The Influence of Patient-Centered Communication on Children’s Anxiety and Use of Anesthesia for MR
Abstract
1. Introduction
2. Materials and Methods
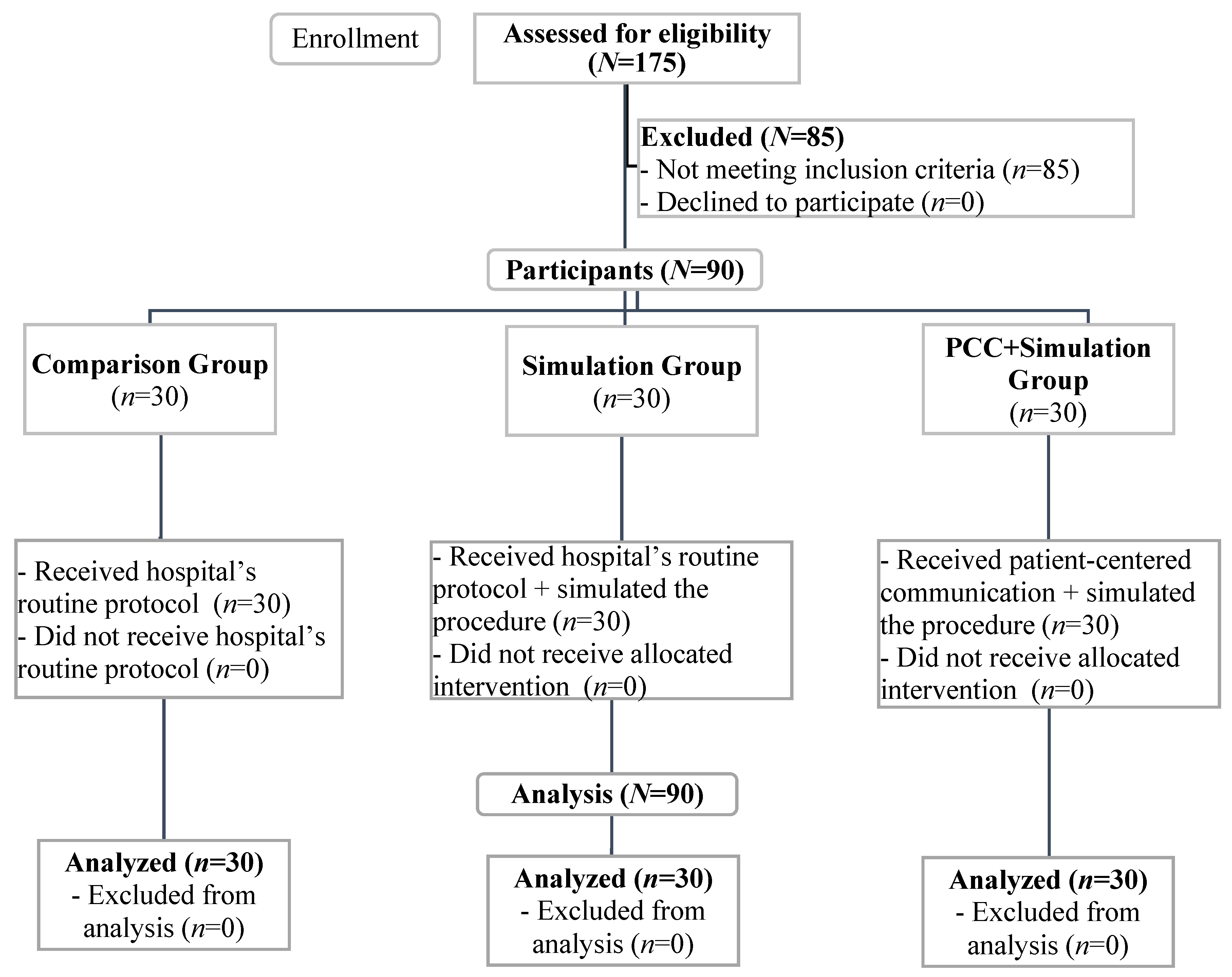
2.1. Participants
2.2. Measures
2.3. Procedure
2.4. Analyses
3. Results
3.1. Anxiety
3.2. Satisfaction
3.3. Use of Anesthesia
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Carter, A.J.; Greer, M.L.; Gray, S.E.; Ware, R.S. Mock MRI: Reducing the need for anaesthesia in children. Pediatr. Radiol. 2010, 40, 1368–1374. [Google Scholar] [CrossRef] [PubMed]
- de Amorim e Silva, C.J.T.; Mackenzie, A.; Hallowell, L.M.; Stewart, S.E.; Ditchfield, M.R. Practice MRI: Reducing the need for sedation and general anaesthesia in children undergoing MRI. Australas. Radiol. 2006, 50, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Lemaire, C.; Moran, G.R.; Swan, H. Impact of audio/visual systems on pediatric sedation in magnetic resonance imaging. J. Magn. Reson. Imaging 2009, 30, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Jaimes, C.; Murcia, D.J.; Miguel, K.; DeFuria, C.; Sagar, P.; Gee, M.S. Identification of quality improvement areas in pediatric MRI from analysis of patient safety reports. Pediatr. Radiol. 2018, 48, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Vanderby, S.A.; Babyn, P.S.; Carter, M.W.; Jewell, S.M.; McKeever, P.D. Effect of anesthesia and sedation on pediatric MR imaging patient flow. Radiology 2010, 256, 229–237. [Google Scholar] [CrossRef]
- Keller, A. MRI and CT Expert Panel: Phase I Report; Ontario Ministry of Health and Long-Term Care: Toronto, ON, Canada, 2005. [Google Scholar]
- Mastro, K.A.; Flynn, L.; Millar, T.F.; DiMartino, T.M.; Ryan, S.M.; Stein, M.H. Reducing anesthesia use for pediatric magnetic resonance imaging: The effects of a patient- and family-centered intervention on image quality, health-care costs, and operational efficiency. J. Radiol. Nurs. 2019, 38, 21–27. [Google Scholar] [CrossRef]
- Kannikeswaran, N.; Mahajan, P.V.; Sethuraman, U.; Groebe, A.; Chen, X. Sedation medication received and adverse events related to sedation for brain MRI in children with and without developmental disabilities. Paediatr. Anesth. 2009, 19, 250–256. [Google Scholar] [CrossRef]
- Cravero, J.P.; Beach, M.L.; Blike, G.T.; Gallagher, S.M.; Hertzog, J.H. Pediatric Sedation Research Consortium. The incidence and nature of adverse events during pediatric sedation/anesthesia with propofol for procedures outside the operating room: A report from the Pediatric Sedation Research Consortium. Anesth. Analg. 2009, 108, 795–804. [Google Scholar] [CrossRef]
- Kitsa, P.; Andronikou, S.; Cardoso, J. Sedation of children undergoing MRI—A risky business! S. Afr. Med. J. 2004, 94, 625–626. [Google Scholar]
- Daud, Y.N.; Carlson, D.W. Pediatric sedation. Pediatr. Clin. N. Am. 2014, 61, 703–717. [Google Scholar] [CrossRef]
