The Impact of Wearable Devices on Physical Activity for Chronic Disease Patients: Findings from the 2019 Health Information National Trends Survey
Abstract
:1. Introduction
2. Methods
2.1. Data
2.1.1. The Use of Wearable Devices
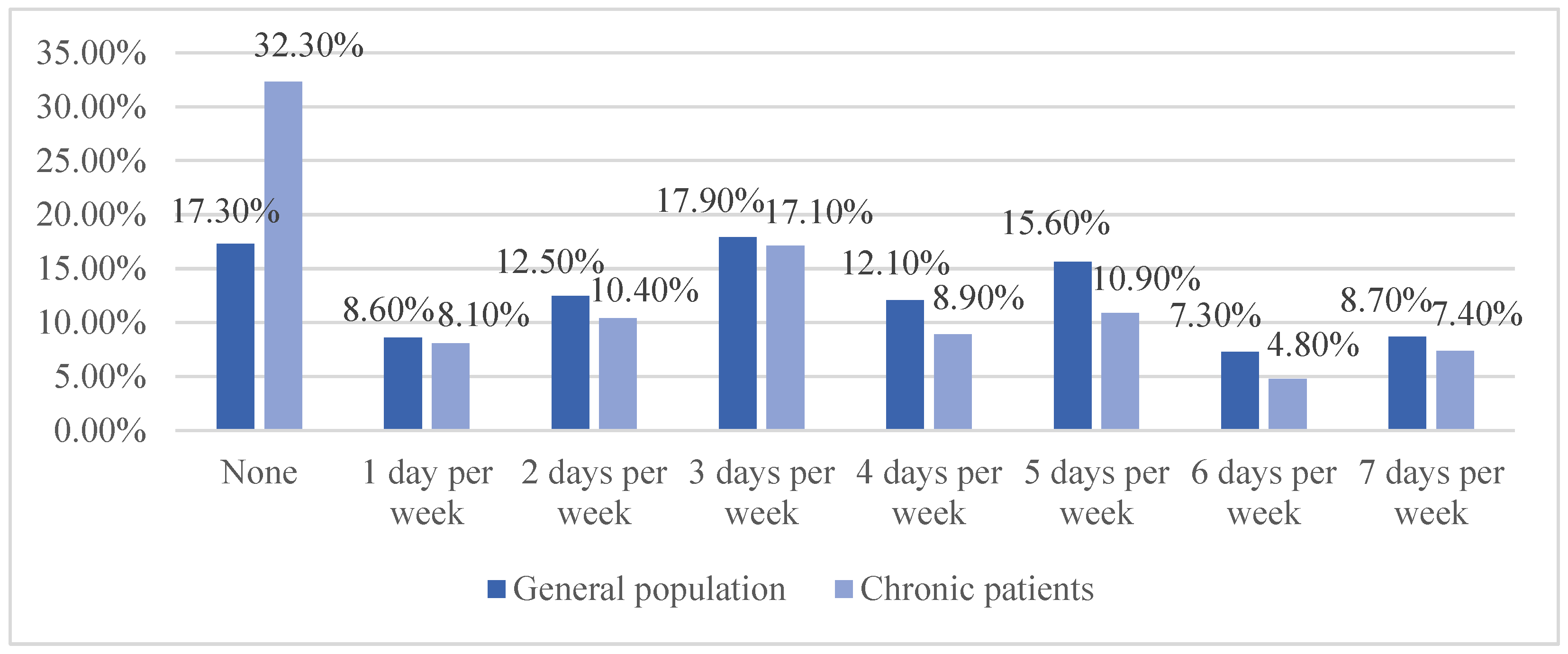
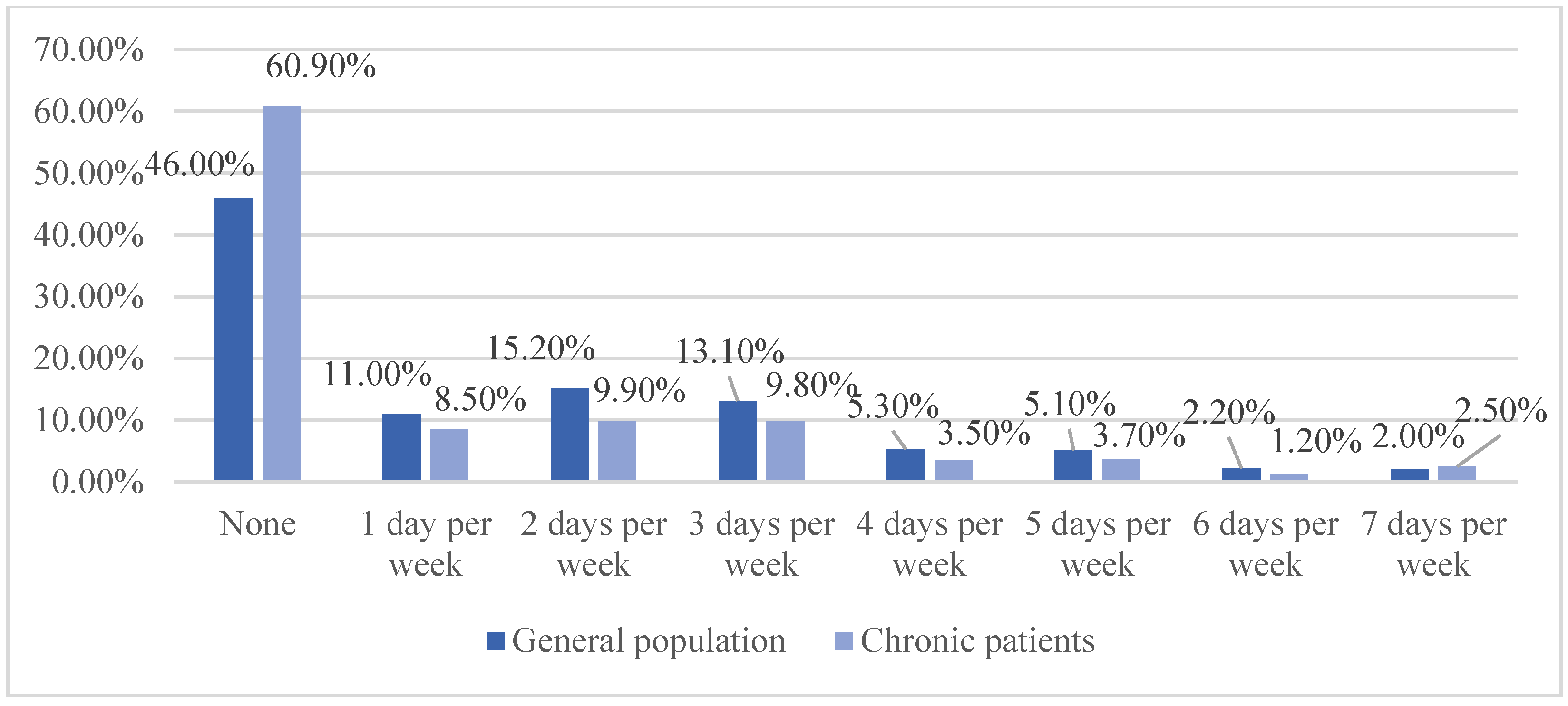
2.1.2. Physical Activity
2.1.3. Covariates
2.2. Analysis
3. Results
3.1. Descriptive Statistics
3.2. Balance of Covariates
3.3. The Impact of Wearable Device Use on Physical Activity
3.4. The Impact of Frequency of Using Wearable Device on Physical Activity
4. Discussion
4.1. Improving Physical Activity by Wearable Devices
4.2. More Benefits for Chronic Patients by Wearable Devices
4.3. Different Effects on Different Chronic Patients
4.4. Strength and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Supplementary Results
| No | Variable | Stats/Values | Freqs (% of Valid) | Valid | Missing |
|---|---|---|---|---|---|
| 1 | Diabetes | Min: 0 Mean: 0.2 Max: 1 | 0: 4147 (78.3%) 1: 1149 (21.7%) | 5296 (97.39%) | 142 (2.61%) |
| 2 | Hypertension | Min: 0 Mean: 0.5 Max: 1 | 0: 2917 (55.0%) 1: 2390 (45.0%) | 5307 (97.59%) | 131 (2.41%) |
| 3 | Heart condition | Min: 0 Mean: 0.1 Max:1 | 0: 4795 (90.1%) 1: 526 (9.9%) | 5321 (97.85%) | 117 (2.15%) |
| 4 | Lung disease | Min: 0 Mean: 0.1 Max:1 | 0: 4697 (88.2%) 1: 631 (11.8%) | 5328 (97.98%) | 110 (2.02%) |
| 5 | Depression | Min: 0 Mean: 0.2 Max:1 | 0: 4168 (78.5%) 1: 1139 (21.5%) | 5307 (97.59%) | 131 (2.41%) |
| Matched Sample Means | var Ratio (Tr/Co) | p-Value | ||
|---|---|---|---|---|
| Mean Treatment | Mean Control | |||
| Age Age 18–31 years (referent) Age 31–40 years | ||||
| before matched | 0.191 | 0.103 | 1.676 | <0.001 |
| after matched | 0.191 | 0.187 | 1.017 | 0.635 |
| Age 41–50 years | ||||
| before matched | 0.175 | 0.127 | 1.308 | <0.001 |
| after matched | 0.175 | 0.184 | 0.962 | 0.317 |
| Age 51–64 years | ||||
| before matched | 0.305 | 0.300 | 1.011 | 0.737 |
| after matched | 0.305 | 0.316 | 0.982 | 0.242 |
| Age 65+ | ||||
| before matched | 0.183 | 0.400 | 0.625 | <0.001 |
| after matched | 0.183 | 0.177 | 1.030 | 0.227 |
| Gender Male (referent) Female | ||||
| before matched | 0.604 | 0.554 | 0.968 | 0.003 |
| after matched | 0.604 | 0.606 | 1.002 | 0.480 |
| Education High school or less (referent) Some college | ||||
| before matched | 0.266 | 0.308 | 0.917 | 0.007 |
| after matched | 0.266 | 0.270 | 0.992 | 0.793 |
| College or more | ||||
| before matched | 0.643 | 0.421 | 0.942 | <0.001 |
| after matched | 0.643 | 0.637 | 0.993 | 0.668 |
| Income <$20,000 (referent) $20,000 to $49,999 | ||||
