Abstract
Quality improvement plays a major role in healthcare, and numerous approaches have been developed to implement changes. However, the reasons for success or failure of the methods applied often remains obscure. Normalization process theory, recently developed in sociology, provides a flexible framework upon which to construct quality improvement. We sought to determine if examination of a successful quality improvement project, using normalization process theory and social marketing, provided insight into implementation. We performed a retrospective analysis of the steps taken to implement a pain management program in an electrophysiology clinic. We mapped these steps, and the corresponding social marketing tools used, to elements of normalization process theory. The combination of mapping implementation steps and marketing approaches to the theory provided insight into the quality-improvement process. Specifically, examination of the steps in the context of normalization process theory highlighted barriers to implementation at individual, group, and organizational levels. Importantly, the mapping also highlighted how facilitators were able to overcome the barriers with marketing techniques. Furthermore, integration with social marketing revealed how promotion of tangibility of benefits aided communication and how process co-creation between stakeholders enhanced value. Our implementation of a pain-management program was successful in a challenging environment composed of several stakeholder groups with entrenched initial positions. Therefore, we propose that the behavior change elements of normalization process theory combined with social marketing provide a flexible framework to initiate quality improvement.
1. Introduction
Pain is disabling and often adds to costs [1]. Consequently, pain management has attracted attention [2,3]. One focus has been on assessment of pain-management programs [4]. For example, examination of pain-management guidelines for healthcare workers [5] and communication with patients about pain management after cardiac surgery [6].
Many procedures in cardiac electrophysiology are minimally invasive, and therefore post-interventional pain management programs appear unnecessary [7,8]. Nevertheless, even minor, minimally invasive interventions, such as percutaneous cardiac ablation for atrial fibrillation, followed by bed rest can result in back pain. Similarly, implantation of pacemakers or defibrillation devices through skin incisions can produce high post-interventional pain levels [7,9]. Moreover, the number of such interventions is increasing [10]. Therefore, pain management has value for patients. In turn, patient welfare is crucial to hospital reputation and economic wellbeing. Pain management also has value for hospital staff.
We implemented a post-interventional pain management program in cardiac electrophysiology that achieved positive results; the proportion of patients who experienced moderate-to-severe pain decreased from 61% before the program to 47% after (p < 0.05) [8]. However, the barriers faced by project leaders, the group dynamics navigated, and steps along the road to the program’s implementation were not described. Therefore, the current paper aims to describe the process. Because pain-management program initiation represents a behavioral change intervention, and because such changes are difficult to accomplish, it is important to provide guidance to assist others in implementation of similar programs. We should note such programs can also be regarded as quality improvement.
Therefore, the objective of this paper was to analyze how the pain-management program was implemented in the electrophysiology clinic. The tools used derive from normalization process theory and social marketing. Normalization process theory, derived from sociology, aims to understand the mechanics by which complex interventions are implemented. The method explains how participants behave in the organizational and social context of those interventions. Social marketing aims to achieve the “greater good” by using marketing concepts to influence behavior. Such changes in practice are common in quality-improvement processes, and therefore our goal was to provide a template for others to implement similar change programs.
2. Methods
Because the methodology we employed will be unfamiliar to many healthcare professionals, we will deviate from the standard manuscript format. Instead, before describing the specific methods used, we will explain (1) the practice change setting, (2) why a practice change was needed, (3) outline the theory behind the approaches used to implement and assess practice change, and (4) introduce the language associated with normalization practice theory.
(1) Practice change setting. The Helios Heart Center Leipzig is a 440-bed tertiary referral center that specializes in general cardiology, electrophysiology, cardiac surgery, and pediatric cardiology. Our electrophysiology department treats approximately 3,000 patients per year. Most clinic patients suffer from cardiac arrhythmias that require interventional therapy; for example, ablation procedures for atrial fibrillation and ventricular tachycardia, and pacemaker and cardioverter defibrillator implantations.