- Efron, D.; Vutskits, L.; Davidson, A.J. Can we really suggest that anesthesia might cause attention-deficit/hyperactivity disorder? Anesthesiology 2017, 127, 209–211. [Google Scholar] [CrossRef] [PubMed]
- Sprung, J.; Flick, R.P.; Katusic, S.K.; Colligan, R.C.; Barbaresi, W.J.; Bojanić, K.; Welch, T.; Olson, M.D.; Hanson, A.C.; Schroeder, D.R.; et al. Attention-deficit/hyperactivity disorder after early exposure to procedures requiring general anesthesia. Mayo Clin. Proc. 2012, 87, 120–129. [Google Scholar] [CrossRef]
- Hu, D.; Flick, R.P.; Zaccariello, M.J.; Colligan, R.C.; Katusic, S.K.; Schroeder, D.R.; Hanson, A.C.; Buenvenida, S.L.; Gleich, S.J.; Wilder, R.T.; et al. Association between exposure of young children to procedures requiring general anesthesia and learning and behavioral outcomes in a population-based birth cohort. Anesthesiology 2017, 127, 227–240. [Google Scholar] [CrossRef] [PubMed]
- Durand, D.J.; Young, M.; Nagy, P.; Tekes, A.; Huisman, T.A. Mandatory child life consultation and its impact on pediatric MRI workflow in an academic medical center. J. Am. Coll. Radiol. 2015, 12, 594–598. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Jordan, Z. Interventions to reduce anxiety, distress, and the need for sedation in pediatric patients undergoing magnetic resonance imaging: A systematic review. J. Radiol. Nurs. 2013, 32, 87–96. [Google Scholar] [CrossRef]
- Perez, M.; Cuscaden, C.; Somers, J.F.; Simms, N.; Shaheed, S.; Kehoe, L.A.; Holowka, S.A.; Aziza, A.A.; Shroff, M.M.; Greer, M.-L.C. Easing anxiety in preparation for pediatric magnetic resonance imaging: A pilot study using animal-assisted therapy. Pediatr. Radiol. 2019, 49, 1000–1009. [Google Scholar] [CrossRef]
- Harned, R.K.; Strain, J.D. MRI-compatible audio/visual system: Impact on pediatric sedation. Pediatr. Radiol. 2001, 31, 247–250. [Google Scholar] [CrossRef]
- Tornqvist, E.; Mansson, A.; Hallstrom, I. Children having magnetic resonance imaging: A preparatory storybook and audio/visual media are preferable to anesthesia or deep sedation. J. Child Health Care 2015, 19, 359–369. [Google Scholar] [CrossRef]
- Viggiano, M.P.; Giganti, F.; Rossi, A.; Di Feo, D.; Vagnoli, L.; Calcagno, G.; Defilippi, C. Impact of psychological interventions on reducing anxiety, fear and the need for sedation in children undergoing magnetic resonance imaging. Pediatr. Rep. 2015, 7, 5682. [Google Scholar] [CrossRef]
- Li, J.; Li, Q.; Dai, X.; Li, J.; Zhang, X. Does pre-scanning training improve the image quality of children receiving magnetic resonance imaging? Medicine 2019, 98, e14323. [Google Scholar] [CrossRef]
- De Bie, H.M.A.; Boersma, M.; Wattjes, M.P.; Adriaanse, S.; Vermeulen, R.J.; Oostrom, K.J.; Huisman, J.; Veltman, D.J.; De Waal, H.A.D.-V. Preparing children with a mock scanner training protocol results in high quality structural and functional MRI scans. Eur. J. Pediatr. 2010, 169, 1079–1085. [Google Scholar] [CrossRef] [PubMed]
