The Role of Trust in COVID-19 Vaccine Acceptance: Considerations from a Systematic Review
Abstract
1. Introduction
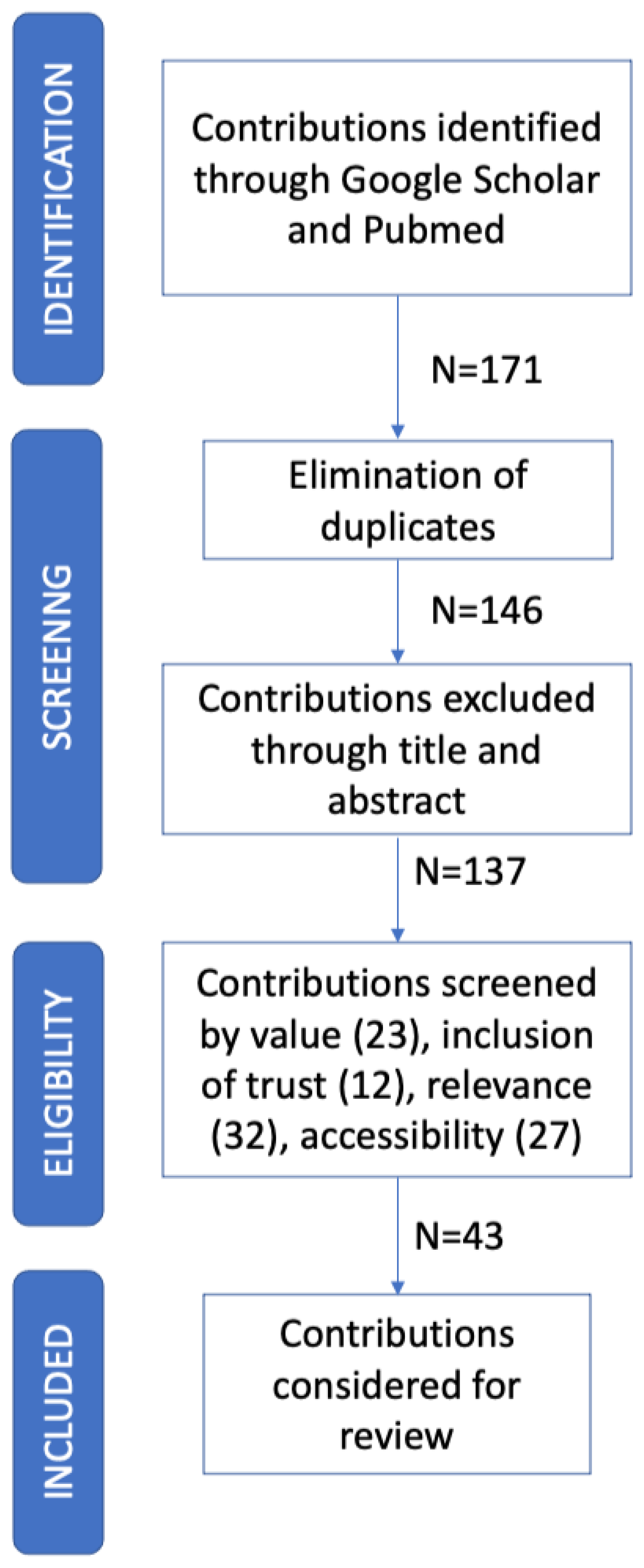
2. Methods
2.1. Design
2.2. Search Strategy
- Value, the article must address the problem of subjects’ COVID-19 vaccine acceptance/hesitancy, together with its determinants;
- Inclusion of trust, the work should at least consider one type/dimension of trust as a determinant of COVID-19 vaccine acceptance;
- Relevance, the contribution must be written in English and published in a relevant journal. We considered 2.5 as a cut-off value for the impact factor;
- Accessibility, the full article should be accessible via one of the previously mentioned portals.
3. Results
3.1. Data Extraction
- Concerns about commercial profiteering: the negative relationship, identified by Gerretsen [35], is easy to understand, since believing that the production and distribution of vaccines are motivated and conditioned by profit reasons leads reasonably to believe that other interests may prevail, not necessarily linked to the protection of health.
- Trust in religion: Rozek [57], in their seventeen-country study, reported that trusting religious leaders increases vaccine hesitancy. In support of this, Jafar [39] noted that Muslim respondents were found to be less confident towards vaccines compared to non-Muslim respondents. However, Mueangpoon [50] found that religion has a non-significant (n.s.) effect on vaccine hesitancy, while Riad [56] reported that the vast majority of participants (87.4%) stated that their religious values did not impact their vaccination decision.
- Trust in government: while trust in the government is always detected as positive, Trent [65] identified an opposite situation in the USA. We will elaborate on this point further, in the specific subsection related to trust in the government (see Section 3.3).
3.2. Trust in the COVID-19 Vaccine
3.3. Trust in Government
- Wang [67] considered trust in the government for communicating information about the COVID-19 vaccine;
- Mueangpoon [50] estimated trust in the government about encouraging COVID-19 vaccination;
- Szilagyi [64] considered the purpose of ensuring that the COVID-19 vaccine is safe for the public;
- Trent [65] introduced a scale that considers generic trust, pandemic management, and trust as a source of information about the pandemic;
- Goodwin [36] used a scale that considers generic trust, pandemic management, and vaccination management.
