Ecological Momentary Assessment of Masseter Muscle Activity in Patients with Bruxism
Abstract
1. Introduction
2. Materials and Methods
2.1. Participant Selection Process
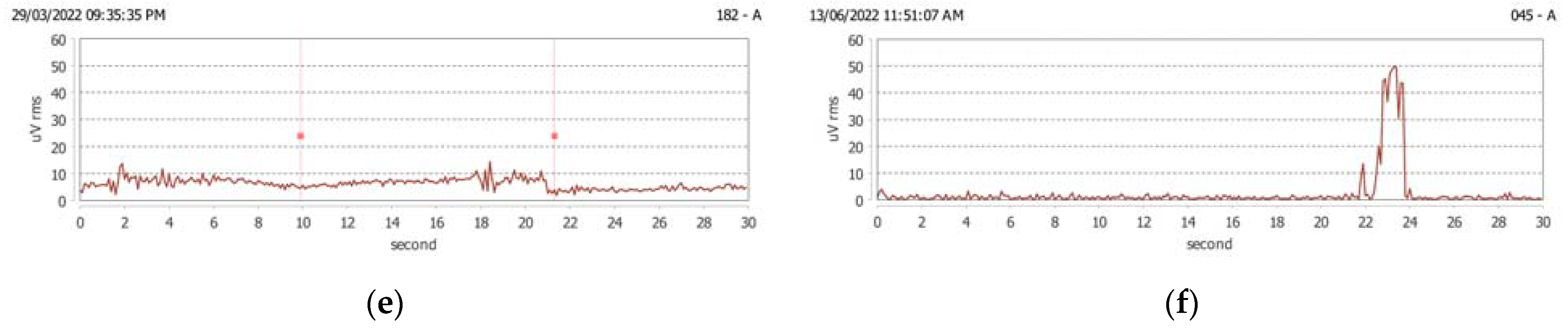
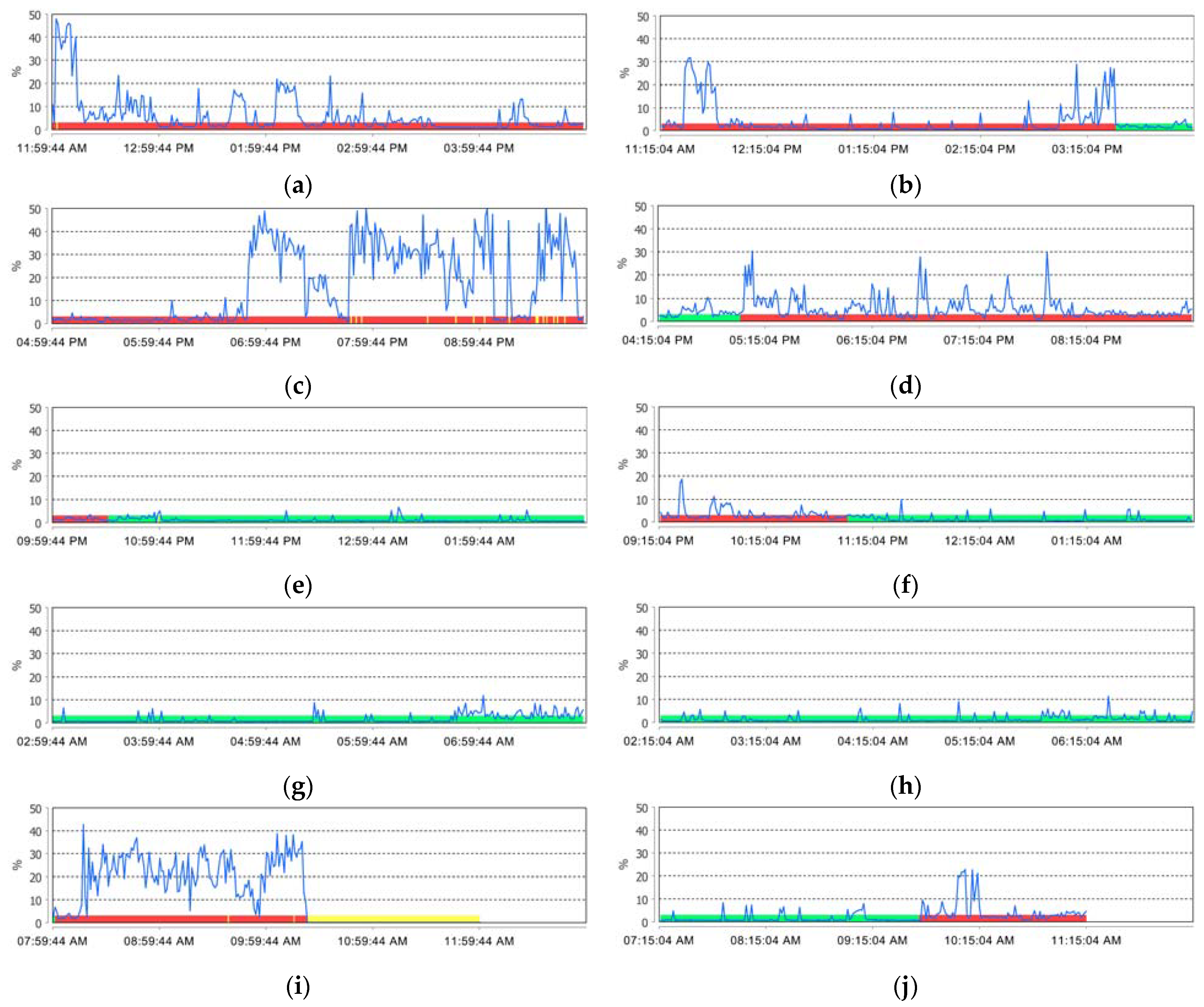
2.2. sEMG Recordings
- T: total duration of the period in which data were acquired;
- t: the time interval between the reception of two events, in this case, 100 mS;
- n: total number of recorded data points;
- i: reference number between 1 and n (inclusive);
- xi: value of data recorded by sEMG (in μV);
- xmax: maximum value recorded by sEMG (in μV);
- ki: binary value related to recorded data.
