Community Perceptions of Arsenic Contaminated Drinking Water and Preferences for Risk Communication in California’s San Joaquin Valley
Abstract
1. Introduction
2. Materials and Methods
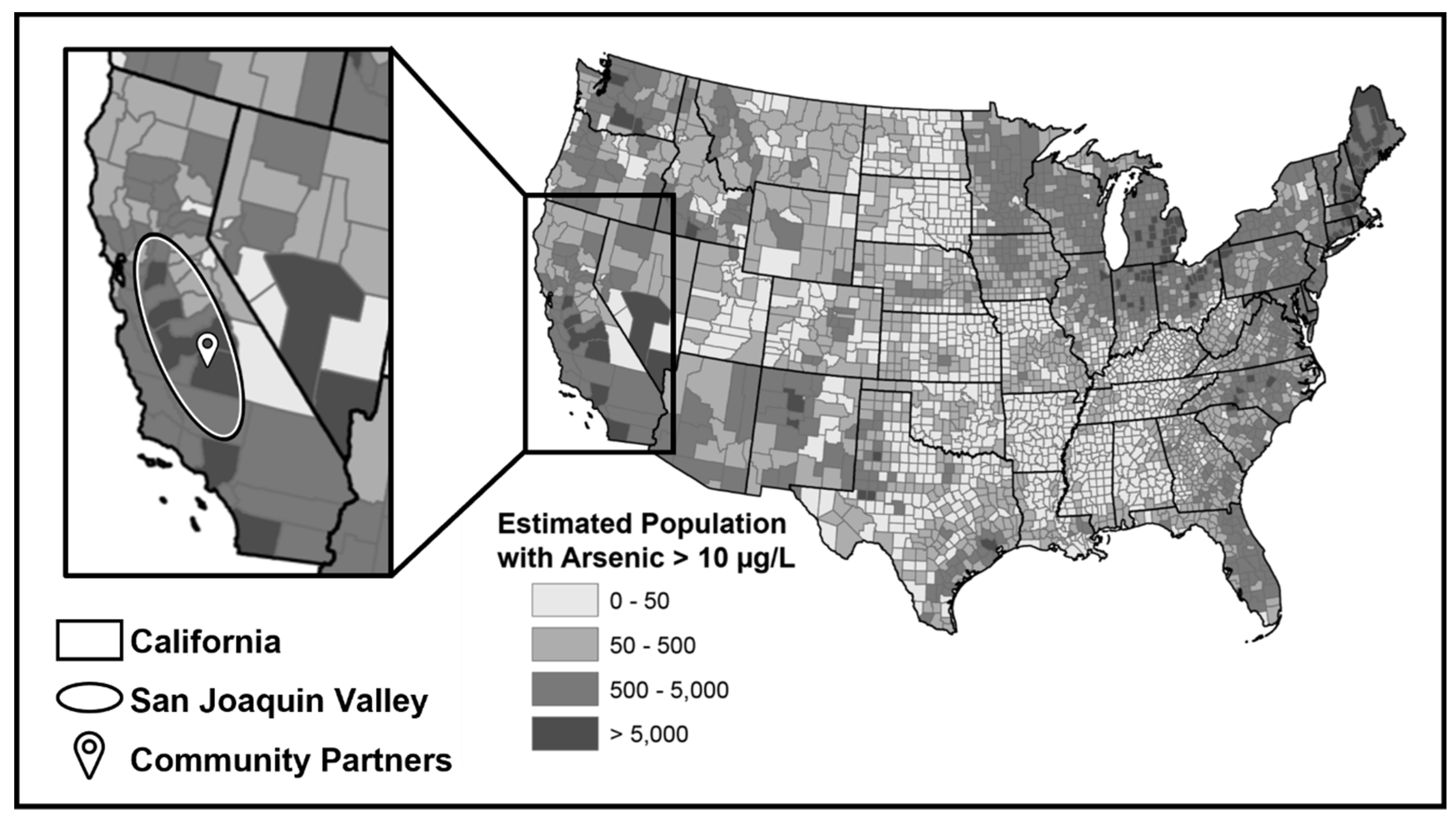
2.1. Study Area
2.2. Sampling Plan and Recruitment
2.3. Data Collection
2.4. Data Analysis
3. Results
3.1. Summary of CI Characteristics
3.2. Community Understanding of Arsenic Risk in Drinking Water
3.2.1. Community Perceptions and Experiences with Arsenic Exposure in Drinking Water Systems
“Arsenic is just prevalent in this area. It’s naturally occurring in our groundwater and so very likely to be present in public water systems, private wells, pretty much any groundwater source it’s likely to be found.” (Public Water Representative)
“I mean, here in [town name], you never know what you’re drinking, because I mean, there’s so much that we don’t know.” (Local School District Member)
“It [Arsenic-contaminated water] affects the student’s learning capacity. I imagine what it does to someone that’s 40, 50, 60, 70 years old drinking the same water. Again, it deteriorates the [student’s] body from within and that has a big effect.” (Tribal Nation Leader)
“The mere fact that we have arsenic, any trace of arsenic in the water, is pushing a lot of very low-income people to go out and buy water [even though they cannot afford it].” (Local School District Member)
3.2.2. Lack of Understanding about Health Risks from Exposure to Arsenic and Other Water Contaminants in Drinking Water among Community Residents
3.2.3. Reasons for the Lack of Understanding about the Health Risks from Arsenic Contamination in the Drinking Water
“There needs to be more awareness of the water and things in the community. They [the community] don’t get involved a lot, and then, they complain, and then, I tell them well, if you are going to complain, why don’t you go to the meeting?” (Community Resident)
3.3. Barriers and Preferences for Risk Communication and Education
3.3.1. Structural Barriers to Risk Communication and Education
“The challenge is always trying to figure out what’s the best sort of day and time to do a presentation. You have working families, you have people who work different times and days of the week and so it’s always trying to figure out when it’s going to work best for the majority of the community so that they are able to attend” (Public Water Representative).