3.4. Trust in Manufacturers
3.5. Trust in Healthcare System and Science
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CDC | Centers for Disease Control and Prevention |
| n.s. | not significant |
| SAGE | Strategic Advisory Group of Experts on Immunization |
| WHO | World Health Organization |
References
- Falcone, R.; Colì, E.; Felletti, S.; Sapienza, A.; Castelfranchi, C.; Paglieri, F. All we need is trust: How the COVID-19 outbreak reconfigured trust in Italian public institutions. Front. Psychol. 2020, 11, 561747. [Google Scholar] [CrossRef] [PubMed]
- Lenton, T.M.; Boulton, C.A.; Scheffer, M. Resilience of countries to COVID-19 correlated with trust. Sci. Rep. 2022, 12, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Falcone, R.; Sapienza, A. An agent-based model to assess citizens’ acceptance of COVID-19 restrictions. J. Simul. 2021, 1–15. [Google Scholar] [CrossRef]
- Shanka, M.S.; Menebo, M.M. When and how trust in government leads to compliance with COVID-19 precautionary measures. J. Bus. Res. 2022, 139, 1275–1283. [Google Scholar] [CrossRef] [PubMed]
- Bollyky, T.J.; Angelino, O.; Wigley, S.; Dieleman, J.L. Trust made the difference for democracies in COVID-19. Lancet 2022, 400, 657. [Google Scholar] [CrossRef]
- Antinyan, A.; Bassetti, T.; Corazzini, L.; Pavesi, F. Trust in the health system and COVID-19 treatment. Front. Psychol. 2021, 12, 2733. [Google Scholar] [CrossRef]
- Alijanzadeh, M.; Ahorsu, D.K.; Alimoradi, Z.; Mahmoudi, N.; Griffiths, M.D.; Lin, C.Y.; Liu, H.-K.; Pakpour, A.H. Fear of COVID-19 and trust in the healthcare system mediates the association between individual’s risk perception and preventive COVID-19 behaviours among iranians. Int. J. Environ. Res. Public Health 2021, 18, 12146. [Google Scholar] [CrossRef]
- Vergara, R.J.D.; Sarmiento, P.J.D.; Lagman, J.D.N. Building public trust: A response to COVID-19 vaccine hesitancy predicament. J. Public Health 2021, 43, e291–e292. [Google Scholar] [CrossRef]
- Cordero, D.A., Jr. Rebuilding public trust: A clarified response to COVID-19 vaccine hesitancy predicament. J. Public Health 2021, 43, e303–e304. [Google Scholar] [CrossRef]
- Gakuba, C.; Sar, A.; Gaborieau, I.; Hanouz, J.L.; Verger, P. Willingness to get a COVID-19 vaccine among critical care non-medical healthcare workers and impact of a vaccine information session. Anaesth. Crit. Care Pain Med. 2021, 40, 100860. [Google Scholar] [CrossRef]
- Opel, D.J.; Salmon, D.A.; Marcuse, E.K. Building trust to achieve confidence in COVID-19 vaccines. JAMA Netw. Open 2020, 3, e2025672. [Google Scholar] [CrossRef] [PubMed]
- Marzo, R.R.; Sami, W.; Alam, M.; Acharya, S.; Jermsittiparsert, K.; Songwathana, K.; Pham, N.T.; Respati, T.; Faller, E.M.; Yi, S.; et al. Hesitancy in COVID-19 vaccine uptake and its associated factors among the general adult population: A cross-sectional study in six Southeast Asian countries. Trop. Med. Health 2022, 50, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Sabahelzain, M.M.; Hartigan-Go, K.; Larson, H.J. The politics of COVID-19 vaccine confidence. Curr. Opin. Immunol. 2021, 71, 92–96. [Google Scholar] [CrossRef]
- Verger, P.; Dubé, E. Restoring confidence in vaccines in the COVID-19 era. Expert Rev. Vaccines 2020, 19, 991–993. [Google Scholar] [CrossRef] [PubMed]
- Lipscy, P.Y. COVID-19 and the Politics of Crisis. Int. Organ. 2020, 74, E98–E127. [Google Scholar] [CrossRef]
- Baker, D.W. Trust in health care in the time of COVID-19. JAMA 2020, 324, 2373–2375. [Google Scholar] [CrossRef]
- Ronzani, P.; Panizza, F.; Martini, C.; Savadori, L.; Motterlini, M. Countering vaccine hesitancy through medical expert endorsement. Vaccine 2022, 40, 4635–4643. [Google Scholar] [CrossRef]
- Falcone, R.; Sapienza, A. How COVID-19 changed the information needs of Italian citizens. Int. J. Environ. Res. Public Health 2020, 17, 6988. [Google Scholar] [CrossRef]
- Apuke, O.D.; Omar, B. Fake news and COVID-19: Modelling the predictors of fake news sharing among social media users. Telemat. Inform. 2021, 56, 101475. [Google Scholar] [CrossRef]
- Orso, D.; Federici, N.; Copetti, R.; Vetrugno, L.; Bove, T. Infodemic and the spread of fake news in the COVID-19-era. Eur. J. Emerg. Med. 2020, 27, 327–328. [Google Scholar] [CrossRef]
