Type of Findings Generated by the Occupational Therapy Workforce Research Worldwide: Scoping Review and Content Analysis
Abstract
:1. Introduction
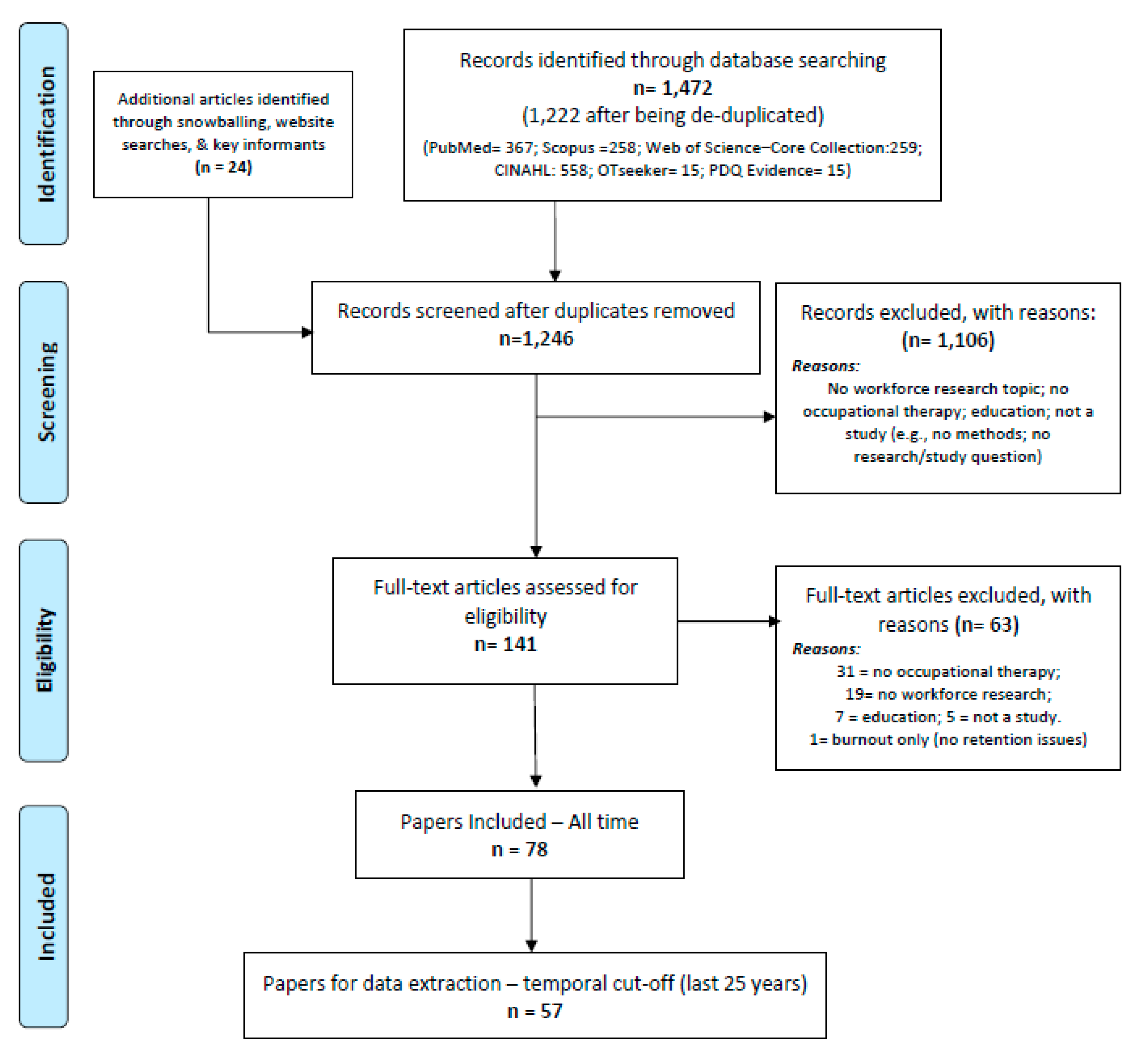
2. Materials and Methods
2.1. Searches
2.2. Eligibility Criteria
2.3. Data Extraction
2.4. Data Synthesis
3. Results
3.1. Attractiveness and Retention
3.1.1. Reasons to Choose and Remain in a Career
3.1.2. Determinants of Attrition
3.1.3. Intention to Leave Mental Health Practice
3.1.4. Attractiveness of Mental Health as a Practice Area
3.1.5. Retention in Rural Areas
3.2. Supply, Demand, and Distribution
3.2.1. Supply and Demand, including Forecasts
3.2.2. Supply and Distribution per Country Region and Sector
3.2.3. Supply, Utilization, and Unmet Demand by Service Type
3.3. Staffing Levels—Upscaling and Monitoring
3.4. Competencies, Regulation, and Continuous Education Requirements
3.5. Human Resources Management—Recruitment, Leadership, and Workload
3.6. International Mobility—And Integration of Those Internationally Trained
3.7. Career Transitions—To Supervisor Roles, Return to the Career
3.8. Salary Levels
3.9. Training of New Graduates
3.10. Racial/Ethnic Representation
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Federation of Occupational Therapists. Occupational Therapy Human Resources; World Federation of Occupational Therapists: Geneva, Switzerland, 2021. [Google Scholar]
- World Federation of Occupational Therapists. Defintions of Occupational Therapy from Member Organizations; Online; World Federation of Occupational Therapists: Geneva, Switzerland, 2013. [Google Scholar]
- Reitz, S.M.; Scaffa, M.E.; Dorsey, J. Occupational Therapy in the Promotion of Health and Well-Being. Am. J. Occup. Ther. 2020, 74, 7403420010p1–7403420010p14. [Google Scholar] [PubMed]
- World Federation of Occupational Therapists. Occupational Therapy and Human Rights (Revised); WFOT: Geneva, Switzerland, 2019. [Google Scholar]
- Serrata Malfitano, A.P.; Gomes da Mota de Souza, R.; Esquerdo Lopes, R. Occupational Justice and Its Related Concepts: An Historical and Thematic Scoping Review. OTJR Occup. Particip. Health 2016, 36, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Bailliard, A.L.; Dallman, A.R.; Carroll, A.; Lee, B.D.; Szendrey, S. Doing Occupational Justice: A Central Dimension of Everyday Occupational Therapy Practice. Can. J. Occup. Therapy. Rev. Can. D’ergotherapie 2020, 87, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Kuhlmann, E.; Batenburg, R.; Wismar, M.; Dussault, G.; Maier, C.B.; Glinos, I.A.; Azzopardi-Muscat, N.; Bond, C.; Burau, V.; Correia, T.; et al. A call for action to establish a research agenda for building a future health workforce in Europe. Health Res. Policy Syst. 2018, 16, 52. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.; Buchan, J.; Cometto, G.; David, B.; Dussault, G.; Fogstad, H.; Fronteira, I.; Lozano, R.; Nyonator, F.; Pablos-Méndez, A.; et al. Human resources for health and universal health coverage: Fostering equity and effective coverage. Bull. World Health Organ. 2013, 91, 853–863. [Google Scholar] [CrossRef] [PubMed]
- George, A.S.; Campbell, J.; Ghaffar, A. Advancing the science behind human resources for health: Highlights from the Health Policy and Systems Research Reader on Human Resources for Health. Health Res. Policy Syst. 2018, 16, 80. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J. Towards universal health coverage: A health workforce fit for purpose and practice. Bull. World Health Organ. 2013, 91, 887–888. [Google Scholar] [CrossRef]