2.3. Bruxism Time Index
2.4. Bruxism Effort Index
2.5. Personal Bruxism Index
2.6. Statistical Analysis
3. Results
3.1. Characteristics of the Study Groups
3.2. sEMG Evaluation Results
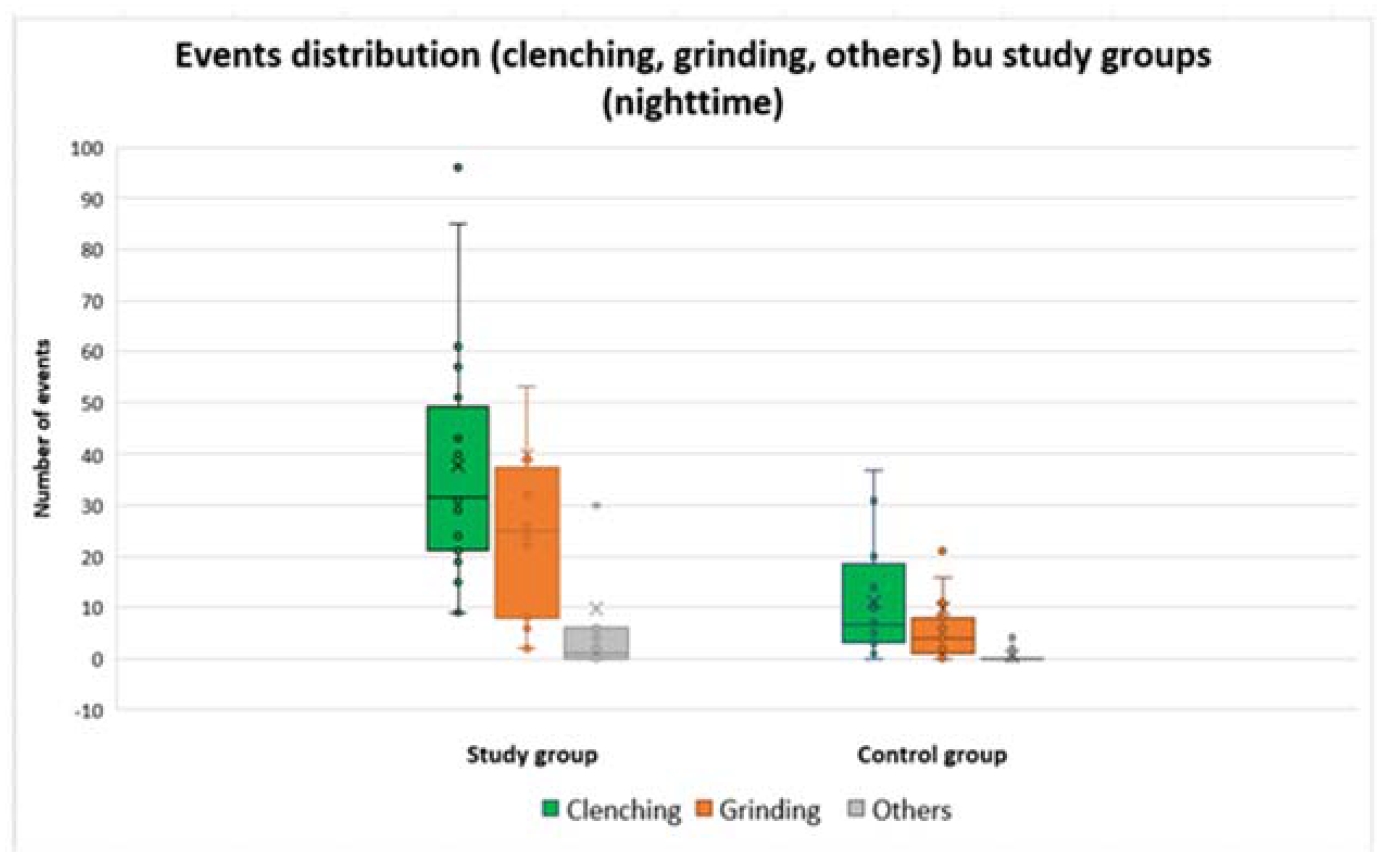
3.3. Evaluation of Recorded Activities in Bruxism
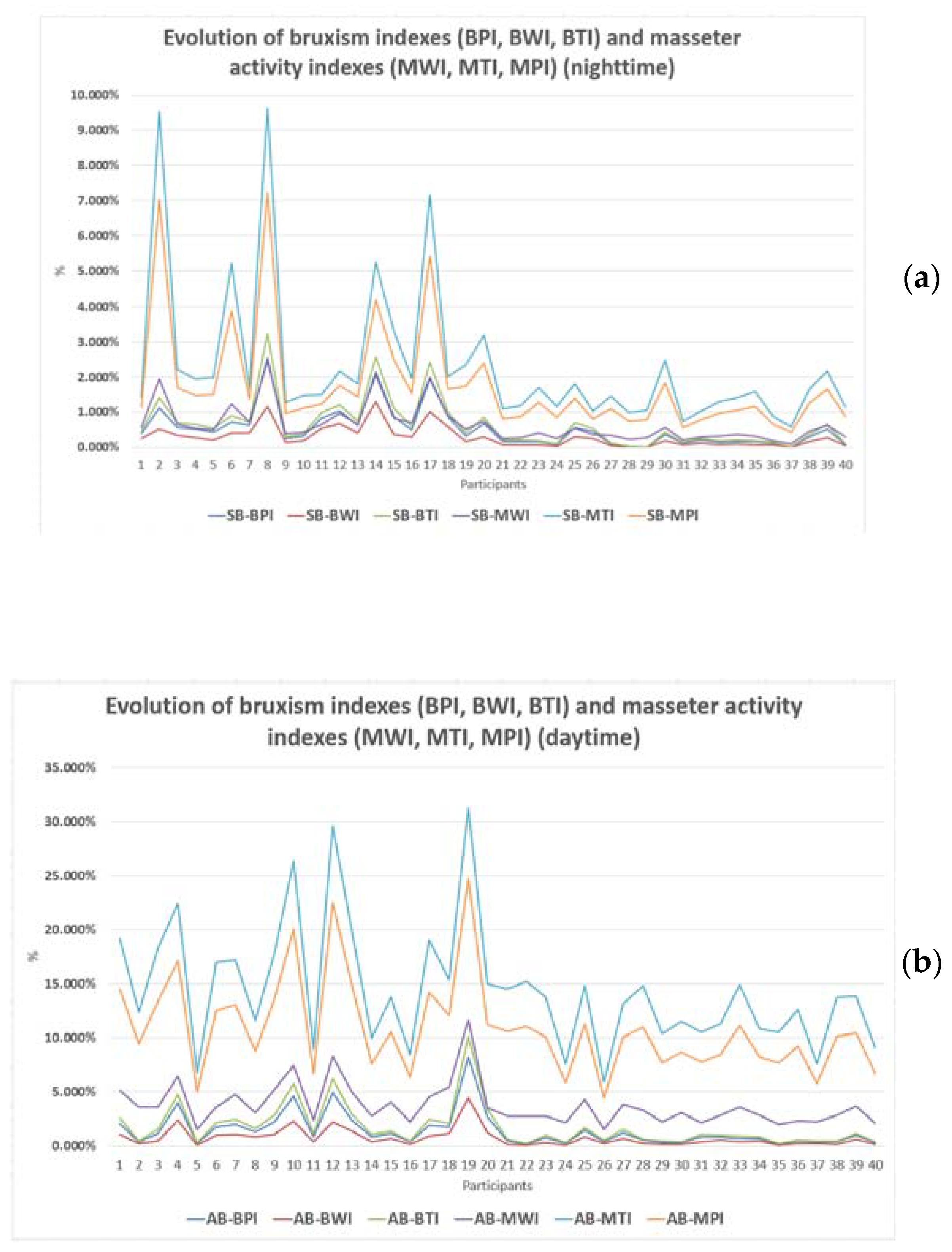
3.4. Assessment of the Effort Made during Bruxism Activity (BWI)
3.5. Duration of Bruxism-Specific Activity (BTI)
3.6. Evaluation of the Personal Bruxism Index (BPI)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Reddy, S.V.; Kumar, M.P.; Sravanthi, D.; Mohsin, A.H.; Anuhya, V. Bruxism: A literature review. J. Int. Oral Health 2014, 6, 105–109. [Google Scholar]
- Frohman, B.S. Application of psychotherapy to dental problems. Dent. Cosmet. 1931, 73, 1117–1122. [Google Scholar]
- Lobbezoo, F.; Ahlberg, J.; Glaros, A.G.; Kato, T.; Koyano, K.; Lavigne, G.J.; de Leeuw, R.; Manfredini, D.; Svensson, P.; Winocur, E. Bruxism defined and graded: An international consensus. J. Oral Rehabil. 2013, 40, 2–4. [Google Scholar] [CrossRef]
- De Leeuw, R.; Klasser, G.D. (Eds.) Orofacial Pain. Guidelines for Assessment, Diagnosis, and Management, 4th ed.; Quintessence Publishing Co, Inc.: Chicago, IL, USA, 2008; p. 316. [Google Scholar]
- American Academy of Sleep Medicine. International Classification of Sleep Disorders, 2nd ed.; American Academy of Sleep Medicine: Westchester, NY, USA, 2005. [Google Scholar]
- The glossary of prosthodontics terms, 8th ed. J. Prosthet. Dent. 2005, 94, 10–92. [CrossRef]
- Lobbezoo, F.; Ahlberg, J.; Raphael, K.G.; Wetselaar, P.; Glaros, A.G.; Kato, T.; Santiago, V.; Winocur, E.; de Laat, A.; de Leeuw, R.; et al. International consensus on the assessment of bruxism: Report of a work in progress. J. Oral Rehabil. 2018, 45, 837–844. [Google Scholar] [CrossRef]
- Manfredini, D.; Ahlberg, J.; Wetselaar, P.; Svensson, P.; Lobbezoo, F. The bruxism construct: From cut-off points to a continuum spectrum. J. Oral Rehabil. 2019, 46, 991–997. [Google Scholar] [CrossRef]
- Manfredini, D.; Ahlberg, J.; Lobbezoo, F. Bruxism definition: Past, present, and future—What should a prosthodontist know? J. Prosthet. Dent. 2022, 128, 905–912. [Google Scholar] [CrossRef]
- Manfredini, D.; Ahlberg, J.; Aarab, G.; Bracci, A.; Durham, J.; Emodi-Perlman, A.; Ettlin, D.; Gallo, L.M.; Häggman-Henrikson, B.; Koutris, M.; et al. The development of the Standardised Tool for the Assessment of Bruxism (STAB): An international road map. J. Oral Rehabil. 2022, 47, 549–556. [Google Scholar] [CrossRef]
- Manfredini, D.; Ahlberg, J.; Aarab, G.; Bracci, A.; Durham, J.; Ettlin, D.; Gallo, L.M.; Koutris, M.; Wetselaar, P.; Svensson, P.; et al. Towards a Standardized Tool for the Assessment of Bruxism (STAB)-Overview and general remarks of a multidimensional bruxism evaluation system. J. Oral Rehabil. 2020, 47, 549–556. [Google Scholar] [CrossRef]
