; Sastry, J.; Nguyen, H.; Rowe, H.; Popplestone, S.; Stocker, R.; Stubber, C.; Kirkman, M. Mental health of people in Australia in the first month of COVID-19 restrictions: A national survey. Med. J. Aust. 2020, 213, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. 2033.0.55.001—Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia. 2016. Available online: https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/2033.0.55.0012016 (accessed on 11 September 2021).
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Kenward, M.G.; Roger, J.H. An improved approximation to the precision of fixed effects from restricted maximum likelihood. Comput. Stat. Data Anal. 2009, 53, 2583–2595. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Hutchinson, D.; Cummins, R.A.; Capic, T.; Khor, S.; Fuller-Tyszkiewicz, M.; Olsson, C.; Kerr-Smith, E.; Smith, B.; Markwell, K.; Yates, C.; et al. The Australian Unity Wellbeing Index 20th Anniversary Commemorative Edition. Australian Unity and Deakin University: Melbourne, Australia, 2021; p. 51. Retrieved from: Australian Centre on Quality of Life, School of Psychology, Deakin University. Available online: http://www.acqol.com.au/uploads/surveys/20yr-anniversary-report.pdf (accessed on 2 November 2021).
- Giorgi, G.; Lecca, L.I.; Alessio, F.; Finstad, G.L.; Bondanini, G.; Lulli, L.G.; Arcangeli, G.; Mucci, N. COVID-19-Related Mental Health Effects in the Workplace: A Narrative Review. Int. J. Environ. Res. Public Health 2020, 17, 7857. [Google Scholar] [CrossRef] [PubMed]
- Billings, J.; Ching, B.C.; Gkofa, V.; Greene, T.; Bloomfield, M. Experiences of frontline healthcare workers and their views about support during COVID-19 and previous pandemics: A systematic review and qualitative meta-synthesis. BMC Health Serv. Res. 2021, 21, 923. [Google Scholar] [CrossRef]
- Shah, D. Healthy worker effect phenomenon. Indian J. Occup. Environ. Med. 2009, 13, 77–79. [Google Scholar] [CrossRef]
- Foley, D.A.; Kirk, M.; Jepp, C.; Brophy-Williams, S.; Tong, S.Y.C.; Davis, J.S.; Blyth, C.C.; O’Brien, M.P.; Bowen, A.; Yeoh, D.K.; et al. COVID-19 and paediatric health services: A survey of paediatric physicians in Australia and New Zealand. J. Paediatr. Child Health 2020, 56, 1219–1224. [Google Scholar] [CrossRef]
- Newby, J.M.; O’Moore, K.; Tang, S.; Christensen, H.; Faasse, K. Acute mental health responses during the COVID-19 pandemic in Australia. PLoS ONE 2020, 15, e0236562. [Google Scholar] [CrossRef]
- Smallwood, N.; Karimi, L.; Pascoe, A.; Bismark, M.; Putland, M.; Johnson, D.; Dharmage, S.C.; Barson, E.; Atkin, N.; Long, C.; et al. Coping strategies adopted by Australian frontline health workers to address psychological distress during the COVID-19 pandemic. Gen. Hosp. Psychiatry 2021, 72, 124–130. [Google Scholar] [CrossRef] [PubMed]
- De Cieri, H.; Shea, T.; Cooper, B.; Oldenburg, B. Effects of Work-Related Stressors and Mindfulness on Mental and Physical Health Among Australian Nurses and Healthcare Workers. J. Nurs. Sch. 2019, 51, 580–589. [Google Scholar] [CrossRef] [PubMed]
- Courtney, J.A.; Francis, A.J.P.; Paxton, S. Caring for the Country: Fatigue, Sleep and Mental Health in Australian Rural Paramedic Shiftworkers. J. Community Health 2012, 38, 178–186. [Google Scholar] [CrossRef]