“We’ve tried a number of times to get people to dial in [for meetings], but that’s the other part of the problem. We don’t have good internet access here. It’s improving, but it’s not free. For somebody that has limited funds, I mean subscribing to an internet service is not viable. To try to get them to join the Zoom call, especially if they’re going to pay to join on their cell phone, makes no sense to them. We’ve had that as a challenge so far.” (Community Resident)
3.3.2. Preferences for Education and Risk Communication about Drinking Water Safety
“The kids basically have a little seminar, and then [afterwards] they talk to their parents at least somewhat about it. Again, it depends on whether their parents are interested in or concerned about those kinds of issues or not and whether or not they’ll hear them out. From what I’ve noticed, it seems to be the case that the information usually at least gets to their parents.” (Rural Community Leader)
“If you’re able to set up basically an event within the [community] event that’s already there, you’d be guaranteed a pretty good amount of community exposure, which then would allow you to hopefully get a good amount of community participation.” (Rural Community Leader)
“Word of mouth could go a long way. If you get somebody, like if my Tia (aunt) or my comadre (godmother) would tell me, then I would trust her, right? Because I feel like she’s a trustworthy person. I think if you could just talk to as many people as you can and hopefully the word of mouth gets around.” (Community Resident)
4. Discussion
4.1. Community Awareness and Barriers to Knowledge Acquisition
4.2. Community Suggestions for Health Education Strategies
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arsenic. World Health Organization 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/arsenic (accessed on 5 October 2022).
- Podgorski, J.; Berg, M. Global threat of arsenic in groundwater. Science 2020, 368, 845–850. [Google Scholar] [CrossRef] [PubMed]
- US EPA, O. Chemical Contaminant Rules. 2015. Available online: https://www.epa.gov/dwreginfo/chemical-contaminant-rules (accessed on 6 October 2022).
