Loneliness in Older Indian Dyads
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Measures
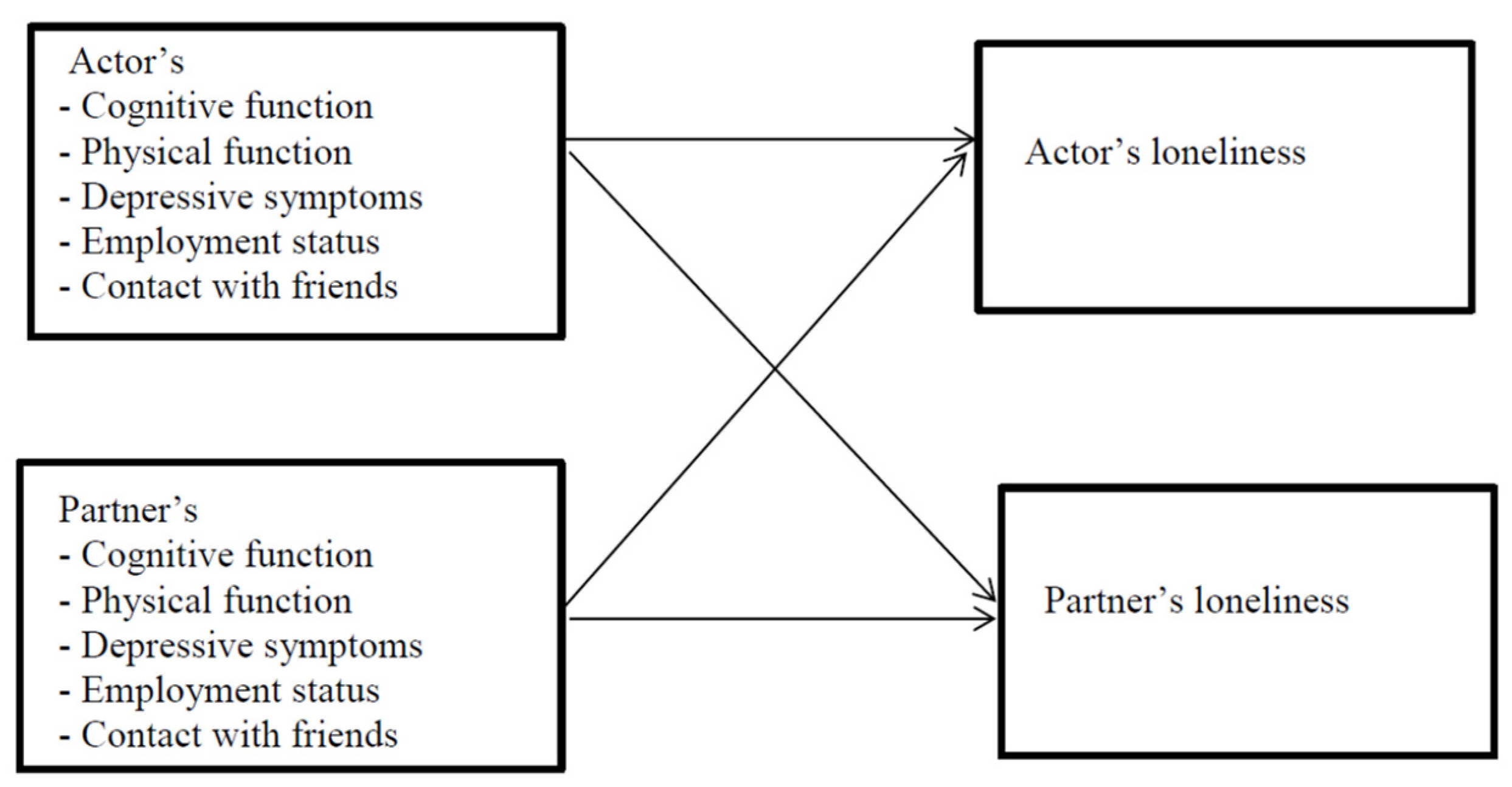
2.3. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Peplau, L.A.; Perlman, D. Perspectives on loneliness. In Loneliness: A Sourcebook of Current Theory, Research and Therapy; Peplau, L.A., Perlman, D., Eds.; John Wiley & Sons: New York, NY, USA, 1982; pp. 1–18. [Google Scholar]
- Cornwell, E.Y.; Waite, L.J. Social disconnectedness, perceived isolation, and health among older adults. J. Health Soc. Behav. 2009, 50, 31–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leigh-Hunt, N.; Bagguley, D.; Bash, K.; Turner, V.; Turnbull, S.; Valtorta, N.; Caan, W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 2017, 152, 157–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Surkalim, D.L.; Luo, M.; Eres, R.; Gebel, K.; van Buskirk, J.; Bauman, A.; Ding, D. The prevalence of loneliness across 113 countries: Systematic review and meta-analysis. BMJ 2022, 376, e067068. [Google Scholar] [CrossRef] [PubMed]
- Prohaska, T.; Burholt, V.; Burns, A.; Golden, J.; Hawkley, L.; Lawlor, B.; Leavey, G.; Lubben, J.; Sullivan, R.; Perissinotto, C.; et al. Consensus statement: Loneliness in older adults, the 21st century social determinant of health? BMJ Open 2020, 10, e034967. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences; Division of Behavioral and Social Sciences and Education; Health and Medicine Division; Board on Behavioral; Sensory Sciences; Board on Health Sciences Policy; Committee on the Health and Medical Dimensions of Social Isolation and Loneliness in Older Adults. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System; National Academies Press (US): Washington, DC, USA, 2020. [Google Scholar]
- Ong, A.D.; Uchino, B.N.; Wethington, E. Loneliness and Health in Older Adults: A Mini-Review and Synthesis. Gerontology 2016, 62, 443–449. [Google Scholar] [CrossRef] [PubMed]
- NSO. Elderly in India 2021; National Statistical Office, Ministry of Statistics & Programme Implementation, Government of India: New Delhi, India, 2021.
- United Nations Population Fund. Caring for Our Elders: Early Responses-India Ageing Report–2017; UNFPA: New Delhi, India, 2017. [Google Scholar]
- About LASI. Available online: https://www.hsph.harvard.edu/pgda/major-projects/lasi-2/ (accessed on 2 April 2022).
- Perianayagam, A.; Bloom, D.; Lee, J.; Parasuraman, S.; Sekher, T.V.; Mohanty, S.K.; Chattopadhyay, A.; Govil, D.; Pedgaonkar, S.; Gupta, S.; et al. Cohort Profile: The Longitudinal Ageing Study in India (LASI). Int. J. Epidemiol. 2022, dyab266. [Google Scholar] [CrossRef]
- Cohen-Mansfield, J.; Hazan, H.; Lerman, Y.; Shalom, V. Correlates and predictors of loneliness in older-adults: A review of quantitative results informed by qualitative insights. Int. Psychogeriatr. 2016, 28, 557–576. [Google Scholar] [CrossRef]
- Pengpid, S.; Peltzer, K. Associations of loneliness with poor physical health, poor mental health and health risk behaviours among a nationally representative community-dwelling sample of middle-aged and older adults in India. Int. J. Geriatr. Psychiatry 2021, 36, 1722–1731. [Google Scholar] [CrossRef]
