Sedentary Behaviour and Its Relationship with Early Vascular Ageing in the General Spanish Population: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Ethical Considerations
2.4. Variables and Measurement Instruments
2.4.1. Measurement of Sedentary Time
2.4.2. Criteria to Define Vascular Ageing
- The vascular ageing index (VAI) [19], calculated from the carotid–femoral pulse wave velocity (cfPWV) and the carotid intima–media thickness (cIMT), with the following formula: VAI = (log (1.09) × 10 cIMT + log (1.14) cfPWV) × 39.1 + 4.76. The participants were ordered in percentiles of VAI, by age and sex, classifying them as: EVA, if VAI ≥ 90th percentile; normal vascular ageing (NVA), if 10th percentile < VAI < 90th percentile; and healthy vascular ageing (HVA), if VAI ≤ 10th percentile.
- The 10th and 90th percentiles of cfPWV, by age, of the reference values published by Boutouyrie P in the European population [41], were used to classify the participants as EVA if cfPWV ≥ 90th percentile; NVA, if 10th percentile < cfPWV < 90th percentile; and HVA, if cfPWV ≤ 10th percentile.
- Coronary age was estimated with the D’Agostino version of the scale of cardiovascular risk (CVR) based on the study of Framingham [42]. Distributing the individuals following the criterion established by Appiah et al. [43], we classified them as EVA if the difference between chronological age and heart age was greater than 5 years, NVA if the difference was 5 years, and HVA if the difference was lower than 5 years.
2.4.3. Measurement of Vascular Injury
2.4.4. Measurement of Arterial Stiffness
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
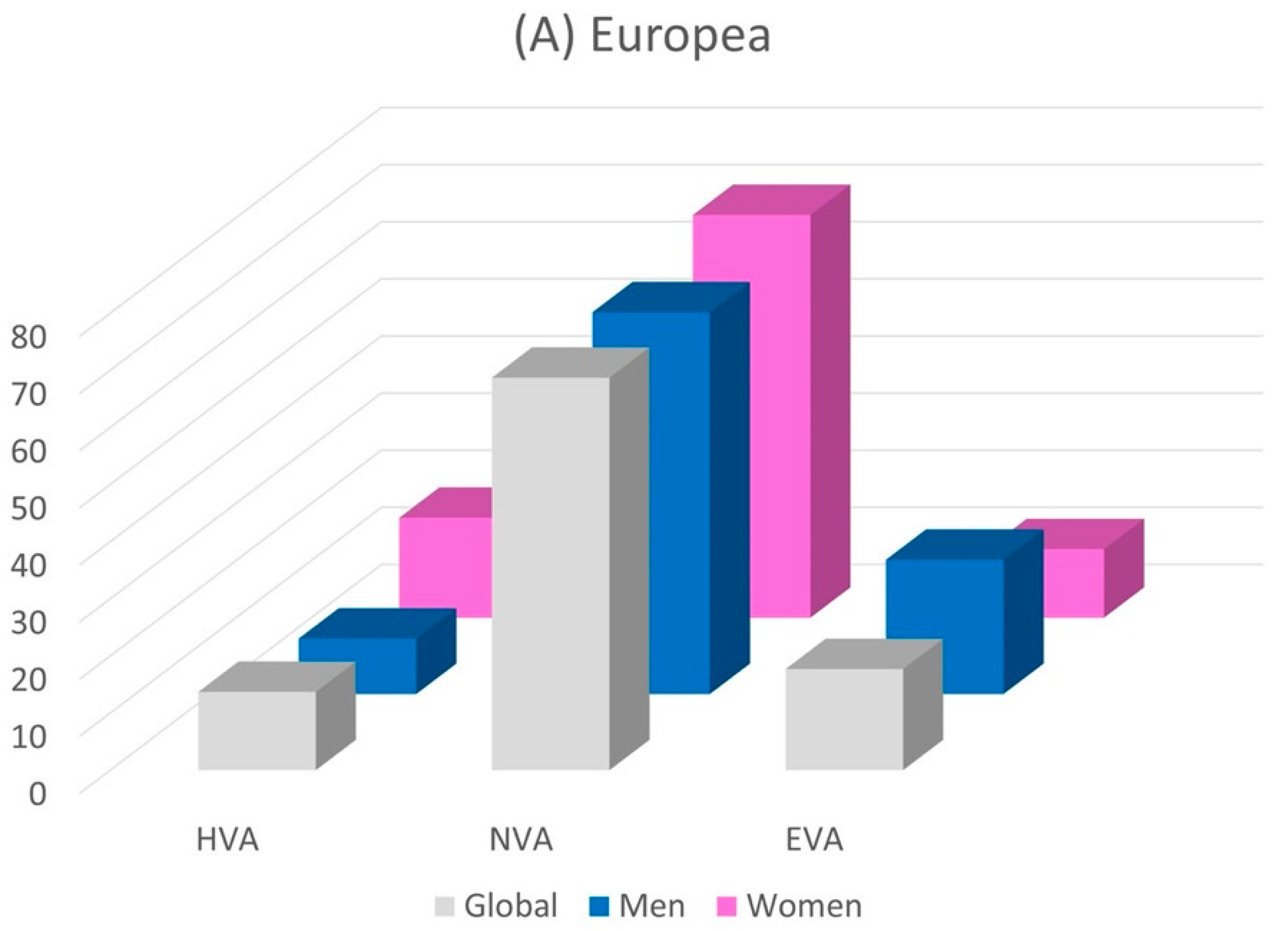
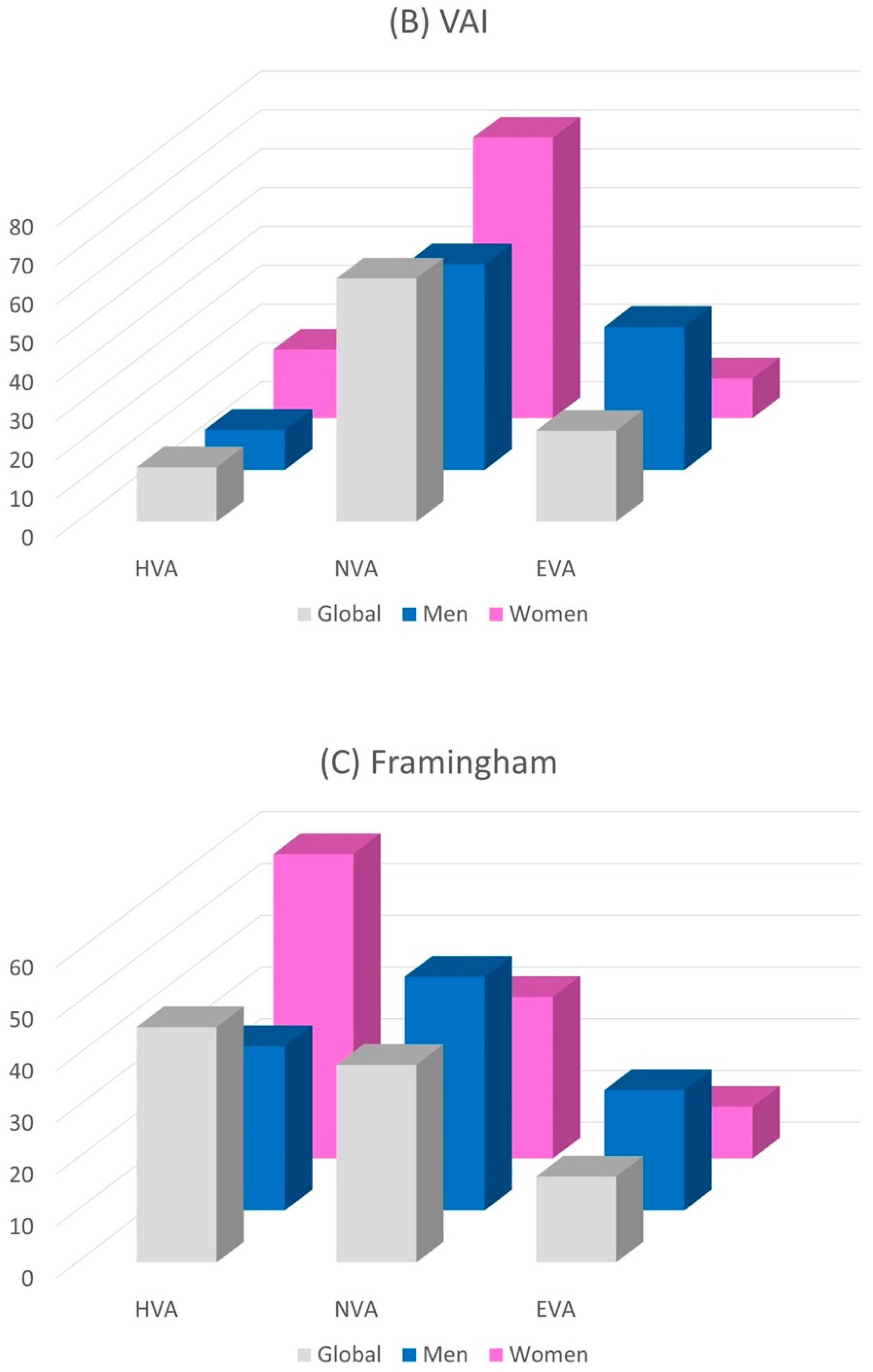
3.2. Relationship between Sedentary Time and Vascular Ageing
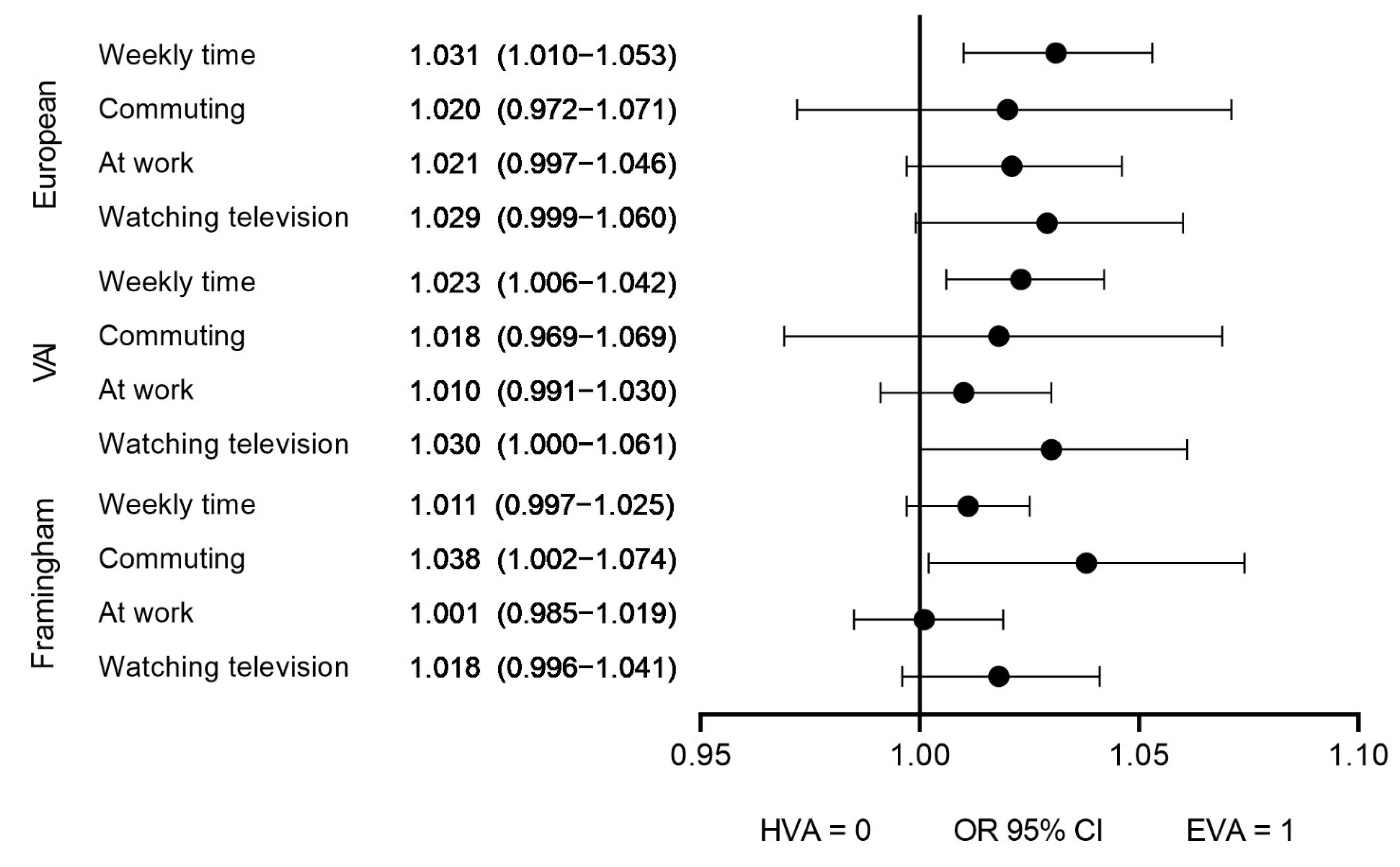
3.3. Association of Sedentary Time with Vascular Ageing
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rodulfo, J.I.A. Sedentary lifestyle a disease from xxi century. Clin. Investig. Arterioscler. 2019, 31, 233–240. [Google Scholar] [CrossRef]
- Lavie, C.J.; Ozemek, C.; Carbone, S.; Katzmarzyk, P.T.; Blair, S.N. Sedentary Behavior, Exercise, and Cardiovascular Health. Circ. Res. 2019, 124, 799–815. [Google Scholar] [CrossRef] [PubMed]
- Owen, N.; Healy, G.N.; Matthews, C.E.; Dunstan, D.W. Too much sitting: The population health science of sedentary behavior. Exerc. Sport Sci. Rev. 2010, 38, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Dunstan, D.W.; Howard, B.; Healy, G.N.; Owen, N. Too much sitting—A health hazard. Diabetes Res. Clin. Pract. 2012, 97, 368–376. [Google Scholar] [CrossRef] [PubMed]
