Thermophysiological and Perceptual Responses of Amateur Healthcare Workers: Impacts of Ambient Condition, Inner-Garment Insulation and Personal Cooling Strategy
Abstract
1. Introduction
2. Methods
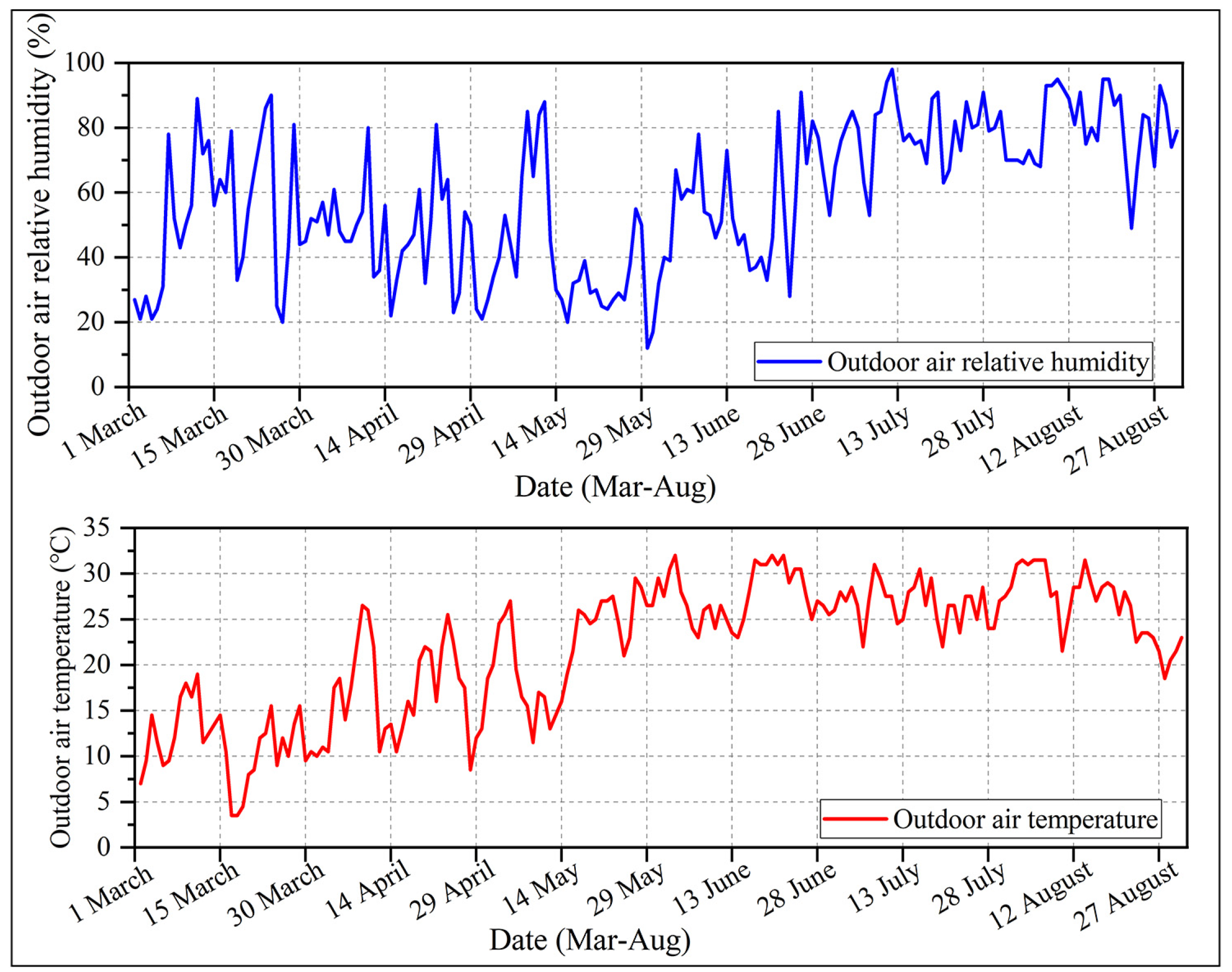
2.1. Field Study Conditions and Instruments
2.2. Experimental Environment and Instruments
2.3. Experimental PPE and Ensembles
2.4. Experimental Setup
2.5. Evaluation Indices
2.6. Statistical Analysis
3. Results
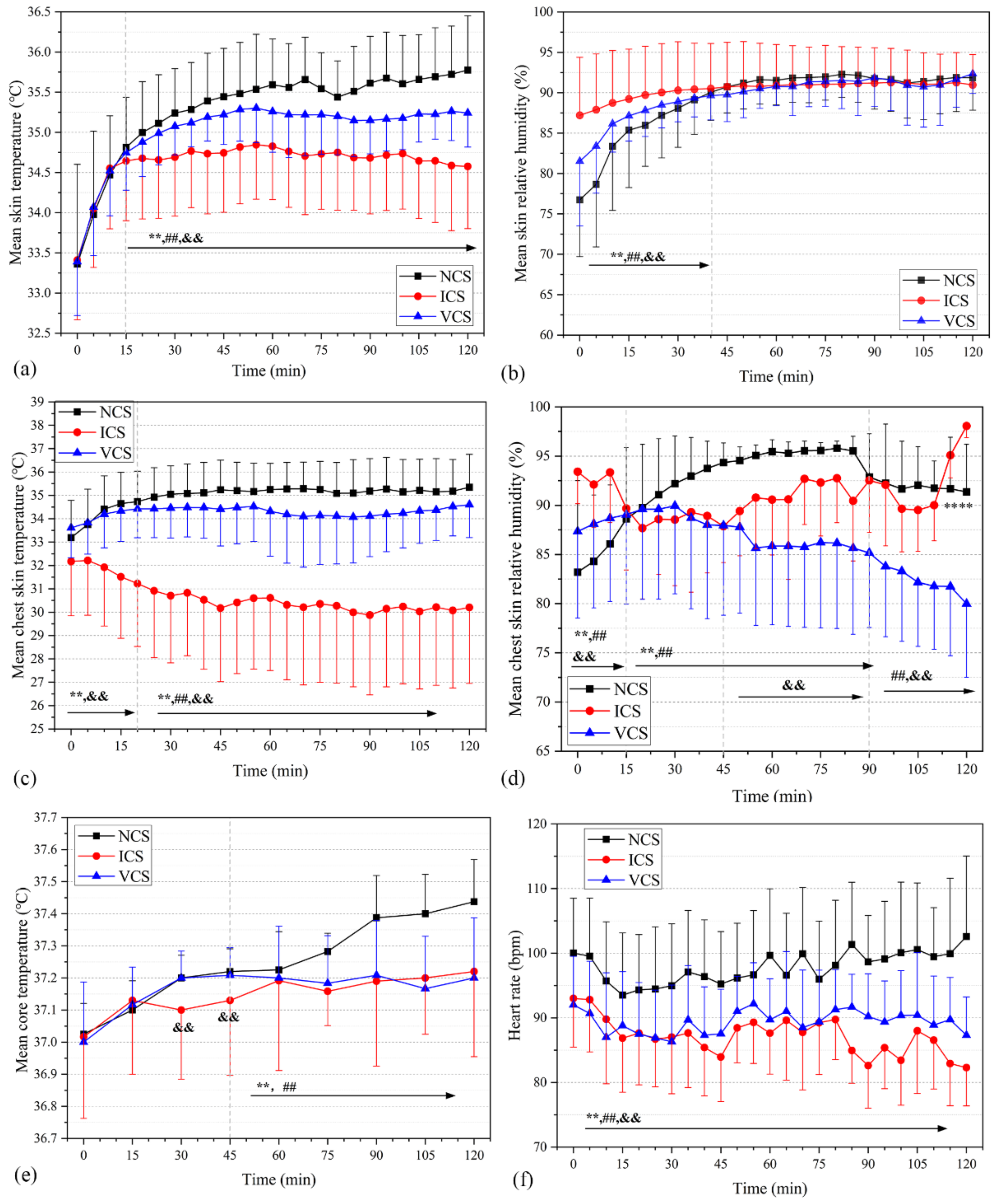
3.1. Physiological Responses in Basic Trials
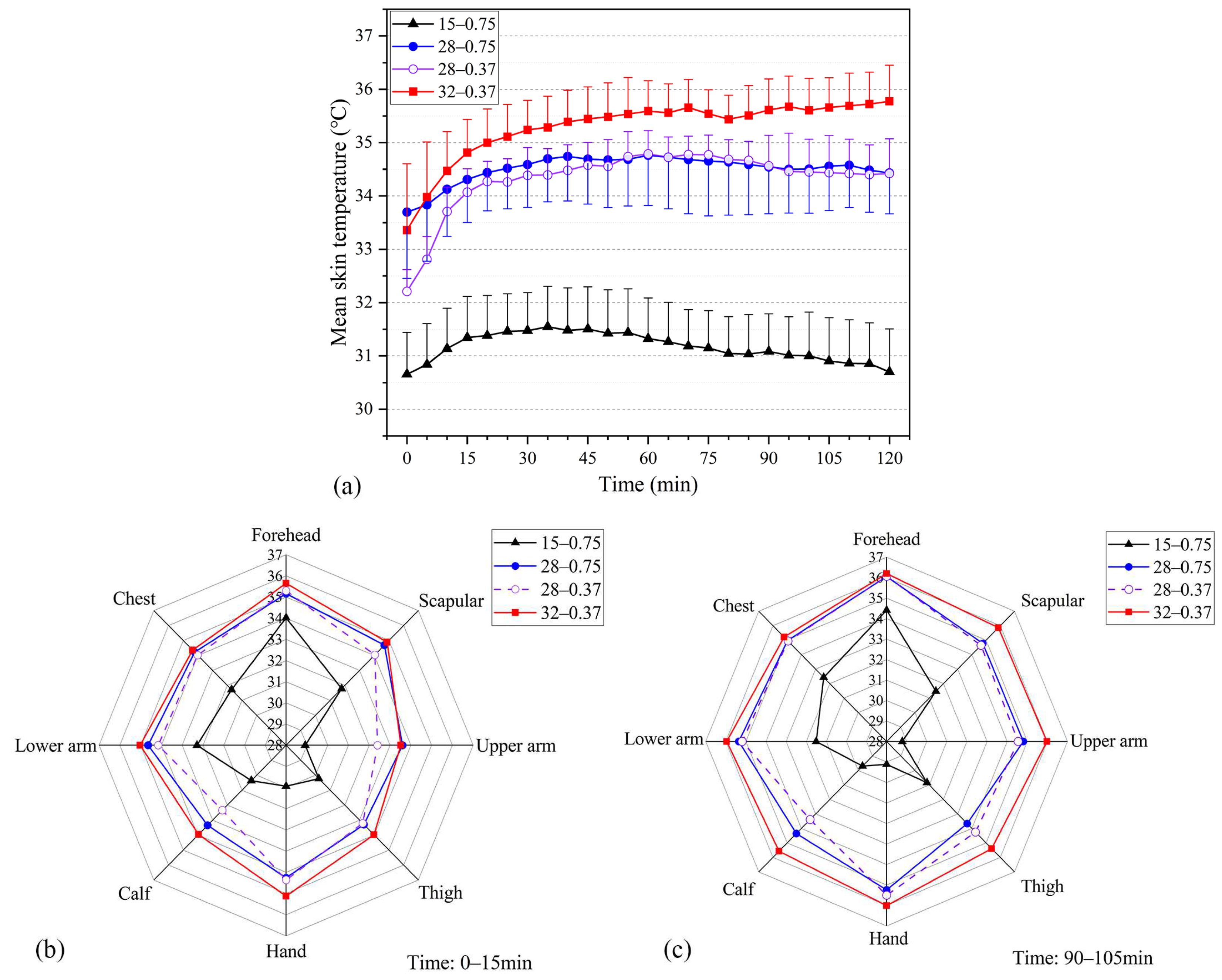
3.1.1. Mean and Local Skin Temperatures
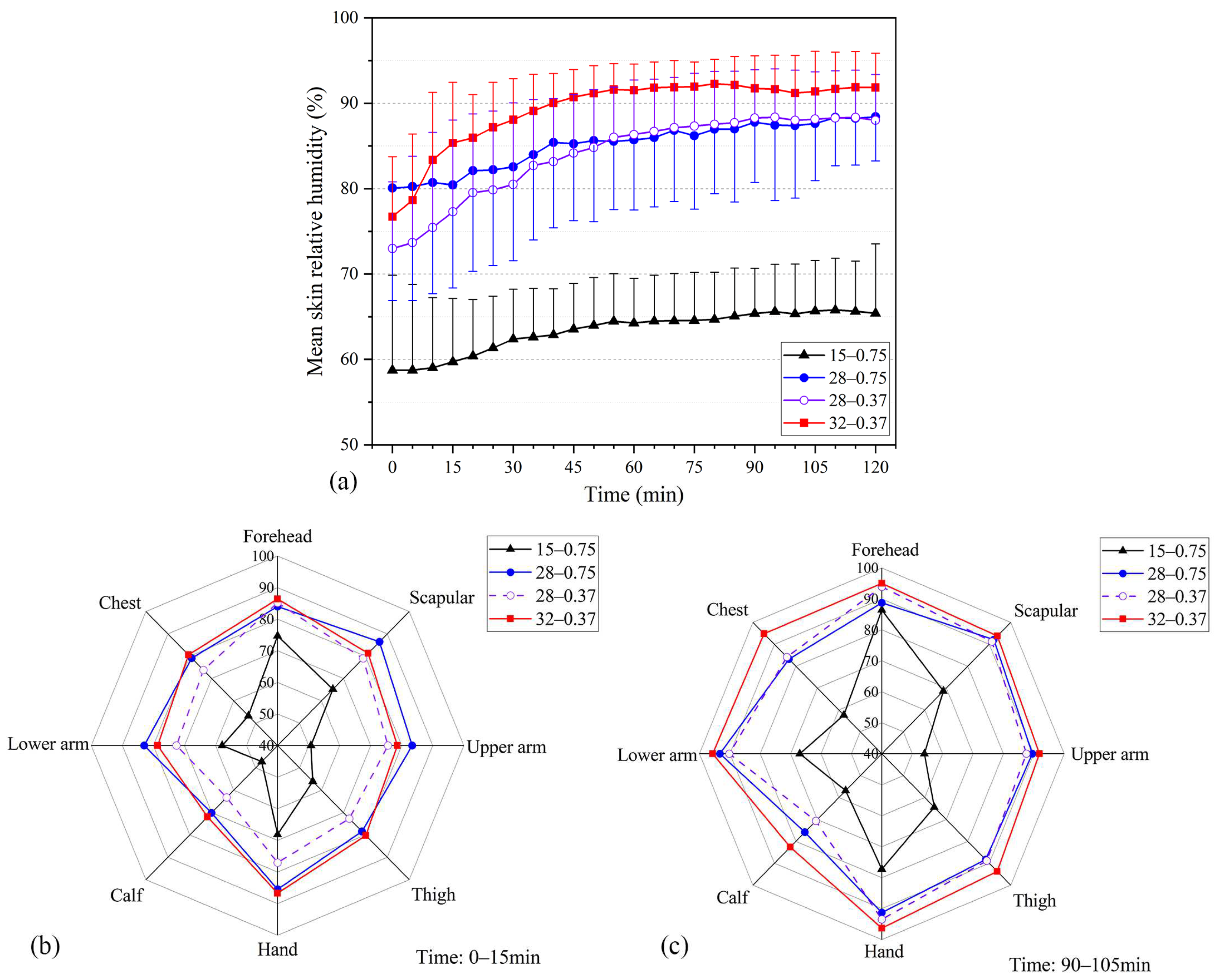
3.1.2. Skin Relative Humidity
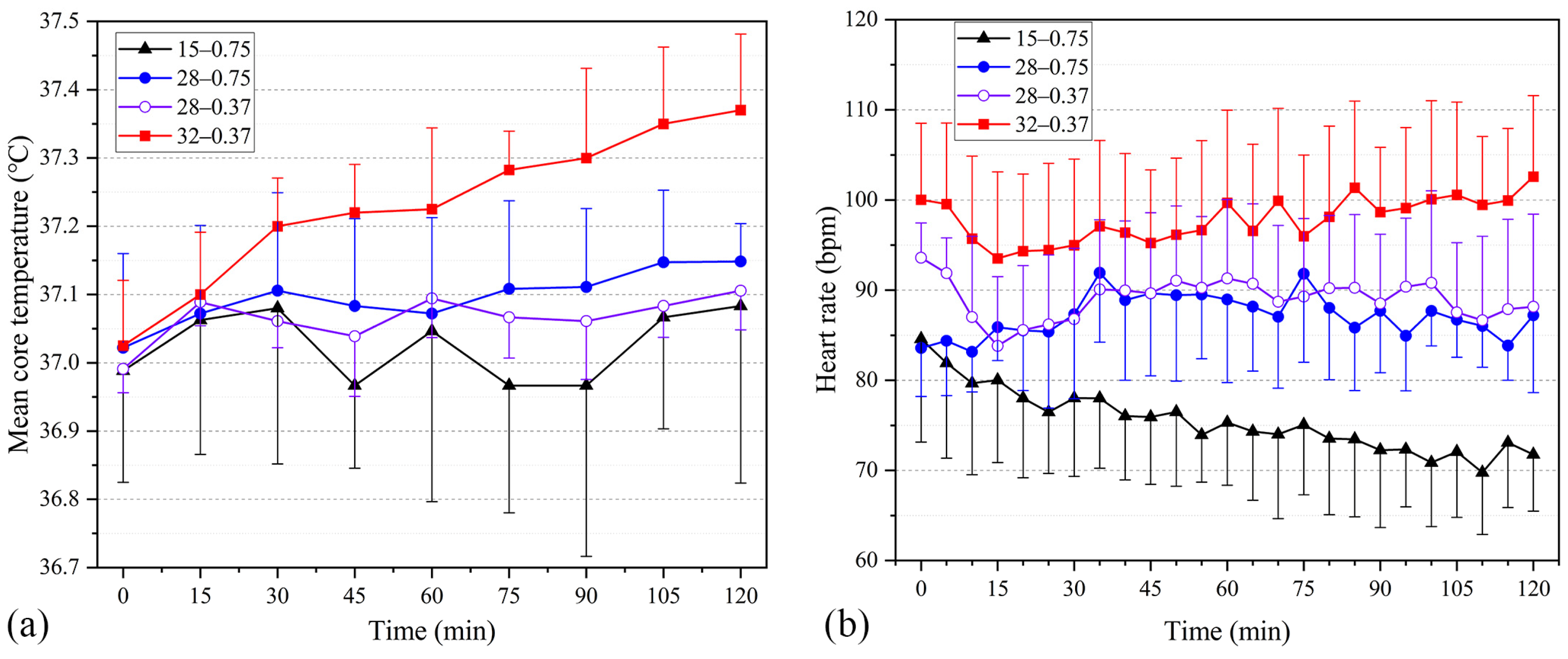
3.1.3. Core Temperature and Heart Rate
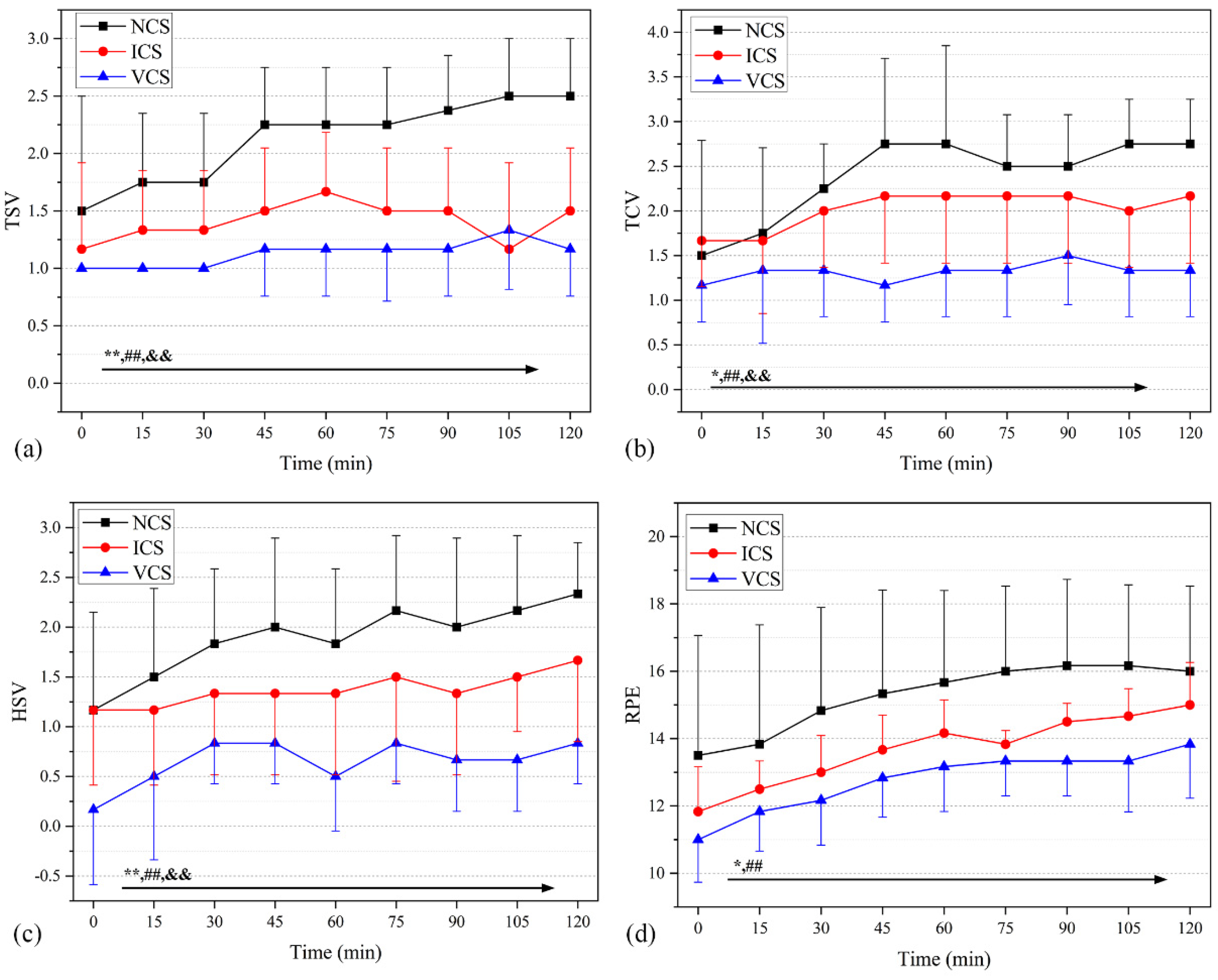
3.2. Perceptual Responses in Basic Trials
3.3. Correlation between Physiological Parameters and WBGT (or Perceptual Responses)
3.4. Cooling Trials
3.4.1. Physiological Responses
3.4.2. Perceptual Responses
4. Discussion and Limitations
5. Conclusions
- (1)
- Tskin was 31.2 °C at WBGT = 15 °C with 0.75 clo inner garments. The low temperature environment significantly affected the skin temperature at the scapula, arm, hand, and leg. Hskin was maintained at 60–65% and HR was about 75.5 bpm, all of which were within the thermal comfort zone.
- (2)
- At WBGT = 28 °C, Tskin plateaued at around 34.7 °C, and participants reported experiencing “hot” thermal sensations. Reducing the thermal resistance of the inner garment only slightly affected the participants’ physiological parameters, but the subjective evaluation index decreased as the thermal resistance of the inner garment was reduced. The insulation reduction of inner garments from 0.75 clo to 0.37 clo did not significantly improve the participants’ physiological thermal comfort.
- (3)
- At WBGT = 32 °C, Tskin was maintained at 35.2–35.7 °C, Hskin was nearly 90% RH, Tcore exceeded 37.1 °C, and the mean HR was 91.9 bpm. These results indicate that such a working scenario was uncompensable from the heat stress perspective. Hence, personal cooling to mitigate heat stress was required.
- (4)