- Aw, J.; Seng, J.J.B.; Seah, S.S.Y.; Low, L.L. COVID-19 vaccine hesitancy—A scoping review of literature in high-income countries. Vaccines 2021, 9, 900. [Google Scholar] [CrossRef]
- Biswas, N.; Mustapha, T.; Khubchandani, J.; Price, J.H. The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. J. Community Health 2021, 46, 1244–1251. [Google Scholar] [CrossRef]
- Chevallier, C.; Hacquin, A.S.; Mercier, H. COVID-19 vaccine hesitancy: Shortening the last mile. Trends Cogn. Sci. 2021, 25, 331–333. [Google Scholar] [CrossRef] [PubMed]
- Finney Rutten, L.J.; Zhu, X.; Leppin, A.L.; Ridgeway, J.L.; Swift, M.D.; Griffin, J.M.; Sauverm, J.L.; Virk, A.; Jacobson, R.M. Evidence-based strategies for clinical organizations to address COVID-19 vaccine hesitancy. Mayo Clin. Proc. 2021, 96, 699–707. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. COVID-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- Troiano, G.; Nardi, A. Vaccine hesitancy in the era of COVID-19. Public Health 2021, 194, 245–251. [Google Scholar] [CrossRef]
- Abdou, M.S.; Kheirallah, K.A.; Aly, M.O.; Ramadan, A.; Elhadi, Y.A.M.; Elbarazi, I.; Deghidy, E.A.; Saeh, H.M.E.; Salem, K.M.; Ghazy, R.M. The coronavirus disease 2019 (COVID-19) vaccination psychological antecedent assessment using the Arabic 5c validated tool: An online survey in 13 Arab countries. PLoS ONE 2021, 16, e0260321. [Google Scholar] [CrossRef] [PubMed]
- Allington, D.; McAndrew, S.; Moxham-Hall, V.; Duffy, B. Coronavirus conspiracy suspicions, general vaccine attitudes, trust and coronavirus information source as predictors of vaccine hesitancy among UK residents during the COVID-19 pandemic. Psychol. Med. 2021, 1–12. [Google Scholar] [CrossRef]
- Babicki, M.; Mastalerz-Migas, A. Attitudes toward vaccination against COVID-19 in Poland. A longitudinal study performed before and two months after the commencement of the population vaccination programme in Poland. Vaccines 2021, 9, 503. [Google Scholar] [CrossRef]
- Brindle, H.; Rogers, N.T.; Eggo, R.M.; Enria, L.; Lees, S. Vaccine Confidence and Hesitancy at the start of COVID-19 vaccine deployment in the UK: An embedded mixed-methods study. Front. Public Health 2021, 9, 745630. [Google Scholar]
- Daly, M.; Jones, A.; Robinson, E. Public trust and willingness to vaccinate against COVID-19 in the US from 14 October 2020 to 29 March 2021. JAMA 2021, 325, 2397–2399. [Google Scholar] [CrossRef]
- Dorman, C.; Perera, A.; Condon, C.; Chau, C.; Qian, J.; Kalk, K.; DiazDeleon, D. Factors associated with willingness to be vaccinated against COVID-19 in a large convenience sample. J. Community Health 2021, 46, 1013–1019. [Google Scholar] [CrossRef] [PubMed]
- Falcone, R.; Ansani, A.; Colì, E.; Marini, M.; Sapienza, A.; Castelfranchi, C.; Paglieri, F. Trusting COVID-19 vaccines as individual and social goal. Sci. Rep. 2022, 12, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Penny, F.E.; Jolkovsky, E.L.; Shofer, F.S.; Hemmert, K.C.; Valiuddin, H.; Uspal, J.E.; Sands, N.A.; Abella, B.S. COVID-19 vaccine hesitancy among patients in two urban emergency departments. Acad. Emerg. Med. 2021, 28, 1100–1107. [Google Scholar] [CrossRef]
- Gerretsen, P.; Kim, J.; Caravaggio, F.; Quilty, L.; Sanches, M.; Wells, S.; Brown, E.E.; Agic, B.; Polloc, B.G.; Graff-Guerrero, A. Individual determinants of COVID-19 vaccine hesitancy. PLoS ONE 2021, 16, e0258462. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, R.; Ben-Ezra, M.; Takahashi, M.; Luu, L.A.N.; Borsfay, K.; Kovács, M.; Hou, W.K.; Hamama-Raz, Y.; Levin, Y. Psychological factors underpinning vaccine willingness in Israel, Japan and Hungary. Sci. Rep. 2022, 12, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Han, K.; Francis, M.R.; Zhang, R.; Wang, Q.; Xia, A.; Lu, L.; Yang, B.; Hou, Z. Confidence, acceptance and willingness to pay for the COVID-19 vaccine among migrants in Shanghai, China: A cross-sectional study. Vaccines 2021, 9, 443. [Google Scholar] [CrossRef]