- Bracci, A.; Lobbezoo, F.; Häggman-Henrikson, B.; Colonna, A.; Nykänen, L.; Pollis, M.; Ahlberg, J.; Manfredini, D. International Network for Orofacial Pain and Related Disorders Methodology. Current Knowledge and Future Perspectives on Awake Bruxism Assessment: Expert Consensus Recommendations. J. Clin. Med. 2022, 11, 5083. [Google Scholar] [CrossRef]
- Lobbezoo, F.; Ahlberg, J.; Aarab, G.; Manfredini, D. Why using ‘harmless behaviour’, ‘risk factor’ and ‘protective factor’ as terms describing the various possible consequences of bruxism is still the best option. J. Oral Rehabil. 2021, 48, 762–763. [Google Scholar] [CrossRef] [PubMed]
- Lavigne, G.; Kato, T.; Herrero Babiloni, A.; Huynh, N.; Dal Fabbro, C.; Svensson, P.; Aarab, G.; Ahlberg, J.; Baba, K.; Carra, M.C.; et al. Research routes on improved sleep bruxism metrics: Toward a standardised approach. J. Sleep Res. 2021, 30, e13320. [Google Scholar] [CrossRef] [PubMed]
- Vlăduțu, D.; Popescu, S.M.; Mercuț, R.; Ionescu, M.; Scrieciu, M.; Glodeanu, A.D.; Stănuși, A.; Rîcă, A.M.; Mercuț, V. Associations between Bruxism, Stress, and Manifestations of Temporomandibular Disorder in Young Students. Int. J. Environ. Res. Public Health 2022, 19, 5415. [Google Scholar] [CrossRef] [PubMed]
- Brandão de Almeida, A.; Rodrigues, R.S.; Simão, C.; de Araújo, R.P.; Figueiredo, J. Prevalence of Sleep Bruxism Reported by Parents/Caregivers in a Portuguese Pediatric Dentistry Service: A Retrospective Study. Int. J. Environ. Res. Public Health 2022, 19, 7823. [Google Scholar] [CrossRef]
- Ommerborn, M.A.; Walentek, N.; Bergmann, N.; Franken, M.; Gotter, A.; Schäfer, R. Validation of a new diagnostic method for quantification of sleep bruxism activity. Clin. Oral Investig. 2022, 26, 4351–4359. [Google Scholar] [CrossRef]
- Rompré, P.H.; Daigle-Landry, D.; Guitard, F.; Montplaisir, J.Y.; Lavigne, G.J. Identification of a sleep bruxism subgroup with a higher risk of pain. J. Dent. Res. 2007, 86, 837–842. [Google Scholar] [CrossRef]
- Lavigne, G.J.; Rompré, P.H.; Montplaisir, J.Y. Sleep bruxism: Validity of clinical research diagnostic criteria in a controlled polysomnographic study. J. Dent. Res. 1996, 75, 546–552. [Google Scholar] [CrossRef]
- Yoshida, Y.; Suganuma, T.; Takaba, M.; Ono, Y.; Abe, Y.; Yoshizawa, S.; Sakai, T.; Yoshizawa, A.; Nakamura, H.; Kawana, F.; et al. Association between patterns of jaw motor activity during sleep and clinical signs and symptoms of sleep bruxism. J. Sleep Res. 2017, 26, 415–421. [Google Scholar] [CrossRef]
- Gupta, A.; Gupta, A.; Agarwal, L. Electromyography and its role in dentistry. IP Indian J. Clin. Exp. Dermatol. 2016, 2, 132–136. [Google Scholar]
- Nishi, S.E.; Rahman, N.A.; Basri, R.; Alam, M.K.; Noor, N.F.M.; Zainal, S.A.; Husein, A. Surface Electromyography (sEMG) Activity of Masticatory Muscle (Masseter and Temporalis) with Three Different Types of Orthodontic Bracket. Biomed. Res. Int. 2021, 2021, 6642254. [Google Scholar] [CrossRef]