- Significant positive correlations were found between Tskin, Hskin, HR, Tcore, and WBGT values at the p ≤ 0.01 level, with Tskin exhibiting the highest correlation coefficient with WBGT (r = 0.92), indicating that Tskin was more significantly affected by the thermal stress of the external environment. Tskin, Hskin, HR, Tcore were positively correlated with TSV, TCV, RPE (p < 0.01).
- (5)
- When compared with that in NCS (no cooling), mean skin temperatures in ICS and VCS were reduced by 0.61 °C and 0.22 °C, respectively; chest temperature was as low as 30.6 °C; HRs were reduced by 10.7 and 8.5 bpm; and core temperatures were maintained at 37.2 °C with both personalized cooling strategies. Hskin in ICS was high because of moisture condensation from the ice packs. Perceptual responses in ICS and VCS improved significantly throughout the entire field trials, with VCS outperforming ICS in the individual cooling effect.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Nomenclature
| Hskin | mean skin relative humidity, % |
| Icl | thermal resistance of clothing, clo |
| RH | relative humidity, % |
| ta | dry bulb temperature, °C |
| Tcore | mean core temperature, °C |
| tg | black globe temperature, °C |
| Tskin | mean skin temperature, °C |
| tw | wet bulb temperature, °C |
| v | air velocity, m/s |
| Abbreviation | |
| COVID-19 | Coronavirus Disease-2019 |
| HR | heart rate, bpm |
| HSV | humid sensation votes |
| ICS | ice bag cooling system |
| NCS | no cooling system |
| RPE | Borg’s rating of perceived exertion |
| TCV | thermal comfort votes |
| TEV | thermal expectations votes |
| TSV | thermal sensation votes |
| VCS | ventilation cooling system |
| WBGT | wet bulb globe temperature, °C |
| Subscripts | |
| cl | a set of clothing |
| i | single piece clothes |
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Stratton, C.W.; Tang, Y.W. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J. Med. Virol. 2020, 92, 401–402. [Google Scholar] [CrossRef] [PubMed]
- Higo, H.; Taguchi, Y.; Suzaki, N.; Nagata, T.; Marukawa, M. Indications for SARS-CoV-2 nucleic acid amplification test for areas with low endemicity. J. Infect. Chemother. 2022, 28, 238–241. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef]