- Gao, Q.; Prina, A.M.; Prince, M.; Acosta, D.; Luisa Sosa, A.; Guerra, M.; Huang, Y.; Jimenez-Velazquez, I.Z.; Llibre Rodriguez, J.J.; Salas, A.; et al. Loneliness Among Older Adults in Latin America, China, and India: Prevalence, Correlates and Association With Mortality. Int. J. Public Health 2021, 66, 604449. [Google Scholar] [CrossRef]
- Farrell, A.K.; Stanton, S.C.E. Toward a Mechanistic Understanding of Links Between Close Relationships and Physical Health. Curr. Dir. Psychol. Sci. 2019, 28, 483–489. [Google Scholar] [CrossRef] [Green Version]
- Holt-Lunstad, J. Why Social Relationships Are Important for Physical Health: A Systems Approach to Understanding and Modifying Risk and Protection. Annu. Rev. Psychol. 2018, 69, 437–458. [Google Scholar] [CrossRef] [PubMed]
- Walker, S.C.; McGlone, F.P. The social brain: Neurobiological basis of affiliative behaviours and psychological well-being. Neuropeptides 2013, 47, 379–393. [Google Scholar] [CrossRef] [PubMed]
- Victor, C.R.; Scambler, S.J.; Bowling, A.N.N.; Bond, J. The prevalence of, and risk factors for, loneliness in later life: A survey of older people in Great Britain. Ageing Soc. 2005, 25, 357–375. [Google Scholar] [CrossRef] [Green Version]
- de Jong Gierveld, J.; van Groenou, M.B.; Hoogendoorn, A.W.; Smit, J.H. Quality of marriages in later life and emotional and social loneliness. J. Gerontol. B Psychol. Sci. Soc. Sci. 2009, 64, 497–506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- English, T.; Carstensen, L.L. Selective Narrowing of Social Networks Across Adulthood is Associated With Improved Emotional Experience in Daily Life. Int. J. Behav. Dev. 2014, 38, 195–202. [Google Scholar] [CrossRef] [Green Version]
- Warner, D.F.; Adams, S.A. Physical Disability and Increased Loneliness among Married Older Adults: The Role of Changing Social Relations. Soc. Ment. Health 2016, 6, 106–128. [Google Scholar] [CrossRef]
- Warner, D.F.; Kelley-Moore, J. The social context of disablement among older adults: Does marital quality matter for loneliness? J. Health Soc. Behav. 2012, 53, 50–66. [Google Scholar] [CrossRef]
- Stokes, J.E. Marital quality and loneliness in later life: A dyadic analysis of older married couples in Ireland. J. Soc. Pers. Relatsh. 2016, 34, 114–135. [Google Scholar] [CrossRef] [Green Version]
- Lara, E.; Martín-María, N.; De la Torre-Luque, A.; Koyanagi, A.; Vancampfort, D.; Izquierdo, A.; Miret, M. Does loneliness contribute to mild cognitive impairment and dementia? A systematic review and meta-analysis of longitudinal studies. Ageing Res. Rev. 2019, 52, 7–16. [Google Scholar] [CrossRef]
- Gale, C.R.; Westbury, L.; Cooper, C. Social isolation and loneliness as risk factors for the progression of frailty: The English Longitudinal Study of Ageing. Age Ageing 2018, 47, 392–397. [Google Scholar] [CrossRef] [Green Version]
- Perissinotto, C.M.; Stijacic Cenzer, I.; Covinsky, K.E. Loneliness in older persons: A predictor of functional decline and death. Arch. Intern. Med. 2012, 172, 1078–1083. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Domènech-Abella, J.; Mundó, J.; Switsers, L.; van Tilburg, T.; Fernández, D.; Aznar-Lou, I. Social network size, loneliness, physical functioning and depressive symptoms among older adults: Examining reciprocal associations in four waves of the Longitudinal Aging Study Amsterdam (LASA). Int. J. Geriatr. Psychiatry 2021, 36, 1541–1549. [Google Scholar] [CrossRef] [PubMed]