| before matched | 0.164 | 0.288 | 0.670 | <0.001 |
| after matched | 0.164 | 0.164 | 1 | 1 |
| $50,000 to $99,999 | ||||
| before matched | 0.341 | 0.293 | 1.084 | 0.004 |
| after matched | 0.341 | 0.351 | 0.985 | 0.005 |
| $100,000 or more | ||||
| before matched | 0.435 | 0.200 | 1.539 | <0.001 |
| after matched | 0.435 | 0.426 | 1.005 | 0.007 |
| Medical insurance No medical insurance (referent) Have medical insurance | ||||
| before matched | 0.177 | 0.407 | 0.604 | <0.001 |
| after matched | 0.177 | 0.177 | 1 | 1 |
| Overall health condition Poor (referent) Good | ||||
| before matched | 3.699 | 3.335 | 0.859 | <0.001 |
| after matched | 3.699 | 3.687 | 1.078 | 0.109 |
| Historical experience of using wearable devices No experience (referent) Have experience | ||||
| before matched | 0.304 | 0.291 | 1.025 | 0.431 |
| after matched | 0.304 | 0.301 | 1.005 | 0.180 |
| Weight perception Right weight (referent) Slightly overweight/underweight | ||||
| before matched | 0.454 | 0.428 | 1.013 | 0.124 |
| after matched | 0.454 | 0.458 | 0.999 | 0.157 |
| Overweight/Underweight | ||||
| before matched | 0.330 | 0.311 | 1.031 | 0.254 |
| after matched | 0.330 | 0.330 | 1 | 1 |
| Willingness to change weight No attention (referent) Maintain weight | ||||
| before matched | 0.186 | 0.248 | 0.812 | <0.001 |
| after matched | 0.186 | 0.188 | 0.993 | 0.157 |
| Lose/gain weight | ||||
| before matched | 0.705 | 0.502 | 0.833 | <0.001 |
| after matched | 0.705 | 0.705 | 1 | 1 |
| Matched Sample Means | var Ratio (Tr/Co) | t-Test p-Value | ||
|---|---|---|---|---|
| Mean Treatment | Mean Control | |||
| Age Age 18–31 years (referent) Age 31–40 years | ||||
| before matched | 0.200 | 0.157 | 1.21 | 0.058 |
| after matched | 0.20 | 0.203 | 0.991 | 0.157 |
| Age 41–50 years | ||||
| before matched | 0.183 | 0.138 | 1.255 | 0.042 |
| after matched | 0.183 | 0.183 | 1 | 1 |
| Age 51–64 years | ||||
| before matched | 0.288 | 0.363 | 0.885 | 0.010 |
| after matched | 0.288 | 0.288 | 1 | 1 |
| Age 65+ | ||||
| before matched | 0.191 | 0.212 | 0.923 | 0.400 |
| after matched | 0.191 | 0.191 | 1 | 1 |
| Marital status Divorced (referent) Living as married | ||||
| before matched | 0.0548 | 0.061 | 0.902 | 0.669 |
| after matched | 0.0548 | 0.070 | 0.796 | 0.002 |
| Married | ||||
| before matched | 0.613 | 0.512 | 0.948 | 0.001 |
| after matched | 0.613 | 0.621 | 1.008 | 0.032 |
| Separated | ||||
| before matched | 0.016 | 0.027 | 0.621 | 0.275 |
| after matched | 0.016 | 0.008 | 1.984 | 0.008 |
| Single, never been married | ||||
| before matched | 0.164 | 0.186 | 0.907 | 0.368 |