- Balazs, C.L.; Morello-Frosch, R.; Hubbard, A.E.; Ray, I. Environmental justice implications of arsenic contamination in California’s San Joaquin Valley: A cross-sectional, cluster-design examining exposure and compliance in community drinking water systems. Environ. Health 2012, 11, 84. [Google Scholar] [CrossRef] [PubMed]
- Frisbie, S.H.; Mitchell, E.J. Arsenic in drinking water: An analysis of global drinking water regulations and recommendations for updates to protect public health. PLoS ONE 2022, 17, e0263505. [Google Scholar] [CrossRef] [PubMed]
- Naujokas, M.F.; Anderson, B.; Ahsan, H.; Aposhian, H.V.; Graziano, J.H.; Thompson, C.; Suk, W.A. The Broad Scope of Health Effects from Chronic Arsenic Exposure: Update on a Worldwide Public Health Problem. Environ. Health Perspect. 2013, 121, 295–302. [Google Scholar] [CrossRef]
- Hasanvand, M.; Mohammadi, R.; Khoshnamvand, N.; Jafari, A.; Palangi, H.S.; Mokhayeri, Y. Dose-response meta-analysis of arsenic exposure in drinking water and intelligence quotient. J. Env. Health Sci. Eng. 2020, 18, 1691–1697. [Google Scholar] [CrossRef]
- Kuo, C.-C.; Moon, K.A.; Wang, S.-L.; Silbergeld, E.; Navas-Acien, A. The Association of Arsenic Metabolism with Cancer, Cardiovascular Disease, and Diabetes: A Systematic Review of the Epidemiological Evidence. Environ. Health Perspect. 2017, 125, 087001. [Google Scholar] [CrossRef]
- Mayer, J.E.; Goldman, R.H. Arsenic and skin cancer in the USA: The current evidence regarding arsenic-contaminated drinking water. Int. J. Dermatol. 2016, 55, e585–e591. [Google Scholar] [CrossRef]
- Shakoor, M.B.; Nawaz, R.; Hussain, F.; Raza, M.; Ali, S.; Rizwan, M.; Oh, S.-E.; Ahmad, S. Human health implications, risk assessment and remediation of As-contaminated water: A critical review. Sci. Total Environ. 2017, 601–602, 756–769. [Google Scholar] [CrossRef]
- Sinha, D.; Prasad, P. Health effects inflicted by chronic low-level arsenic contamination in groundwater: A global public health challenge. J. Appl. Toxicol. 2020, 40, 87–131. [Google Scholar] [CrossRef]
- IARC. Arsenic, Metals, Fibres, and Dusts; IARC: Lyon, France, 2012; ISBN 978-92-832-1320-8. [Google Scholar]
- Pelton, T.; Bernhardt, C.; Schaeffer, E. Arsenic in California Drinking Water: Three Years After EPA Notice of Noncompliance to State, Arsenic Levels Still Unsafe in Drinking Water for 55,000 Californians 2016. Available online: https://environmentalintegrity.org/wp-content/uploads/CA-Arsenic-Report.pdf (accessed on 17 March 2022).
- U.S. Environmental Protection Agency. Information about Public Water Systems. 2021. Available online: https://www.epa.gov/dwreginfo/information-about-public-water-systems (accessed on 5 October 2022).
- Small Water Systems Program. Sacramento County Environmental Management n.d. Available online: https://emd.saccounty.net:443/EC/Pages/Smallwater.aspx (accessed on 5 October 2022).
- London, J.; Fencl, A.; Watterson, S.; Jarin, J.; Aranda, A.; King, A.; Pannu, C.; Seaton, P.; Firestone, L.; Dawson, M.; et al. The Struggle for Water Justice in California’s San Joaquin Valley: A Focus on Disadvantaged Unincorporated Communities; UC Davis: Center for Regional Change: Davis, CA, USA, 2018. [Google Scholar]
- GAMA—Domestic Well Project Site | California State Water Resources Control Board. CAGov n.d. Available online: https://www.waterboards.ca.gov/gama/domestic_well.html (accessed on 5 October 2022).
- Martin United Nations Sustainable Development Goals: Water and Sanitation. United Nations Sustainable Development n.d. Available online: https://www.un.org/sustainabledevelopment/water-and-sanitation/ (accessed on 3 December 2022).
- Flegal, L.; Rice, S.; Mann, J.; Tran, J. California Unincorporated: Mapping Disadvantaged Communities in the San Joaquin Valley; PolicyLink: San Joaquin Valley, CA, USA, 2013; p. 48. [Google Scholar]
- Balazs, C.L.; Ray, I. The Drinking Water Disparities Framework: On the Origins and Persistence of Inequities in Exposure. Am. J. Public Health 2014, 104, 603–611. [Google Scholar] [CrossRef]
- VanDerslice, J. Drinking Water Infrastructure and Environmental Disparities: Evidence and Methodological Considerations. Am. J. Public Health 2011, 101, S109–S114. [Google Scholar] [CrossRef] [PubMed]
- U.S. Environmental Protection Agency. Public Notification Rule. United States Environmental Protection Agency 2015. Available online: https://www.epa.gov/dwreginfo/public-notification-rule (accessed on 5 October 2022).