- Okely, J.A.; Deary, I.J. Longitudinal Associations between Loneliness and Cognitive Ability in the Lothian Birth Cohort 1936. J. Gerontol. Ser. B 2019, 74, 1376–1386. [Google Scholar] [CrossRef] [PubMed]
- Zhong, B.-L.; Chen, S.-L.; Tu, X.; Conwell, Y. Loneliness and Cognitive Function in Older Adults: Findings From the Chinese Longitudinal Healthy Longevity Survey. J. Gerontol. B Psychol. Sci. Soc. Sci. 2017, 72, 120–128. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Hawkley, L.C.; Thisted, R.A. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol. Aging 2010, 25, 453–463. [Google Scholar] [CrossRef] [Green Version]
- McHugh Power, J.; Hannigan, C.; Hyland, P.; Brennan, S.; Kee, F.; Lawlor, B.A. Depressive symptoms predict increased social and emotional loneliness in older adults. Aging Mental. Health 2020, 24, 110–118. [Google Scholar] [CrossRef]
- Hsieh, N.; Hawkley, L. Loneliness in the older adult marriage: Associations with dyadic aversion, indifference, and ambivalence. J. Soc. Pers. Relatsh. 2018, 35, 1319–1339. [Google Scholar] [CrossRef]
- Sbarra, D.A.; Hazan, C. Coregulation, dysregulation, self-regulation: An integrative analysis and empirical agenda for understanding adult attachment, separation, loss, and recovery. Personal. Soc. Psychol. Rev. Off. J. Soc. Personal. Soc. Psychol. Inc. 2008, 12, 141–167. [Google Scholar] [CrossRef]
- Wong, J.S.; Hsieh, N. Functional Status, Cognition, and Social Relationships in Dyadic Perspective. J. Gerontol. B Psychol. Sci. Soc. Sci. 2019, 74, 703–714. [Google Scholar] [CrossRef]
- Leggett, A.N.; Choi, H.; Chopik, W.J.; Liu, H.; Gonzalez, R. Early Cognitive Decline and its Impact on Spouse’s Loneliness. Res. Hum. Dev. 2020, 17, 78–93. [Google Scholar] [CrossRef]
- Korporaal, M.; Broese van Groenou, M.I.; van Tilburg, T.G. Effects of Own and Spousal Disability on Loneliness Among Older Adults. J. Aging Health 2008, 20, 306–325. [Google Scholar] [CrossRef] [PubMed]
- Siegel, M.J.; Bradley, E.H.; Gallo, W.T.; Kasl, S.V. The Effect of Spousal Mental and Physical Health on Husbands’ and Wives’ Depressive Symptoms, Among Older Adults: Longitudinal Evidence From the Health and Retirement Survey. J. Aging Health 2004, 16, 398–425. [Google Scholar] [CrossRef] [PubMed]
- Kouros, C.D.; Cummings, E.M. Longitudinal Associations Between Husbands’ and Wives’ Depressive Symptoms. J. Marriage Fam. 2010, 72, 135–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Butterworth, P.; Rodgers, B. Concordance in the mental health of spouses: Analysis of a large national household panel survey. Psychol. Med. 2005, 36, 685–697. [Google Scholar] [CrossRef]
- Ermer, A.E.; Segel-Karpas, D.; Benson, J.J. Loneliness trajectories and correlates of social connections among older adult married couples. J. Fam. Psychol. JFP J. Div. Fam. Psychol. Am. Psychol. Assoc. 2020, 34, 1014–1024. [Google Scholar] [CrossRef]
- Ermer, A.E.; Proulx, C.M. Social support and well-being among older adult married couples: A dyadic perspective. J. Soc. Pers. Relatsh. 2019, 37, 1073–1091. [Google Scholar] [CrossRef]