| after matched | 0.164 | 0.170 | 0.975 | 0.121 |
| Widowed | ||||
| before matched | 0.045 | 0.074 | 0.630 | 0.060 |
| after matched | 0.045 | 0.042 | 1.079 | 0.083 |
| Degree of enjoying exercise Don’t enjoy (referent) Enjoy | ||||
| before matched | 2.965 | 2.852 | 0.945 | 0.046 |
| after matched | 2.965 | 2.965 | 1 | 1 |
References
- Booth, F.W.; Roberts, C.K.; Laye, M.J. Lack of Exercise Is a Major Cause of Chronic Diseases. Compr. Physiol. 2012, 2, 1143–1211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yen, H.-Y.; Liao, Y.; Huang, H.-Y. Smart Wearable Device Users’ Behavior Is Essential for Physical Activity Improvement. Int. J. Behav. Med. 2022, 29, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Gorina, M.; Limonero, J.T.; Alvarez, M. Educational Diagnosis of Self-Management Behaviours in Patients with Diabetes Mellitus, Hypertension and Hypercholesterolaemia Based on the PRECEDE Model: Qualitative Study. J. Clin. Nurs. 2019, 28, 1745–1759. [Google Scholar] [CrossRef] [PubMed]
- Bacon, S.L.; Sherwood, A.; Hinderliter, A.; Blumenthal, J.A. Effects of Exercise, Diet and Weight Loss on High Blood Pressure. Sports Med. 2004, 34, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, J.E.; Blair, S.N.; Jakicic, J.M.; Manore, M.M.; Rankin, J.W.; Smith, B.K. Appropriate Physical Activity Intervention Strategies for Weight Loss and Prevention of Weight Regain for Adults. Med. Sci. Sports Exerc. 2009, 41, 459–471. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, S.; Thoma, C.; Houghton, D.; Trenell, M.I. High-Intensity Interval Training: A Review of Its Impact on Glucose Control and Cardiometabolic Health. Diabetologia 2017, 60, 7–23. [Google Scholar] [CrossRef] [Green Version]
- Puhan, M.A.; Gimeno-Santos, E.; Cates, C.J.; Troosters, T. Pulmonary Rehabilitation Following Exacerbations of Chronic Obstructive Pulmonary Disease. Cochrane Database Syst. Rev. 2016, 12, CD005305. [Google Scholar] [CrossRef]
- Smith, P.J.; Merwin, R.M. The role of exercise in management of mental health disorders: An integrative review. Ann. Rev. Med. 2021, 72, 45–62. [Google Scholar]
- Franssen, W.M.A.; Franssen, G.H.L.M.; Spaas, J.; Solmi, F.; Eijnde, B.O. Can Consumer Wearable Activity Tracker-Based Interventions Improve Physical Activity and Cardiometabolic Health in Patients with Chronic Diseases? A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 57. [Google Scholar] [CrossRef]
- Brickwood, K.-J.; Watson, G.; O’Brien, J.; Williams, A.D. Consumer-Based Wearable Activity Trackers Increase Physical Activity Participation: Systematic Review and Meta-Analysis. JMIR mHealth uHealth 2019, 7, e11819. [Google Scholar] [CrossRef]