The first author (KB) was assigned responsibility to obtain federal government certification for the electrophysiology department’s pain management program. The multidisciplinary team consisted of one physician from each hospital department, a nurse specialist in pain management, the head of nursing, the head of quality management, and an anesthesiologist. These personnel, together with the 45 nurses and 20 physicians who participated in the implementation of the program, were primary stakeholders. The hospital administration, although consulted throughout the process, was considered an indirect stakeholder.
(2) Need for practice change. An initial assessment of pain management practices was conducted in all departments by an external certification organization. This evaluation revealed quality targets for pain management had not been achieved. The initial reaction by senior physicians within the Electrophysiology Department was, “we do excellent work, and there is no need for pain management”. Physicians questioned the assessment methodology and disputed recommendations for a post-interventional pain-management program. In contrast, the department’s nurses stated that patients often reported moderate-to-severe pain after interventional procedures.
To address resistance among physicians, we conducted an additional survey, focused solely on patients’ needs. We expanded the sample size well above that of the original survey. This survey’s main finding was a high prevalence of post-procedural pain [7]. These new data served numerous purposes to illustrate the need for practice change. (1) Data forced physicians to appreciate there was indeed a problem with pain management that required attention. (2) Because the survey was conducted in-house, physicians considered the data legitimate. The results also validated the initial assessment. (3) The results enabled the consensus required to proceed with implementation of the program. (4) The data also revealed barriers to effective pain management from the perspectives of patients, nurses, and physicians. (5) The survey identified potential collaborative efforts that nurses, and physicians could adopt to benefit patients. The policy developed to initiate the program is outlined in reference [7].
(3) Theory of the approaches used to implement change. To embed complex interventions in complex settings requires collective, rather than individual, action [11]. Normalization process theory examines behaviors associated with new ways of implementation, conceptualization, or organization of practice. Such change includes collective action that results from complex patterns of social relations or interactions [12,13]. Application of normalization process theory can be assisted by social marketing tools. The latter are defined and categorized by the methodological program of the Cochrane Effective Practice and Organization of Care Review Group (EPOC) [14]. The framework provided enables comparison of research on behavioral change interventions.
(4) Normalization Process Theory. Normalization process theory represents a conceptual framework [15]. The intent is to promote understanding and explanations of dynamic processes involved in normalizing innovation [11]. The goal is to make complex interventions routine [13,16] and to embed them into social contexts [12]. The approach is content-specific, and thereby seeks to improve sustainability of change intervention [17] to the extent that the change becomes part of an organization’s culture [18]. Normalization process theory addresses the roles of individuals and groups; the realities of implementation of practice changes require both to succeed [19]. Consequently, the approach appeared well-suited to our quality improvement goal because it was used in previous successful programs [20].
There are four theoretical components to normalization process theory and each of the four components contains four elements. These 16 parts represent a considerable amount of information, which is most easily understood in practical terms (as described in Table 1). Therefore, here, we will outline them briefly:

Table 1.
NPT elements relevant to the program, and the EPOC and social marketing tools used.
(1) Coherence/Sense Making—represents how individuals and groups think, understand, and organize when implementing new processes; (a) Differentiation—understanding how the previous and proposed practices differ; (b) Communal Specification—involves the entire team working together to understand how new practices can be implemented; (c) Individual Specification—focuses on what is required of each person; (d) Internalization—appreciation of the value of the change.
(2) Cognitive Participation—the work involved to initiate the process, to organize and become involved, to contribute, and to stay involved to achieve the change. (a) Initiation—key participants should work to advance the project; (b) Enrollment—participants may need to be reorganized and appreciate how their work may change; (c) Legitimation—ensures that participants believe it is appropriate for them to be involved and that they can contribute; (d) Activation—participants must understand what is required to maintain practice change.
(3) Collective Action—how people interact and gain confidence with each other and with the elements of the change, and how resources and work are allocated. (a) Interactional workability—how participants interact with each other and the program; (b) Relational integration—how participants maintain trust in each other and in the program; (c) Skill set workability—the allocation of tasks is appropriate; (d) Contextual integration—ensures that allocation of resources is appropriate.