- Hou, Z.; Tong, Y.; Du, F.; Lu, L.; Zhao, S.; Yu, K.; Piatek, S.J.; Larson, H.J.; Lin, L. Assessing COVID-19 vaccine hesitancy, confidence, and public engagement: A global social listening study. J. Med. Internet Res. 2021, 23, e27632. [Google Scholar] [CrossRef]
- Jafar, A.; Dambul, R.; Dollah, R.; Sakke, N.; Mapa, M.T.; Joko, E.P. COVID-19 vaccine hesitancy in Malaysia: Exploring factors and identifying highly vulnerable groups. PLoS ONE 2022, 17, e0270868. [Google Scholar] [CrossRef]
- Jennings, W.; Stoker, G.; Bunting, H.; Valgarðsson, V.O.; Gaskell, J.; Devine, D.; McKay, L.; Mills, M.C. Lack of trust, conspiracy beliefs, and social media use predict COVID-19 vaccine hesitancy. Vaccines 2021, 9, 593. [Google Scholar] [CrossRef]
- Kerekes, S.; Ji, M.; Shih, S.F.; Chang, H.Y.; Harapan, H.; Rajamoorthy, Y.; Singh, A.; Kanwar, S.; Wagner, A.L. Differential effect of vaccine effectiveness and safety on COVID-19 vaccine acceptance across socioeconomic groups in an international sample. Vaccines 2021, 9, 1010. [Google Scholar] [CrossRef] [PubMed]
- King, W.C.; Rubinstein, M.; Reinhart, A.; Mejia, R. COVID-19 vaccine hesitancy January-May 2021 among 18–64 year old US adults by employment and occupation. Prev. Med. Rep. 2021, 24, 101569. [Google Scholar] [CrossRef] [PubMed]
- Kreps, S.; Prasad, S.; Brownstein, J.S.; Hswen, Y.; Garibaldi, B.T.; Zhang, B.; Kriner, D.L. Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA Netw. Open 2020, 3, e2025594. [Google Scholar] [CrossRef] [PubMed]
- Kwok, K.O.; Li, K.K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef] [PubMed]
- Latkin, C.A.; Dayton, L.; Yi, G.; Konstantopoulos, A.; Boodram, B. Trust in a COVID-19 vaccine in the US: A social-ecological perspective. Soc. Sci. Med. 2021, 270, 113684. [Google Scholar] [CrossRef]
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl. Trop. Dis. 2020, 14, e0008961. [Google Scholar] [CrossRef]
- Liu, R.; Li, G.M. Hesitancy in the time of coronavirus: Temporal, spatial, and sociodemographic variations in COVID-19 vaccine hesitancy. SSM-Popul. Health 2021, 15, 100896. [Google Scholar] [CrossRef]
- Machida, M.; Nakamura, I.; Kojima, T.; Saito, R.; Nakaya, T.; Hanibuchi, T.; Takamiya, T.; Odagiri, a.Y.; Fukushima, A.N.; Inoue, S.; et al. Trends in COVID-19 vaccination intent from pre-to post-COVID-19 vaccine distribution and their associations with the 5C psychological antecedents of vaccination by sex and age in Japan. Hum. Vaccines Immunother. 2021, 17, 3954–3962. [Google Scholar] [CrossRef]
- Mellis, A.M.; Kelly, B.C.; Potenza, M.N.; Hulsey, J.N. Trust in a COVID-19 vaccine among people with substance use disorders. Drug Alcohol Depend. 2021, 220, 108519. [Google Scholar] [CrossRef]
- Mueangpoon, K.; Inchan, C.; Kaewmuneechoke, P.; Rattana, P.; Budsratid, S.; Japakiya, S.; Ngamchaliew, P.; Vichitkunakorn, P. Self-Reported COVID-19 Vaccine Hesitancy and Willingness to Pay: A Cross-Sectional Survey in Thailand. Vaccines 2022, 10, 627. [Google Scholar] [CrossRef]
- Orangi, S.; Pinchoff, J.; Mwanga, D.; Abuya, T.; Hamaluba, M.; Warimwe, G.; Austrian, K.; Barasa, E. Assessing the level and determinants of COVID-19 vaccine confidence in Kenya. Vaccines 2021, 9, 936. [Google Scholar] [CrossRef] [PubMed]
- Park, H.K.; Ham, J.H.; Jang, D.H.; Lee, J.Y.; Jang, W.M. Political ideologies, government trust, and COVID-19 vaccine hesitancy in South Korea: A cross-sectional survey. Int. J. Environ. Res. Public Health 2021, 18, 10655. [Google Scholar] [CrossRef] [PubMed]
- Parsons Leigh, J.; Halperin, D.; Mizen, S.J.; FitzGerald, E.A.; Moss, S.J.; Fiest, K.M.; Castri, A.D.; Stelfox, H.T.; Halperin, S. Exploring the impact of media and information on self-reported intentions to vaccinate against COVID-19: A qualitative interview-based study. Hum. Vaccines Immunother. 2022, 18, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Pogue, K.; Jensen, J.L.; Stancil, C.K.; Ferguson, D.G.; Hughes, S.J.; Mello, E.J.; Burgess, R.; Berges, B.K.; Quaye, A.; Poole, B.D. Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines 2020, 8, 582. [Google Scholar] [CrossRef]
- Reiter, P.L.; Pennell, M.L.; Katz, M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated. Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef]
