A Novel Empowerment System for Patients Living with a Chronic Disease in a Precarious Context
Abstract
:1. Introduction
2. Discussion
2.1. Combination of the eHealth CCM and SBNH
2.1.1. Shared Assumptions
2.1.2. Cultural Applicability
2.1.3. Disciplinary Boundaries
2.1.4. Nursing Education
2.1.5. Focus of Care
2.1.6. Process or Product Distinction
2.1.7. Shared Values
2.1.8. Scientific Orientation
2.2. Results of the Neith Program
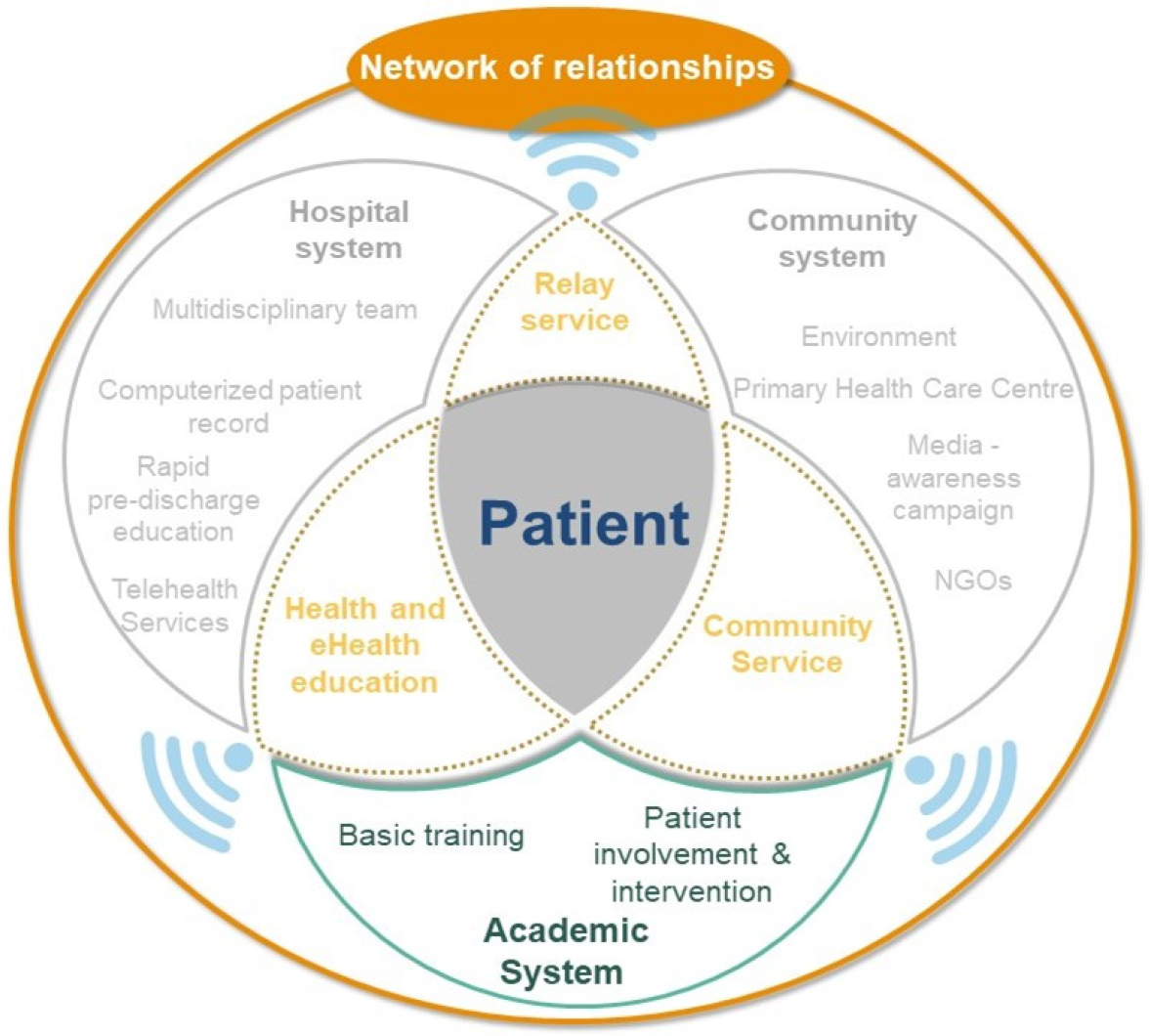
2.3. Components of a System Promoting the Empowerment of Patients with Chronic Disease Living in a Precarious Context
2.3.1. Network of Relationships
Relay Services to the Community System
Predischarge Education in Hospital Systems
Incorporating Community Services within Academic Institutions
2.3.2. Contextualization and Co-Management of Educational Sessions
3. Conclusions
4. Limitations and Further Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Non Communicable Diseases. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 15 September 2022).