(4) Reflexive monitoring—appraisal of how the new program affects individuals and the organization. (a) Systematization—collection of information related to the program’s effects; (b) Communal appraisal—how participants evaluate data collected; (c) Individual appraisal—how participants evaluate program effects on them and their work; (d) Reconfiguration—does communal or individual appraisal result in attempts to change the program or practices within the program.
Each element can either assist or resist change because each element is derived from existing norms and conventions [12]. Knowledge of such norms and conventions help design interventions that are culturally acceptable to the group [23].
The steps, materials, and documentation described above were recorded at each stage in the process, which enabled precise recall [24]. This information was then coded according to the normalization process theory framework, adapted from earlier work [25,26,27,28]. The senior author (HA) conducted a cross-comparison [28] of the results to ensure their relation to the normalization theory framework. Similarly, the data were also coded according to the EPOC framework [14]. When that framework failed to reflect the tasks performed, we added additional marketing concepts. The collection and coding of the qualitative data addressed issues to do with validity, reliability and generalizability [29].
3. Results
Our analysis consisted of three facets. First, information on steps taken was coded and split into two sections. The first section divided processes involved in the pain-management program according to the 16 elements of normalization process theory described above: Table 1, column 3. The second section divided processes using the EPOC taxonomy and social marketing as they related to the normalization process theory elements (Table 1, column 4).
The third facet, performed in parallel with the second, focused on the social marketing. Figure 1 shows a schematic representation of our approach to marketing the program. The first step was research to identify the key stakeholders and establish their needs and wants. Subsequently, we determined the value each stakeholder group could derive from the program. In turn, this step enabled us to define the required behavior changes and their implications in terms of benefits and costs [30]. Two potential loops were identified. We initiated one of these loops to reinforce the changes and their value. We sought direct involvement of participants in as many aspects of the program as possible. In general, the greater the involvement, the greater the perceived value participants derived. The second loop involved provision of tangible benefits to stakeholders and promise of future benefits.
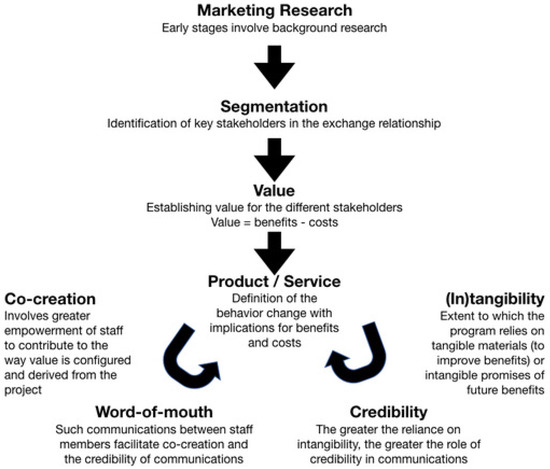
Figure 1.
Social marketing concepts involved in the implementation of the behavior change intervention.
4. Discussion
Our analysis revealed how positive results from a quality-improvement project appeared consistent with successful application of normalization process theory. Furthermore, social marketing efforts enhanced the project. The program reduced the risk of late (between 8 and 24 h) post-interventional pain three-fold (odds ratio 0.32, 95% confidence intervals [0.16 to 0.64]; p = 0.001) [8].
Normalization process theory has typically been applied in the context of introduction of new interventions or practices [31]. However, the concept has also been extended to continuity of care [32]. Although such innovations can be regarded as quality improvement, direct connection between the two has seldom been made [33,34]. Since Donabedian’s seminal work [35], quality has been a focus of healthcare. Efforts to improve quality have likewise become a focus. Although methods for quality improvement, for example plan-do-study-act cycles, have been developed, the reasons behind the success or failure of such innovations remain obscure [36]. Many of the issues discussed in Siriwardena’s review [36] parallel the structure of normalization process theory. Similar parallels appear in a review of a proposed method of quality improvement in surgery [37]. Therefore, we speculated that the framework of normalization process theory could serve as a template for successful quality improvement. The advantage of normalization process theory, as emphasized by May, is not to provide a rigid set of instruction, but instead to offer a flexible framework [38].