- Chen, Y.; Feeley, T.H. Social support, social strain, loneliness, and well-being among older adults: An analysis of the Health and Retirement Study. J. Soc. Pers. Relatsh. 2013, 31, 141–161. [Google Scholar] [CrossRef]
- International Institute for Population Sciences (IIPS); National Programme for Health Care of Elderly (NPHCE); MoHFW; Harvard, T.H.; Chan School of Public Health. Longitudinal Study of Ageing in India-Wave 1 India Report; The University of Southern California (USC): Mumbai, India, 2020. [Google Scholar]
- Redden, S. Older Workers Statistical Information Booklet 2013; Department for Work and Pensions: London, UK, 2013.
- Cruwys, T.; Haslam, C.; Steffens, N.K.; Haslam, S.A.; Fong, P.; Lam, B.C.P. Friendships that money can buy: Financial security protects health in retirement by enabling social connectedness. BMC Geriatr. 2019, 19, 319. [Google Scholar] [CrossRef]
- Loibl, C.; Drost, M.; Huisman, M.; Suanet, B.; Bruine de Bruin, W.; McNair, S.; Summers, B. Worry about debt is related to social loneliness in older adults in the Netherlands. Ageing Soc. 2021, 1–23. [Google Scholar] [CrossRef]
- Kenny, D.; Kashy, D.; Cook, W. Dyadic Data Analysis; Guilford Press: New York, NY, USA, 2006. [Google Scholar]
- International Institute for Population Sciences; Harvard School of Public Health; RAND Corporation USA. Longitudinal Ageing Study in India (LASI-Pilot Survey), 2010; IIPS: Mumbai, India, 2012. [Google Scholar]
- Sonnega, A.; Faul, J.D.; Ofstedal, M.B.; Langa, K.M.; Phillips, J.W.R.; Weir, D.R. Cohort Profile: The Health and Retirement Study (HRS). Int. J. Epidemiol. 2014, 43, 576–585. [Google Scholar] [CrossRef] [Green Version]
- Steptoe, A.; Breeze, E.; Banks, J.; Nazroo, J. Cohort Profile: The English Longitudinal Study of Ageing. Int. J. Epidemiol. 2013, 42, 1640–1648. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Cacioppo, J.T. A Short Scale for Measuring Loneliness in Large Surveys: Results From Two Population-Based Studies. Res. Aging 2004, 26, 655–672. [Google Scholar] [CrossRef] [PubMed]
- Brandt, J.; Spencer, M.; Folstein, M. The Telephone Interview for Cognitive Status. Cogn. Behav. Neurol. 1988, 1, 111–117. [Google Scholar]
- Ofstedal, M.B.; Fisher, G.G.; Herzog, A.R. Documentation of Cognitive Functioning Measures in the Health and Retirement Study; Institute for Social Research, University of Michigan: Ann Arbor, MI, USA, 2005. [Google Scholar]
- Tombaugh, T.N.; Kozak, J.; Rees, L. Normative data stratified by age and education for two measures of verbal fluency: FAS and animal naming. Arch. Clin. Neuropsychol. Off. J. Natl. Acad. Neuropsychol. 1999, 14, 167–177. [Google Scholar]
- Radloff, L.S. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Steffick, D.E. Documentation of Affective Functioning Measures in the Health and Retirement Study; The University of Michigan: Ann Arbor, MI, USA, 2000. [Google Scholar]
- Briggs, R.; Carey, D.; O’Halloran, A.; Kenny, R.; Kennelly, D.S. Validation of the 8-item Centre for Epidemiological Studies Depression Scale in a cohort of community-dwelling older people: Data from The Irish Longitudinal Study on Ageing (TILDA). Eur. Geriatr. Med. 2018, 9, 121–126. [Google Scholar] [CrossRef]