- Gomes, E.S.A.; Ramsey, K.A.; Rojer, A.G.M.; Reijnierse, E.M.; Maier, A.B. The Association of Objectively Measured Physical Activity and Sedentary Behavior with (Instrumental) Activities of Daily Living in Community-Dwelling Older Adults: A Systematic Review. Clin. Interv. Aging 2021, 16, 1877–1915. [Google Scholar] [CrossRef]
- Moraes-Silva, I.C.; Rodrigues, B.; Coelho-Junior, H.J.; Feriani, D.J.; Irigoyen, M.-C. Myocardial Infarction and Exercise Training: Evidence from Basic Science. Adv. Exp. Med. Biol. 2017, 999, 139–153. [Google Scholar] [CrossRef]
- Bellettiere, J.; LaMonte, M.J.; Evenson, K.R.; Rillamas-Sun, E.; Kerr, J.; Lee, I.-M.; Di, C.; Rosenberg, D.E.; Stefanick, M.L.; Buchner, D.M.; et al. Sedentary Behavior and Cardiovascular Disease in Older Women: The Objective Physical Activity and Cardiovascular Health (OPACH) Study. Circulation 2019, 139, 1036–1046. [Google Scholar] [CrossRef]
- Choi, Y.-A.; Lee, J.S.; Park, J.H.; Kim, Y.H. Patterns of physical activity and sedentary behavior and their associated factors among nondisabled stroke survivors. Maturitas 2022, 158, 10–15. [Google Scholar] [CrossRef]
- Jingjie, W.; Yang, L.; Jing, Y.; Ran, L.; Yiqing, X.; Zhou, N. Sedentary time and its association with risk of cardiovascular diseases in adults: An updated systematic review and meta-analysis of observational studies. BMC Public Health 2022, 22, 286. [Google Scholar] [CrossRef]
- Yerramalla, M.S.; van Hees, V.T.; Chen, M.; Fayosse, A.; Chastin, S.F.M.; Sabia, S. Objectively Measured Total Sedentary Time and Pattern of Sedentary Accumulation in Older Adults: Associations With Incident Cardiovascular Disease and All-Cause Mortality. J. Gerontol. A Biol. Sci. Med. Sci. 2022, 77, 842–850. [Google Scholar] [CrossRef]
- Zhuang, Z.; Gao, M.; Yang, R.; Li, N.; Liu, Z.; Cao, W.; Huang, T. Association of physical activity, sedentary behaviours and sleep duration with cardiovascular diseases and lipid profiles: A Mendelian randomization analysis. Lipids Health Dis. 2020, 19, 86. [Google Scholar] [CrossRef] [PubMed]
- Matthews, C.E.; Chen, K.Y.; Freedson, P.S.; Buchowski, M.S.; Beech, B.M.; Pate, R.R.; Troiano, R.P. Amount of Time Spent in Sedentary Behaviors in the United States, 2003–2004. Am. J. Epidemiol. 2008, 167, 875–881. [Google Scholar] [CrossRef] [PubMed]
- Colley, R.C.; Garriguet, D.; Janssen, I.; Craig, C.L.; Clarke, J.; Tremblay, M.S. Physical activity of Canadian adults: Accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep. 2011, 22, 7–14. [Google Scholar] [PubMed]
- Bennie, J.A.; Chau, J.Y.; van der Ploeg, H.P.; Stamatakis, E.; Do, A.; Bauman, A. The prevalence and correlates of sitting in European adults—A comparison of 32 Eurobarometer-participating countries. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 107. [Google Scholar] [CrossRef]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Mâsse, L.C.; Tilert, T.; Mcdowell, M. Physical Activity in the United States Measured by Accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef]
