Oral Health Service Access in Racial/Ethnic Minority Neighborhoods: A Geospatial Analysis in Washington, DC, USA
Abstract
:1. Introduction
2. The Setting: Washington, DC
3. Methods
3.1. Data and Measures
3.2. Methods of Analysis
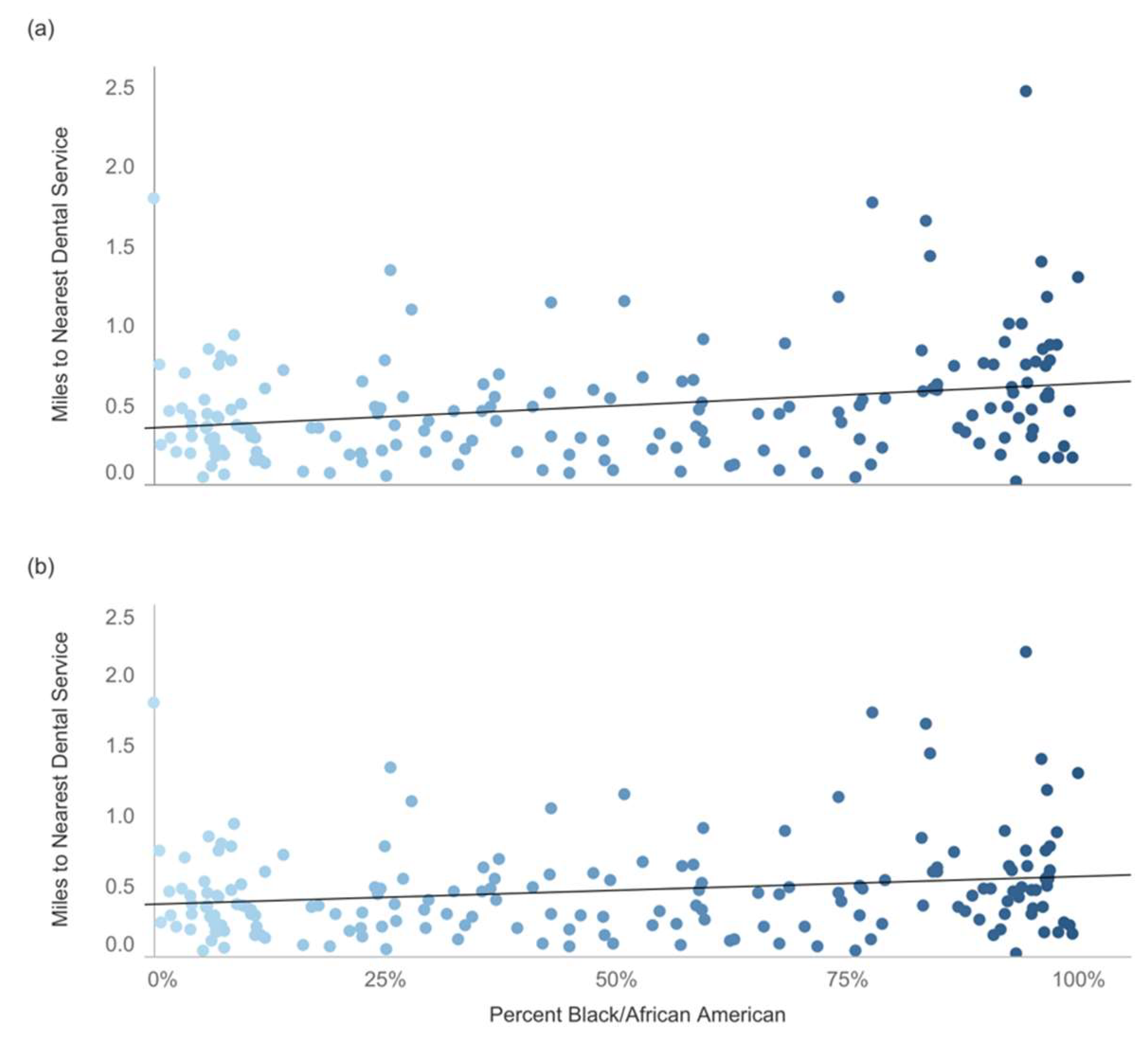
4. Results
5. Discussion
6. Implications
7. Limitations
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chi, D.L.; Carpiano, R.M. Neighborhood social capital, neighborhood attachment, and dental care use for Los Angeles family and neighborhood survey adults. Am. J. Public Health 2013, 103, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.C.; Li, C.Y.; Serag, H.; Tabrizi, M.; Kuo, Y.-F. Exploring the impact of ACA on rural-urban disparity in oral health services among US noninstitutionalized adults. J. Rural Health 2020, 37, 103–113. [Google Scholar] [CrossRef] [PubMed]
- FDI World Dental Federation. Oral Health Worldwide: A Report by FDI World Dental Federation. Available online: https://www.fdiworlddental.org/sites/default/files/2020-11/2015_wohd-whitepaper-oral_health_worldwide.pdf (accessed on 4 February 2022).