- Zhou, A.; Carder, M.; Gittins, M.; Agius, R. Work-related ill health in doctors working in Great Britain: Incidence rates and trends. Br. J. Psychiatry 2017, 211, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Booker, L.A.; Sletten, T.; Alvaro, P.K.; Barnes, M.; Collins, A.; Chai-Coetzer, C.L.; Naqvi, A.; McMahon, M.; Lockley, S.W.; Rajaratnam, S.; et al. Exploring the associations between shift work disorder, depression, anxiety and sick leave taken amongst nurses. J. Sleep Res. 2019, 29, e12872. [Google Scholar] [CrossRef] [PubMed]
- Khan, W.A.; Conduit, R.; Kennedy, G.A.; Jackson, M.L. The relationship between shift-work, sleep, and mental health among paramedics in Australia. Sleep Health 2020, 6, 330–337. [Google Scholar] [CrossRef]
- Kain, J.; Jex, S. Karasek’s (1979) job demands-control model: A summary of current issues and recommendations for future research. In New Developments in Theoretical and Conceptual Approaches to Job Stress; Perrewé, P., Ganster, D., Eds.; Emerald Group Publishing Limited: Bingley, UK, 2010; Volume 8, pp. 237–268. [Google Scholar] [CrossRef]
- Eaton, W.W.; Neufeld, K.; Chen, L.S.; Cai, G. A comparison of self-report and clinical diagnostic interviews for depression: Diagnostic interview schedule and schedules for clinical assessment in neuropsychiatry in the Baltimore epidemiologic catchment area follow-up. Arch. Gen. Psychiatry 2000, 57, 217–222. [Google Scholar] [CrossRef] [Green Version]
- Roberts, N.J.; McAloney-Kocaman, K.; Lippiett, K.; Ray, E.; Welch, L.; Kelly, C. Levels of resilience, anxiety and depression in nurses working in respiratory clinical areas during the COVID pandemic. Respir. Med. 2020, 176, 106219. [Google Scholar] [CrossRef]
- Batterham, P.J.; Calear, A.L.; McCallum, S.M.; Morse, A.R.; Banfield, M.; Farrer, L.M.; Gulliver, A.; Cherbuin, N.; Harris, R.M.R.; Shou, Y.; et al. Trajectories of depression and anxiety symptoms during the COVID-19 pandemic in a representative Australian adult cohort. Med. J. Aust. 2021, 214, 462–468. [Google Scholar] [CrossRef]
- Gasteiger, N.; Vedhara, K.; Massey, A.; Jia, R.; Ayling, K.; Chalder, T.; Coupland, C.; Broadbent, E. Depression, anxiety and stress during the COVID-19 pandemic: Results from a New Zealand cohort study on mental well-being. BMJ Open 2021, 11, e045325. [Google Scholar] [CrossRef]
- Choudhury, T.; Debski, M.; Wiper, A.; Abdelrahman, A.; Wild, S.; Chalil, S.; More, R.; Goode, G.; Patel, B.; Abdelaziz, H.K. COVID-19 Pandemic: Looking After the Mental Health of Our Healthcare Workers. J. Occup. Environ. Med. 2020, 62, e373–e376. [Google Scholar] [CrossRef] [PubMed]
- Hennein, R.; Mew, E.J.; Lowe, S.R. Socio-ecological predictors of mental health outcomes among healthcare workers during the COVID-19 pandemic in the United States. PLoS ONE 2021, 16, e0246602. [Google Scholar] [CrossRef] [PubMed]
- Young, K.P.; Kolcz, D.L.; O’Sullivan, D.M.; Ferrand, J.; Fried, J.; Robinson, K.C. Health Care Workers’ Mental Health and Quality of Life During COVID-19: Results from a Mid-Pandemic, National Survey. Psychiatr. Serv. 2021, 72, 122–128. [Google Scholar] [CrossRef]