- Riad, A.; Pokorná, A.; Antalová, N.; Krobot, M.; Zviadadze, N.; Serdiuk, I.; Koščík, M.; Klugar, M. Prevalence and drivers of COVID-19 vaccine hesitancy among Czech university students: National cross-sectional study. Vaccines 2021, 9, 948. [Google Scholar] [CrossRef]
- Rozek, L.S.; Jones, P.; Menon, A.; Hicken, A.; Apsley, S.; King, E.J. Understanding vaccine hesitancy in the context of COVID-19: The role of trust and confidence in a seventeen-country survey. Int. J. Public Health 2021, 66, 636255. [Google Scholar] [CrossRef]
- Rzymski, P.; Zeyland, J.; Poniedziałek, B.; Małecka, I.; Wysocki, J. The perception and attitudes toward COVID-19 vaccines: A cross-sectional study in Poland. Vaccines 2021, 9, 382. [Google Scholar] [CrossRef]
- Simione, L.; Vagni, M.; Gnagnarella, C.; Bersani, G.; Pajardi, D. Mistrust and beliefs in conspiracy theories differently mediate the effects of psychological factors on propensity for COVID-19 vaccine. Front. Psychol. 2021, 12, 683684. [Google Scholar] [CrossRef]
- Schernhammer, E.; Weitzer, J.; Laubichler, M.D.; Birmann, B.M.; Bertau, M.; Zenk, L.; Caniglia, G.; Jäger, C.C.; Steiner, G. Correlates of COVID-19 vaccine hesitancy in Austria: Trust and the government. J. Public Health 2022, 44, e106–e116. [Google Scholar] [CrossRef]
- Soares, P.; Rocha, J.V.; Moniz, M.; Gama, A.; Laires, P.A.; Pedro, A.R.; Dias, S.; Leite, A.; Nunes, C. Factors associated with COVID-19 vaccine hesitancy. Vaccines 2021, 9, 300. [Google Scholar] [CrossRef] [PubMed]
- Stoler, J.; Enders, A.M.; Klofstad, C.A.; Uscinski, J.E. The limits of medical trust in mitigating COVID-19 vaccine hesitancy among black Americans. J. Gen. Intern. Med. 2021, 36, 3629–3631. [Google Scholar] [CrossRef] [PubMed]
- Strupat, C.; Shigute, Z.; Bedi, A.S.; Rieger, M. Willingness to take COVID-19 vaccination in low-income countries: Evidence from Ethiopia. PLoS ONE 2020, 17, e0264633. [Google Scholar] [CrossRef] [PubMed]
- Szilagyi, P.G.; Thomas, K.; Shah, M.D.; Vizueta, N.; Cui, Y.; Vangala, S.; Fox, C.; Kapteyn, A. The role of trust in the likelihood of receiving a COVID-19 vaccine: Results from a national survey. Prev. Med. 2021, 153, 106727. [Google Scholar] [CrossRef]
- Trent, M.; Seale, H.; Chughtai, A.A.; Salmon, D.; MacIntyre, C.R. Trust in government, intention to vaccinate and COVID-19 vaccine hesitancy: A comparative survey of five large cities in the United States, United Kingdom, and Australia. Vaccine 2022, 40, 2498–2505. [Google Scholar] [CrossRef]
- Viswanath, K.; Bekalu, M.; Dhawan, D.; Pinnamaneni, R.; Lang, J.; McLoud, R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health 2020, 21, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Han, B.; Zhao, T.; Liu, H.; Liu, B.; Chen, L.; Du, J.; Liu, Y.; Lu, Q.; Cui, F. Vaccination willingness, vaccine hesitancy, and estimated coverage at the first round of COVID-19 vaccination in China: A national cross-sectional study. Vaccine 2021, 39, 2833–2842. [Google Scholar] [CrossRef]
- Williams, N.L.; Nguyen, T.H.H.; Del Chiappa, G.; Fedeli, G.; Wassler, P. COVID-19 vaccine confidence and tourism at the early stage of a voluntary mass vaccination campaign: A PMT segmentation analysis. Curr. Issues Tour. 2022, 25, 475–489. [Google Scholar] [CrossRef]
- Willis, D.E.; Andersen, J.A.; Bryant-Moore, K.; Selig, J.P.; Long, C.R.; Felix, H.C.; Curran, G.M.; McElfish, P.A. COVID-19 vaccine hesitancy: Race/ethnicity, trust, and fear. Clin. Transl. Sci. 2021, 14, 2200–2207. [Google Scholar] [CrossRef]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Castelfranchi, C.; Falcone, R. Trust Theory: A Socio-Cognitive and Computational Model; John Wiley & Sons.: Hoboken, NJ, USA, 2010. [Google Scholar]
- Vaccination and Trust. Available online: https://www.who.int/publications/i/item/vaccination-and-trust (accessed on 25 October 2022).
- WHO Released a New Operational Guide to Promote COVID-19 Vaccination Uptake and Tackle Vaccine Hesitancy among Refugees and Migrants. Available online: https://www.who.int/news/item/14-03-2022-who-released-a-new-operational-guide-to-promote-covid-19-vaccination-uptake-and-tackle-vaccine-hesitancy-among-refugees-and-migrants (accessed on 25 October 2022).