- Karim, J.; Weisz, R.; Bibi, Z.; ur Rehman, S. Validation of the Eight-Item Center for Epidemiologic Studies Depression Scale (CES-D) Among Older Adults. Curr. Psychol. 2015, 34, 681–692. [Google Scholar] [CrossRef]
- Cook, W.L.; Kenny, D.A. The Actor–Partner Interdependence Model: A model of bidirectional effects in developmental studies. Int. J. Behav. Dev. 2005, 29, 101–109. [Google Scholar] [CrossRef]
- Stas, L.; Kenny, D.; Mayer, A.; Loeys, T. Giving Dyadic Data Analysis Away: A User-Friendly App for Actor-Partner Interdependence Models. Pers. Relatsh. 2018, 25, 103–119. [Google Scholar] [CrossRef] [Green Version]
- Moorman, S.M. Dyadic perspectives on marital quality and loneliness in later life. J. Soc. Pers. Relatsh. 2015, 33, 600–618. [Google Scholar] [CrossRef]
- Dahlberg, L.; McKee, K.J.; Frank, A.; Naseer, M. A systematic review of longitudinal risk factors for loneliness in older adults. Aging Ment. Health 2022, 26, 225–249. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.; Jung, S.Y. Marital Satisfaction and Depressive Symptoms Among Korean Couples With Young Children: Dyadic Autoregressive Cross-Lagged Modeling. Fam. Relat. 2021, 70, 1384–1398. [Google Scholar] [CrossRef]
- Dekel, R.; Vilchinsky, N.; Liberman, G.; Leibowitz, M.; Khaskia, A.; Mosseri, M. Marital satisfaction and depression among couples following men’s acute coronary syndrome: Testing dyadic dynamics in a longitudinal design. Br. J. Health Psychol. 2014, 19, 347–362. [Google Scholar] [CrossRef]
- Morrish, N.; Medina-Lara, A. Does unemployment lead to greater levels of loneliness? A systematic review. Soc. Sci. Med. 2021, 287, 114339. [Google Scholar] [CrossRef]
- Kim, M.-H.; Do, Y.K. Effect of Husbands’ Employment Status on Their Wives’ Subjective Well-being in Korea. J. Marriage Fam. 2013, 75, 288–299. [Google Scholar] [CrossRef]
- Voßemer, J.; Baranowska, A. Partner’s Unemployment and Well-Being: The Mediating Role of Relationship Quality and Stability; CEDAR Working Papers; Umeå University: Umeå, Sweden, 2020. [Google Scholar]
- Esche, F. Is the problem mine, yours, or ours? The impact of unemployment on couples’ life satisfaction and specific domain satisfaction. Adv. Life Course Res. 2020, 46, 100354. [Google Scholar] [CrossRef]
- Inanc, H. Unemployment, Temporary Work, and Subjective Well-Being: The Gendered Effect of Spousal Labor Market Insecurity. Am. Sociol. Rev. 2018, 83, 536–566. [Google Scholar] [CrossRef]
- Leinonen, T.; Chandola, T.; Laaksonen, M.; Martikainen, P. Socio-economic differences in retirement timing and participation in post-retirement employment in a context of a flexible pension age. Ageing Soc. 2018, 40, 348–368. [Google Scholar] [CrossRef]
- Sampat, K.; Dey, N. Inadequate Pensions Leave India’s Elderly No Choice but to Work; India Spend: Mumbai, India, 2017. [Google Scholar]
- Dhillon, P.; Ladusingh, L. Economic activity in post retirement life in India. Asia-Pac. Popul. J. 2011, 26, 55–71. [Google Scholar] [CrossRef]
- Burholt, V.; Windle, G.; Morgan, D.J.; Team, C.W. A Social Model of Loneliness: The Roles of Disability, Social Resources, and Cognitive Impairment. Gerontologist 2017, 57, 1020–1030. [Google Scholar] [CrossRef] [Green Version]