- Huffman, E.M.; Athanasiadis, D.I.; Anton, N.E.; Haskett, L.A.; Doster, D.L.; Stefanidis, D.; Lee, N.K. How resilient is your team? Exploring healthcare providers’ well-being during the COVID-19 pandemic. Am. J. Surg. 2020, 221, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Aggar, C.; Samios, C.; Penman, O.; Whiteing, N.; Massey, D.; Rafferty, R.; Bowen, K.; Stephens, A. The impact of COVID-19 pandemic-related stress experienced by Australian nurses. Int. J. Ment. Health Nurs. 2021, 31, 91–103. [Google Scholar] [CrossRef] [PubMed]
- Hammond, N.E.; Crowe, L.; Abbenbroek, B.; Elliott, R.; Tian, D.H.; Donaldson, L.H.; Fitzgerald, E.; Flower, O.; Grattan, S.; Harris, R.; et al. Impact of the coronavirus disease 2019 pandemic on critical care healthcare workers’ depression, anxiety, and stress levels. Aust. Crit. Care 2020, 34, 146–154. [Google Scholar] [CrossRef]
- Holton, S.; Wynter, K.; Trueman, M.; Bruce, S.; Sweeney, S.; Crowe, S.; Dabscheck, A.; Eleftheriou, P.; Booth, S.; Hitch, D.; et al. Psychological well-being of Australian hospital clinical staff during the COVID-19 pandemic. Aust. Health Rev. 2020, 45, 297–305. [Google Scholar] [CrossRef]
- Axisa, C.; Nash, L.; Kelly, P.; Willcock, S. Burnout and distress in Australian physician trainees: Evaluation of a wellbeing workshop. Australas. Psychiatry 2019, 27, 255–261. [Google Scholar] [CrossRef]
- Wu, F.; Ireland, M.; Hafekost, K.; Lawrence, D. National Mental Health Survey of Doctors and Medical Students; Beyond Blue: Melbourne, Australia, 2013; p. 156. [Google Scholar]
- Creedy, D.K.; Sidebotham, M.; Gamble, J.; Pallant, J.; Fenwick, J. Prevalence of burnout, depression, anxiety and stress in Australian midwives: A cross-sectional survey. BMC Pregnancy Childbirth 2017, 17, 13. [Google Scholar] [CrossRef] [Green Version]
- Hegney, D.G.; Craigie, M.; Hemsworth, D.; Osseiran-Moisson, R.; Aoun, S.; Francis, K.; Drury, V. Compassion satisfaction, compassion fatigue, anxiety, depression and stress in registered nurses in Australia: Study 1 results. J. Nurs. Manag. 2013, 22, 506–518. [Google Scholar] [CrossRef]
- Maharaj, S.; Lees, T.; Lal, S. Prevalence and Risk Factors of Depression, Anxiety, and Stress in a Cohort of Australian Nurses. Int. J. Environ. Res. Public Health 2019, 16, 61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGarry, S.; Girdler, S.; McDonald, A.; Valentine, J.; Lee, S.-L.; Blair, E.; Wood, F.; Elliott, C. Paediatric health-care professionals: Relationships between psychological distress, resilience and coping skills. J. Paediatr. Child Health 2013, 49, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Pyper, Z.; Paterson, J.L. Fatigue and mental health in Australian rural and regional ambulance personnel. Emerg. Med. Australas. 2015, 28, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Rossell, S.L.; Neill, E.; Phillipou, A.; Tan, E.J.; Toh, W.L.; Van Rheenen, T.E.; Meyer, D. An overview of current mental health in the general population of Australia during the COVID-19 pandemic: Results from the COLLATE project. Psychiatry Res. 2020, 296, 113660. [Google Scholar] [CrossRef] [PubMed]
- Stanton, R.; To, Q.G.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. Depression, Anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in australian adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef]