- Larson, H.J.; De Figueiredo, A.; Xiahong, Z.; Schulz, W.S.; Verger, P.; Johnston, I.G.; Cook, A.R.; Jones, N.S. The state of vaccine confidence 2016: Global insights through a 67-country survey. EBioMedicine 2016, 12, 295–301. [Google Scholar] [CrossRef] [PubMed]
- 7 Punkte für eine Wirksame Corona-Impfstrategie. Available online: https://www.spoe.at/2020/11/23/7-punkte-fuer-eine-wirksame-corona-impfstrategie/?fbclid=IwAR3_8cn--GerU-n_PH4INTD5GuwI2DK92ETLQidIJl9BcmZHLzq_hyxM4GA (accessed on 10 December 2022).
- Beate Meinl-Reisinger’s COVID Critique, Review and Restart for Austria. Available online: https://www.iglobenews.org/beate-meinl-reisingers-covid-critique-review-and-restart-for-austria/ (accessed on 10 December 2022).
- Falkenbach, M.; Heiss, R. The Populist Radical Right and Health; Springer: Cham, Switzerland, 2021; pp. 25–45. [Google Scholar]
- Sensationserfolg für Impfgegner-Partei. Available online: https://www.wienerzeitung.at/nachrichten/politik/oesterreich/2122129-Sensationserfolg-fuer-Impfgegner-Partei.html (accessed on 10 December 2022).
- Van Aelst, P.; Blumler, J.G. Political Communication in the Time of Coronavirus; Routledge: London, UK, 2021. [Google Scholar]
- Calls for Inquiry as UK Reports Highest Covid-19 Death Toll in Europe. Available online: https://www.theguardian.com/world/2020/may/05/uk-coronavirus-death-toll-rises-above-32000-to-highest-in-europe (accessed on 25 October 2022).
- Pressure on Dominic Cummings to Quit Over Lockdown Breach. Available online: https://www.theguardian.com/politics/2020/may/22/dominic-cummings-durham-trip-coronavirus-lockdown (accessed on 25 October 2022).
- Timeline of Trump’s COVID-19 Comments. Available online: https://www.factcheck.org/2020/10/timeline-of-trumps-covid-19-comments/ (accessed on 25 October 2022).
- Breaking with Trump, Fauci says U.S. Will Do ‘More Testing, Not Less’. Available online: https://www.nbcnews.com/politics/congress/fauci-says-u-s-will-expand-testing-not-slow-it-n1231877 (accessed on 25 October 2022).
- Coronavirus: Hydroxychloroquine Ineffective Says Fauci. Available online: https://www.bbc.com/news/world-us-canada-53575964 (accessed on 25 October 2022).
- Trump Administration Outlines Audacious Plan to Deliver ‘Hundreds of Millions’ of Covid-19 Vaccine Doses by End of 2020. Available online: https://www.statnews.com/2020/05/15/trump-audacious-plan-vaccine-covid19/ (accessed on 25 October 2022).
- Trump Contradicts Health Officials, Says ‘Probably’ a Covid-19 Vaccine in October. Available online: https://www.politico.com/news/2020/09/04/trump-coronavirus-vaccine-october-409248 (accessed on 25 October 2022).
- McCarthy, J. Big Pharma Sinks to the Bottom of US Industry Rankings; Gallup Inc.: Washington, DC, USA, 2019. [Google Scholar]
- Funk, C.; Kennedy, B.; Johnson, C. Trust in Medical Scientists Has Grown in US, But Mainly among Democrats; Pew Research Center: Washington, DC, USA, 2020. [Google Scholar]
- Marini, M.; Ansani, A.; Paglieri, F.; Caruana, F.; Viola, M. The impact of facemasks on emotion recognition, trust attribution and re-identification. Sci. Rep. 2021, 11, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J.A. Vaccine hesitancy: An overview. Hum. Vaccines Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, R.M.; Sauver, J.L.S.; Rutten, L.J.F. Vaccine hesitancy. Mayo Clin. Proc. 2015, 90, 1562–1568. [Google Scholar] [CrossRef]
- Binagwaho, A.; Mathewos, K.; Davis, S. Time for the ethical management of COVID-19 vaccines. Lancet Glob. Health 2021, 9, e1169–e1171. [Google Scholar] [CrossRef] [PubMed]
- Huang, P.H. COVID-19 vaccination and the right to take risks. J. Med. Ethics 2020, 48, 534–537. [Google Scholar] [CrossRef]
- King, J.; Ferraz, O.L.M.; Jones, A. Mandatory COVID-19 vaccination and human rights. Lancet 2022, 399, 220–222. [Google Scholar] [CrossRef]
- Pagnini, F.; Bonanomi, A.; Tagliabue, S.; Balconi, M.; Bertolotti, M.; Confalonieri, E.; Dio, C.D.; Gilli, G.; Graffigna, G.; Villani, D.; et al. Knowledge, concerns, and behaviors of individuals during the first week of the coronavirus disease 2019 pandemic in Italy. JAMA Netw. Open 2020, 3, e2015821. [Google Scholar] [CrossRef]