- Aparicio Betancourt, M.; Duarte-Díaz, A.; Vall-Roqué, H.; Seils, L.; Orrego, C.; Perestelo-Pérez, L.; Barrio-Cortes, J.; Beca-Martínez, M.T.; Molina Serrano, A.; Bermejo-Caja, C.J.; et al. Global healthcare needs related to COVID-19: An evidence map of the first year of the pandemic. Int. J. Environ. Res. Public Health 2022, 19, 10332. [Google Scholar] [CrossRef]
- Kim, I.H.; Kang, B.H.; Seo, S.H.; Park, Y.E.; Kim, G.J.; Lee, S.W.; Jang, J.H.; Jo, S.K.; Jeon, J.H.; Kim, J.M.; et al. Early laboratory preparedness of the Korea disease control and prevention agency and response to unknown pneumonia outbreak from Wuhan, China, in January 2020. Ann. Lab. Med. 2021, 41, 532–539. [Google Scholar] [CrossRef]
- Hui, D.S.; E, I.A.; Madani, T.A.; Ntoumi, F.; Kock, R.; Dar, O.; Ippolito, G.; McHugh, T.D.; Memish, Z.A.; Drosten, C.; et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—The latest 2019 novel coronavirus outbreak in Wuhan, China. Int. J. Infect. Dis. 2020, 91, 264–266. [Google Scholar] [CrossRef]
- Ruskin, K.J.; Ruskin, A.C.; Musselman, B.T.; Harvey, J.R.; Nesthus, T.E.; O’Connor, M. COVID-19, personal protective equipment, and human performance. Anesthesiology 2021, 134, 518–525. [Google Scholar] [CrossRef]
- Lan, J.; Song, Z.; Miao, X.; Li, H.; Li, Y.; Dong, L.; Yang, J.; An, X.; Zhang, Y.; Yang, L.; et al. Skin damage among health care workers managing coronavirus disease-2019. J. Am. Acad. Dermatol. 2020, 82, 1215–1216. [Google Scholar] [CrossRef]
- Ong, J.J.Y.; Bharatendu, C.; Goh, Y.; Tang, J.Z.Y.; Sooi, K.W.X.; Tan, Y.L.; Tan, B.Y.Q.; Teoh, H.L.; Ong, S.T.; Allen, D.M.; et al. Headaches associated with personal protective equipment—A cross-sectional study among frontline healthcare workers during COVID-19. Headache 2020, 60, 864–877. [Google Scholar] [CrossRef]
- Jose, S.; Cyriac, M.C.; Dhandapani, M. Health problems and skin damages caused by personal protective equipment: Experience of frontline nurses caring for critical COVID-19 patients in intensive care units. Indian J. Crit. Care Med. 2021, 25, 134–139. [Google Scholar] [PubMed]