- Jesus, T.S.; Castellini, G.; Gianola, S. Global health workforce research: Comparative analyses of the scientific publication trends in PubMed. Int. J. Health Plan. Manag. 2021. [Google Scholar] [CrossRef] [PubMed]
- Kobbero, T.K.; Lynch, C.H.; Boniface, G.; Forwell, S.J. Occupational therapy private practice workforce: Issues in the 21st century. Can. J. Occup. Therapy. Rev. Can. D’ergotherapie 2018, 85, 58–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jesus, T.S.; Landry, M.D.; Dussault, G.; Fronteira, I. Human resources for health (and rehabilitation): Six Rehab-Workforce Challenges for the century. Hum. Resour Health 2017, 15, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jesus, T.S.; Landry, M.D.; Hoenig, H.; Dussault, G.; Koh, G.C.; Fronteira, I. Is Physical Rehabilitation Need Associated With the Rehabilitation Workforce Supply? An Ecological Study Across 35 High-Income Countries. Int. J. Health Policy Manag. 2022, 11, 434–442. [Google Scholar] [CrossRef]
- Ledgerd, R.; WFOT. WFOT report: WFOT human resources project 2018 and 2020. WFOT Bull. 2020, 76, 69–74. [Google Scholar] [CrossRef]
- Buchan, J.; Campbell, J.; McCarthy, C. Research to support evidence-informed decisions on optimizing the contributions of nursing and midwifery workforces. Hum. Resour. Health 2020, 18, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jesus, T.S.; von Zweck, C.; Mani, K.; Kamalakannan, S.; Bhattacharjya, S.; Ledgerd, R. Mapping the occupational therapy workforce research worldwide: Study protocol for a scoping review. Work 2021, 70, 677–686. [Google Scholar] [CrossRef]
- Jesus, T.; Mani, K.; von Zweck, C.; Bhattacharjya, S.; Kamalakannan, S.; Ledgerd, R.; WFOT. The global status of occupational therapy workforce research worldwide: Scoping review. 2022; under review. [Google Scholar]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colquhoun, H.L.; Levac, D.; O’Brien, K.K.; Straus, S.; Tricco, A.C.; Perrier, L.; Kastner, M.; Moher, D. Scoping reviews: Time for clarity in definition, methods, and reporting. J. Clin. Epidemiol. 2014, 67, 1291–1294. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Implement. 2021, 19, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Daudt, H.M.; van Mossel, C.; Scott, S.J. Enhancing the scoping study methodology: A large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med. Res. Methodol. 2013, 13, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- McGowan, J.; Sampson, M.; Salzwedel, D.M.; Cogo, E.; Foerster, V.; Lefebvre, C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J. Clin. Epidemiol. 2016, 75, 40–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Global Strategy on Human Resources for Health: Workforce 2030; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Colquhoun, H.L.; Jesus, T.S.; O’Brien, K.K.; Tricco, A.C.; Chui, A.; Zarin, W.; Lillie, E.; Hitzig, S.L.; Seaton, S.; Engel, L.; et al. Scoping Review on Rehabilitation Scoping Reviews. Arch. Phys. Med. Rehabil. 2020, 101, 1462–1469. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for conducting systematic scoping reviews. Int. J. Evid.-Based Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsieh, H.F.; Shannon, S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef] [PubMed]
- Katz, N.; Izhaky, S.G.; Dror, Y.F. Reasons for choosing a career and workplace among occupational therapists and speech language pathologists. Work 2013, 45, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Randolph, D.S. Predicting the effect of extrinsic and intrinsic job satisfaction factors on recruitment and retention of rehabilitation professionals. J. Healthc. Manag. 2005, 50, 49–60. [Google Scholar] [CrossRef] [Green Version]