- Strain, T.; Kelly, P.; Mutrie, N.; Fitzsimons, C. Differences by age and sex in the sedentary time of adults in Scotland. J. Sports Sci. 2018, 36, 732–741. [Google Scholar] [CrossRef]
- Laurent, S.; Boutouyrie, P.; Cunha, P.G.; Lacolley, P.; Nilsson, P.M. Concept of Extremes in Vascular Aging. Hypertension 2019, 74, 218–228. [Google Scholar] [CrossRef]
- Nowak, K.L.; Rossman, M.J.; Chonchol, M.; Seals, D.R. Strategies for Achieving Healthy Vascular Aging. Hypertension 2018, 71, 389–402. [Google Scholar] [CrossRef]
- Nilsson Wadström, B.; Fatehali, A.-A.H.; Engström, G.; Nilsson, P.M. A Vascular Aging Index as Independent Predictor of Cardiovascular Events and Total Mortality in an Elderly Urban Population. Angiology 2019, 70, 929–937. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; De Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J. Hypertens. 2018, 36, 1953–2041. [Google Scholar] [CrossRef]
- Tao, B.; Li, Y.; Wang, C.; Luo, X.; Chen, S.; Wang, G.; Yang, P.; Hou, L.; Cui, L.; Wu, S. Influencing factors of supernormal vascular aging in Chinese population. J Hypertens 2022, 40, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Chong, M.S.; Tan, C.N.; Yew, S.; Lim, J.P.; Lim, W.S.; Lieu, P.K. Successful Ageing in Nonagenarians: Bio-psychosocial Factors Determining Successful Ageing in Long-Lived Older Adults. J. Am. Med. Dir. Assoc. 2018, 19, 90–92. [Google Scholar] [CrossRef] [PubMed]
- Seals, D.R.; DeSouza, C.A.; Donato, A.J.; Tanaka, H. Habitual exercise and arterial aging. J. Appl. Physiol. 2008, 105, 1323–1332. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Marcos, M.A.; Recio-Rodríguez, J.I.; Patino-Alonso, M.C.; Martinez-Vizcaino, V.; Martin-Borras, C.; De-La-Cal-Dela-Fuente, A.; Sauras-Llera, I.; Sanchez-Perez, A.; Agudo-Conde, C.; García-Ortiz, L.; et al. Relationship between Physical Activity and Plasma Fibrinogen Concentrations in Adults without Chronic Diseases. PLoS ONE 2014, 9, e87954. [Google Scholar] [CrossRef]
- Seals, D.R.; Jablonski, K.L.; Donato, A.J. Aging and vascular endothelial function in humans. Clin. Sci. 2011, 120, 357–375. [Google Scholar] [CrossRef]
- Andersson, C.; Lyass, A.; Larson, M.G.; Spartano, N.L.; Vita, J.A.; Benjamin, E.J.; Murabito, J.M.; Esliger, D.W.; Blease, S.J.; Hamburg, N.M.; et al. Physical Activity Measured by Accelerometry and its Associations With Cardiac Structure and Vascular Function in Young and Middle-Aged Adults. J. Am. Heart Assoc. 2015, 4, e001528. [Google Scholar] [CrossRef]
- Niiranen, T.J.; Lyass, A.; Larson, M.G.; Hamburg, N.M.; Benjamin, E.J.; Mitchell, G.F.; Vasan, R.S. Prevalence, Correlates, and Prognosis of Healthy Vascular Aging in a Western Community-Dwelling Cohort: The Framingham Heart Study. Hypertension 2017, 70, 267–274. [Google Scholar] [CrossRef]