- California Drinking Water-Related Laws | California State Water Resources Control Board. CAGov n.d. Available online: https://www.waterboards.ca.gov/drinking_water/certlic/drinkingwater/Lawbook.html (accessed on 5 October 2022).
- Frequently Asked Questions: Public Water System Data on the Human Right to Water Portal. Available online: https://www.waterboards.ca.gov/water_issues/programs/hr2w/docs/general/faqs.pdf (accessed on 5 October 2022).
- Dubrovsky, N.M.; Burow, K.R.; Clark, G.M.; Gronberg, J.A.; Hamilton, P.A.; Hitt, K.J.; Mueller, D.K.; Munn, M.D.; Nolan, B.T.; Puckett, L.J.; et al. The Quality of Our Nation’s Waters--Nutrients in the Nation’s Streams and Groundwater, 1992–2004: U.S. Geological Survey Circular 1350; U.S. Geological Survey: Reston, VA, USA, 2010; p. 174.
- Smith, R.; Knight, R.; Fendorf, S. Overpumping leads to California groundwater arsenic threat. Nat. Commun. 2018, 9, 2089. [Google Scholar] [CrossRef] [PubMed]
- Bangia, K.; August, L.; Slocombe, A.; Faust, J. Assessment of contaminants in California drinking water by region and system size. AWWA Water Sci. 2020, 2, e1194. [Google Scholar] [CrossRef]
- Estimated population with arsenic greater than 10 micrograms per liter | U.S. Geological Survey. Available online: https://www.usgs.gov/media/images/estimated-population-arsenic-greater-10-micrograms-liter (accessed on 3 December 2022).
- San Joaquin Valley | California, United States | Britannica. Britannica 2009. Available online: https://www.britannica.com/place/San-Joaquin-Valley (accessed on 21 February 2022).
- American Community Survey: Selected Characteristics of the Total and Native Populations in the United States. United States Census Bureau 2021. Available online: https://data.census.gov/cedsci/table?q=Fresno%20Merced%20Madera%20Kern%20county%20Kings%20Stanislaus%20San%20Joaquin%20Tulare%20county%20acs%20race&tid=ACSST1Y2021.S0601 (accessed on 21 February 2022).
- Pace, C.; Balazs, C.; Bangia, K.; Depsky, N.; Renteria, A.; Morello-Frosch, R.; Cushing, L.J. Inequities in Drinking Water Quality Among Domestic Well Communities and Community Water Systems, California, 2011–2019. Am. J. Public Health 2022, 112, 88–97. [Google Scholar] [CrossRef]
- Amrose, S.; Burt, Z.; Ray, I. Safe Drinking Water for Low-Income Regions. Annu. Rev. Environ. Resour. 2015, 40, 203–231. [Google Scholar] [CrossRef]
- Chen, Y.; van Geen, A.; Graziano, J.H.; Pfaff, A.; Madajewicz, M.; Parvez, F.; Hussain, A.Z.M.I.; Slavkovich, V.; Islam, T.; Ahsan, H. Reduction in Urinary Arsenic Levels in Response to Arsenic Mitigation Efforts in Araihazar, Bangladesh. Env. Health Perspect. 2007, 115, 917–923. [Google Scholar] [CrossRef]
- Shantz, A.; Chanthea, C.; Makara, T.; Phalla, H.; Daniell, W. A Study of Options for Safe Water Access in Arsenic Affected Communities in Cambodia; Water and Sanitation Programme; Resource Development International Cambodia: Phnom Penh, Cambodia, 2012. [Google Scholar]
- Jones-Hughes, T.; Peters, J.; Whear, R.; Cooper, C.; Evans, H.; Depledge, M.; Pearson, M. Are interventions to reduce the impact of arsenic contamination of groundwater on human health in developing countries effective? A systematic review. Environ. Evid. 2013, 2, 11. [Google Scholar] [CrossRef]