- Lee, H.C.; Goh, C.L. ’Occupational dermatoses from Personal Protective Equipment during the COVID-19 pandemic in the tropics—A Review’. J. Eur. Acad. Dermatol. Venereol. 2021, 35, 589–596. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Venugopal, V.; Latha, P.K.; Alhadad, S.B.; Leow, C.H.W.; Goh, N.Y.; Tan, E.; Kjellstrom, T.; Morabito, M.; Lee, J.K.W. Heat stress and thermal perception amongst healthcare workers during the COVID-19 pandemic in India and Singapore. Int. J. Environ. Res. Public Health 2020, 17, 8100. [Google Scholar] [CrossRef] [PubMed]
- Davey, S.L.; Lee, B.J.; Robbins, T.; Randeva, H.; Thake, C.D. Heat stress and PPE during COVID-19: Impact on healthcare workers’ performance, safety and well-being in NHS settings. J. Hosp. Infect. 2021, 108, 185–188. [Google Scholar] [CrossRef]
- Bongers, C.; de Korte, J.Q.; Zwartkruis, M.; Levels, K.; Kingma, B.R.M.; Eijsvogels, T.M.H. Heat strain and use of heat mitigation strategies among COVID-19 healthcare workers wearing personal protective equipment-a retrospective study. Int. J. Environ. Res. Public Health 2022, 19, 1905. [Google Scholar] [CrossRef] [PubMed]
- Messeri, A.; Bonafede, M.; Pietrafesa, E.; Pinto, I.; de’Donato, F.; Crisci, A.; Lee, J.K.W.; Marinaccio, A.; Levi, M.; Morabito, M.; et al. A web survey to evaluate the thermal stress associated with personal protective equipment among healthcare workers during the COVID-19 pandemic in Italy. Int. J. Environ. Res. Public Health 2021, 18, 3861. [Google Scholar] [CrossRef]
- Westermann, C.; Zielinski, N.; Altenburg, C.; Dulon, M.; Kleinmüller, O.; Kersten, J.F.; Nienhaus, A. Prevalence of adverse skin reactions in nursing staff due to personal protective equipment during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2022, 19, 12530. [Google Scholar] [CrossRef]
- Loibner, M.; Hagauer, S.; Schwantzer, G.; Berghold, A.; Zatloukal, K. Limiting factors for wearing personal protective equipment (PPE) in a health care environment evaluated in a randomised study. PLoS ONE 2019, 14, e0210775. [Google Scholar] [CrossRef]
- Grélot, L.; Koulibaly, F.; Maugey, N.; Janvier, F.; Foissaud, V.; Aletti, M.; Savini, H.; Cotte, J.; Dampierre, H.; Granier, H.; et al. Moderate thermal strain in healthcare workers wearing personal protective equipment during treatment and care activities in the context of the 2014 Ebola Virus Disease outbreak. J. Infect. Dis. 2016, 213, 1462–1465. [Google Scholar] [CrossRef]