- Furtado, L.G.; da Nóbrega, M.M.L. Model of care in chronic disease: Inclusion of a theory of nursing. Texto Contexto-Enferm. 2013, 22, 1197–1204. Available online: http://www.scielo.br/scielo.php?script=sci_abstract&pid=S0104-07072013000400039&lng=en&nrm=iso&tlng=en (accessed on 3 March 2022). [CrossRef]
- Wagner, E.H.; Austin, B.T.; Von Korff, M. Organizing care for patients with chronic illness. Milbank Q. 1996, 74, 511–544. Available online: https://www.jstor.org/stable/3350391 (accessed on 2 February 2022). [CrossRef] [PubMed]
- Gee, P.M.; Greenwood, D.A.; Paterniti, D.A.; Ward, D.; Miller, L.M.S. The eHealth enhanced chronic care model: A theory derivation approach. J. Med. Int. Res. 2015, 17, e86. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4398883/ (accessed on 29 February 2020). [CrossRef] [PubMed]
- Gottlieb, L.N. Strengths-based nursing. Am. J. Nurs. 2014, 114, 24–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puchalski Ritchie, L.M.; Khan, S.; Moore, J.E.; Timmings, C.; van Lettow, M.; Vogel, J.P.; Khan, D.N.; Mbaruku, G.; Mrisho, M.; Mugerwa, K.; et al. Low- and middle-income countries face many common barriers to implementation of maternal health evidence products. J. Clin. Epidemiol. 2016, 76, 229–237. Available online: https://www.jclinepi.com/article/S0895-4356(16)00154-2/abstract (accessed on 29 February 2020). [CrossRef] [PubMed] [Green Version]
- Fernagu, S. Les capabilités au prisme de la capacité à s’autodéterminer: Les Clubs de dirigeants de PME. Form. Empl. Rev. Française De Sci. Soc. 2018, 23, 231–254. Available online: https://journals.openedition.org/formationemploi/5943#xd_co_f=OWY1Yzg2ZmYtNjI0NS00ZmFkLWI3M2YtOWUwNzEwOTM5YzU2~ (accessed on 23 March 2022). [CrossRef]
- Neuman, B.; Fawcett, J. The Neuman Systems Model, 5th ed.; Pearson: Upper Saddle River, NJ, USA, 2011. [Google Scholar]
- Kolcaba, K.; Kolcaba, R. Integrative Theorizing: Linking Middle Range Nursing Theories with the Neuman System Model. In The Neuman System Model, 5th ed.; Neuman, B., Fawcett, J., Eds.; Pearson Education: London, UK, 2011. [Google Scholar]
- Gottlieb, L.N. Les Soins Infirmiers Fondés sur les Forces; Renouveau Pedagogique INC: Montréal, QC, Canada, 2014; 457 p. [Google Scholar]
- Sebai, J.; Yatim, F. Approche centrée sur le patient et nouvelle gestion publique : Confluence et paradoxe. Sante Publique 2018, 30, 517–526. Available online: https://www.cairn.info/revue-sante-publique-2018-4-page-517.htm (accessed on 1 May 2020). [CrossRef] [PubMed]
- Nohra, R.G.; Bou Serhal, R.; Sacre, H.; Salameh, P.; Rothan-Tondeur, M. Effective components of self-management programs for chronic obstructive pulmonary disease patients: Scoping review. Adv. Respir. Med. 2020, 88, 223–232. Available online: https://journals.viamedica.pl/advances_in_respiratory_medicine/article/view/ARM.2020.0117 (accessed on 2 September 2021). [CrossRef] [PubMed]
- Nohra, R.G.; Morvillers, J.M.; Sacre, H.; Salameh, P.; Rothan-Tondeur, M. Living with chronic obstructive pulmonary disease in Lebanon: A phenomenological study. East. Mediterr. Health J. 2022, 28, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Nohra, R.G.; Chaaban, T.; Sacre, H.; Salameh, P.; Aoun Bacha, Z.; Le Bon Chami, B.; Rizk, F.A.; Makhlouf, P.; Rothan-Tondeur, M. Evaluating the feasibility and pretesting the impact of an educational and telemonitoring program for COPD patients in Lebanon. Int. J. Chronic Obstr. Pulm. Dis. 2022, 17, 949–965. Available online: https://www.dovepress.com/evaluating-the-feasibility-and-pretesting-the-impact-of-an-educational-peer-reviewed-fulltext-article-COPD (accessed on 22 May 2022). [CrossRef] [PubMed]
- Nohra, R.G.; Sacre, H.; Salameh, P.; Rothan-Tondeur, M. Evaluating the feasibility, acceptability and pre testing the impact of a self-management and tele monitoring program for chronic obstructive pulmonary disease patients in Lebanon: Protocol for a feasibility study. Medicine 2020, 99, e19021. Available online: https://journals.lww.com/md-journal/Fulltext/2020/02070/Evaluating_the_feasibility,_acceptability_and_pre.29.aspx (accessed on 5 August 2021). [CrossRef] [PubMed]
- Deci, E.L.; Ryan, R.M. Intrinsic Motivation and Self-Determination in Human Behavior; Springer: Boston, MA, USA, 1985; Available online: http://link.springer.com/10.1007/978-1-4899-2271-7 (accessed on 23 March 2022).