Social marketing tools complement the use of normalization process theory. For example, our use of empirical data helped convince senior managers of the initiative’s value [39]. We were unable to offer monetary benefits. We instead emphasized the following: (1) adequate pain management is an ethical concern; (2) pain management is required for faster recovery; (3) patient satisfaction is crucial because it underpins future decisions on where to obtain healthcare [40]; (4) early pain assessment and treatment reduces patient dissatisfaction [8]; (5) patient dissatisfaction stresses hospital staff and thereby decreases job satisfaction.
In a previous study, nurses identified the inability to consult pharmacists on pain management as a barrier to effective therapy [41]. Likewise, Van Valen et al. revised their pain-management protocols such that nurses were not required to consult physicians [42]. Our protocols provided nurses with autonomy to administer pain medication, within defined limits, without physician approval. Nonetheless, physicians were tasked with ensuring adequate pain management. These combined efforts to address post-interventional pain underlined the abovementioned benefits; i.e., they serve to increase patient and staff satisfaction, and enhance hospital reputation [40,43].
Educational seminars helped develop proposals for standard operating procedures. Both nurses and physicians were able to incorporate ideas and suggestions as the program developed. This process enabled participants to derive value not only at the start of the program, but also as the program progressed [44], an illustration of value co-creation. Marketing concepts also played a role in the seminars; for example, exchange and “get” notions [45,46]. In these interactions, value is defined as the benefit received minus the cost incurred. For patients, the benefit is less pain minus the cost of providing personal information to nurses. For nurses, the benefit is increased patient satisfaction and the cost is time spent asking patients about pain and chart documentation [47,48,49]. Because we demonstrated significant decreases in the post-interventional pain after successful implementation of our pain-management program, it is reasonable to assume all stakeholders would perceive the change as beneficial.
Analysis of behavior change interventions with normalization process theory and the EPOC approaches has been reported at population [50] and organization [51] levels. These sociology-based theories help understand the implementation, integration, and consolidation of innovation in healthcare [52]. We applied the theories to behavior change intervention to reveal the dynamics and barriers to, and facilitators of, change. We employed a participatory approach. Participatory normalization process theory methods were recently used to incorporate an electronic patient-reported outcome measure in routine care [53].
In the step-coding process, we did not assign processes to every normalization process theory category—an issue described by other investigators [54]. Although such omissions could be perceived as weakness, one strength of normalization process theory is that it permits coding flexibility, and analysis should consider context [20]. Furthermore, because implementation processes are dynamic, the expectation that a single theory covers all aspects of all processes is unrealistic.
In this context, we should acknowledge that normalization process theory can be regarded as one element of the broader field of implementation science [55]. Implementation science’s goal of translating clinical innovation into clinical practice matches what we sought to achieve. There are multiple strategies [56], frameworks, and theories [57] that can be applied in implementation science. The appropriate choices will likely be determined by context.
Marketing: Our analysis added two concepts to the EPOC framework to explain the efficacy of marketing tools. Tangibility: the participants’ ability to define and describe the program and process will aid their understanding of its potential attributes and value [58,59]. Our use of seminars and distribution of educational material contributed to tangibility. Of course, tangibility cannot always be achieved and sometimes only intangibles can be offered, such as promises of future benefits [60]. However, for the latter to be effective, the change agent must be trusted and credible, as shown by the second novel concept in Figure 1.
Persistent Challenges: We, like many academic medical facilities, face the challenge of considerable staff turnover. Therefore, to maintain adherence requires constant effort. Current and new staff require frequent training sessions and motivation to continue with the development of normalization process theory. Nonetheless, despite these persistent challenges, diligent application of our implementation strategy resulted in persistence of quality improvement in the pain management program, as we described [8].
5. Conclusions
Implementation of change and quality-improvement initiatives invariably present challenges. We demonstrated successful intervention to change behavior, and improve quality, based upon normalization process theory and adaptation of tools from social marketing and from the EPOC. We propose that concepts from marketing disciplines will provide further insights into how acceptability of such behavioral change and quality improvement interventions can be enhanced. Specifically, concepts of tangibility and co-creation enable change instigators to focus on the clarity of the processes and outcomes of change and thereby explain the relevance to stakeholders.