- Barnea-Goraly, N.; Weinzimer, S.A.; Ruedy, K.J.; Mauras, N.; Beck, R.W.; Marzelli, M.J.; Mazaika, P.K.; Aye, T.; White, N.H.; Tsalikian, E.; et al. High success rates of sedation-free brain MRI scanning in young children using simple subject preparation protocols with and without a commercial mock scanner—The Diabetes Research in Children Network (DirecNet) experience. Pediatr. Radiol. 2014, 44, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Bray, L.; Booth, L.; Gray, V.; Maden, M.; Thompson, J.; Saron, H. Interventions and methods to prepare, educate or familiarise children and young people for radiological procedures: A scoping review. Insights Imaging 2022, 13, 146. [Google Scholar] [CrossRef] [PubMed]
- Li, W.H.C.; Chung, J.O.K.; Ho, K.Y.; Kwok, B.M.C. Play interventions to reduce anxiety and negative emotions in hospitalized children. BMC Pediatr. 2016, 16, 36. [Google Scholar] [CrossRef] [PubMed]
- Bharti, B.; Malhi, P.; Khandelwal, N. MRI customized play therapy in children reduces the need for sedation—A randomized controlled trial. Indian J. Pediatr. 2016, 83, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Bray, L.; Appleton, V.; Sharpe, A. The information needs of children having clinical procedures in hospital: Will it hurt? Will I feel scared? What can I do to stay calm? Child Care Health Dev. 2019, 45, 737–743. [Google Scholar] [CrossRef] [PubMed]
- Carter, B.; Bray, L.; Dickinson, A.; Edwards, M.; Ford, K. Child-Centred Nursing: Promoting Critical Thinking; Sage: London, UK, 2014. [Google Scholar]
- Söderbäck, M.; Coyne, I.; Harder, M. The importance of including both a child perspective and the child’s perspective within health care settings to provide truly child-centred care. J. Child Health Care 2011, 15, 99–106. [Google Scholar] [CrossRef]
- Hart, C.; Chesson, R. Children as consumers. BMJ. 1998, 316, 1600–1603. [Google Scholar] [CrossRef]
- Southall, D.P.; Burr, S.; Smith, R.D.; Bull, D.N.; Radford, A.; Williams, A.; Nicholson, S. The Child-Friendly Healthcare Initiative (CFHI): Healthcare provision in accordance with the UN Convention on the Rights of the Child. Child Advocacy International. Department of Child and Adolescent Health and Development of the World Health Organization (WHO). Royal College of Nursing (UK). Royal College of Paediatrics and Child Health (UK). United Nations Children’s Fund (UNICEF). Pediatrics 2000, 106, 1054–1064. [Google Scholar]
- Coyne, I. Consultation with children in hospital: Children, parents’ and nurses’ perspectives. J. Clin. Nurs. 2006, 15, 61–71. [Google Scholar] [CrossRef]
- Runge, S.B.; Christensen, N.L.; Jensen, K.; Jensen, I.E. Children centered care: Minimizing the need for anesthesia with a multi-faceted concept for MRI in children aged 4–6. Eur. J. Radiol. 2018, 107, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Pereira, L.; Figueiredo-Braga, M.; Carvalho, I.P. Preoperative anxiety in ambulatory surgery: The impact of an empathic patient-centered approach on psychological and clinical outcomes. Patient Educ. Couns. 2016, 99, 733–738. [Google Scholar] [CrossRef] [PubMed]