- Porter, S.; Lexén, A. Swedish occupational therapists’ considerations for leaving their profession: Outcomes from a national survey. Scand. J. Occup. Ther. 2022, 29, 79–88. [Google Scholar] [CrossRef]
- Chun, B.Y.; Song, C.S. A moderated mediation analysis of occupational stress, presenteeism, and turnover intention among occupational therapists in Korea. J. Occup. Health 2020, 62, e12153. [Google Scholar] [CrossRef]
- Meade, I.; Brown, G.T.; Trevan-Hawke, J. Female and male occupational therapists: A comparison of their job satisfaction level. Aust. Occup. Ther. J. 2005, 52, 136–148. [Google Scholar] [CrossRef]
- Brown, G.T. Male Occupational Therapists in Canada: A Demographic Profile. Br. J. Occup. Ther. 1998, 61, 561–567. [Google Scholar] [CrossRef]
- Scanlan, J.N.; Still, M. Relationships between burnout, turnover intention, job satisfaction, job demands and job resources for mental health personnel in an Australian mental health service. BMC Health Serv. Res. 2019, 19, 62. [Google Scholar] [CrossRef] [PubMed]
- Scanlan, J.N.; Meredith, P.; Poulsen, A.A. Enhancing retention of occupational therapists working in mental health: Relationships between wellbeing at work and turnover intention. Aust. Occup. Ther. J. 2013, 60, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Scanlan, J.N.; Still, M. Job satisfaction, burnout and turnover intention in occupational therapists working in mental health. Aust. Occup. Ther. J. 2013, 60, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Scanlan, J.N.; Still, M.; Stewart, K.; Croaker, J. Recruitment and retention issues for occupational therapists in mental health: Balancing the pull and the push. Aust. Occup. Ther. J. 2010, 57, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Ceramidas, D.; de Zita, C.F.; Eklund, M.; Kirsh, B. The 2009 world team of mental health occupational therapists: A resilient and dedicated workforce. WFOT Bull. 2009, 60, 9–17. [Google Scholar] [CrossRef]
- Rodger, S.; Thomas, Y.; Holley, S.; Springfield, E.; Edwards, A.; Broadbridge, J.; Greber, C.; McBryde, C.; Banks, R.; Hawkins, R. Increasing the occupational therapy mental health workforce through innovative practice education: A pilot project. Aust. Occup. Ther. J. 2009, 56, 409–417. [Google Scholar] [CrossRef]
- Hunter, E.; Nicol, M. Systematic review: Evidence of the value of continuing professional development to enhance recruitment and retention of occupational therapists in mental health. Br. J. Occup. Ther. 2002, 65, 207–215. [Google Scholar] [CrossRef]
- Smith, T.; Cooper, R.; Brown, L.; Hemmings, R.; Greaves, J. Profile of the rural allied health workforce in northern New South Wales and comparison with previous studies. Aust. J. Rural. Health 2008, 16, 156–163. [Google Scholar] [CrossRef] [PubMed]
- McAuliffe, T.; Barnett, F. Factors influencing occupational therapy students’ perceptions of rural and remote practice. Rural. Remote Health 2009, 9, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Mills, A.; Millsteed, J. Retention: An unresolved workforce issue affecting rural occupational therapy services. Aust. Occup. Ther. J. 2002, 49, 170–181. [Google Scholar] [CrossRef]
- Merritt, J.; Perkins, D.; Boreland, F. Regional and remote occupational therapy: A preliminary exploration of private occupational therapy practice. Aust. Occup. Ther. J. 2013, 60, 276–287. [Google Scholar] [CrossRef] [PubMed]
- McAuliffe, T.; Barnett, F. Perceptions towards rural and remote practice: A study of final year occupational therapy students studying in a regional university in Australia. Aust. Occup. Ther. J. 2010, 57, 293–300. [Google Scholar] [CrossRef]