- Siegrist, M.; Zingg, A. The role of public trust during pandemics: Implications for crisis communication. Eur. Psychol. 2014, 19, 23. [Google Scholar] [CrossRef]
- Lewnard, J.A.; Lo, N.C. Scientific and ethical basis for social-distancing interventions against COVID-19. Lancet Infect. Dis. 2020, 20, 631–633. [Google Scholar] [CrossRef]
- French, J.; Deshpande, S.; Evans, W.; Obregon, R. Key guidelines in developing a pre-emptive COVID-19 vaccination uptake promotion strategy. Int. J. Environ. Res. Public Health 2020, 17, 5893. [Google Scholar] [CrossRef] [PubMed]
- Megget, K. Even COVID-19 can’t kill the anti-vaccination movement. BMJ 2020, 369, m2184. [Google Scholar] [CrossRef] [PubMed]
- Mylan, S.; Hardman, C. COVID-19, cults, and the anti-vax movement. Lancet 2021, 397, 1181. [Google Scholar] [CrossRef] [PubMed]
- Gambetta, D. Can we trust trust. Trust. Mak. Break. Coop. Relations 2000, 13, 213–237. [Google Scholar]
- Hardin, R. Trust and Trustworthiness; Russell Sage Foundation: New York, NY, USA, 2002. [Google Scholar]
- Luhmann, N. Trust and Power; Wiley: New York, NY, USA, 1979. [Google Scholar]
- Falcone, R.; Castelfranchi, C. Trust and transitivity: How trust-transfer works. In Highlights on Practical Applications of Agents and Multi-Agent Systems; Springer: Berlin/Heidelberg, Germany, 2012; pp. 179–187. [Google Scholar]
- Falcone, R.; Sapienza, A.; Castelfranchi, C. The relevance of categories for trusting information sources. ACM Trans. Internet Technol. (Toit) 2015, 15, 1–21. [Google Scholar] [CrossRef]
- Kuter, B.J.; Offit, P.A.; Poland, G.A. The development of COVID-19 vaccines in the United States: Why and how so fast. Vaccine 2021, 39, 2491. [Google Scholar] [CrossRef] [PubMed]
- Bolsen, T.; Palm, R. Politicization and COVID-19 vaccine resistance in the US. Prog. Mol. Biol. Transl. Sci. 2022, 188, 81. [Google Scholar]
- Hart, P.S.; Chinn, S.; Soroka, S. Politicization and polarization in COVID-19 news coverage. Sci. Commun. 2020, 42, 679–697. [Google Scholar] [CrossRef]
- Van Scoy, L.J.; Snyder, B.; Miller, E.L.; Toyobo, O.; Grewel, A.; Ha, G.; Gillespie, S.; Patel, M.; Reilly, J.; Lennon, R.P.; et al. Public anxiety and distrust due to perceived politicization and media sensationalism during early COVID-19 media messaging. J. Commun. Healthc. 2021, 14, 193–205. [Google Scholar] [CrossRef]

| Contribution | Country | Surveying Period | Sample Size |
|---|---|---|---|
| Abdou [27] | 13 Arab countries | Dec 2020–Feb 2021 | 4474 |
| Allington [28] | UK | Nov–Dec 2020 | 4343 |
| Babicki [29] | Poland | Dec 2020–Mar 2021 | 2022 |
| Brindle [30] | UK | Dec 2020 | 4535 |
| Daly [31] | USA | Oct 2020–Mar 2021 | 7420 |
| Dorman [32] | USA | Oct–Nov 2020 | 26,324 |
| Falcone [33] | Italy | Mar–Apr 2021 | 4096 |
| Fernández [34] | USA | Jan–May 2021 | 1068 |
| Gerretsen [35] | USA and Canada | May 2020, Jul 2020, and Mar 2021 | 7678 |
| Goodwin [36] | Israel, Japan, and Hungary | Jan-Apr 2021 | 2127 |
| Han [37] | China | Nov 2020 | 2126 |
| Hou [38] | USA, UK, Brazil, India, China | Jun–Jul 2020 | 12,886 |
| Jafar [39] | Malaysia | Mar–Apr 2021 | 1024 |
| Jennings [40] | UK | Dec 2020 | 1476 |
| Kerekes [41] | US, China, Taiwan, Malaysia, Indonesia, and India | Mar–Nov 2020 | 12,915 |
| King [42] | USA | Jan–May 2021 | 525,809 |
| Kreps [43] | USA | Jul 2020 | 1971 |
| Kwok [44] | Hong Kong | Mar–Apr 2020 | 1205 |
| Latkin [45] | USA | Mar 2020–Nov 2020 | 592 |
| Lin [46] | China | May 2020 | 3541 |
| Liu [47] | USA | Jan–Mar 2021 | 443,680 |
| Machida [48] | Japan | Jan–Apr 2021 | 2655 |
| Mellis [49] | USA | Sep 2020 | 87 |
| Mueangpoon [50] | Thailand | Sep 2021–Jan 2022 | 705 |
| Orangi [51] | Kenya | Feb 2021 | 4136 |
| Park [52] | South Korea | Feb 2021 | 1000 |
| Parsons [53] | Canada | Feb–May 2021 | 60 |
| Pogue [54] | USA | n.a. | 316 |
| Reiter [55] | USA | May 2020 | 2006 |
| Riad [56] | Czech Republic | Apr–Jun 2021 | 1351 |