- Szyszka-Sommerfeld, L.; Machoy, M.; Lipski, M.; Woźniak, K. The diagnostic value of electromyography in identifying patients with pain-related temporomandibular disorders. Front. Neurol. 2019, 10, 180. [Google Scholar] [CrossRef] [PubMed]
- Woźniak, K.; Piątkowska, D.; Lipski, M.; Mehr, K. Surface electromyography in orthodontics—A literature review. Med. Sci. Monit. 2013, 19, 416–423. [Google Scholar] [PubMed]
- Rainoldi, A.; Melchiorri, G.; Caruso, I. A method for positioning electrodes during surface EMG recordings in lower limb muscles. J. Neurosci. Methods 2004, 134, 37–43. [Google Scholar] [CrossRef]
- Chaves, T.C.; Santos Aguiar, A.; Felicio, L.R.; Greghi, S.M.; Hallak Regalo, S.C.; Bevilaqua-Grossi, D. Electromyographic ratio of masseter and anterior temporalis muscles in children with and without temporomandibular disorders. Int. J. Pediatr. Otorhinolaryngol. 2017, 97, 35–41. [Google Scholar] [CrossRef]
- Berni, K.C.; Dibai-Filho, A.V.; Pires, P.F.; Rodrigues-Bigaton, D. Accuracy of the surface electromyography RMS processing for the diagnosis of myogenous temporomandibular disorder. J. Electromyogr. Kinesiol. 2015, 25, 596–602. [Google Scholar] [CrossRef] [PubMed]
- Lauriti, L.; Motta, L.J.; Godoy, C.H.L.; Biasotto-Gonzalez, D.A.; Politti, F.; Mesquita-Ferrari, R.A.; Santos Fernandes, K.P.; Bussadori, S.K. Influence of temporomandibular disorder on temporal and masseter muscles and occlusal contacts in adolescents: An electromyographic study. BMC Musculoskelet Disord. 2014, 10, 123. [Google Scholar] [CrossRef] [PubMed]
- Al-Saleh, M.A.; Armijo-Olivo, S.; Flores-Mir, C.; Thie, N.M. Electromyography in diagnosing temporomandibular disorders. J. Am. Dent. Assoc. 2012, 143, 351–362. [Google Scholar] [CrossRef] [PubMed]
- Targalia, G.M.; Lodetti, G.; Paiva, G.; de Felício, C.M.; Sforza, C. Surface electromyographic assessment of patients with long lasting temporomandibular joint disorder pain. J. Electromyogr. Kinesiol. 2011, 21, 659–664. [Google Scholar]
- Szyszka-Sommerfeld, L.; Sycińska-Dziarnowska, M.; Budzyńska, A.; Woźniak, K. Accuracy of surface electromyography in the diagnosis of pain-related temporomandibular disorders in children with awake bruxism. J. Clin. Med. 2022, 11, 1323. [Google Scholar] [CrossRef]
- Nishi, S.E.; Basri, R.; Alam, M.K. Uses of electromyography in dentistry: An overview with meta-analysis. Eur. J. Dent. 2016, 10, 419–425. [Google Scholar] [CrossRef]
- Shiffman, S.; Stone, A.A.; Hufford, M.R. Ecological momentary assessment. Annu. Rev. Clin. Psychol. 2008, 4, 1–32. [Google Scholar] [CrossRef] [PubMed]
- Bucci, R.; Manfredini, D.; Lenci, F.; Simeon, V.; Bracci, A.; Michelotti, A. Comparison between Ecological Momentary Assessment and Questionnaire for Assessing the Frequency of Waking-Time Non-Functional Oral Behaviours. J. Clin. Med. 2022, 11, 5880. [Google Scholar] [CrossRef]