- Mao, Y.; Zhu, Y.; Guo, Z.; Zheng, Z.; Fang, Z.; Chen, X. Experimental investigation of the effects of personal protective equipment on thermal comfort in hot environments. Build. Environ. 2022, 222, 109352. [Google Scholar] [CrossRef]
- Zhao, Y.; Liu, J.; Kim, M.K.; Zhou, S.; Du, Y. Experimental investigation on thermal comfort of COVID-19 nucleic acid sampling staff in hot and humid environment: A pilot study of university students. Appl. Sci. 2021, 11, 11492. [Google Scholar] [CrossRef]
- Bartkowiak, G.; Dąbrowska, A.; Marszałek, A. Assessment of the human responses to the influence of personal liquid cooling system in the hot environment. Int. J. Cloth Sci. Technol. 2014, 26, 145–163. [Google Scholar] [CrossRef]
- Hou, J.; Yang, Z.; Xu, P.; Huang, G. Design and performance evaluation of novel personal cooling garment. Appl. Therm. Eng. 2019, 154, 131–139. [Google Scholar] [CrossRef]
- Teunissen, L.P.; Wang, L.C.; Chou, S.N.; Huang, C.H.; Jou, G.T.; Daanen, H.A. Evaluation of two cooling systems under a firefighter coverall. Appl. Ergon. 2014, 45, 1433–1438. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Chow, C.S.-W.; Zheng, Q.; Ke, Y.; Yang, B.; Zheng, X.; Noor, N.; Zhang, Q.; Zhang, C.; Zhou, H. On the use of personal cooling suits to mitigate heat strain of mascot actors in a hot and humid environment. Energy Build. 2019, 205, 109561. [Google Scholar] [CrossRef]
- Su, X.; Tian, S.; Li, H.; Zhang, X.; Shao, X.; Gao, J.; Ye, H. Thermal and humid environment improvement of the protective clothing for medical use with a portable cooling device: Analysis of air supply parameters. Energy Build. 2021, 240, 110909. [Google Scholar] [CrossRef]
- Wu, G.; Liu, H.; Wu, S.; Liu, Z.; Mi, L.; Gao, L. A study on the capacity of a ventilation cooling vest with pressurized air in hot and humid environments. Int. J. Ind. Ergonom. 2021, 83, 103106. [Google Scholar] [CrossRef]
- Network, C.M.D. National meteorological information center. Available online: http://data.cma.cn/data/cdcdetail/dataCode/A.0012.0001.html (accessed on 1 October 2022).