- Lee, J.S.; Somerman, M.J. The importance of oral health in comprehensive health care. JAMA 2018, 320, 339–340. [Google Scholar] [CrossRef] [PubMed]
- National Advisory Committee on Rural Health and Human Services. Improving Oral Health Care Services in Rural America. Available online: https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/rural/publications/2018-Oral-Health-Policy-Brief.pdf (accessed on 1 February 2019).
- Nazir, M.A. Prevalence of periodontal disease, its association with systemic diseases and prevention. Int. J. Health Sci. 2017, 11, 72–80. [Google Scholar]
- Dave, M.; Barry, S.; Coulthard, P.; Daniels, R.; Greenwood, M.; Seoudi, N.; Walton, G.; Patel, N. An evaluation of sepsis in dentistry. Br. Dent. J. 2021, 8, 32–39. [Google Scholar] [CrossRef]
- Hung, M.; Moffat, R.; Gill, G.; Lauren, E.; Ruiz-Negrón, B.; Rosales, M.N.; Richey, J.; Licari, F.W. Oral health as a gateway to overall health and well-being: Surveillance of the geriatric population in the United States. Spec. Care Dent. 2019, 39, 354–361. [Google Scholar] [CrossRef]
- Institute of Medicine. The U.S. Oral Health Workforce in the Coming Decade: Workshop Summary; The National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Lee, J.Y.; Divaris, K. The ethical imperative of addressing oral health disparities: A unifying framework. J. Dent. Res. 2014, 93, 224–230. [Google Scholar] [CrossRef] [Green Version]
- Chattopadhyay, A. Oral health disparities in the United States. Dent. Clin. N. Am. 2008, 52, 297–318. [Google Scholar] [CrossRef]
- Patrick, D.L.; Lee, R.S.Y.; Nucci, M.; Grembowski, D.; Jolles, C.Z.; Milgrom, P. Reducing oral health disparities: A focus on social and cultural determinants. BMC Oral Health 2006, 6, S4. [Google Scholar] [CrossRef]
- Henshaw, M.M.; Garcia, R.I.; Weintraub, J.A. Oral health disparities across the life span. Dent. Clin. N. Am. 2018, 62, 177–193. [Google Scholar] [CrossRef]
- Northridge, M.E. Oral health equity for minority populations in the United States. Oxf. Bibliogr. Public Health 2018, 1–17. [Google Scholar] [CrossRef]
- Bastos, J.L.; Celeste, R.K.; Paradies, Y.C. Racial inequalities in oral health. J. Dent. Res. 2018, 97, 878–886. [Google Scholar] [CrossRef] [PubMed]
- Akintobi, T.H.; Hoffman, L.M.; McAllister, C.; Goodin, L.; Hernandez, N.D.; Rollins, L.; Miller, A. Assessing the oral health needs of African American men in low-income, urban communities. Am. J. Men’s Health 2018, 12, 326–337. [Google Scholar] [CrossRef] [PubMed]
- Koppelman, J.; Cohen, R.S. Dental Health Is Worse in Communities of Color: Four Key Disparities Show How These Populations Are Vulnerable. Available online: https://www.pewtrusts.org/en/research-and-analysis/articles/2016/05/12/dental-health-is-worse-in-communities-of-color (accessed on 4 February 2022).