- Sanghera, J.; Pattani, N.; Hashmi, Y.; Varley, K.F.; Cheruvu, M.S.; Bradley, A.; Burke, J.R. The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting—A Systematic Review. J. Occup. Health 2020, 62, e12175. [Google Scholar] [CrossRef] [PubMed]
- Serrano-Ripoll, M.J.; Meneses-Echavez, J.F.; Ricci-Cabello, I.; Fraile-Navarro, D.; Fiol-deRoque, M.A.; Pastor-Moreno, G.; Gonçalves-Bradley, D.C. Impact of viral epidemic outbreaks on mental health of healthcare workers: A rapid systematic review and meta-analysis. J. Affect. Disord. 2020, 277, 347–357. [Google Scholar] [CrossRef]
- Tran, T.D.; Hammarberg, K.; Kirkman, M.; Nguyen, H.T.M.; Fisher, J. Alcohol use and mental health status during the first months of COVID-19 pandemic in Australia. J. Affect. Disord. 2020, 277, 810–813. [Google Scholar] [CrossRef]
- Rahman, M.A.; Hoque, N.; Alif, S.M.; Salehin, M.; Islam, S.M.S.; Banik, B.; Sharif, A.; Nazim, N.B.; Sultana, F.; Cross, W. Factors associated with psychological distress, fear and coping strategies during the COVID-19 pandemic in Australia. Glob. Health 2020, 16, 95. [Google Scholar] [CrossRef]
- Bhoyroo, R.; Chivers, P.; Millar, L.; Bulsara, C.; Piggott, B.; Lambert, M.; Codde, J. Life in a time of COVID: A mixed method study of the changes in lifestyle, mental and psychosocial health during and after lockdown in Western Australians. BMC Public Health 2021, 21, 1947. [Google Scholar] [CrossRef]
| Characteristics | Total Cohort n (%) | Occupational Group | ||||
|---|---|---|---|---|---|---|
| Paramedics n (%) | Nurses n (%) | Allied Health ^ n (%) | Doctors n (%) | Others * n (%) | ||
| Overall | 984 (100.0%) | 126 (12.8%) | 319 (32.4%) | 174 (17.7%) | 123 (12.5%) | 242 (24.6%) |
| Gender | ||||||
| Male | 267 (27.1%) | 70 (55.6%) | 37 (11.6%) | 28 (16.1%) | 66 (53.7%) | 66 (27.3%) |
| Female | 714 (72.6%) | 55 (43.7%) | 282 (88.4%) | 145 (83.3%) | 57 (46.3%) | 175 (72.3%) |
| Non-binary | 3 (0.3%) | 1 (0.8%) | 0 (0.0%) | 1 (0.6%) | 0 (0.0%) | 1 (0.4%) |
| Age | ||||||
| <45 years | 499 (50.7%) | 83 (65.9%) | 151 (47.3%) | 98 (56.3%) | 62 (50.4%) | 105 (43.4%) |
| ≥45 years | 485 (49.3%) | 43 (34.1%) | 168 (52.7%) | 76 (43.7%) | 61 (49.6%) | 137 (56.6%) |
| Work setting | ||||||
| Hospital | 808 (82.1%) | 0 (0.0%) | 309 (96.9%) | 168 (96.6%) | 112 (91.1%) | 219 (90.5%) |
| Ambulance | 141 (14.3%) | 126 (100.0%) | 2 (0.6%) | 2 (1.1%) | 0 (0.0%) | 11 (4.5%) |
| Aged care | 7 (0.7%) | 0 (0.0%) | 1 (0.3%) | 3 (1.7%) | 0 (0.0%) | 3 (1.2%) |
| Primary care | 28 (2.8%) | 0 (0.0%) | 7 (2.2%) | 1 (0.6%) | 11 (8.9%) | 9 (3.7%) |
| COVID Infection Status (n = 983) | ||||||
| COVID-19 Infected | 22 (2.2%) | 2 (1.6%) | 11 (3.4%) | 1 (0.6%) | 1 (0.8%) | 7 (2.9%) |
| Furloughed but not infected | 203 (20.7%) | 47 (37.3%) | 79 (24.8%) | 33 (19.0%) | 15 (12.2%) | 29 (12.0%) |
| Neither infected nor furloughed | 758 (77.1%) | 77 (61.1%) | 229 (71.8%) | 140 (80.5%) | 107 (87.0%) | 205 (85.1%) |
| Work Experience | ||||||
| ≤10 years | 386 (39.2%) | 66 (52.4%) | 101 (31.7%) | 64 (36.8%) | 32 (26.0%) | 123 (50.8%) |
| >10 years | 598 (60.8%) | 60 (47.6%) | 218 (68.3%) | 110 (63.2%) | 91 (74.0%) | 119 (49.2%) |
| Validated Scales | Total Cohort n (%) | Paramedics n (%) | Nurses n (%) | Allied Health n (%) | Doctors n (%) | Others n (%) |