- Nykänen, L.; Manfredini, D.; Lobbezoo, F.; Kämppi, A.; Colonna, A.; Zani, A.; Almeida, A.M.; Emodi-Perlman, A.; Savolainen, A.; Bracci, A.; et al. Ecological Momentary Assessment of Awake Bruxism with a Smartphone Application Requires Prior Patient Instruction for Enhanced Terminology Comprehension: A Multi-Center Study. J. Clin. Med. 2022, 11, 3444. [Google Scholar] [CrossRef] [PubMed]
- Emodi-Perlman, A.; Manfredini, D.; Shalev, T.; Yevdayev, I.; Frideman-Rubin, P.; Bracci, A.; Arnias-Winocur, O.; Eli, I. Awake Bruxism-Single-Point Self-Report versus Ecological Momentary Assessment. J. Clin. Med. 2021, 10, 1699. [Google Scholar] [CrossRef]
- Zani, A.; Lobbezoo, F.; Bracci, A.; Ahlberg, J.; Manfredini, D. Ecological Momentary Assessment and Intervention Principles for the Study of Awake Bruxism Behaviors, Part 1: General Principles and Preliminary Data on Healthy Young Italian Adults. Front. Neurol. 2019, 10, 169. [Google Scholar] [CrossRef]
- Hugger, A.; Hugger, S.; Schindler, H.J. Surface electromyography of the masticatory muscles for application in dental practice. Current evidence and future developments. Int. J. Comput. Dent. 2008, 11, 81–106. [Google Scholar]
- Castroflorio, T.; Bracco, P.; Farina, D. Surface electromyography in the assessment of jaw elevator muscles. J. Oral Rehabil. 2008, 35, 638–645. [Google Scholar] [CrossRef]
- Oncins, M.C.; Vieira, M.M.; Bommarito, S. Eletromiografia dos músculos mastigatórios: Análise em valor original e RMS. Revista CEFAC. 2014, 16, 1215–1221. [Google Scholar] [CrossRef][Green Version]
- Yamaguchi, T.; Mikami, S.; Maeda, M.; Saito, T.; Nakajima, T.; Yachida, W.; Gotouda, A. Portable and wearable electromyographic devices for the assessment of sleep bruxism and awake bruxism: A literature review. Cranio 2020, 1, 1–9. [Google Scholar] [CrossRef]
- Prasad, S.; Paulin, M.; Cannon, R.D.; Palla, S.; Farella, M. Smartphone-assisted monitoring of masticatory muscle activity in freely moving individuals. Clin. Oral Investig. 2019, 23, 3601–3611. [Google Scholar] [CrossRef]
- Monteiro, U.M.; Soares, V.B.R.B.; Soares, C.B.R.B.; Pinto, T.C.C.; Ximenes, R.C.C.; Araújo Cairrão Rodrigues, M. Electromyographic Patterns and the Identification of Subtypes of Awake Bruxism. Front. Hum. Neurosci. 2021, 14, 601881. [Google Scholar] [CrossRef]
- Thymi, M.; Lobbezoo, F.; Aarab, G.; Ahlberg, J.; Baba, K.; Carra, M.C.; Gallo, L.M.; de Laat, A.; Manfredini, D.; Lavigne, G.; et al. Signal acquisition and analysis of ambulatory electromyographic recordings for the assessment of sleep bruxism: A scoping review. J. Oral Rehabil. 2021, 48, 846–871. [Google Scholar] [CrossRef]
- Lan, K.W.; Jiang, L.L.; Yan, Y. Comparative study of surface electromyography of masticatory muscles in patients with different types of bruxism. World J. Clin. Cases 2022, 10, 6876–6889. [Google Scholar] [CrossRef]
- Muzalev, K.; Visscher, C.M.; Koutris, M.; Lobbezoo, F. Long-term variability of sleep bruxism and psychological stress in patients with jaw-muscle pain: Report of two longitudinal clinical cases. J. Oral Rehabil. 2018, 45, 104–109. [Google Scholar] [CrossRef]