- Zhang, H.; Xie, X.; Hong, S.; Lv, H. Impact of metabolism and the clothing thermal resistance on inpatient thermal comfort. Energy Built Environ. 2021, 2, 223–232. [Google Scholar] [CrossRef]
- D’Ambrosio Alfano, F.R.; Malchaire, J.; Palella, B.I.; Riccio, G. WBGT index revisited after 60 years of use. Ann. Occup. Hyg. 2014, 58, 955–970. [Google Scholar]
- Foster, J.; Hodder, S.G.; Goodwin, J.; Havenith, G. Occupational heat stress and practical cooling solutions for healthcare and industry workers during the COVID-19 pandemic. Ann. Work Expo Health 2020, 64, 915–922. [Google Scholar] [CrossRef]
- Johnson, J.M.; Minson, C.T.; Kellogg, D.L., Jr. Cutaneous vasodilator and vasoconstrictor mechanisms in temperature regulation. Compr. Physiol. 2014, 4, 33–89. [Google Scholar] [PubMed]
- Agarwal, A.; Agarwal, S.; Motiani, P. Difficulties encountered while using PPE kits and how to overcome them: An Indian perspective. Cureus 2020, 12, e11652. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Tao, M.; Liu, W. High temperature impairs cognitive performance during a moderate intensity activity. Build. Environ. 2020, 186, 107372. [Google Scholar] [CrossRef]
- Zhang, S.; Zhu, N.; Lu, S. Responses of human perception and skin temperature to directed thermal radiation in hot environments. Build. Environ. 2021, 197, 107857. [Google Scholar] [CrossRef]
- Grabowski, A.; Farley, C.T.; Kram, R. Independent metabolic costs of supporting body weight and accelerating body mass during walking. J. Appl. Physiol. 2005, 98, 579–583. [Google Scholar] [CrossRef]
- Cadarette, B.S.; Levine, L.; Kolka, M.A.; Proulx, G.N.; Correa, M.M.; Sawka, M.N. Heat strain reduction by ice-based and vapor compression liquid cooling systems with a toxic agent protective uniform. Aviat. Space Environ. Med. 2002, 73, 665–672. [Google Scholar]
- Ong, J.J.Y.; Chan, A.C.Y.; Bharatendu, C.; Teoh, H.L.; Chan, Y.C.; Sharma, V.K. Headache related to PPE use during the COVID-19 pandemic. Curr. Pain Headache Rep. 2021, 25, 53. [Google Scholar] [CrossRef]