- HRSA Health Workforce. Allied Health Workforce Projections, 2016–2030:Occupational and Physical Therapists; HRSA Health Workforce: Rockville, MD, USA, 2016. [Google Scholar]
- Lin, V.; Zhang, X.; Dixon, P. Occupational Therapy Workforce in the United States: Forecasting Nationwide Shortages. PM&R J. Inj. Funct. Rehabil. 2015, 7, 946–954. [Google Scholar]
- Powell, J.M.; Kanny, E.M.; Ciol, M.A. State of the occupational therapy workforce: Results of a national study. Am. J. Occup. Ther. 2008, 62, 97–105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Powell, J.M.; Griffith, S.L.; Kanny, E.M. Occupational therapy workforce needs: A model for demand-based studies. Am. J. Occup. Ther. 2005, 59, 467–474. [Google Scholar] [CrossRef] [Green Version]
- Wilson, R.D.; Lewis, S.A.; Murray, P.K. Trends in the Rehabilitation Therapist Workforce in Underserved Areas: 1980–2000. J. Rural Health 2009, 25, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Millsteed, J. Issues affecting Australia’s rural occupational therapy workforce. Aust. J Rural. Health 2000, 8, 73–76. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, M.L.; do Pinho, R.J.; Malfitano, A.P.S. Occupational therapists inclusion in the ‘Sistema Unico de Assistencia Social’ (Brazilian Social Police System): Official records on our route. Braz. J. Occup. Ther. 2019, 27, 828–842. [Google Scholar]
- Ned, L.; Tiwari, R.; Buchanan, H.; Van Niekerk, L.; Sherry, K.; Chikte, U. Changing demographic trends among South African occupational therapists: 2002 to 2018. Hum. Resour Health 2020, 18, 22. [Google Scholar] [CrossRef] [PubMed]
- Mueller, E.; Arthur, P.; Ivy, M.; Pryor, L.; Armstead, A.; Li, C.Y. Addressing the Gap: Occupational Therapy in Hospice Care. Occup. Ther. Health Care 2021, 35, 125–137. [Google Scholar] [CrossRef] [PubMed]
- McBain, R.K.; Kareddy, V.; Cantor, J.H.; Stein, B.D.; Yu, H. Systematic Review: United States Workforce for Autism-Related Child Healthcare Services. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 113–139. [Google Scholar] [CrossRef] [PubMed]
- De Boer, M.E.; Leemrijse, C.J.; Van Den Ende, C.H.; Ribbe, M.W.; Dekker, J. The availability of allied health care in nursing homes. Disabil. Rehabil. 2007, 29, 665–670. [Google Scholar] [CrossRef] [PubMed]
- Josi, R.; De Pietro, C. Skill mix in Swiss primary care group practices—A nationwide online survey. BMC Fam. Pract. 2019, 20, 39. [Google Scholar] [CrossRef] [PubMed]
- Al-Senani, F.; Salawati, M.; AlJohani, M.; Cuche, M.; Ravest, V.S.; Eggington, S. Workforce requirements for comprehensive ischaemic stroke care in a developing country: The case of Saudi Arabia. Hum. Resour. Health 2019, 17, 90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McHugh, G.; Swain, I.D. A comparison between reported therapy staffing levels and the department of health therapy staffing guidelines for stroke rehabilitation: A national survey. BMC Health Serv. Res. 2014, 14, 216. [Google Scholar] [CrossRef] [PubMed]
- McGarry, B.E.; White, E.M.; Resnik, L.J.; Rahman, M.; Grabowski, D.C. Medicare’s New Patient Driven Payment Model Resulted In Reductions In Therapy Staffing In Skilled Nursing Facilities. Health Aff. 2021, 40, 392–399. [Google Scholar] [CrossRef]
- Prusynski, R.A.; Leland, N.E.; Frogner, B.K.; Leibbrand, C.; Mroz, T.M. Therapy Staffing in Skilled Nursing Facilities Declined after Implementation of the Patient-Driven Payment Model. J. Am. Med. Dir. Assoc. 2021, 22, 2201–2206. [Google Scholar] [CrossRef] [PubMed]
- Maass, R.; Bonsaksen, T.; Gramstad, A.; Sveen, U.; Stigen, L.; Arntzen, C.; Horghagen, S. Factors Associated with the Establishment of New Occupational Therapist Positions in Norwegian Municipalities after the Coordination Reform. Health Serv. Insights 2021, 14, 1178632921994908. [Google Scholar] [CrossRef] [PubMed]