- Rathert, C.; Wyrwich, M.D.; Boren, S.A. Patient-centred care and outcomes: A systematic review of the literature. Med. Care Res. Rec. 2013, 70, 351–379. [Google Scholar] [CrossRef] [PubMed]
- Florence, S.; Gambotti, L.; Tezenas du Montcel, S.; Straczek, C.; Raphaël, M.; Cisse, A.; Renard, R.; Trosini-Desert, V.; Leblond, V.; Astagneau, P. Patients’ perception of information received when a complementary medical examination is prescribed. Sante Publique 2009, 21, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Rocha, J.; Carvalho, I.P. The influence of professionals’ empathy on parents’ anxiety in cases of juvenile criminology. Soc. Work 2019, 64, 242–252. [Google Scholar] [CrossRef]
- Brouwers, M.; Rasenberg, E.; van Weel, C.; Laan, R.; van Weel-Baumgarten, E. Assessing patient-centred communication in teaching: A systematic review of instruments. Med. Educ. 2017, 51, 1103–1117. [Google Scholar] [CrossRef]
- Stewart, M.; Brown, J.B.; Donner, A.; McWhinney, I.R.; Oates, J.; Weston, W.W.; Jordan, J. The impact of patient-centered care on outcomes. J. Fam. Pract. 2000, 49, 796–804. [Google Scholar]
- Eklund, J.H.; Holmström, I.K.; Kumlin, T.; Kaminsky, E.; Skoglund, K.; Höglander, J.; Sundler, A.J.; Condén, E.; Meranius, M.S. “Same same or different?” A review of reviews of person-centered and patient-centered care. Patient Educ. Couns. 2019, 102, 3–11. [Google Scholar] [CrossRef]
- Silverman, J.; Kurtz, S.; Draper, J. Skills for Communicating with Patients, 3rd ed.; CRC Press: Boca Raton, FL, USA, 2013. [Google Scholar]
- Ivey, A.E.; Ivey, M.B.; Zalaquett, C. Intentional Interviewing and Counseling, 9th revised ed.; Brooks/Cole Cengage Learning: Belmont, CA, USA, 2018. [Google Scholar]
- Ford, K.; Campbell, S.; Carter, B.; Earwaker, L. The concept of child-centered care in healthcare: A scoping review protocol. JBI Database Syst. Rev. Implement Rep. 2018, 16, 845–851. [Google Scholar] [CrossRef]
- Buchanan, H.; Niven, N. Validation of a Facial Image Scale to assess child dental anxiety. Int. J. Paediatr. Dent. 2002, 12, 47–52. [Google Scholar]
- Preece, J.; Rogers, Y.; Sharp, H. Interaction Design: Beyond Human-Computer Interaction, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2007. [Google Scholar]

| Total | CG | Simulation | PCC + Simulation | Group Difference | ||
|---|---|---|---|---|---|---|
| N = 90 | n = 30 | n = 30 | n = 30 | p-Value | ||
| Age (years)-Mean (SD) | 6.53 (1.95) | 6.47 (2.05) | 6.20 (2.09) | 6.93 (1.70) | 0.343 a | |
| Gender-n (%) | Boys | 45 (50.0%) | 18 (60.0) | 12 (40.0) | 15 (50.0) | 0.301 b |
| Girls | 45 (50.0%) | 12 (40.0) | 18 (60.0) | 15 (50.0) | ||
| Exam type-n (%) | Neuroradiology | 45 (50.0%) | 19 (63.3) | 13 (43.3) | 13 (43.3) | 0.202 b |
| General radiology | 45 (50.0%) | 11 (36.7) | 17 (56.7) | 17 (56.7) | ||