- Lyons, E.J.; Swartz, M.C.; Lewis, Z.H.; Martinez, E.; Jennings, K. Feasibility and Acceptability of a Wearable Technology Physical Activity Intervention with Telephone Counseling for Mid-Aged and Older Adults: A Randomized Controlled Pilot Trial. JMIR Mhealth Uhealth 2017, 5, e28. [Google Scholar] [CrossRef]
- Ellis, D.A.; Piwek, L. Failing to Encourage Physical Activity with Wearable Technology: What Next? J. R. Soc. Med. 2018, 111, 310–313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boehn, B.; Karwiese, S.D.; Boehm, H.; Oberhoffer, R. Effects of Mobile Health Including Wearable Activity Trackers to Increase Physical Activity Outcomes among Healthy Children and Adolescents: Systematic Review. JMIR mHealth uHealth 2019, 7, e8298. [Google Scholar] [CrossRef]
- Huh, U.; Tak, Y.J.; Song, S.; Chung, S.W.; Sung, S.M.; Lee, C.W.; Bae, M.; Ahn, H.Y. Feedback on Physical Activity through a Wearable Device Connected to a Mobile Phone App in Patients With Metabolic Syndrome: Pilot Study. JMIR Mhealth Uhealth 2019, 7, e13381. [Google Scholar] [CrossRef] [PubMed]
- Chang, R.C.-S.; Lu, H.-P.; Yang, P.; Luarn, P. Reciprocal Reinforcement Between Wearable Activity Trackers and Social Network Services in Influencing Physical Activity Behaviors. JMIR mHealth uHealth 2016, 4, e84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jang, I.-Y.; Kim, H.R.; Lee, E.; Jung, H.-W.; Park, H.; Cheon, S.-H.; Lee, Y.S.; Park, Y.R. Impact of a Wearable Device-Based Walking Programs in Rural Older Adults on Physical Activity and Health Outcomes: Cohort Study. JMIR mHealth uHealth 2018, 6, e11335. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.-M.; Ho, T.-W.; Chang, Y.-T.; Hsu, C.; Tsai, C.J.; Lai, F.; Lin, M.-T. Wearable-Based Mobile Health App in Gastric Cancer Patients for Postoperative Physical Activity Monitoring: Focus Group Study. JMIR mHealth uHealth 2019, 7, e11989. [Google Scholar] [CrossRef]
- Powell, L.; Parker, J.; St-James, M.M.; Mawson, S. The Effectiveness of Lower-Limb Wearable Technology for Improving Activity and Participation in Adult Stroke Survivors: A Systematic Review. J. Med. Internet Res. 2016, 18, e259. [Google Scholar] [CrossRef]
- Turner, K.; Jo, A.; Wei, G.; Tabriz, A.A.; Clary, A.; Jim, H.S.L. Sharing Patient-Generated Data with Healthcare Providers: Findings from a 2019 National Survey. J. Am. Med. Inf. Assoc. 2021, 28, 371–376. [Google Scholar] [CrossRef]
- Gupta, A.; Dhiman, N.; Yousaf, A.; Arora, N. Social Comparison and Continuance Intention of Smart Fitness Wearables: An Extended Expectation Confirmation Theory Perspective. Behav. Inf. Technol. 2021, 40, 1341–1354. [Google Scholar] [CrossRef]