Author Contributions
Conceptualization, H.A. and K.B.; Methodology, H.A. and K.B.; Validation, H.A., K.B., M.D., P.W. and Y.B.; Formal Analysis, H.A., K.B. and P.W.; Investigation, H.A., K.B., M.D., P.W. and Y.B.; Data Curation, H.A. and K.B.; Writing—Original Draft Preparation, K.B.; Writing—Review & Editing, H.A., K.B. and P.W.; Visualization, H.A., K.B. and P.W.; Supervision, H.A., K.B. and P.W.; Project Administration, K.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lester, P.E.; Shehata, J.; Fazzari, M.; Islam, S. Impact of Hospital-Wide Comprehensive Pain Management Initiatives. Am. J. Med. Qual. 2017, 32, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Brenn, B.R.; Choudhry, D.K.; Sacks, K.; Como-Fluehr, S.; Strain, R. Toward Better Pain Management: The Development of a “Pain Stewardship Program” in a Tertiary Children’s Hospital. Hosp. Pediatr. 2016, 6, 520–528. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Park, M. Geriatric nurses’ empathy, attitude and pain management for patients with dementia. Korean J. Adult Nurs. 2016, 28, 388–398. [Google Scholar] [CrossRef]
- Breivik, H. How to implement an acute pain service. Best Pract. Res. Clin. Anaesthesiol. 2002, 16, 527–547. [Google Scholar] [CrossRef] [PubMed]
- Andersson, V.; Bergman, S.; Henoch, I.; Ene, K.W.; Otterstrom-Rydberg, E.; Simonsson, H.; Ahlberg, K. Pain and pain management in hospitalized patients before and after an intervention. Scand. J. Pain 2017, 15, 22–29. [Google Scholar] [CrossRef]
- Bjornnes, A.K.; Parry, M.; Lie, I.; Fagerland, M.W.; Watt-Watson, J.; Rustoen, T.; Stubhaug, A.; Leegaard, M. The impact of an educational pain management booklet intervention on postoperative pain control after cardiac surgery. Eur. J. Cardiovasc. Nurs. 2017, 16, 18–27. [Google Scholar] [CrossRef]
- Bode, K.; Breithardt, O.A.; Kreuzhuber, M.; Mende, M.; Sommer, P.; Richter, S.; Doering, M.; Dinov, B.; Rolf, S.; Arya, A.; et al. Patient discomfort following catheter ablation and rhythm device surgery. Europace 2015, 17, 1129–1135. [Google Scholar] [CrossRef]
- Dorschner, M.; Bollmann, A.; Dinov, B.; Richter, S.; Doring, M.; Arya, A.; Mussigbrodt, A.; Kircher, S.; Dagres, N.; Sommer, P.; et al. Structured pain management reduces patient discomfort after catheter ablation and rhythm device surgery. Eur. J. Pain 2017, 21, 1723–1731. [Google Scholar] [CrossRef]
- Gerbershagen, H.J. Transition from acute to chronic postsurgical pain. Physiology, risk factors and prevention. Schmerz 2013, 27, 81–93, quiz 94–95. [Google Scholar] [CrossRef]
- Raatikainen, M.J.P.; Arnar, D.O.; Merkely, B.; Nielsen, J.C.; Hindricks, G.; Heidbuchel, H.; Camm, J. A Decade of Information on the Use of Cardiac Implantable Electronic Devices and Interventional Electrophysiological Procedures in the European Society of Cardiology Countries: 2017 Report from the European Heart Rhythm Association. Europace 2017, 19, ii1–ii90. [Google Scholar] [CrossRef]
- Johnson, M.J.; May, C.R. Promoting professional behaviour change in healthcare: What interventions work, and why? A theory-led overview of systematic reviews. BMJ Open 2015, 5, e008592. [Google Scholar] [CrossRef] [PubMed]
- May, C.; Finch, T. Implementing, Embedding, and Integrating Practices: An Outline of Normalization Process Theory. Sociology 2009, 43, 535–554. [Google Scholar] [CrossRef]
- May, C.; Finch, T.; Ballini, L.; MacFarlane, A.; Mair, F.; Murray, E.; Treweek, S.; Rapley, T. Evaluating complex interventions and health technologies using normalization process theory: Development of a simplified approach and web-enabled toolkit. BMC Health Serv. Res. 2011, 11, 245. [Google Scholar] [CrossRef] [PubMed]
- Cochrane-Group. The Data Collection Checklist. Available online: http://methods.cochrane.org/sites/methods.cochrane.org.bias/files/public/uploads/EPOC%20Data%20Collection%20Checklist.pdf (accessed on 3 July 2019).