- Gomez-Sanchez, M.; Gomez-Sanchez, L.; Patino-Alonso, M.C.; Cunha, P.; Recio-Rodriguez, J.I.; Alonso-Dominguez, R.; Sanchez-Aguadero, N.; Rodriguez-Sanchez, E.; Maderuelo-Fernandez, J.A.; Garcia-Ortiz, L.; et al. Vascular aging and its relationship with lifestyles and other risk factors in the general Spanish population: Early Vascular Ageing Study. J. Hypertens. 2020, 38, 1110–1122. [Google Scholar] [CrossRef]
- Shams, A.; Nobari, H.; Afonso, J.; Abbasi, H.; Mainer-Pardos, E.; Pérez-Gómez, J.; Bayati, M.; Bahrami, A.; Carneiro, L. Effect of Aerobic-Based Exercise on Psychological Well-Being and Quality of Life Among Older People: A Middle East Study. Front. Public Health 2021, 9, 764044. [Google Scholar] [CrossRef]
- Nobari, H.; Rezaei, S.; Sheikh, M.; Fuentes-García, J.P.; Pérez-Gómez, J. Effect of Virtual Reality Exercises on the Cognitive Status and Dual Motor Task Performance of the Aging Population. Int. J. Environ. Res. Public Health 2021, 18, 8005. [Google Scholar] [CrossRef]
- Jørgensen, A.B.; Frikke-Schmidt, R.; Nordestgaard, B.G.; Tybjærg-Hansen, A. Loss-of-Function Mutations in APOC3 and Risk of Ischemic Vascular Disease. N. Engl. J. Med. 2014, 371, 32–41. [Google Scholar] [CrossRef] [PubMed]
- García-Ortiz, L.; Recio-Rodríguez, J.I.; Schmidt-Trucksäss, A.; Puigdomenech-Puig, E.; Martínez-Vizcaíno, V.; Fernández-Alonso, C.; Rubio-Galan, J.; Agudo-Conde, C.; Patino-Alonso, M.C.; Rodríguez-Sánchez, E.; et al. Relationship between objectively measured physical activity and cardiovascular aging in the general population—The EVIDENT trial. Atherosclerosis 2014, 233, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Wolters, F.J.; Ikram, M.A. Epidemiology of Vascular Dementia. Arter. Thromb. Vasc. Biol. 2019, 39, 1542–1549. [Google Scholar] [CrossRef] [PubMed]
- Mönkäre, S.; Kuuluvainen, L.; Schleutker, J.; Bras, J.; Roine, S.; Pöyhönen, M.; Guerreiro, R.; Myllykangas, L. Genetic analysis reveals novel variants for vascular cognitive impairment. Acta Neurol. Scand. 2022. [Google Scholar] [CrossRef] [PubMed]
- Pasi, M.; Cordonnier, C. Clinical Relevance of Cerebral Small Vessel Diseases. Stroke 2020, 51, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Marcos, M.A.; Martinez-Salgado, C.; Gonzalez-Sarmiento, R.; Hernandez-Rivas, J.M.; Sanchez-Fernandez, P.L.; I Recio-Rodriguez, J.; Rodriguez-Sanchez, E.; García-Ortiz, L. Association between different risk factors and vascular accelerated ageing (EVA study): Study protocol for a cross-sectional, descriptive observational study. BMJ Open 2016, 6, e011031. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Sánchez, M.; Patino-Alonso, M.C.; Gómez-Sánchez, L.; Recio-Rodríguez, J.I.; Rodríguez-Sánchez, E.; Maderuelo-Fernández, J.A.; García-Ortiz, L.; Gómez-Marcos, M.A.; EVA Group. Reference values of arterial stiffness parameters and their association with cardiovascular risk factors in the Spanish population. The EVA Study. Rev. Esp. Cardiol. (Engl. Ed.) 2020, 73, 43–52. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Marshall, A.L.; Miller, Y.D.; Burton, N.W.; Brown, W.J. Measuring Total and Domain-Specific Sitting: A study of reliability and validity. Med. Sci. Sports Exerc. 2010, 42, 1094–1102. [Google Scholar] [CrossRef]
- Miller, R.; Brown, W. Steps and sitting in a working population. Int. J. Behav. Med. 2004, 11, 219–224. [Google Scholar] [CrossRef]
- Reference Values for Arterial Stiffness’ Collaboration. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘establishing normal and reference values’. Eur. Heart J. 2010, 31, 2338–2350. [Google Scholar] [CrossRef] [PubMed]
- D’Agostino, R.B., Sr.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General Cardiovascular Risk Profile for Use in Primary Care: The Framingham Heart Study. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef] [PubMed]
- Appiah, D.; Capistrant, B.D. Cardiovascular Disease Risk Assessment in the United States and Low- and Middle-Income Countries Using Predicted Heart/Vascular Age. Sci. Rep. 2017, 7, 16673. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Marcos, M.A.; Recio-Rodríguez, J.I.; Patino-Alonso, M.C.; Agudo-Conde, C.; Gómez-Sanchez, L.; Gómez-Sanchez, M.; Rodriguez-Sanchez, E.; Garcia-Ortiz, L. Protocol for Measuring Carotid Intima-Media Thickness That Best Correlates With Cardiovascular Risk and Target Organ Damage. Am. J. Hypertens. 2012, 25, 955–961. [Google Scholar] [CrossRef] [PubMed]
- Van Bortel, L.M.; Laurent, S.; Boutouyrie, P.; Chowienczyk, P.; Cruickshank, J.K.; De Backer, T.; Filipovsky, J.; Huybrechts, S.; Mattace-Raso, F.U.; Protogerou, A.D.; et al. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J. Hypertens. 2012, 30, 445–448. [Google Scholar] [CrossRef]
- Huynh, Q.L.; Blizzard, C.L.; Sharman, J.E.; Magnussen, C.G.; Dwyer, T.; Venn, A.J. The cross-sectional association of sitting time with carotid artery stiffness in young adults. BMJ Open 2014, 4, e004384. [Google Scholar] [CrossRef]
- Parsons, T.J.; Sartini, C.; Ellins, E.A.; Halcox, J.P.J.; Smith, K.E.; Ash, S.; Lennon, L.T.; Wannamethee, S.G.; Lee, I.-M.; Whincup, P.H.; et al. Objectively measured physical activity, sedentary time and subclinical vascular disease: Cross-sectional study in older British men. Prev. Med. 2016, 89, 194–199. [Google Scholar] [CrossRef]