- Park, E. User Acceptance of Smart Wearable Devices: An Expectation-Confirmation Model Approach. Telemat. Inform. 2020, 47, 101318. [Google Scholar] [CrossRef]
- Sekhon, J.S. Multivariate and Propensity Score Matching Software with Automated Balance Optimization: The Matching Package for R. J. Stat. Softw. 2011, 42, 1–52. [Google Scholar] [CrossRef] [Green Version]
- Sekhon, J.S.; Grieve, R.D. A Matching Method for Improving Covariate Balance in Cost-Effectiveness Analyses. Health Econ. 2012, 21, 695–714. [Google Scholar] [CrossRef] [PubMed]
- Kreif, N.; Grieve, R.; Radice, R.; Sadique, Z.; Ramsahai, R.; Sekhon, J.S. Methods for Estimating Subgroup Effects in Cost-Effectiveness Analyses That Use Observational Data. Med. Decis. Mak. 2012, 32, 750–763. [Google Scholar] [CrossRef] [PubMed]
- Soto-Gordoa, M.; de Manuel, E.; Fullaondo, A.; Merino, M.; Arrospide, A.; Ignacio Igartua, J.; Mar, J. Impact of Stratification on the Effectiveness of a Comprehensive Patient-Centered Strategy for Multimorbid Patients. Health Serv. Res. 2019, 54, 466–473. [Google Scholar] [CrossRef]
- Phillips, S.M.; Cadmus-Bertram, L.; Rosenberg, D.; Buman, M.P.; Lynch, B.M. Wearable Technology and Physical Activity in Chronic Disease: Opportunities and Challenges. Am. J. Prev. Med. 2018, 54, 144–150. [Google Scholar] [CrossRef]
- Lorig, K.R.; Holman, H.R. Self-Management Education: History, Definition, Outcomes, and Mechanisms. Ann. Behav. Med. 2003, 26, 1–7. [Google Scholar] [CrossRef]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. JAMA-J. Am. Med. Assoc. 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- HajGhanbari, B.; Holsti, L.; Road, J.D.; Reid, W.D. Pain in People with Chronic Obstructive Pulmonary Disease (COPD). Respir. Med. 2012, 106, 998–1005. [Google Scholar] [CrossRef] [Green Version]
- Elsawy, B.; Higgins, K.E. Physical Activity Guidelines for Older Adults. Am. Fam. Physician 2010, 81, 55–59. [Google Scholar]
- Dontje, M.L.; Krijnen, W.P.; de Greef, M.H.G.; Peeters, G.G.M.E.E.; Stolk, R.P.; van der Schans, C.P.; Brown, W.J. Effect of Diagnosis with a Chronic Disease on Physical Activity Behavior in Middle-Aged Women. Prev. Med. 2016, 83, 56–62. [Google Scholar] [CrossRef]
- Rabbi, M.; Pfammatter, A.; Zhang, M.; Spring, B.; Choudhury, T. Automated Personalized Feedback for Physical Activity and Dietary Behavior Change With Mobile Phones: A Randomized Controlled Trial on Adults. JMIR mHealth uHealth 2015, 3, e42. [Google Scholar] [CrossRef] [PubMed]