- May, C. Agency and implementation: Understanding the embedding of healthcare innovations in practice. Soc. Sci. Med. 2013, 78, 26–33. [Google Scholar] [CrossRef]
- Andreasen, A.R. Marketing Social Change: Changing Behavior to Promote Health, Social Development, and the Environment; John Wiley & Sons: New York, NY, USA, 1995. [Google Scholar]
- Willis, K.; Small, R.; Brown, S. Using documents to investigate links between implementation and sustainability in a complex community intervention: The PRISM study. Soc. Sci. Med. 2012, 75, 1222–1229. [Google Scholar] [CrossRef]
- Schudson, M.; Baykurt, B. How does a culture of health change? Lessons from the war on cigarettes. Soc. Sci. Med. 2016, 165, 289–296. [Google Scholar] [CrossRef]
- de Brun, T.; O’Reilly-de Brun, M.; O’Donnell, C.A.; MacFarlane, A. Learning from doing: The case for combining normalisation process theory and participatory learning and action research methodology for primary healthcare implementation research. BMC Health Serv. Res. 2016, 16, 346. [Google Scholar] [CrossRef]
- McEvoy, R.; Ballini, L.; Maltoni, S.; O’Donnell, C.A.; Mair, F.S.; Macfarlane, A. A qualitative systematic review of studies using the normalization process theory to research implementation processes. Implement. Sci. IS 2014, 9, 2. [Google Scholar] [CrossRef]
- Foedermayr, E.K.; Diamantopoulos, A. Market Segmentation in Practice: Review of Empirical Studies, Methodological Assessment, and Agenda for Future Research. J. Strateg. Mark. 2008, 16, 223–265. [Google Scholar] [CrossRef]
- Kozinets, R.V.; de Valck, K.; Wojnicki, A.C.; Wilner, S.J.S. Networked Narratives: Understanding Word-of-Mouth Marketing in Online Communities. J. Mark. 2010, 74, 71–89. [Google Scholar] [CrossRef]
- Panter-Brick, C.; Clarke, S.E.; Lomas, H.; Pinder, M.; Lindsay, S.W. Culturally compelling strategies for behaviour change: A social ecology model and case study in malaria prevention. Soc. Sci. Med. 2006, 62, 2810–2825. [Google Scholar] [CrossRef] [PubMed]
- Egan, G. Working the Shadow Side: A Guide to Positive behind The Scenes Management; Jossey-Bass: San Francisco, CA, USA, 1994. [Google Scholar]
- Gallacher, K.; May, C.R.; Montori, V.M.; Mair, F.S. Understanding patients’ experiences of treatment burden in chronic heart failure using normalization process theory. Ann. Fam. Med. 2011, 9, 235–243. [Google Scholar] [CrossRef] [PubMed]
- MacFarlane, A.; O’Donnell, C.; Mair, F.; O’Reilly-de Brun, M.; de Brun, T.; Spiegel, W.; van den Muijsenbergh, M.; van Weel-Baumgarten, E.; Lionis, C.; Burns, N.; et al. REsearch into implementation STrategies to support patients of different ORigins and language background in a variety of European primary care settings (RESTORE): Study protocol. Implement. Sci. IS 2012, 7, 111. [Google Scholar] [CrossRef] [PubMed]
- Macfarlane, A.; O’Reilly-de Brun, M. Using a theory-driven conceptual framework in qualitative health research. Qual. Health Res. 2012, 22, 607–618. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, A.; Kaner, E. Are Brief Alcohol Interventions Adequately Embedded in UK Primary Care? A Qualitative Study Utilising Normalisation Process Theory. Int. J. Environ. Res. Public Health 2017, 14, 350. [Google Scholar] [CrossRef]
- Leung, L. Validity, reliability, and generalizability in qualitative research. J. Fam. Med. Prim. Care 2015, 4, 324–327. [Google Scholar] [CrossRef]