- Fields, S.M.; Unsworth, C.A.; Harreveld, B. The revision of competency standards for occupational therapy driver assessors in Australia: A mixed methods approach. Aust. Occup. Ther. J. 2021, 68, 257–271. [Google Scholar] [CrossRef] [PubMed]
- Rodger, S.; Clark, M.; Banks, R.; O’Brien, M.; Martinez, K. A national evaluation of the Australian Occupational Therapy Competency Standards (1994): A multistakeholder perspective. Aust. Occup. Ther. J. 2009, 56, 384–392. [Google Scholar] [CrossRef] [PubMed]
- Hall, S.R.; Crifasi, K.A.; Marinelli, C.M.; Yuen, H.K. Continuing education requirements among State Occupational Therapy Regulatory Boards in the United States of America. J. Educ. Eval. Health Prof. 2016, 13, 37. [Google Scholar] [CrossRef]
- White, E. Continuing professional development: The impact of the College of Occupational Therapists’ standard on dedicated time. Br. J. Occup. Ther. 2005, 68, 196–201. [Google Scholar] [CrossRef] [Green Version]
- Vachon, B.; Foucault, M.L.; Giguère, C.; Rochette, A.; Thomas, A.; Morel, M. Factors Influencing Acceptability and Perceived Impacts of a Mandatory ePortfolio Implemented by an Occupational Therapy Regulatory Organization. J. Contin. Educ. Health Prof. 2018, 38, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Mulholland, S.; Derdall, M. Exploring recruitment strategies to hire occupational therapists. Can. J. Occup. Therapy. Rev. Can. D’ergotherapie 2005, 72, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, M.; Rugg, S. Advertising for and recruiting basic grade occupational therapists in the United Kingdom. Br. J. Occup. Ther. 2000, 63, 583–590. [Google Scholar] [CrossRef]
- Hitch, D.; Lhuede, K.; Giles, S.; Low, R.; Cranwell, K.; Stefaniak, R. Perceptions of leadership styles in occupational therapy practice. Leadersh. Health Serv. 2020, 33, 295–306. [Google Scholar] [CrossRef]
- Summers, B.E.; Laver, K.E.; Nicks, R.J.; Lannin, N.A. What factors influence time-use of occupational therapists in the workplace? A systematic review. Aust. Occup. Ther. J. 2018, 65, 225–237. [Google Scholar] [CrossRef] [PubMed]
- Pittman, P.; Frogner, B.; Bass, E.; Dunham, C. International recruitment of allied health professionals to the United States: Piecing together the picture with imperfect data. J. Allied Health 2014, 43, 79–87. [Google Scholar] [PubMed]
- Dhillon, S.; Dix, L.; Baptiste, S.; Moll, S.; Stroinska, M.; Solomon, P. Internationally educated occupational therapists transitioning to practice in Canada: A qualitative study. Aust. Occup. Ther. J. 2019, 66, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Mulholland, S.J.; Dietrich, T.A.; Bressler, S.I.; Corbett, K.G. Exploring the integration of internationally educated occupational therapists into the workforce. Can. J. Occup. Therapy. Rev. Can. D’ergotherapie 2013, 80, 8–18. [Google Scholar] [CrossRef] [PubMed]
- Nelson, H.; Giles, S.; McInnes, H.; Hitch, D. Occupational therapists’ experiences of career progression following promotion. Aust. Occup. Ther. J. 2015, 62, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Dodds, K.; Herkt, J. Exploring transition back to occupational therapy practice following a career break. N. Z. J. Occup. Ther. 2013, 60, 5–12. [Google Scholar]
- Mani, K.; Sundar, S. Occupational Therapy Workforce in India: A National Survey. Indian J. Occup. Ther. 2019, 51, 45–51. [Google Scholar] [CrossRef]
- Mroz, T.M.; Dahal, A.; Prusynski, R.; Skillman, S.M.; Frogner, B.K. Variation in Employment of Therapy Assistants in Skilled Nursing Facilities Based on Organizational Factors. Med. Care Res. Rev. 2021, 78 (Suppl. 1), 40S–46S. [Google Scholar] [CrossRef] [PubMed]