- Tigbe, W.W.; Granat, M.H.; Sattar, N.; Lean, M.E.J. Time spent in sedentary posture is associated with waist circumference and cardiovascular risk. Int. J. Obes. 2017, 41, 689–696. [Google Scholar] [CrossRef][Green Version]
- Nauman, J.; Stensvold, D.; Coombes, J.S.; Wisløff, U. Cardiorespiratory Fitness, Sedentary Time, and Cardiovascular Risk Factor Clustering. Med. Sci. Sports Exerc. 2016, 48, 625–632. [Google Scholar] [CrossRef]
- Healy, G.N.; Dunstan, D.W.; Salmon, J.; Shaw, J.E.; Zimmet, P.Z.; Owen, N. Television Time and Continuous Metabolic Risk in Physically Active Adults. Med. Sci. Sports Exerc. 2008, 40, 639–645. [Google Scholar] [CrossRef]
- Oudegeest-Sander, M.H.; Thijssen, D.H.; Smits, P.; Van Dijk, A.P.; Rikkert, M.G.O.; Hopman, M.T. Association of Fitness Level With Cardiovascular Risk and Vascular Function in Older Nonexercising Individuals. J. Aging Phys. Act. 2015, 23, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Vélez, R.; Hernández-Quiñones, P.A.; Tordecilla-Sanders, A.; Álvarez, C.; Ramírez-Campillo, R.; Izquierdo, M.; Correa-Bautista, J.E.; Garcia-Hermoso, A.; Garcia, R.G. Effectiveness of HIIT compared to moderate continuous training in improving vascular parameters in inactive adults. Lipids Health Dis. 2019, 18, 42. [Google Scholar] [CrossRef] [PubMed]
- García-Hermoso, A.; Notario-Pacheco, B.; Recio-Rodríguez, J.I.; Martínez-Vizcaíno, V.; de Pablo, E.R.; Belio, J.M.F.; Gómez-Marcos, M.A.; García-Ortiz, L.; EVIDENT Group. Sedentary behaviour patterns and arterial stiffness in a Spanish adult population—The EVIDENT trial. Atherosclerosis 2015, 243, 516–522. [Google Scholar] [CrossRef] [PubMed]
- Suboc, T.B.; Knabel, D.; Strath, S.J.; Dharmashankar, K.; Coulliard, A.; Malik, M.; Haak, K.; Widlansky, M.E. Associations of Reducing Sedentary Time With Vascular Function and Insulin Sensitivity in Older Sedentary Adults. Am. J. Hypertens. 2016, 29, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Wennman, H.; Vasankari, T.; Borodulin, K. Where to Sit? Type of Sitting Matters for the Framingham Cardiovascular Risk Score. AIMS Public Health 2016, 3, 577–591. [Google Scholar] [CrossRef]
- Slivovskaja, I.; Ryliskyte, L.; Serpytis, P.; Navickas, R.; Badarienė, J.; Celutkiene, J.; Puronaite, R.; Ryliskiene, K.; Cypiene, A.; Rinkuniene, E.; et al. Aerobic Training Effect on Arterial Stiffness in Metabolic Syndrome. Am. J. Med. 2018, 131, 148–155. [Google Scholar] [CrossRef]
- Ahmadi-Abhari, S.; Sabia, S.; Shipley, M.J.; Kivimäki, M.; Singh-Manoux, A.; Tabak, A.; McEniery, C.; Wilkinson, I.B.; Brunner, E.J. Physical Activity, Sedentary Behavior, and Long-Term Changes in Aortic Stiffness: The Whitehall II Study. J. Am. Heart Assoc. 2017, 6, e005974. [Google Scholar] [CrossRef]
- Chau, J.Y.; Grunseit, A.; Midthjell, K.; Holmen, J.; Holmen, T.L.; Bauman, A.E.; van der Ploeg, H.P. Cross-sectional associations of total sitting and leisure screen time with cardiometabolic risk in adults. J. Sci. Med. Sport 2014, 17, 78–84. [Google Scholar] [CrossRef]