- Finfgeld-Connett, D. Generalizability and transferability of meta-synthesis research findings. J. Adv. Nurs. 2010, 66, 246–254. [Google Scholar] [CrossRef]
- Huddlestone, L.; Turner, J.; Eborall, H.; Hudson, N.; Davies, M.; Martin, G. Application of normalisation process theory in understanding implementation processes in primary care settings in the UK: A systematic review. BMC Fam. Pract. 2020, 21, 52. [Google Scholar] [CrossRef]
- Corrigan, A.E.; Lake, S.; McInnes, R.J. Normalisation process theory as a conceptual framework for continuity of carer implementation. Women Birth 2021, 34, e204–e209. [Google Scholar] [CrossRef]
- Trietsch, J.; van Steenkiste, B.; Hobma, S.; Frericks, A.; Grol, R.; Metsemakers, J.; van der Weijden, T. The challenge of transferring an implementation strategy from academia to the field: A process evaluation of local quality improvement collaboratives in Dutch primary care using the normalization process theory. J. Eval. Clin. Pract. 2014, 20, 1162–1171. [Google Scholar] [CrossRef]
- Wagner, N.R.; Melin, T.T.; Wood, F. Implementation of Telehealth: Normalization Process Theory and NoMAD-Ex. J. Nurse Pract. 2021, 17, 1141–1143. [Google Scholar] [CrossRef]
- Donebedian, A. Evaluating the Quality of Medical Care. Milbank Q. 2005, 44, 166–203. [Google Scholar] [CrossRef]
- Siriwardena, A.N. Why quality improvement initiatives succeed or fail: The MUSIQ of quality improvement. Qual. Prim. Care 2012, 20, 1–3. [Google Scholar] [PubMed]
- Wiegmann, D.A. Understanding Why Quality Initiatives Succeed or Fail: A Sociotechnical Systems Perspective. Ann. Surg. 2016, 263, 9–11. [Google Scholar] [CrossRef]
- May, C. A rational model for assessing and evaluating complex interventions in health care. BMC Health Serv. Res. 2006, 6, 86. [Google Scholar] [CrossRef]
- Erlingsdottir, G.; Ersson, A.; Borell, J.; Rydenfalt, C. Driving for successful change processes in healthcare by putting staff at the wheel. J. Health Organ. Manag. 2018, 32, 69–84. [Google Scholar] [CrossRef]
- Hewison, A.; Sawbridge, Y.; Cragg, R.; Rogers, L.; Lehmann, S.; Rook, J. Leading with compassion in health care organisations. J. Health Organ. Manag. 2018, 32, 338–354. [Google Scholar] [CrossRef]
- Medrzycka-Dabrowska, W.A.; Dabrowski, S.; Basinski, A.; Pilch, D. Perception of barriers to postoperative pain management in elderly patients in Polish hospitals with and without a “Hospital without Pain” Certificate—A multi-center study. Arch. Med. Sci. 2016, 12, 808–818. [Google Scholar] [CrossRef]
- van Valen, R.; van Vuuren, H.; van Domburg, R.T.; van der Woerd, D.; Hofland, J.; Bogers, A.J. Pain management after cardiac surgery: Experience with a nurse-driven pain protocol. Eur. J. Cardiovasc. Nurs. 2012, 11, 62–69. [Google Scholar] [CrossRef]
- De Gieter, S.; De Cooman, R.; Pepermans, R.; Caers, R.; Du Bois, C.; Jegers, M. Identifying nurses’ rewards: A qualitative categorization study in Belgium. Hum. Resour. Health 2006, 4, 15. [Google Scholar] [CrossRef][Green Version]
- Trout, A.; Magnusson, A.R.; Hedges, J.R. Patient satisfaction investigations and the emergency department: What does the literature say? Acad. Emerg. Med. 2000, 7, 695–709. [Google Scholar] [CrossRef] [PubMed]