- Haddad, A.E.; Morita, M.C.; Pierantoni, C.R.; Brenelli, S.L.; Passarella, T.; Campos, F.E. Undergraduate programs for health professionals in Brazil: An analysis from 1991 to 2008. Rev. Saúde Pública 2010, 44, 385–393. [Google Scholar]
- Agho, A.O.; John, E.B. Occupational therapy and physiotherapy education and workforce in Anglophone sub-Saharan Africa countries. Hum. Resour. Health 2017, 15, 37. [Google Scholar] [CrossRef] [PubMed]
- Salsberg, E.; Richwine, C.; Westergaard, S.; Portela Martinez, M.; Oyeyemi, T.; Vichare, A.; Chen, C.P. Estimation and Comparison of Current and Future Racial/Ethnic Representation in the US Health Care Workforce. JAMA Netw. Open 2021, 4, e213789. [Google Scholar] [CrossRef] [PubMed]
- Prust, M.L.; Kamanga, A.; Ngosa, L.; McKay, C.; Muzongwe, C.M.; Mukubani, M.T.; Chihinga, R.; Misapa, R.; van den Broek, J.W.; Wilmink, N. Assessment of interventions to attract and retain health workers in rural Zambia: A discrete choice experiment. Hum. Resour. Health 2019, 17, 26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Law, T.J.; Subhedar, S.; Bulamba, F.; O’Hara, N.N.; Nabukenya, M.T.; Sendagire, C.; Hewitt-Smith, A.; Lipnick, M.S.; Tumukunde, J. Factors affecting job choice among physician anesthesia providers in Uganda: A survey of income composition, discrete choice experiment, and implications for the decision to work rurally. Hum. Resour. Health 2021, 19, 93. [Google Scholar] [CrossRef]
- Lamba, S.; Arora, N.; Keraga, D.W.; Kiflie, A.; Jembere, B.M.; Berhanu, D.; Dubale, M.; Marchant, T.; Schellenberg, J.; Umar, N.; et al. Stated job preferences of three health worker cadres in Ethiopia: A discrete choice experiment. Health Policy Plan. 2021, 36, 1418–1427. [Google Scholar] [CrossRef] [PubMed]
- Stobbe, E.J.; Groenewegen, P.P.; Schäfer, W. Job satisfaction of general practitioners: A cross-sectional survey in 34 countries. Hum. Resour. Health 2021, 19, 57. [Google Scholar] [CrossRef]
- Jesus, T.S.; Koh, G.; Landry, M.; Ong, P.H.; Lopes, A.M.; Green, P.L.; Hoenig, H. Finding the “Right-Size” Physical Therapy Workforce: International Perspective Across 4 Countries. Phys. Ther. 2016, 96, 1597–1609. [Google Scholar] [CrossRef] [PubMed]
- Wakerman, J.; Humphreys, J.; Russell, D.; Guthridge, S.; Bourke, L.; Dunbar, T.; Zhao, Y.; Ramjan, M.; Murakami-Gold, L.; Jones, M.P. Remote health workforce turnover and retention: What are the policy and practice priorities? Hum. Resour. Health 2019, 17, 99. [Google Scholar] [CrossRef] [PubMed]
- Russell, D.; Mathew, S.; Fitts, M.; Liddle, Z.; Murakami-Gold, L.; Campbell, N.; Ramjan, M.; Zhao, Y.; Hines, S.; Humphreys, J.S.; et al. Interventions for health workforce retention in rural and remote areas: A systematic review. Hum. Resour. Health 2021, 19, 103. [Google Scholar] [CrossRef] [PubMed]
- Gailey, S.; Bruckner, T.A.; Lin, T.K.; Liu, J.X.; Alluhidan, M.; Alghaith, T.; Alghodaier, H.; Tashkandi, N.; Herbst, C.H.; Hamza, M.M.; et al. A needs-based methodology to project physicians and nurses to 2030: The case of the Kingdom of Saudi Arabia. Hum. Resour. Health 2021, 19, 55. [Google Scholar] [CrossRef] [PubMed]
- Magnago, C.; Pierantoni, C.R. Situational analysis and reflections on the introduction of advanced practice nurses in Brazilian primary healthcare. Hum. Resour. Health 2021, 19, 90. [Google Scholar] [CrossRef] [PubMed]
- Nigenda, G.; Serván-Mori, E.; Fuentes-Rivera, E.; Aristizabal, P.; Zárate-Grajales, R.A. Performance of the Mexican nursing labor market: A repeated cross-sectional study, 2005–2019. Hum. Resour. Health 2022, 20, 24. [Google Scholar] [CrossRef] [PubMed]