|---|---|---|---|---|---|---|
| Overall | 984 (100%) | 126 (12.8%) | 319 (32.4%) | 174 (17.7%) | 123 (12.5%) | 242 (24.6%) |
| Patient Health Questionnaire-9 (PHQ-9)—Depression | ||||||
| Mean (SD) | 6.0 (5.4) | 7.3 (5.5) | 6.9 (5.8) | 5.0 (4.8) | 4.3 (4.1) | 6.0 (5.4) |
| ≥10 (Moderate-Severe) | 221 (22.5%) | 40 (31.7%) | 81 (25.4%) | 27 (15.5%) | 15 (12.2%) | 58 (24.0%) |
| <10 (Minimal-Mild) | 763 (77.5%) | 86 (68.3%) | 238 (74.6%) | 147 (84.5%) | 108 (87.8%) | 184 (76.0%) |
| PHQ item 9 (thoughts of being better off dead or self-harm) | ||||||
| Several days or more frequently | 87 (8.8%) | 12 (9.5%) | 39 (12.2%) | 10 (5.7%) | 7 (5.7%) | 19 (7.9%) |
| Not at all | 897 (91.2%) | 114 (90.5%) | 280 (87.8%) | 164 (94.3%) | 116 (94.38%) | 223 (92.1%) |
| Generalised Anxiety Disorder 7-item scale (GAD-7)—Anxiety | ||||||
| Mean (SD) | 4.6 (4.7) | 5.1 (4.6) | 5.1 (4.9) | 3.9 (4.5) | 3.2 (3.7) | 4.8 (4.8) |
| ≥10 (Moderate-Severe) | 138 (14.0%) | 21 (16.7%) | 54 (16.9%) | 15 (8.6%) | 10 (8.1%) | 38 (15.7%) |
| <10 (Minimal-Mild) | 846 (86.0%) | 105 (83.3%) | 265 (83.1%) | 159 (91.4%) | 113 (91.9%) | 204 (84.3%) |
| GAD-7 item 6 (becoming easily annoyed or irritable) | ||||||
| Several days or more frequently | 599 (60.9%) | 86 (68.3%) | 210 (65.82%) | 89(51.1%) | 71 (57.7%) | 143 (59.1%) |
| Not at all | 385 (39.1%) | 40 (31.7%) | 109 (34.2%) | 85 (48.9%) | 52 (42.3%) | 99 (40.9%) |
| Impact of Event Scale-6 (IES-6)—Post-traumatic stress disorder (PTSD) | ||||||
| Mean (SD) * | 0.9 (0.8) | 1.1 (0.9) | 1.0 (0.9) | 0.8 (0.7) | 0.7 (0.7) | 1.0 (0.9) |
| >9 (Moderate-Severe) # | 201 (20.4%) | 32 (25.4%) | 80 (25.1%) | 21 (12.1%) | 12 (9.8%) | 56 (23.1%) |
| ≤9 (None/Minimal) # | 783 (79.6%) | 94 (74.6%) | 239 (74.9%) | 153 (87.9%) | 111 (90.2%) | 186 (76.9%) |
| Connor-Davidson Resilience Scale 2-item (CD-RISC-2)—Resilience | ||||||
| Mean (SD) | 6.3 (1.4) | 6.3 (1.4) | 6.2 (1.3) | 6.3 (1.4) | 6.4 (1.4) | 6.3 (1.3) |
| Personal wellbeing index-Adult (PWI-A)—Wellbeing | ||||||
| PWI-A (Well-being)—Mean (SD) | 69.7 (17.3) | 67.5 (17.3) | 67.6 (18.4) | 72.8 (14.6) | 76.2 (13.9) | 68.3 (17.9) |
| PWI Item 1 (Life Satisfaction)—Mean (SD) | 68.9 (18.9) | 66.8 (19.0) | 66.5 (20.4) | 71.3 (15.8) | 75.1 (14.9) | 68.1 (19.9) |
| Abbreviated Maslach Burnout Inventory (aMBI)—Burnout | ||||||
| Emotional Exhaustion (n = 941) | ||||||
| Mean (SD) | 8.7 (4.7) | 9.5 (4.9) | 9.6 (4.7) | 8.4 (4.5) | 7.7 (4.2) | 7.8 (5.0) |
| ≥7 (Moderate-Severe burnout) | 613 (65.1%) | 85 (68.5%) | 223 (71.7%) | 109 (64.5%) | 74 (60.7%) | 122 (56.7%) |
| <7 (No-Low burnout) | 328 (34.9%) | 39 (31.5%) | 88 (28.3%) | 60 (35.5%) | 48 (39.3%) | 93 (43.3%) |
| Depersonalization (n = 803) | ||||||
| Mean (SD) | 3.0 (3.9) | 5.9 (4.8) | 2.9 (3.7) | 2.2 (3.0) | 2.5 (3.2) | 2.1 (3.6) |
| ≥4 (Moderate-Severe burnout) | 252 (31.4%) | 71 (60.7%) | 95 (32.1%) | 36 (22.9%) | 29 (24.4%) | 21 (18.4%) |
| <4 (No-Low burnout) | 551 (68.6%) | 46 (39.3%) | 201 (67.9%) | 121 (77.1%) | 90 (75.6%) | 93 (81.6%) |
| Personal Accomplishment (n = 772) | ||||||
| Mean (SD) | 14.3 (2.9) | 13.2 (3.3) | 14.4 (2.9) | 14.7 (2.6) | 14.6 (2.8) | 14.3 (3.0) |
| ≤14 (Moderate-Severe burnout) | 348 (45.1%) | 74 (61.2%) | 133 (45.9%) | 55 (36.9%) | 45 (38.1%) | 41 (43.6%) |