- Muzalev, K.; Lobbezoo, F.; Janal, M.N.; Raphael, K.G. Inter-episode sleep bruxism intervals and myofascial face pain. Sleep 2017, 40, zsx078. [Google Scholar] [CrossRef][Green Version]
- Stuginski-Barbosa, J.; Porporatti, A.L.; Costa, Y.M.; Svensson, P.; Conti, P.C. Diagnostic validity of the use of a portable single-channel electromyography device for sleep bruxism. Sleep Breath. 2016, 20, 695–702. [Google Scholar] [CrossRef]
- Saito, M.; Yamaguchi, T.; Mikami, S.; Watanabe, K.; Gotouda, A.; Okada, K.; Hishikawa, R.; Shibuya, E.; Shibuya, Y.; Lavigne, G. Weak association between sleep bruxism and obstructive sleep apnea. A sleep laboratory study. Sleep Breath. 2016, 20, 703–709. [Google Scholar] [CrossRef]
- Castroflorio, T.; Bargellini, A.; Rossini, G.; Cugliari, G.; Deregibus, A.; Manfredini, D. Agreement between clinical and portable EMG/ECG diagnosis of sleep bruxism. J. Oral Rehabil. 2015, 42, 759–764. [Google Scholar] [CrossRef]
- Jadidi, F.; Castrillon, E.; Svensson, P. Effect of conditioning electrical stimuli on temporalis electromyographic activity during sleep. J. Oral Rehabil. 2008, 35, 171–183. [Google Scholar] [CrossRef]
- Svensson, P.; Lavigne, G. Clinical bruxism semantics beyond academic debates: Normo- and patho-bruxism as a new proposal. J. Oral Rehabil. 2020, 47, 547–548. [Google Scholar] [CrossRef]
- Casett, E.; Réus, J.C.; Stuginski-Barbosa, J.; Porporatti, A.L.; Carra, M.C.; Peres, M.A.; de Luca Canto, G.; Manfredini, D. Validity of different tools to assess sleep bruxism: A meta-analysis. J. Oral Rehabil. 2017, 44, 722–734. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Lombardo, L.; Visentin, A.; Arreghini, A.; Siciliani, G. Correlation Between Sleep-Time Masseter Muscle Activity and Tooth Wear: An Electromyographic Study. J. Oral Facial Pain Headache 2019, 33, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Chiriac, A.M.; Mercut, V.; Popescu, S.M.; Alexandru, D.; Mercut, R.; Popescu, F.D.; Luchiancenco, D.; Resceanu, I. Applications of Factorial Analysis in the Study of Risk Factors and their Chemical Influence for Erosive Dental Wear. Revista de Chimie 2019, 70, 693–699. [Google Scholar] [CrossRef]
- Stănuși, A.; Ionescu, M.; Cerbulescu, C.; Popescu, S.M.; Osiac, E.; Mercuț, R.; Scrieciu, M.; Pascu, R.M.; Stănuși, A.Ş.; Mercuț, V. Modifications of the Dental Hard Tissues in the Cervical Area of Occlusally Overloaded Teeth Identified Using Optical Coherence Tomography. Medicina 2022, 58, 702. [Google Scholar] [CrossRef] [PubMed]
- Fluerașu, M.I.; Bocșan, I.C.; Țig, I.-A.; Iacob, S.M.; Popa, D.; Buduru, S. The Epidemiology of Bruxism in Relation to Psychological Factors. Int. J. Environ. Res. Public Health 2022, 19, 691. [Google Scholar] [CrossRef]