- Russo, G.; Fronteira, I.; Jesus, T.S.; Buchan, J. Understanding nurses’ dual practice: A scoping review of what we know and what we still need to ask on nurses holding multiple jobs. Hum. Resour. Health 2018, 16, 14. [Google Scholar] [CrossRef] [PubMed]
- Deussom, R.; Mwarey, D.; Bayu, M.; Abdullah, S.S.; Marcus, R. Systematic review of performance-enhancing health worker supervision approaches in low- and middle-income countries. Hum. Resour. Health 2022, 20, 2. [Google Scholar] [CrossRef] [PubMed]
- Rowe, S.Y.; Ross-Degnan, D.; Peters, D.H.; Holloway, K.A.; Rowe, A.K. The effectiveness of supervision strategies to improve health care provider practices in low- and middle-income countries: Secondary analysis of a systematic review. Hum. Resour. Health 2022, 20, 1. [Google Scholar] [CrossRef] [PubMed]
- Nove, A.; Ten Hoope-Bender, P.; Boyce, M.; Bar-Zeev, S.; de Bernis, L.; Lal, G.; Matthews, Z.; Mekuria, M.; Homer, C.S.E. The State of the World’s Midwifery 2021 report: Findings to drive global policy and practice. Hum. Resour. Health 2021, 19, 146. [Google Scholar] [CrossRef]
- Ajuebor, O.; McCarthy, C.; Li, Y.; Al-Blooshi, S.M.; Makhanya, N.; Cometto, G. Are the Global Strategic Directions for Strengthening Nursing and Midwifery 2016-2020 being implemented in countries? Findings from a cross-sectional analysis. Hum. Resour. Health 2019, 17, 54. [Google Scholar] [CrossRef] [PubMed]
- Fort, A.L.; Deussom, R.; Burlew, R.; Gilroy, K.; Nelson, D. The Human Resources for Health Effort Index: A tool to assess and inform Strategic Health Workforce Investments. Hum. Resour. Health 2017, 15, 47. [Google Scholar] [CrossRef] [PubMed]
- Dubey, S.; Vasa, J.; Zadey, S. Do health policies address the availability, accessibility, acceptability, and quality of human resources for health? Analysis over three decades of National Health Policy of India. Hum. Resour. Health 2021, 19, 139. [Google Scholar] [CrossRef]
- Azzam, M.; Puvirajah, A.; Girard, M.A.; Grymonpre, R.E. Interprofessional education-relevant accreditation standards in Canada: A comparative document analysis. Hum. Resour. Health 2021, 19, 66. [Google Scholar] [CrossRef] [PubMed]
- Aftab, W.; Khan, M.; Rego, S.; Chavan, N.; Rahman-Shepherd, A.; Sharma, I.; Wu, S.; Zeinali, Z.; Hasan, R.; Siddiqi, S. Variations in regulations to control standards for training and licensing of physicians: A multi-country comparison. Hum. Resour. Health 2021, 19, 91. [Google Scholar] [CrossRef] [PubMed]
- Leslie, K.; Moore, J.; Robertson, C.; Bilton, D.; Hirschkorn, K.; Langelier, M.H.; Bourgeault, I.L. Regulating health professional scopes of practice: Comparing institutional arrangements and approaches in the US, Canada, Australia and the UK. Hum. Resour. Health 2021, 19, 15. [Google Scholar] [CrossRef] [PubMed]
- Kunjumen, T.; Okech, M.; Diallo, K.; McQuide, P.; Zapata, T.; Campbell, J. Global experiences in health workforce policy, planning and management using the Workload Indicators of Staffing Need (WISN) method, and way forward. Hum. Resour. Health 2022, 19 (Suppl. 1), 152. [Google Scholar] [CrossRef] [PubMed]
- Stankovic, S.; Santric Milicevic, M. Use of the WISN method to assess the health workforce requirements for the high-volume clinical biochemical laboratories. Hum. Resour. Health 2022, 19 (Suppl. 1), 143. [Google Scholar] [CrossRef] [PubMed]
- Namaganda, G.N.; Whitright, A.; Maniple, E.B. Lessons learned from implementation of the Workload Indicator of Staffing Need (WISN) methodology: An international Delphi study of expert users. Hum. Resour. Health 2022, 19 (Suppl. 1), 138. [Google Scholar] [CrossRef] [PubMed]