- Kim, Y.; Wilkens, L.R.; Park, S.-Y.; Goodman, M.T.; Monroe, K.R.; Kolonel, L.N. Association between various sedentary behaviours and all-cause, cardiovascular disease and cancer mortality: The Multiethnic Cohort Study. Int. J. Epidemiol. 2013, 42, 1040–1056. [Google Scholar] [CrossRef]
| Global (501) | Men (249) | Women (252) | p Value | |
|---|---|---|---|---|
| Conventional Risk Factors | ||||
| Age, years | 55.90 ± 14.24 | 55.95 ± 14.30 | 55.85 ± 14.19 | 0.935 |
| Framingham’s heart age, years | 52.98 ± 17.31 | 55.09 ±16.53 | 50.92 ± 17.85 | 0.007 |
| Heart age–chronological age, years | −2.98 ± 10.13 | −0.92 ± 10.21 | −5.01 ± 9.65 | <0.001 |
| Smoker, n (%) | 90 (18.00) | 49 (19.70) | 41.00 (16.30) | 0.190 |
| Hypertensive, n (%) | 147 (29.30) | 82 (32.90) | 65 (25.80) | <0.001 |
| Antihypertensive drugs, n (%) | 96 (19.20) | 50 (20.10) | 46 (18.30) | 0.650 |
| Dyslipidemia, n (%) | 191 (38.10) | 95 (38.10) | 96 (38.20) | 0.989 |
| Lipid–lowering drugs, n (%) | 102 (20.40) | 49 (19.70) | 53 (21.00) | 0.396 |
| Diabetes mellitus, n (%) | 38 (7.60) | 26 (10.50) | 12 (4.80) | 0.012 |
| Hypoglycemic drugs, n (%) | 35 (7.00) | 23 (9.20) | 12 (4.80) | 0.055 |
| Obesity, n (%) | 94 (18.80) | 42 (16.90) | 52 (20.60) | 0.304 |
| Sedentary Time | ||||
| Weekly time, h/W | 42.18 ± 16.93 | 47.60 ±16,58 | 36.76 ±17.29 | <0.001 |
| Commuting, h/W | 3.31 ± 7.48 | 3.64 ± 8.35 | 2.99 ± 6.62 | 0.335 |
| At work, h/W | 13.19 ± 15.52 | 16.66 ± 16.16 | 9.73 ± 14.89 | <0.001 |
| Watching television, h/W | 20.13 ± 12.18 | 21.55 ± 12.45 | 18.72 ± 11.91 | 0.010 |
| Vascular Assessment | ||||
| c-IMT (mm) | 0.682 ± 0.109 | 0.699 ± 0.115 | 0.665 ± 0.100 | 0.001 |
| cfPWV (m/s) | 8.17 ± 2.49 | 8.58 ± 2.74 | 7.77 ± 2.24 | <0.001 |
| VAI | 61.25 ± 12.64 | 63.47 ± 13.75 | 59.04 ± 11.54 | <0.001 |
| HVA | NVA | EVA | p Value | |
|---|---|---|---|---|
| Using 10th Percentile and 90th Percentile of European Population Cut Points | ||||
| Weekly time, h/W ¥,# | 38.78 ± 18.53 | 41.60 ± 17.91 | 46.62 ± 15.95 | 0.015 |
| Commuting, h/W | 2.78 ± 6.07 | 3.43 ± 7.54 | 3.37 ± 8.60 | 0.808 |
| At work, h/W | 12.41 ± 14.39 | 13.09 ± 16.32 | 14.17 ± 15.48 | 0.776 |
| Watching television, h/W ¥,# | 18.29 ± 11.66 | 19.56 ± 12.08 | 23.46 ± 12.47 | 0.012 |
| Using 10th Percentile and 90th Percentile of VAI | ||||
| Weekly time, h/W ¥,# | 39.69 ± 19.94 | 40.82 ± 17.42 | 47.05 ± 16.43 | 0.003 |
| Commuting, h/W | 2.62 ± 6.52 | 3.60 ± 7.76 | 3.07 ± 7.69 | 0.574 |
| At work, h/W | 13.95 ± 18.05 | 12.51 ± 15.45 | 15.23 ± 16.01 | 0.282 |
| Watching television, h/W ¥,# | 18.08 ± 9.77 | 19.49 ± 12.23 | 22.76 ± 12.90 | 0.017 |