- Okeson, J.P.; de Leeuw, R. Differential diagnosis of temporomandibular disorders and other orofacial pain disorders. Dent. Clin. N. Am. 2011, 55, 105–120. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Lobbezoo, F. Relationship between bruxism and temporo-mandibular disorders: A systematic review of literature from 1998 to 2008. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2010, 109, e26–e50. [Google Scholar] [CrossRef]
- Feteih, R.M. Signs and symptoms of temporomandibular disorders and oral parafunctions in urban Saudi Arabian adolescents: A research report. Head Face Med. 2006, 2, 25. [Google Scholar] [CrossRef]
- Anastassaki, A.; Magnusson, T. Patients referred to a specialist clinic because of suspected temporomandibular disorders: A survey of 3194 patients in respect of diagnoses, treatments, and treatment outcome. Acta Odontol. Scand. 2004, 62, 183–192. [Google Scholar] [CrossRef]


| Value | Study Group (N = 20) | Control Group (N = 20) | p * | |
|---|---|---|---|---|
| Age | Minimum | 20 | 21 | - |
| Maximum | 35 | 53 | - | |
| Mean ± SD | 25.4 ± 3.74 | 28.6 ± 8.76 | 0.398 | |
| Gender | Females | 15 (75%) | 15 (75%) | - |
| Males | 5 (25%) | 5 (25%) | - |
| dia-BRUXO Parameter | Study Group | Control Group | p | ||||
|---|---|---|---|---|---|---|---|
| Min | Max | Mean ± SD | Min | Max | Mean ± SD | ||
| Sleep duration (%) | 24.000 | 48.900 | 34.790 ± 7.670 | 19.200 | 50.700 | 30.485 ± 8.600 | 0.103 * |
| Awake duration (%) | 51.100 | 76.000 | 64.615x ± 7.993 | 49.300 | 80.800 | 69.515 ± 8.600 | 0.070 * |
| Detachment duration (%) | 0.000 | 17.400 | 1.430 ± 4.152 | 0.000 | 7.100 | 0.530 ± 1.633 | 0.058 ** |
| dia-BRUXO Parameter | Study Group | Control Group | p | ||||
|---|---|---|---|---|---|---|---|
| Min | Max | Mean ± SD | Min | Max | Mean ± SD | ||
| SB—Clenching | 9 | 96 | 37.850 ± 23.374 | 0 | 37 | 11.050 ± 11.133 | <0.005 * |
| SB—Grinding | 2 | 201 | 39.950 ± 50.784 | 0 | 21 | 5.150 ± 5.696 | <0.005 * |
| SB—Others | 0 | 127 | 9.850 ± 28.380 | 0 | 4 | 0.500 ± 1.277 | 0.008 * |
| AB—Clenching | 17 | 533 | 204.250 ± 143.934 | 13 | 227 | 76.250 ± 65.240 | 0.002 * |
| AB—Grinding | 1 | 162 | 42.750 ± 45.163 | 0 | 33 | 8.350 ± 9.155 | 0.002 * |
| AB—Others | 0 | 50 | 11.600 ± 14.486 | 0 | 17 | 7.100 ± 5.261 | 0.860 * |
| dia-BRUXO Parameter | Study Group | Control Group | p | ||||
|---|---|---|---|---|---|---|---|
| Min | Max | Mean ± SD | Min | Max | Mean ± SD | ||
| SB—BWI (%) | 0.134 | 1.283 | 0.470 ± 0.330 | 0.000 | 0.294 | 0.098 ± 0.085 | <0.005 * |
| SB—BTI (%) | 0.294 | 3.236 | 1.054 ± 0.790 | 0.000 | 0.692 | 0.233 ± 0.200 | <0.005 * |
| AB—BWI (%) | 0.094 | 4.480 | 1.177 ± 1.028 | 0.078 | 0.853 | 0.310 ± 0.214 | <0.005 * |
| AB—BTI (%) | 0.279 | 10.103 | 2.788 ± 2.380 | 0.239 | 1.720 | 0.721 ± 0.421 | <0.005 * |
| dia-BRUXO Parameter | Study Group | Control Group | p | ||||
|---|---|---|---|---|---|---|---|
| Min | Max | Mean ± SD | Min | Max | Mean ± SD | ||
| SB—BPI (%) | 0.240 | 2.542 | 0.860 ± 0.632 | 0.000 | 0.560 | 0.188 ± 0.162 | <0.005 * |
| AB—BPI (%) | 0.217 | 8.230 | 2.251 ± 1.925 | 0.187 | 1.431 | 0.585 ± 0.350 | <0.005 * |