- Machado, C.R.; Brasil, D.; Dal Poz, M.R. Application of workload indicators to assess the allocation of orthopedists in a national referral hospital in Brazil. Hum. Resour. Health 2022, 19 (Suppl. 1), 123. [Google Scholar] [CrossRef] [PubMed]
- Orkin, A.M.; Rao, S.; Venugopal, J.; Kithulegoda, N.; Wegier, P.; Ritchie, S.D.; VanderBurgh, D.; Martiniuk, A.; Salamanca-Buentello, F.; Upshur, R. Conceptual framework for task shifting and task sharing: An international Delphi study. Hum. Resour. Health 2021, 19, 61. [Google Scholar] [CrossRef]
- Russo, G.; Silva, T.J.; Gassasse, Z.; Filippon, J.; Rotulo, A.; Kondilis, E. The impact of economic recessions on health workers: A systematic review and best-fit framework synthesis of the evidence from the last 50 years. Health Policy Plan. 2021, 36, 542–551. [Google Scholar] [CrossRef] [PubMed]
| Inclusion Category | Category Type |
|---|---|
| 1 | Workforce supply (e.g., supply of practicing therapists or mapping their profile) |
| 2 | Workforce production (e.g., graduates supply or entry-level requirements) |
| 3 | Workforce needs, demands or supply-need/demand shortages; forecasts |
| 4 | Employment trends (e.g., (un)employment patterns, unfilled vacancies) |
| 5 | Workforce distribution (e.g., per geographies, practice area, public vs. private sectors) |
| 6 | Geographical mobility (e.g., (e/i)migration; internationally trained workers) |
| 7 | Attractiveness and retention (e.g., salaries, incentives, job satisfaction, intention to leave the profession, recruitment determinants) |
| 8 | Staff management and performance (e.g., human resources management, workload management, recruitment practices from managers, staffing and scheduling, burnout associated with performance or productivity) |
| 9 | Regulation and licensing (e.g., continuing education requirements, task-shifting, evaluating the impact of licensing or regulatory changes) |
| 10 | Systems-based or systematic analysis of workforce policies |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jesus, T.S.; Mani, K.; von Zweck, C.; Kamalakannan, S.; Bhattacharjya, S.; Ledgerd, R.; on behalf of the World Federation of Occupational Therapists. Type of Findings Generated by the Occupational Therapy Workforce Research Worldwide: Scoping Review and Content Analysis. Int. J. Environ. Res. Public Health 2022, 19, 5307. https://doi.org/10.3390/ijerph19095307
Jesus TS, Mani K, von Zweck C, Kamalakannan S, Bhattacharjya S, Ledgerd R, on behalf of the World Federation of Occupational Therapists. Type of Findings Generated by the Occupational Therapy Workforce Research Worldwide: Scoping Review and Content Analysis. International Journal of Environmental Research and Public Health. 2022; 19(9):5307. https://doi.org/10.3390/ijerph19095307
Chicago/Turabian StyleJesus, Tiago S., Karthik Mani, Claudia von Zweck, Sureshkumar Kamalakannan, Sutanuka Bhattacharjya, Ritchard Ledgerd, and on behalf of the World Federation of Occupational Therapists. 2022. "Type of Findings Generated by the Occupational Therapy Workforce Research Worldwide: Scoping Review and Content Analysis" International Journal of Environmental Research and Public Health 19, no. 9: 5307. https://doi.org/10.3390/ijerph19095307
APA StyleJesus, T. S., Mani, K., von Zweck, C., Kamalakannan, S., Bhattacharjya, S., Ledgerd, R., & on behalf of the World Federation of Occupational Therapists. (2022). Type of Findings Generated by the Occupational Therapy Workforce Research Worldwide: Scoping Review and Content Analysis. International Journal of Environmental Research and Public Health, 19(9), 5307. https://doi.org/10.3390/ijerph19095307