- German, M.; Seingheng, H.; SenGupta, A.K. Mitigating arsenic crisis in the developing world: Role of robust, reusable and selective hybrid anion exchanger (HAIX). Sci. Total Env. 2014, 488–489, 547–553. [Google Scholar] [CrossRef]
- Litter, M.I.; Alarcón-Herrera, M.T.; Arenas, M.J.; Armienta, M.A.; Avilés, M.; Cáceres, R.E.; Cipriani, H.N.; Cornejo, L.; Dias, L.E.; Cirelli, A.F.; et al. Small-scale and household methods to remove arsenic from water for drinking purposes in Latin America. Sci. Total Env. 2012, 429, 107–122. [Google Scholar] [CrossRef]
- Amrose, S.E.; Bandaru, S.R.S.; Delaire, C.; van Genuchten, C.M.; Dutta, A.; DebSarkar, A.; Orr, C.; Roy, J.; Das, A.; Gadgil, A.J. Electro-chemical arsenic remediation: Field trials in West Bengal. Sci. Total Env. 2014, 488–489, 539–546. [Google Scholar] [CrossRef]
- Hernandez, D.; Boden, K.; Paul, P.; Bandaru, S.; Mypati, S.; Roy, A.; Amrose, S.; Roy, J.; Gadgil, A. Strategies for successful field deployment in a resource-poor region: Arsenic remediation technology for drinking water. Dev. Eng. 2019, 4, 100045. [Google Scholar] [CrossRef]
- Bandaru, S.R.S.; van Genuchten, C.M.; Kumar, A.; Glade, S.; Hernandez, D.; Nahata, M.; Gadgil, A. Rapid and Efficient Arsenic Removal by Iron Electrocoagulation Enabled with in Situ Generation of Hydrogen Peroxide. Environ. Sci. Technol. 2020, 54, 6094–6103. [Google Scholar] [CrossRef] [PubMed]
- Balazs, C.L.; Morello-Frosch, R. The Three R’s: How Community Based Participatory Research Strengthens the Rigor, Relevance and Reach of Science. Env. Justice 2013, 6, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Minkler, M.; Vásquez, V.B.; Tajik, M.; Petersen, D. Promoting Environmental Justice Through Community-Based Participatory Research: The Role of Community and Partnership Capacity. Health Educ. Behav. 2008, 35, 119–137. [Google Scholar] [CrossRef] [PubMed]
- Israel, B.A.; Parker, E.A.; Rowe, Z.; Salvatore, A.; Minkler, M.; López, J.; Butz, A.; Mosley, A.; Coates, L.; Lambert, G.; et al. Community-Based Participatory Research: Lessons Learned from the Centers for Children’s Environmental Health and Disease Prevention Research. Environ. Health Perspect. 2005, 113, 1463–1471. [Google Scholar] [CrossRef] [PubMed]
- Minkler, M.; Blackwell, A.G.; Thompson, M.; Tamir, H. Community-Based Participatory Research: Implications for Public Health Funding. Am. J. Public Health 2003, 93, 1210. [Google Scholar] [CrossRef]
- Corburn, J. Street Science: Community Knowledge and Environmental Health Justice; Urban and industrial environments; MIT Press: Cambridge, MA, USA, 2005; ISBN 978-0-262-03333-6. [Google Scholar]
- Cornwall, A.; Jewkes, R. What is participatory research? Soc. Sci. Med. 1995, 41, 1667–1676. [Google Scholar] [CrossRef]
- Glaser, B.G. The Constant Comparative Method of Qualitative Analysis. Soc. Probl. 1965, 12, 436–445. [Google Scholar] [CrossRef]
- Paul, B.K. Arsenic contamination awareness among the rural residents in Bangladesh. Soc. Sci. Med. 2004, 59, 1741–1755. [Google Scholar] [CrossRef]
- Rampey, B.; Xie, H.; Provasnik, S. Highlights of the 2017 U.S. PIAAC Results Web Report. National Center for Education Statistics 2019. Available online: https://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2020777 (accessed on 6 October 2022).