| >14 (No-Low burnout) | 424 (54.9%) | 47 (38.8%) | 157 (54.1%) | 94 (63.1%) | 73 (61.9%) | 53 (56.4%) |
| Optimism | ||||||
| Mean (SD) | 7.0 (1.9) | 6.9 (2.0) | 6.9 (1.9) | 7.2 (1.6) | 7.3 (1.9) | 7.1 (1.9) |
| <8 Low-moderate optimism) | 655 (66.6%) | 86 (68.3%) | 225 (70.5%) | 114 (65.5%) | 68 (55.3%) | 162 (66.9%) |
| ≥8 High optimism | 329 (33.4%) | 40 (31.7%) | 94 (29.5%) | 60 (34.5%) | 55 (44.7%) | 80 (33.1%) |
| Validated Scales | Nurses vs. Paramedics Mean Difference (95% CI) | Allied Health vs. Paramedics Mean Difference (95% CI) | Doctors vs. Paramedics Mean Difference (95% CI) | Others vs. Paramedics Mean Difference (95% CI) | p-Value | Nurses vs. Paramedics Mean Difference (95% CI) | Allied Health vs. Paramedics Mean Difference (95% CI) | Doctors vs. Paramedics Mean Difference (95% CI) | Others vs. Paramedics Mean Difference (95% CI) | p-Value ** |
|---|---|---|---|---|---|---|---|---|---|---|
| Comparison of Continuous Outcomes | Comparison of Binary Outcomes | |||||||||
| PHQ-9—Depression | 0.5 (−0.7, 1.7) | −1.3 (−2.6, 0.0) | −1.8 (−3.3, −0.4) | −0.3 (−1.5, 0.9) | <0.001 | 1.16 (0.81, 1.65) | 0.71 (0.45, 1.12) | 0.57 (0.33, 1.00) | 1.05 (0.73, 1.51) | 0.024 |
| GAD-7—Anxiety | 0.8 (−0.3, 1.8) | −0.4 (−1.5, 0.7) | −0.8 (−2.1, 0.4) | 0.6 (−0.5, 1.6) | 0.006 | 1.40 (0.85, 2.30) | 0.72 (0.37, 1.39) | 0.76 (0.36, 1.60) | 1.30 (0.78, 2.18) | 0.070 |
| IES-6 Post-traumatic stress | 0.1 (−0.2, 0.3) | −0.1 (−0.4, 0.1) | −0.2 (−0.4, 0.0) | 0.1 (−0.2, 0.3) | 0.004 | 1.15 (0.78, 1.70) | 0.55 (0.33, 0.93) | 0.47 (0.25, 0.88) | 1.08 (0.72, 1.61) | 0.001 |
| CD-RISC-2—Resilience | −0.1 (−0.8, 0.5) | −0.0 (−0.7, 0.6) | 0.1 (−0.6, 0.8) | −0.0 (−0.7, 0.6) | 0.65 | N/A | N/A | N/A | N/A | N/A |
| PWI-A—Wellbeing | ||||||||||
| PWI-A (Well-being) | −2.1 (−7.4, 3.3) | 2.6 (−2.9, 8.2) | 6.9 (1.3, 12.6) | −0.9 (−6.2, 4.3) | <0.001 | N/A | N/A | N/A | N/A | N/A |
| PWI Item 1 (Life Satisfaction) | −1.7 (−9.2, 5.9) | 2.7 (−4.9, 10.3) | 7.4 (−0.3, 15.1) | 0.1 (−7.2, 7.4) | <0.001 | N/A | N/A | N/A | N/A | N/A |
| aMBI—Burnout | ||||||||||
| Emotional Exhaustion | 0.6 (−1.2, 2.3) | −0.7 (−2.3, 0.9) | −1.2 (−2.8, 0.5) | −1.1 (−2.6, 0.5) | <0.001 | 1.14 (0.99, 1.32) | 0.99 (0.84, 1.17) | 0.96 (0.80, 1.15) | 0.90 (0.76, 1.06) | 0.002 |
| Depersonalization | −2.3 (−3.5, −1.1) | −3.2 (−4.4, −1.9) | −3.1 (−4.3, −1.8) | −3.1 (−4.3, −1.9) | <0.001 | 0.56 (0.31, 1.04) | 0.39 (0.22, 0.69) | 0.43 (0.24, 0.77) | 0.34 (0.19, 0.60) | 0.003 a |
| Personal Accomplishment | 0.9 (−0.3, 2.0) | 1.4 (0.3, 2.5) | 1.3 (0.2, 2.4) | 0.8 (−0.2, 1.9) | 0.017 | 0.86 (0.52, 1.42) | 0.67 (0.41, 1.10) | 0.67 (0.41, 1.09) | 0.81 (0.52, 1.26) | 0.15 b |
| Optimism | −2.5 (−9.2, 4.3) | 1.2 (−5.5, 8.0) | 4.0 (−2.7, 10.8) | 0.6 (−5.9, 7.1) | 0.029 | 1.06 (0.82, 1.36) | 0.97 (0.78, 1.22) | 0.83 (0.65, 1.05) | 1.01 (0.81, 1.26) | 0.16 a |
| Themes and Subthemes # | Illustrative Quote (Occupational Group, Healthcare Setting) |
|---|---|
Working in a complex and changing environment