- Dye, B.A.; Thorton-Evans, G.; Li, X.; Iafolla, T.J. Dental Caries and Sealant Prevalence in Children and Adolescents in the United States, 2011–2012. Available online: https://www.cdc.gov/nchs/data/databriefs/db191.pdf (accessed on 16 March 2022).
- Osazuwa-Peters, N.; Massa, S.T.; Christopher, K.M.; Walker, R.J.; Varvares, M.A. Race and sex disparities in long-term survival of oral and oropharyngeal cancer in the United States. J. Cancer Res. Clin. Oncol. 2016, 142, 521–528. [Google Scholar] [CrossRef]
- Wiener, R.C.; Sambamoorthi, U.; Shen, C.; Alwhaibi, M.; Findley, P. Food security and unmet dental care needs in adults in the United States. J. Dent. Hyg. 2018, 92, 14–22. [Google Scholar]
- Haider, A.D.; Schneider, E.B.; Sriram, N. Unconscious race and social class bias among acute care surgical clinicians and clinical treatment decisions. JAMA Surg. 2015, 150, 457–464. [Google Scholar] [CrossRef]
- Patel, N.; Patel, S.; Cotti, E.; Bardini, G.; Mannocci, F. Unconscious racial bias may affect dentists’ clinical decisions on tooth restorability: A randomized clinical trial. JDR Clin. Transl. Res. 2019, 4, 19–28. [Google Scholar] [CrossRef]
- Arcury, T.A.; Chen, H.; Savoca, M.R.; Anderson, A.M.; Leng, X.; Bell, R.A.; Quandt, S.A. Ethnic variation in oral health and social integration among older rural adults. J Appl. Gerontol. 2011, 32, 302–323. [Google Scholar] [CrossRef] [Green Version]
- Saman, D.M.; Johnson, A.O.; Arevalo, O.; Odoi, A. Student column: Geospatially illustrating regional-based oral health disparities in Kentucky. Public Health Rep. 2011, 126, 612–618. [Google Scholar] [CrossRef] [Green Version]
- Kurcz, R.; Kruger, E.; Tennant, M. Using GIS to analyze dental practice distribution in Indiana, USA. Community Dent. Health 2013, 30, 155–160. [Google Scholar]
- Brown, T.T.; Finlayson, T.L.; Fulton, B.D.; Jahedi, S. The demand for dental care and financial barriers in accessing care among adults in California. J. Calif. Dent. Assoc. 2009, 37, 539–547. [Google Scholar] [PubMed]
- Yoon, H.; Jang, Y.; Choi, K.; Kim, H. Preventive dental care utilization in Asian Americans in Austin, Texas: Does neighborhood matter? Int. J. Environ. Res. Public Health 2018, 15, 2261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Learning Life. DC Rich and Poor: A Tale of Two Wards. Available online: http://learninglife.info/wards3and8/ (accessed on 4 February 2022).
- Reilly, M. DC’s Ward 7 and 8 Residents “Grocery Walk” to Draw Attention to Lack of Food Access. Available online: https://ggwash.org/view/65095/washington-dc-ward-7-and-8-residents-stage-grocery-walk-to-draw-attention-to-lack-of-food-access (accessed on 4 February 2022).
- Homan, T.R. Unemployment Rate in Washington’s Ward 8 is Highest in U.S. Available online: https://www.dchealthmatters.org/demographicdata?id=131495§ionId=939 (accessed on 28 April 2018).
- Neighborhood Info DC. Neighborhood Profiles: 2012 Council Wards. Available online: https://www.neighborhoodinfodc.org/profiles.html (accessed on 16 August 2018).
- Davis, J.; Liu, M.; Kao, D.; Gu, X.; Cherry-Peppers, G. Using GIS to analyze inequality in access to dental care in the District of Columbia. AMA J. Ethics 2022, 24, 41–47. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. Developmental research, public policy, and the ecology of childhood. Child Dev. 1974, 45, 1–5. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. The Ecology of Human Development: Experiments by Nature and Design; Harvard University Press: Cambridge, MA, USA, 1979; ISBN 0-674-22457-4. [Google Scholar]
- U.S. Census Bureau. Tiger/Line Shapefiles. Available online: https://www.census.gov/geographies/mapping-files/time-series/geo/tiger-line-file.2018.html (accessed on 3 August 2020).