| Using Framingham’s Heart Age | ||||
| Weekly time, h/W * | 39.27 ± 17.17 | 44.88 ± 16.95 | 42.74 ± 20.09 | 0.005 |
| Commuting, h/W | 2.82 ± 5.34 | 3.29 ± 8.12 | 4.66 ± 10.70 | 0.168 |
| At work, h/W | 12.34 ± 15.25 | 14.40 ± 16.19 | 11.88 ± 16.62 | 0.325 |
| Watching television, h/W *,# | 18.34 ± 11.22 | 21.74 ± 12.52 | 21.60 ± 13.94 | 0.010 |
| Difference | 95% CI | |
|---|---|---|
| Using 10th Percentile and 90th Percentile of European Population Cut Points | ||
| Weekly time, h/W | −7.840 | (−13.413–−2.267) |
| Commuting, h/W | −0.589 | (−2.912–1.733) |
| At work, h/W | −1.755 | (−6.500–2.990) |
| Watching television, h/W | −5.173 | (−9.009–−1.338) |
| Using 10th Percentile and 90th Percentile of VAI | ||
| Weekly time, h/W | −7.365 | (−13.041–−1.689) |
| Commuting, h/W | −0.451 | (−2.564–1.661) |
| At work, h/W | −1.287 | (−6.537–3.964) |
| Watching television, h/W | −4.680 | (−8.020–−1.339) |
| Using Framingham’s Heart Age | ||
| Weekly time, h/W | −3.467 | (−8.409–−1.474) |
| Commuting, h/W | −1.840 | (−4.289–0.608) |
| At work, h/W | 0.457 | (−3.694–4.608) |
| Watching television, h/W | −3.263 | (−6.651–−0.126) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Llamas-Ramos, I.; Llamas-Ramos, R.; Alonso-Domínguez, R.; Gómez-Sánchez, L.; Tamayo-Morales, O.; Lugones-Sánchez, C.; Rodríguez-Sánchez, E.; García-Ortiz, L.; Gómez-Marcos, M.A. Sedentary Behaviour and Its Relationship with Early Vascular Ageing in the General Spanish Population: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 5450. https://doi.org/10.3390/ijerph19095450
Llamas-Ramos I, Llamas-Ramos R, Alonso-Domínguez R, Gómez-Sánchez L, Tamayo-Morales O, Lugones-Sánchez C, Rodríguez-Sánchez E, García-Ortiz L, Gómez-Marcos MA. Sedentary Behaviour and Its Relationship with Early Vascular Ageing in the General Spanish Population: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(9):5450. https://doi.org/10.3390/ijerph19095450
Chicago/Turabian StyleLlamas-Ramos, Inés, Rocío Llamas-Ramos, Rosario Alonso-Domínguez, Leticia Gómez-Sánchez, Olaya Tamayo-Morales, Cristina Lugones-Sánchez, Emiliano Rodríguez-Sánchez, Luis García-Ortiz, and Manuel A. Gómez-Marcos. 2022. "Sedentary Behaviour and Its Relationship with Early Vascular Ageing in the General Spanish Population: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 9: 5450. https://doi.org/10.3390/ijerph19095450
APA StyleLlamas-Ramos, I., Llamas-Ramos, R., Alonso-Domínguez, R., Gómez-Sánchez, L., Tamayo-Morales, O., Lugones-Sánchez, C., Rodríguez-Sánchez, E., García-Ortiz, L., & Gómez-Marcos, M. A. (2022). Sedentary Behaviour and Its Relationship with Early Vascular Ageing in the General Spanish Population: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(9), 5450. https://doi.org/10.3390/ijerph19095450