| Rozek [57] | 17 countries | 15,151 | |
| Rzymski [58] | Poland | Feb–Mar 2021 | 1020 |
| Simione [59] | Italy | Apr 2020 | 350 |
| Schernhammer [60] | Austria | Nov–Dec 2020 | 1007 |
| Soares [61] | Portugal | Sep 2020–Jan 2021 | 1943 |
| Stoler [62] | USA | Jun 2020 | 1040 |
| Strupat [63] | Ethiopia | Nov 2020 | 2317 |
| Szilagyi [64] | USA | Dec 2020–Jan 2021 | 5979 |
| Trent [65] | USA, UK, Australia | Jul–Sep 2020 | 2712 |
| Viswanath [66] | USA | Jul 2020 | 1012 |
| Wang [67] | China | Jan 2021 | 8742 |
| Williams [68] | Italy | Jan–Feb 2021 | 3893 |
| Willis [69] | USA | Jul–Aug 2020 | 1205 |
| Positively Related | Negatively Related | Occurrences | |
|---|---|---|---|
| Trust in the COVID-19 vaccine | Abdou [27], Dorman [32], Falcone [33], Gerretsen [35], Han [37], Jafar [39], Jennings [40], King [42], Liu [47], Machida [48], Mueangpoon [50], Parsons [53], Soares [61], Trent [65], Wang [67] | 15 | |
| Vaccine’s safety | Babicki [29], Dorman [32], Gerretsen [35], Han [37], Kerekes [41], King [42], Kreps [43], Lin [46], Mellis [49], Mueangpoon [50], Orangi [51], Park [52], Parsons [53], Pogue [54], Reiter [55], Soares [61], Szilagyi [64], Trent [65], Wang [67], Williams [68] | 20 | |
| Vaccine’s efficacy | Babicki [29], Fernández [34], Gerretsen [35], Goodwin [36], Han [37], Kerekes [41], Kreps [43], Lin [46], Mueangpoon [50], Orangi [51], Pogue [54], Reiter [55], Soares [61], Szilagyi [64], Trent [65], Wang [67], Williams [68] | 17 | |
| Concerns about commercial profiteering | Gerretsen [35] | 1 | |
| General trust in vaccines | Brindle [30], Kwok [44], Parsons [53], Willis [69] | 4 | |
| Trust in government | Allington [28], Brindle [30], Gerretsen [35], Goodwin [36], Jennings [40], King [42], Mellis [49], Mueangpoon [50], Park [52], Parsons [53], Rozek [57], Schernhammer [60], Strupat [63], Szilagyi [64], Trent [65], Wang [67] | Trent [65] | 16 |
| Trust in health system | Allington [28], Jennings [40], Reiter [55], Riad [56], Rozek [57], Simione [59], Soares [61], Stoler [62], Szilagyi [64] | 9 | |
| Trust in sciences | Allington [28], Brindle [30], Fernández [34], Jennings [40], Rozek [57], Simione [59], Viswanath [66] | 7 | |
| Trust in religion | Rozek [57] | 1 | |
| Social trust | Jennings [40] | 1 | |
| Trust in COVID-19 manufacturers | Riad [56], Szilagyi [64], Wang [67], Williams [68] | 4 |
| Contribution | Vaccine Acceptance | Trust in the COVID-19 Vaccine |
|---|---|---|
| Abdou [27], multi-country, December 2020–February 2021 | 27.9% | 26.7% |
| Daly [31], USA, October 2020–March 2021 | 64.8% | 50% |
| Falcone [33], Italy, March–April 2021 | 88.8% | 92.9% |
| Han [37], Cina, November 2020 | 89.1% | 82% |
| Lin [46], China, May 2020 | 83.3% | 94.8% |
| Liu [47], USA, January–March 2021 | 84.1% | 90% |
| Machina [48], Japan, January 2021–April 2021 | 72.4% | 58.7% |
| Mueangpoon [50], Thailand, September 2021–January 2022 | 89.6% | 60.6% |
| Soares [61], Portugal, September 2020–January 2021 | 35% | 58% |
| Wang [67], China, January 2021 | 67.1% | 69% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sapienza, A.; Falcone, R. The Role of Trust in COVID-19 Vaccine Acceptance: Considerations from a Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 665. https://doi.org/10.3390/ijerph20010665
Sapienza A, Falcone R. The Role of Trust in COVID-19 Vaccine Acceptance: Considerations from a Systematic Review. International Journal of Environmental Research and Public Health. 2023; 20(1):665. https://doi.org/10.3390/ijerph20010665
Chicago/Turabian StyleSapienza, Alessandro, and Rino Falcone. 2023. "The Role of Trust in COVID-19 Vaccine Acceptance: Considerations from a Systematic Review" International Journal of Environmental Research and Public Health 20, no. 1: 665. https://doi.org/10.3390/ijerph20010665
APA StyleSapienza, A., & Falcone, R. (2023). The Role of Trust in COVID-19 Vaccine Acceptance: Considerations from a Systematic Review. International Journal of Environmental Research and Public Health, 20(1), 665. https://doi.org/10.3390/ijerph20010665