- Bharatendu, C.; Ong, J.J.Y.; Goh, Y.; Tan, B.Y.Q.; Chan, A.C.Y.; Tang, J.Z.Y.; Leow, A.S.; Chin, A.; Sooi, K.W.X.; Tan, Y.L.; et al. Powered Air Purifying Respirator (PAPR) restores the N95 face mask induced cerebral hemodynamic alterations among Healthcare Workers during COVID-19 Outbreak. J. Neurol. Sci. 2020, 417, 117078. [Google Scholar] [CrossRef]
- Lu, Y.; Wei, F.; Lai, D.; Shi, W.; Wang, F.; Gao, C.; Song, G. A novel personal cooling system (PCS) incorporated with phase change materials (PCMs) and ventilation fans: An investigation on its cooling efficiency. J. Therm. Biol. 2015, 52, 137–146. [Google Scholar] [CrossRef]
- Lou, L.; Chen, K.; Fan, J. Advanced materials for personal thermal and moisture management of health care workers wearing PPE. Mater. Sci. Eng. R Rep. 2021, 146, 100639. [Google Scholar] [CrossRef]
- Pasquier, M.; Paal, P.; Kosinski, S.; Brown, D.; Podsiadlo, P.; Darocha, T. Esophageal temperature measurement. N. Engl. J. Med. 2020, 383, e93. [Google Scholar] [CrossRef] [PubMed]
- Bijur, P.E.; Shah, P.D.; Esses, D. Temperature measurement in the adult emergency department: Oral, tympanic membrane and temporal artery temperatures versus rectal temperature. Emerg. Med. J. 2016, 33, 843–847. [Google Scholar] [CrossRef] [PubMed]




| Parameters | Type | Range | Accuracy | Resolution |
|---|---|---|---|---|
| Air temperature | JI-IAQ-50 | −20~120 °C | ±0.3 °C | 0.02 °C |
| Air humidity | 0~100% | ±2.5% | 0.01% | |
| Globe temperature | 5~60 °C | ±0.5 °C | 0.1 °C | |
| Air velocity | 0.05~2 m/s | ±0.03 m/s | 0.01 m/s | |
| Core temperature | YCT-2 | 32.0~42.9 °C | ±0.1 °C | 0.1 °C |
| Skin temperature | iButton | −20~85 °C | ±0.5 °C | 0.0625 °C |
| Skin humidity | 0~100% | ±5% | 0.04% | |
| Heart rate | POLAR | 30~240 bpm | ±1 bpm | 1 bpm |
| Gender | Age | Height (cm) | Weight (kg) | Body Mass Index | Body Surface Area (m2) |
|---|---|---|---|---|---|
| Males | 22.0 ± 0.6 | 177.2 ± 4.3 | 68.6 ± 4.6 | 21.8 ± 1.6 | 1.93 ± 0.17 |
| Females | 21.9 ± 0.7 | 163.5 ± 5.5 | 56.2 ± 12.3 | 21.0 ± 3.3 | 1.69 ± 0.07 |
| Overall | 21.9 ± 0.6 | 170.0 ± 8.5 | 61.7 ± 10.1 | 21.3 ± 2.4 | 1.80 ± 0.17 |
| Thermal Sensation Vote | Thermal Comfort Vote | Borg’s Rating of Perceived Exertion | Humid Sensation Vote | Thermal Expectation |
|---|---|---|---|---|