| dia-BRUXO Parameter | Study Group | Control Group | p | ||||
|---|---|---|---|---|---|---|---|
| Min | Max | Mean ± SD | Min | Max | Mean ± SD | ||
| SB—MWI (%) | 0.375 | 2.440 | 0.964 ± 0.620 | 0.097 | 0.625 | 0.328 ± 0.131 | <0.005 * |
| SB—MTI (%) | 1.265 | 9.612 | 3.351 ± 2.620 | 0.580 | 2.471 | 1.318 ± 0.469 | <0.005 * |
| SB—MPI (%) | 0.968 | 7.221 | 2.555 ± 1.940 | 0.419 | 1.831 | 0.988 ± 0.353 | <0.005 * |
| AB—MWI (%) | 1.571 | 11.693 | 4.737 ± 2.372 | 1.565 | 4.339 | 2.772 ± 0.716 | 0.001 * |
| AB—MTI (%) | 6.747 | 31.270 | 17.015 ± 6.725 | 5.909 | 15.246 | 11.830 ± 2.761 | 0.005 * |
| AB—MPI (%) | 5.021 | 24.745 | 12.923 ± 5.231 | 4.461 | 11.320 | 8.810 ± 2.026 | 0.004 * |
| Parameter | Value | Study Group (N = 20) | Control Group (N = 20) | p * |
|---|---|---|---|---|
| Tooth wear | No | 8 (40%) | 17 (85%) | 0.003 |
| Yes | 12 (60%) | 3 (15%) | ||
| Abfractions | No | 18 (90%) | 20 (100%) | 0.244 |
| Yes | 2 (10%) | 0 (0%) | ||
| Masticatory muscle pain | No | 3 (15%) | 20 (100%) | <0.005 |
| Yes | 17 (85%) | 0 (0%) | ||
| TMJ disorders | No | 15 (75%) | 19 (95%) | 0.077 |
| Yes | 5 (25%) | 1 (5%) | ||
| Headache/neck pain | No | 13 (65%) | 20 (100%) | 0.004 |
| Yes | 7 (35%) | 0 (0%) | ||
| Interocclusal appliance | No | 17 (85%) | 20 (100%) | 0.115 |
| Yes | 3 (15%) | 0 (0%) | ||
| Snore | No | 14 (70%) | 19 (95%) | 0.046 |
| Yes | 6 (30%) | 1 (5%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vlăduțu, D.E.; Ionescu, M.; Mercuț, R.; Noveri, L.; Lăzărescu, G.; Popescu, S.M.; Scrieciu, M.; Manolea, H.O.; Iacov Crăițoiu, M.M.; Ionescu, A.G.; et al. Ecological Momentary Assessment of Masseter Muscle Activity in Patients with Bruxism. Int. J. Environ. Res. Public Health 2023, 20, 581. https://doi.org/10.3390/ijerph20010581
Vlăduțu DE, Ionescu M, Mercuț R, Noveri L, Lăzărescu G, Popescu SM, Scrieciu M, Manolea HO, Iacov Crăițoiu MM, Ionescu AG, et al. Ecological Momentary Assessment of Masseter Muscle Activity in Patients with Bruxism. International Journal of Environmental Research and Public Health. 2023; 20(1):581. https://doi.org/10.3390/ijerph20010581
Chicago/Turabian StyleVlăduțu, Diana Elena, Mihaela Ionescu, Răzvan Mercuț, Lorenzo Noveri, Grigore Lăzărescu, Sanda Mihaela Popescu, Monica Scrieciu, Horia Octavian Manolea, Monica Mihaela Iacov Crăițoiu, Alin Gabriel Ionescu, and et al. 2023. "Ecological Momentary Assessment of Masseter Muscle Activity in Patients with Bruxism" International Journal of Environmental Research and Public Health 20, no. 1: 581. https://doi.org/10.3390/ijerph20010581
APA StyleVlăduțu, D. E., Ionescu, M., Mercuț, R., Noveri, L., Lăzărescu, G., Popescu, S. M., Scrieciu, M., Manolea, H. O., Iacov Crăițoiu, M. M., Ionescu, A. G., & Mercuț, V. (2023). Ecological Momentary Assessment of Masseter Muscle Activity in Patients with Bruxism. International Journal of Environmental Research and Public Health, 20(1), 581. https://doi.org/10.3390/ijerph20010581