| “Working through COVID in healthcare has been incredibly stressful and draining, we’re nowhere near finished, and most of us are trying to pour from empty cups.” (Allied health worker, hospital) “In a role that is very time poor, it was and remains a constant battle to ensure we are up to date with the latest protocols, knowledge, risks and assessments about Covid.” (Nurse, hospital) “I have never worked so hard in my entire career. I feel mentally and physically drained after work and it takes all of my days off to recuperate then I am back at work being brought down again.” (Paramedic, ambulance) |
Concerns about patient/resident care
| “The impact of isolation on residents was heartbreaking and resulted in significant deconditioning which we are only seeing now.” (Nurse, hospital) “As a social worker we are working with the shadow pandemic of family violence and mental illness to a degree we have never seen before. This will go on for years to come–trying to pick up the pieces.” (Allied health, hospital) |
Isolation and disconnection
| “My fear of passing something on, as well as the sadness of limiting my contact [with family] out of those fears has had a significant negative impact on my general wellbeing and family closeness.” (Paramedic, ambulance) “I found the whole experience frightening—I can only speak for myself but I was living in fear every day of getting COVID or giving it to someone.” (Nurse, hospital) |
Positive experiences
| “I did feel a sense of pride about the way our team rose to the challenge and provided such empathetic and respectful care in such a challenging time.” (Nurse, hospital) “The experience with Covid-19 made me perceive the world differently. I no longer want to keep working extra hours and decided to work 4 days a week. I decided to spend time on myself and surrounding people more than pre-covid.” (Nurse, aged-care) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McGuinness, S.L.; Johnson, J.; Eades, O.; Cameron, P.A.; Forbes, A.; Fisher, J.; Grantham, K.; Hodgson, C.; Hunter, P.; Kasza, J.; et al. Mental Health Outcomes in Australian Healthcare and Aged-Care Workers during the Second Year of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 4951. https://doi.org/10.3390/ijerph19094951
McGuinness SL, Johnson J, Eades O, Cameron PA, Forbes A, Fisher J, Grantham K, Hodgson C, Hunter P, Kasza J, et al. Mental Health Outcomes in Australian Healthcare and Aged-Care Workers during the Second Year of the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2022; 19(9):4951. https://doi.org/10.3390/ijerph19094951
Chicago/Turabian StyleMcGuinness, Sarah L., Josphin Johnson, Owen Eades, Peter A. Cameron, Andrew Forbes, Jane Fisher, Kelsey Grantham, Carol Hodgson, Peter Hunter, Jessica Kasza, and et al. 2022. "Mental Health Outcomes in Australian Healthcare and Aged-Care Workers during the Second Year of the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 19, no. 9: 4951. https://doi.org/10.3390/ijerph19094951
APA StyleMcGuinness, S. L., Johnson, J., Eades, O., Cameron, P. A., Forbes, A., Fisher, J., Grantham, K., Hodgson, C., Hunter, P., Kasza, J., Kelsall, H. L., Kirkman, M., Russell, G., Russo, P. L., Sim, M. R., Singh, K. P., Skouteris, H., Smith, K. L., Stuart, R. L., ... Leder, K. (2022). Mental Health Outcomes in Australian Healthcare and Aged-Care Workers during the Second Year of the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 19(9), 4951. https://doi.org/10.3390/ijerph19094951