- U.S. Census Bureau. American Community Survey (acs). Available online: https://www.census.gov/programs-surveys/acs (accessed on 13 August 2020).
- Centers for Medicare & Medicaid Services. Federally Qualified Health Center. Available online: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/fqhcfactsheet.pdf (accessed on 4 February 2022).
- Open Data DC. Wards from 2012 [Data Set]. Available online: https://opendata.dc.gov/datasets/DCGIS::wards-from-2012/about (accessed on 4 February 2022).
- QGIS. QGIS (Version 3.24.0). 2022. Available online: https://www.qgis.org (accessed on 28 April 2021).
- Anselin, L. Spatial Econometrics. In A Companion to Theoretical Econometrics; Baltagi, B.H., Ed.; Blackwell Publishing Ltd.: Malden, MA, USA, 2003; pp. 310–330. ISBN 0-631-21254-X. [Google Scholar]
- DC Health. Oral Health: District of Columbia Behavioral Risk Factor Surveillance System [Infographic]. Available online: https://dchealth.dc.gov/sites/default/files/dc/sites/doh/service_content/attachments/Oral%20Health%20Infographic.pdf (accessed on 5 February 2022).
- DC Office of Planning. Plans & Initiatives. Available online: https://planning.dc.gov/page/about-ward-8 (accessed on 4 February 2022).
- Jäger, R.; van den Berg, N.; Schwendicke, F. Interventions for enhancing the distribution of dental professionals: A concise systematic review. Int. Dent. J. 2017, 67, 263–271. [Google Scholar] [CrossRef] [Green Version]
- Stapleton, S.; Finlayson, T.L.; Ohmit, A.; Hunte, H.E. Correlates of past year dental health visits: Findings from the Indiana black men’s health study. J. Public Health Dent. 2016, 76, 157–165. [Google Scholar] [CrossRef]
- Hoffman, L.M.; Rollins, L.; Henry Akintobi, T.; Erwin, K.; Lewis, K.; Hernandez, N.; Miller, A. Oral health intervention for low-income African American men in Atlanta, Georgia. Am. J. Public Health 2017, 107, S104–S110. [Google Scholar] [CrossRef]
- Jones, E.; Shi, L.; Hayashi, A.S.; Sharma, R.; Daly, C.; Ngo-Metzger, Q. Access to oral health care: The role of federally qualified health centers in addressing disparities and expanding access. Am. J. Public Health 2013, 103, 488–493. [Google Scholar] [CrossRef]
- Northridge, M.E.; Kumar, A.; Kaur, R. Disparities in access to oral health care. Annu. Rev. Public Health 2020, 41, 513–535. [Google Scholar] [CrossRef] [Green Version]
- Langelier, M.; Moore, J.; Baker, B.K.; Mertz, E. Case Studies of 8 Federally Qualified Health Centers: Strategies to Integrate Oral Health with Primary Care. Oral Health Workforce Research Center. Available online: http://www.oralhealthworkforce.org/wp-content/uploads/2015/11/FQHC-Case-Studies-2015.pdf (accessed on 18 March 2022).
- Baskaradoss, J.K. Relationship between oral health literacy and oral health status. BMC Oral Health 2018, 18, 172. [Google Scholar] [CrossRef]
- Como, D.H.; Stein Duker, L.I.; Polido, J.C.; Cermak, S.A. The persistence of oral health disparities for african american children: A scoping review. Int. J. Environ. Res. Public Health 2019, 16, 710. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Healthy People. Available online: https://www.healthypeople.gov/2020/topics-objectives/topic/oral-health (accessed on 26 March 2022).