| +3 very hot +2 hot +1 warm 0 neutral −1 cool −2 cold −3 very cold | 0 comfortable 1 slightly uncomfortable 2 uncomfortable 3 very uncomfortable 4 intolerable | 6 effortless 7~8 extremely easy 9~10 very easy 11~12 easy 13~14 slightly tired 15~16 tired 17~18 very tired 19 extremely tired 20 exhausted | +3 very humid +2 humid +1 slightly humid 0 neutral −1 slightly dry −2 dry −3 very dry | +1 get warm 0 neutral −1 get cool |
| Type | Clothing Composition | Clothing Display | |
|---|---|---|---|
| Basic trial | Dress 1 Icl1 = 0.75 clo | PPE + Trousers + Long sleeve top + Short sports socks + Sneakers |  |
| Dress 2 Icl2 = 0.37 clo | PPE + Short trousers + T-shirt + Short sports socks + Sneakers |  | |
| Cooling trial | ICS | PPE + Dress2 + Ice bag cooling vest |  |
| VCS | PPE+ Dress2 + Ventilation cooling system |  |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, Y.; Su, M.; Meng, X.; Liu, J.; Wang, F. Thermophysiological and Perceptual Responses of Amateur Healthcare Workers: Impacts of Ambient Condition, Inner-Garment Insulation and Personal Cooling Strategy. Int. J. Environ. Res. Public Health 2023, 20, 612. https://doi.org/10.3390/ijerph20010612
Zhao Y, Su M, Meng X, Liu J, Wang F. Thermophysiological and Perceptual Responses of Amateur Healthcare Workers: Impacts of Ambient Condition, Inner-Garment Insulation and Personal Cooling Strategy. International Journal of Environmental Research and Public Health. 2023; 20(1):612. https://doi.org/10.3390/ijerph20010612
Chicago/Turabian StyleZhao, Yingying, Meng Su, Xin Meng, Jiying Liu, and Faming Wang. 2023. "Thermophysiological and Perceptual Responses of Amateur Healthcare Workers: Impacts of Ambient Condition, Inner-Garment Insulation and Personal Cooling Strategy" International Journal of Environmental Research and Public Health 20, no. 1: 612. https://doi.org/10.3390/ijerph20010612
APA StyleZhao, Y., Su, M., Meng, X., Liu, J., & Wang, F. (2023). Thermophysiological and Perceptual Responses of Amateur Healthcare Workers: Impacts of Ambient Condition, Inner-Garment Insulation and Personal Cooling Strategy. International Journal of Environmental Research and Public Health, 20(1), 612. https://doi.org/10.3390/ijerph20010612