- Kutner, M.; Greenberg, E.; Jin, Y.; Paulsen, C. The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy; Institute of Education Sciences, National Center for Education Statistics: Washington, DC, USA, 2006; p. 76. [Google Scholar]
- Neuhauser, L. Integrating participatory design and health literacy to improve research and interventions. Inf. Serv. Use 2017, 37, 153–176. [Google Scholar] [CrossRef]
- Neuhauser, L.; Kreps, G.L. Online cancer communication: Meeting the literacy, cultural and linguistic needs of diverse audiences. Patient Educ. Couns. 2008, 71, 365–377. [Google Scholar] [CrossRef] [PubMed]
- Kreps, G.L.; Neuhauser, L.; Sparks, L.; Labelle, S. Promoting Convergence Between Health Literacy and Health Communication. Health Lit. Clin. Pract. Public Health 2020, 269, 526–543. [Google Scholar] [CrossRef]
- Khan, K.; Ahmed, E.; Factor-Litvak, P.; Liu, X.; Siddique, A.B.; Wasserman, G.A.; Slavkovich, V.; Levy, D.; Mey, J.L.; van Geen, A.; et al. Evaluation of an Elementary School–based Educational Intervention for Reducing Arsenic Exposure in Bangladesh. Environ. Health Perspect. 2015, 123, 1331–1336. [Google Scholar] [CrossRef] [PubMed]
- Cline, T.; Crafter, S.; O’Dell, L.; de Abreu, G. Young people’s representations of language brokering. J. Multiling. Multicult. Dev. 2011, 32, 207–220. [Google Scholar] [CrossRef]
- Morales, A.; Hanson, W.E. Language Brokering: An Integrative Review of the Literature. Hisp. J. Behav. Sci. 2005, 27, 471–503. [Google Scholar] [CrossRef]
- Valdés, G.; Chávez, C.; Angelelli, C. A Performance Team: Young Interpreters and Their Parents. In Expanding Definitions of Giftedness; Routledge: Mahwah, NJ, USA, 2003; ISBN 978-1-4106-0724-9. [Google Scholar]
- Pietrucha-Urbanik, K.; Rak, J.R. Consumers’ Perceptions of the Supply of Tap Water in Crisis Situations. Energies 2020, 13, 3617. [Google Scholar] [CrossRef]
| CI Type | Job Type |
|---|---|
| Tribal Nation Leaders | Director of Education Center, Director of Recreation, Grounds Supervisor, Utilities Assistant Manager |
| Rural Community Leaders | Head of Community Board, Community Board Leaders, Pastor |
| Rural Community Residents | Farmer, Pipeline Welder, Daycare Provider, Health Clinic Worker |
| Local School District Members | School Board, Superintendent, Principal, Teacher, Parent |
| Public Water Representatives | State Water Board Member, State Water Engineer, County Environmental Health Officer, Local Water District Manager, Regional Manager, Program Manager |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boyden, H.; Gillan, M.; Molina, J.; Gadgil, A.; Tseng, W. Community Perceptions of Arsenic Contaminated Drinking Water and Preferences for Risk Communication in California’s San Joaquin Valley. Int. J. Environ. Res. Public Health 2023, 20, 813. https://doi.org/10.3390/ijerph20010813
Boyden H, Gillan M, Molina J, Gadgil A, Tseng W. Community Perceptions of Arsenic Contaminated Drinking Water and Preferences for Risk Communication in California’s San Joaquin Valley. International Journal of Environmental Research and Public Health. 2023; 20(1):813. https://doi.org/10.3390/ijerph20010813
Chicago/Turabian StyleBoyden, Hollynd, Mayela Gillan, Javier Molina, Ashok Gadgil, and Winston Tseng. 2023. "Community Perceptions of Arsenic Contaminated Drinking Water and Preferences for Risk Communication in California’s San Joaquin Valley" International Journal of Environmental Research and Public Health 20, no. 1: 813. https://doi.org/10.3390/ijerph20010813
APA StyleBoyden, H., Gillan, M., Molina, J., Gadgil, A., & Tseng, W. (2023). Community Perceptions of Arsenic Contaminated Drinking Water and Preferences for Risk Communication in California’s San Joaquin Valley. International Journal of Environmental Research and Public Health, 20(1), 813. https://doi.org/10.3390/ijerph20010813