- Duane, S.; Domegan, C.; McHugh, P.; Devaney, M. From restricted to complex exchange and beyond: Social marketing’s change agenda. J. Mark. Manag. 2016, 32, 856–876. [Google Scholar] [CrossRef]
- Zeithaml, V. Consumer Perceptions of Price, Quality and Value: A Means-End Model and Synthesis of Evidence. J. Mark. 1988, 52, 2–22. [Google Scholar] [CrossRef]
- Karlsson, C.; Sidenvall, B.; Bergh, I.; Ernsth-Bravell, M. Registered Nurses View of Performing Pain Assessment among Persons with Dementia as Consultant Advisors. Open Nurs. J. 2012, 6, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Ovretveit, J. Understanding and improving patient safety: The psychological, social and cultural dimensions. J. Health Organ. Manag. 2009, 23, 581–596. [Google Scholar] [CrossRef]
- Groene, O.; Sunol, R. Patient involvement in quality management: Rationale and current status. J. Health Organ. Manag. 2015, 29, 556–569. [Google Scholar] [CrossRef]
- Paul, C.L.; Sanson-Fisher, R.; Stewart, J.; Anderson, A.E. Being Sorry Is Not Enough. Am. J. Prev. Med. 2010, 38, 566–568. [Google Scholar] [CrossRef]
- Shekelle, P.G.; Pronovost, P.J.; Wachter, R.M.; McDonald, K.M.; Schoelles, K.; Dy, S.M.; Shojania, K.; Reston, J.T.; Adams, A.S.; Angood, P.B.; et al. The top patient safety strategies that can be encouraged for adoption now. Ann. Intern. Med. 2013, 158, 365–368. [Google Scholar] [CrossRef]
- Murray, E.; Treweek, S.; Pope, C.; MacFarlane, A.; Ballini, L.; Dowrick, C.; Finch, T.; Kennedy, A.; Mair, F.; O’Donnell, C.; et al. Normalisation process theory: A framework for developing, evaluating and implementing complex interventions. BMC Med. 2010, 8, 63. [Google Scholar] [CrossRef]
- Knowles, S.E.; Ercia, A.; Caskey, F.; Rees, M.; Farrington, K.; Van der Veer, S.N. Participatory co-design and normalisation process theory with staff and patients to implement digital ways of working into routine care: The example of electronic patient-reported outcomes in UK renal services. BMC Health Serv. Res. 2021, 21, 706. [Google Scholar] [CrossRef]
- Atkins, S.; Lewin, S.; Ringsberg, K.C.; Thorson, A. Provider experiences of the implementation of a new tuberculosis treatment programme: A qualitative study using the normalisation process model. BMC Health Serv. Res. 2011, 11, 275. [Google Scholar] [CrossRef] [PubMed]
- Bauer, M.S.; Kirchner, J. Implementation science: What is it and why should I care? Psychiatry Res. 2020, 283, 112376. [Google Scholar] [CrossRef] [PubMed]
- Kirchner, J.E.; Smith, J.L.; Powell, B.J.; Waltz, T.J.; Proctor, E.K. Getting a clinical innovation into practice: An introduction to implementation strategies. Psychiatry Res. 2020, 283, 112467. [Google Scholar] [CrossRef] [PubMed]
- Damschroder, L.J. Clarity out of chaos: Use of theory in implementation research. Psychiatry Res. 2020, 283, 112461. [Google Scholar] [CrossRef]
- McDougall, G.H.G. The intangibility of services: Measurement and competitive perspectives. J. Serv. Mark. 1990, 4, 27–40. [Google Scholar] [CrossRef]
- Laroche, M.; McDougall, G.H.G.; Bergeron, J.; Yang, Z. Exploring how intangibility affects perceived risk. J. Serv. Res. 2004, 6, 373–389. [Google Scholar] [CrossRef]
- Jyh-Shen, C.; Droge, C. Service quality, trust, specific asset investment and expertise: Direct and indirect effects in a satisfaction-loyalty framework. J. Acad. Mark. Sci. 2006, 34, 613–627. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).