| Referral-n (%) | Outpatient care | 69 (76.7%) | 21 (70.0) | 22 (73.3) | 26 (86.7) | 0.271 b |
| Inpatient care | 21 (23.3%) | 9 (30.0) | 8 (26.7) | 4 (13.3) | ||
| Anxiety | Group | T0 | T1 | p [T1-T0] |
|---|---|---|---|---|
| Self-reported-Median (IQR) 1 | “Sim” | 4 (2–4) | 3 (2–4) | 0.011 a |
| “PCC + Sim” | 3 (2–4) | 2 (1–2) | <0.001 a | |
| p [“Sim”-“PCC + Sim”] | 0.288 b | <0.001 b | ||
| Heart rate (bpm)-Mean (SD) 2 | “Sim” | 96.27 (15.39) | 91.60 (16.66) | 0.010 c |
| “PCC + Sim” | 92.37 (12.86) | 81.20 (9.56) | <0.001 c | |
| p [“Sim”-“PCC + Sim”] | 0.291 d | 0.005 d |
| Satisfaction with the Interaction | “Sim” | “PCC + Sim” | p [“Sim”-“PCC + Sim”] | |
|---|---|---|---|---|
| 1—“Loved it”-Median (IQR) 1 | 4 (3–5) | 5 (4–5) | 0.001 a | |
| 2—“Helped me feel calmer”-n (%) | Yes | 20 (66.7) | 30 (100.0) | 0.001 b |
| No | 10 (33.3) | 0 (0.0) | ||
| I don’t know | 0 (0.0) | 0 (0.0) | ||
| 3—“Decreased my fears”-n (%) | Yes | 20 (66.7) | 30 (100.0) | 0.001 b |
| No | 10 (33.3) | 0 (0.0) | ||
| I don’t know | 0 (0.0) | 0 (0.0) | ||
| 4—“Taught me not to move”-n (%) | Yes | 13 (43.3) | 30 (100.0) | <0.001 b |
| No | 17 (56.7) | 0 (0.0) | ||
| I don’t know | 0 (0.0) | 0 (0.0) | ||
| 5—“Taught me to tolerate loud noises”-n (%) | Yes | 9 (30.0) | 28 (93.3) | NA |
| No | 21 (70.0) | 1 (3.3) | ||
| I don’t know | 0 (0.0) | 1 (3.3) | ||
| 6—“Would like to repeat it next time”-n (%) | Yes | 14 (46.7) | 28 (93.3) | NA |
| No | 12 (40.0) | 1 (3.3) | ||
| I don’t know | 4 (13.3) | 1 (3.3) |
| (Less) Anesthesia Use | ||
|---|---|---|
| OR (95% CI) | p | |
| Reduced anxiety (heartbeat frequency) | 1.39 (1.07–1.79) | 0.013 |
| Age | 3.26 (1.43–7.43) | 0.005 |
| Male gender | 1.51 (0.23–10.15) | 0.671 |
| General radiology exams | 10.69 (1.20–94.81) | 0.033 |
| Referral from inpatient care | 4.07 (0.32–51.37) | 0.278 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castro, M.C.; Ramos, I.; Carvalho, I.P. The Influence of Patient-Centered Communication on Children’s Anxiety and Use of Anesthesia for MR. Int. J. Environ. Res. Public Health 2023, 20, 414. https://doi.org/10.3390/ijerph20010414
Castro MC, Ramos I, Carvalho IP. The Influence of Patient-Centered Communication on Children’s Anxiety and Use of Anesthesia for MR. International Journal of Environmental Research and Public Health. 2023; 20(1):414. https://doi.org/10.3390/ijerph20010414
Chicago/Turabian StyleCastro, M. Conceição, Isabel Ramos, and Irene Palmares Carvalho. 2023. "The Influence of Patient-Centered Communication on Children’s Anxiety and Use of Anesthesia for MR" International Journal of Environmental Research and Public Health 20, no. 1: 414. https://doi.org/10.3390/ijerph20010414
APA StyleCastro, M. C., Ramos, I., & Carvalho, I. P. (2023). The Influence of Patient-Centered Communication on Children’s Anxiety and Use of Anesthesia for MR. International Journal of Environmental Research and Public Health, 20(1), 414. https://doi.org/10.3390/ijerph20010414