- Wehmeyer, M.L.; Abery, B.H.; Mithaug, D.E.; Stancliffe, R.J. Theory in Self-Determination: Foundations for Educational Practice; Charles C Thomas Pub Ltd.: Springfield, IL, USA, 2003; 338 p. [Google Scholar]
- D’Ivernois, J.F.; Gagnayre, R.; Groupe de travail de l’IPCEM. Compétences d’adaptation à la maladie du patient: Une proposition. Ther. Patient Educ. 2011, 3, S201–S205. [Google Scholar] [CrossRef]
- Helou, S.; El Helou, E.; Abou-Khalil, V.; Wakim, J.; El Helou, J.; Daher, A.; El Hachem, C. The effect of the COVID-19 pandemic on physicians’ use and perception of telehealth: The case of Lebanon. Int. J. Environ. Res. Public Health 2020, 17, 4866. [Google Scholar] [CrossRef] [PubMed]
- Van Cauwenberge, H.; Delroualle, A.; Hans, B.; Nguyen Dang, D.; Corhay, J.L.; Louis, R.; Gillet, P. Telemonitoring of severe COPD patients. Rev. Médicale De Liège 2019, 74, 566–571. [Google Scholar]
- Albano, M.G.; Gagnayre, R.; de Andrade, V.; d’Ivernois, J.F. L’éducation précédant la sortie de l’hôpital: Nouvelle forme d’éducation thérapeutique. Critères de qualité et perspectives d’application à notre contexte. Rech. En Soins Infirm. 2020, 141, 70–77. Available online: https://www.cairn.info/revue-recherche-en-soins-infirmiers-2020-2-page-70.htm (accessed on 23 March 2022). [CrossRef]
- Sink, D.W.; Hope, S.A.E.; Hagadorn, J.I. Nurse:patient ratio and achievement of oxygen saturation goals in premature infants. Arch. Dis. Child. Fetal Neonatal Ed. 2011, 96, F93–F98. Available online: https://fn.bmj.com/content/96/2/F93 (accessed on 5 December 2022). [CrossRef]
- Organisation Mondiale de la Santé. Éducation Thérapeutique du Patient: Programme de Formation Continue Pour les Professionnels de Soins Dans le Domaine de la Prévention des Maladies Chroniques, Recommandations d’un Groupe de Travail de l’OMS; Bureau Régional Pour l’Europe: Copenhague, Denmark, 1998. [Google Scholar]
- Richard, E.; Evans, T.; Williams, B. Nursing students’ perceptions of preparation to engage in patient education. Nurs. Educ. Pract. 2018, 28, 1–6. Available online: https://www.sciencedirect.com/science/article/pii/S1471595317306212 (accessed on 24 March 2022). [CrossRef] [PubMed]
- Boelen, C.; Heck, J.E.; World Health Organization, Division of Development of Human Resources for Health. Defining and Measuring the Social Accountability of Medical Schools; World Health Organization: Geneva, Switzerland, 1995; Report No.: WHO/HRH/95.7; Unpublished; Available online: https://apps.who.int/iris/handle/10665/59441 (accessed on 22 March 2022).
- Grimaldi, A. Les défis de la maladie chronique. J. De Médecine Vasc. 2019, 44, 115. Available online: https://www.em-consulte.com/article/1280612/article/les-defis-de-la-maladie-chronique (accessed on 23 March 2022). [CrossRef]
- Bureau-Point, E.; Hermann-Mesfen, J. Les Patients Contemporains face à la Démocratie Sanitaire. Anthropologie & Santé Revue Internationale Francophone D’anthropologie de la Santé. Rev. Int. Francoph. D’anthropologie De La St. 2014. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nohra, R.G.; Rothan-Tondeur, M. A Novel Empowerment System for Patients Living with a Chronic Disease in a Precarious Context. Int. J. Environ. Res. Public Health 2023, 20, 601. https://doi.org/10.3390/ijerph20010601
Nohra RG, Rothan-Tondeur M. A Novel Empowerment System for Patients Living with a Chronic Disease in a Precarious Context. International Journal of Environmental Research and Public Health. 2023; 20(1):601. https://doi.org/10.3390/ijerph20010601
Chicago/Turabian StyleNohra, Rita Georges, and Monique Rothan-Tondeur. 2023. "A Novel Empowerment System for Patients Living with a Chronic Disease in a Precarious Context" International Journal of Environmental Research and Public Health 20, no. 1: 601. https://doi.org/10.3390/ijerph20010601