- Dragojevic, M.; Savage, M.W.; Scott, A.M.; McGinnis, T. Promoting oral health in Appalachia: Effects of threat label and source accent on message acceptance. Health Commun. 2018, 35, 297–307. [Google Scholar] [CrossRef]
- Ramji, R.; Carlson, E.; Brogårdh-Roth, S.; Olofsson, A.N.; Kottorp, A.; Rämgård, M. Understanding behavioral changes through community-based participatory research to promote oral health in socially disadvantaged neighborhoods in Southern Sweden. BMJ Open 2020, 10, e035732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Modha, B. Utilising dentist-dental health educator skill-mix to implement oral health promotion that better supports diverse communities. J. Integr. Care 2022. ahead of print. [Google Scholar] [CrossRef]
- Cornelius, M.E.; Loretan, C.G.; Wang, T.W.; Jamal, A.; Homa, D.M. Tobacco product use among adults—United States, 2020. Morb. Mortal. Wkly. Rep. 2022, 71, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Ford, P.J.; Rich, A.M. Tobacco use and oral health. Addiction 2021, 116, 3531–3540. [Google Scholar] [CrossRef]


| Wards | Dentists | % | FQHCs | % | % African American | % Families in Poverty |
|---|---|---|---|---|---|---|
| All | 755 | 100.0 | 26 | 100.0 | 43.9 | 12.1 |
| 1 | 74 | 9.8 | 3 | 11.5 | 21.2 | 11.9 |
| 2 | 261 | 34.6 | 1 | 3.8 | 13.2 | 5.9 |
| 3 | 147 | 19.5 | 0 | 0.0 | 5.3 | 2.3 |
| 4 | 97 | 12.8 | 1 | 3.8 | 45.9 | 6.8 |
| 5 | 36 | 4.8 | 4 | 15.4 | 55.4 | 7.7 |
| 6 | 82 | 10.9 | 2 | 7.7 | 38.8 | 7.9 |
| 7 | 27 | 3.6 | 7 | 26.9 | 91.7 | 23.3 |
| 8 | 31 | 4.1 | 8 | 30.8 | 91.8 | 26.6 |
| Characteristics | Dental Offices | Dental Offices + FQHCs |
|---|---|---|
| Percent African American | 0.26 *** | 0.19 ** |
| Percent Hispanic | −0.30 *** | −0.30 *** |
| Percent Male | 0.11 | 0.11 * |
| Percent Poverty | 0.17 * | 0.17 |
| Median Age | −0.18 * | −0.18 |
| Dental Offices | Dental Offices + FQHCs | |||
|---|---|---|---|---|
| Characteristics | OLS | Spatial Lag | OLS | Spatial Lag |
| Percent African American | 0.32 ** | 0.28 ** | 0.25 * | 0.23 * |
| Percent Hispanic | −1.08 ** | −0.61 * | −0.98 ** | −0.53 |
| Percent Male | 1.36 ** | 1.46 *** | 1.50 ** | 1.54 *** |
| Percent Poverty | −0.37 | −0.43 | −0.33 | −0.36 |
| Median Age | −0.01 * | −0.01 ** | −0.01 * | −0.01 * |
| Spatial Lag | - | 0.46 *** | 0.47 *** | |
| Constant | 0.24 | −0.04 | 0.11 | −0.14 |
| R-squared | 0.19 | 0.30 | 0.16 | 0.29 |
| AIC | 123.8 | 105.7 | 111.7 | 91.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, M.; Kao, D.; Gu, X.; Holland, W.; Cherry-Peppers, G. Oral Health Service Access in Racial/Ethnic Minority Neighborhoods: A Geospatial Analysis in Washington, DC, USA. Int. J. Environ. Res. Public Health 2022, 19, 4988. https://doi.org/10.3390/ijerph19094988
Liu M, Kao D, Gu X, Holland W, Cherry-Peppers G. Oral Health Service Access in Racial/Ethnic Minority Neighborhoods: A Geospatial Analysis in Washington, DC, USA. International Journal of Environmental Research and Public Health. 2022; 19(9):4988. https://doi.org/10.3390/ijerph19094988
Chicago/Turabian StyleLiu, Meirong, Dennis Kao, Xinbin Gu, Whittni Holland, and Gail Cherry-Peppers. 2022. "Oral Health Service Access in Racial/Ethnic Minority Neighborhoods: A Geospatial Analysis in Washington, DC, USA" International Journal of Environmental Research and Public Health 19, no. 9: 4988. https://doi.org/10.3390/ijerph19094988