- Yin, J.; Lassale, C.; Steptoe, A.; Cadar, D. Exploring the bidirectional associations between loneliness and cognitive functioning over 10 years: The English longitudinal study of ageing. Int. J. Epidemiol. 2019, 48, 1937–1948. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zülke, A.E.; Luppa, M.; Röhr, S.; Weißenborn, M.; Bauer, A.; Samos, F.-A.Z.; Kühne, F.; Zöllinger, I.; Döhring, J.; Brettschneider, C.; et al. Association of mental demands in the workplace with cognitive function in older adults at increased risk for dementia. BMC Geriatr. 2021, 21, 688. [Google Scholar] [CrossRef] [PubMed]
- Berkman, L.F.; Sekher, T.V.; Capistrant, B. Social Networks, Family, and Care Giving Among Older Adults in India.; National Academies Press (US): Washington, DC, USA, 2012. [Google Scholar]
- Lykes, V.A.; Kemmelmeier, M. What Predicts Loneliness? Cultural Difference Between Individualistic and Collectivistic Societies in Europe. J. Cross-Cult. Psychol. 2014, 45, 468–490. [Google Scholar] [CrossRef]
- McDaid, D.; Qualter, P.; Arsenault, L.; Barreto, M.; Fett, A.-K.; Hey, J.; Johnson, S.; Kharicha, K.; Matthew, T.; Pearce, E.; et al. Tackling Loneliness Evidence Review; Department for Digital, Culture, Media and Sport: London, UK, 2022.
- Umberson, D.; Williams, K.; Powers, D.A.; Liu, H.; Needham, B. You make me sick: Marital quality and health over the life course. J. Health Soc. Behav. 2006, 47, 1–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lubben, J.E. Assessing social networks among elderly populations. Fam. Community Health 1988, 11, 42–52. [Google Scholar] [CrossRef]
| Husbands | Wives | |
|---|---|---|
| Age in years–Mean (SD) | 57.9 (10.6) | 51.7 (10.2) |
| Any chronic condition–n (%) | 126 (31.7) | 117 (29.4) |
| Total recall score–Mean (SD) | 9.4 (3.3) | 9.2 (3.4) |
| Verbal fluency–Mean (SD) | 10.4 (5.7) | 9.5 (4.8) |
| Having at least one functional limitation–n (%) | 39 (9.8%) | 42 (10.6%) |
| Depressive symptoms–Mean (SD) | 3.0 (2.8) | 3.1 (2.9) |
| Loneliness–Mean (SD) | 3.8 (1.2) | 3.8 (1.2) |
| Contact with friends–n (%) | 214 (53.8%) | 129 (32.4%) |
| Currently in work–n (%) | 105 (26.4%) | 41 (10.3%) |
| Actor’s Loneliness | Partner’s Loneliness | |
|---|---|---|
| Total recall score | 0.025 (0.013) | 0.021 (0.013) |
| Verbal fluency | −0.007 (0.009) | 0.008 (0.009) |
| Having at least one functional limitation | 0.111 (0.068) | 0.003 (0.067) |
| Depressive symptoms | 0.122 (0.014) ** | 0.071 (0.014) ** |
| Contact with friends | −0.029 (0.041) | −0.043 (0.041) |
| Currently in work | −0.057 (0.052) | −0.111 (0.050) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shankar, A.; Kidd, T. Loneliness in Older Indian Dyads. Int. J. Environ. Res. Public Health 2022, 19, 5302. https://doi.org/10.3390/ijerph19095302
Shankar A, Kidd T. Loneliness in Older Indian Dyads. International Journal of Environmental Research and Public Health. 2022; 19(9):5302. https://doi.org/10.3390/ijerph19095302
Chicago/Turabian StyleShankar, Aparna, and Tara Kidd. 2022. "Loneliness in Older Indian Dyads" International Journal of Environmental Research and Public Health 19, no. 9: 5302. https://doi.org/10.3390/ijerph19095302
APA StyleShankar, A., & Kidd, T. (2022). Loneliness in Older Indian Dyads. International Journal of Environmental Research and Public Health, 19(9), 5302. https://doi.org/10.3390/ijerph19095302