- Jerant, A.F.; von Friederichs-Fitzwater, M.M.; Moore, M. Patients’ Perceived Barriers to Active Self-Management of Chronic Conditions. Patient Educ. Couns. 2005, 57, 300–307. [Google Scholar] [CrossRef] [PubMed]
- Weston, K.S.; Wisloff, U.; Coombes, J.S. High-Intensity Interval Training in Patients with Lifestyle-Induced Cardiometabolic Disease: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2014, 48, 1227-U52. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, S.; Rusu, C.; Bernatsky, S.; Hawker, G.; Canizares, M.; MacKay, C.; Badley, E. Exercise/Physical Activity and Weight Management Efforts in Canadians with Self-Reported Arthritis. Arthritis Care Res. 2013, 65, 2015–2023. [Google Scholar] [CrossRef] [PubMed]
- Keats, M.R.; Cui, Y.; DeClercq, V.; Dummer, T.J.B.; Forbes, C.; Grandy, S.A.; Hicks, J.; Sweeney, E.; Yu, Z.M.; Parker, L. Multimorbidity in Atlantic Canada and Association with Low Levels of Physical Activity. Prev. Med. 2017, 105, 326–331. [Google Scholar] [CrossRef]
- Li, X.; Li, T.; Chen, J.; Xie, Y.; An, X.; Lv, Y.; Lin, A. A WeChat-Based Self-Management Intervention for Community Middle-Aged and Elderly Adults with Hypertension in Guangzhou, China: A Cluster-Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 16, 4058. [Google Scholar] [CrossRef] [Green Version]
- Bapna, R.; Ramaprasad, J.; Umyarov, A. Monetizing Freemium Communities: Does Paying for Premium Increase Social Engagement? MIS Q. 2018, 42, 719. [Google Scholar] [CrossRef]
| Proportion of the Whole Population Using Wearable Devices in at Least Moderate Exercise | Proportion of Chronic Patients Using Wearable Devices in at Least Moderate Exercise | Proportion of the Whole Population Using Wearable Devices in Strength Training | Proportion of Chronic Patients Using Wearable Devices Strength Training | |
|---|---|---|---|---|
| None | 12.39% | 11.78% | 18.56% | 17.10% |
| 1 day/week | 24.34% | 20.69% | 35.24% | 31.76% |
| 2 days/week | 27.23% | 26.98% | 34.00% | 31.52% |
| 3 days/week | 30.09% | 27.08% | 34.30% | 28.36% |
| 4 days/week | 32.17% | 27.78% | 28.49% | 28.72% |
| 5 days/week | 34.68% | 29.93% | 42.62% | 40.82% |
| 6 days/week | 30.49% | 29.92% | 42.42% | 37.93% |
| 7 days/week | 29.94% | 26.80% | 17.71% | 14.06% |
| Frequency of at Least Moderate Exercise (Times per Week) | Duration of at Least Moderate Exercise in One Day (Minute) | Frequency of Strength Training (Times per Week) | ||||
|---|---|---|---|---|---|---|
| Estimate | p-Value | Estimate | p-Value | Estimate | p-Value | |
| Whole Population | 0.460 | <0.001 | −0.802 | 0.756 | 0.402 | <0.001 |
| Chronic Patients | 0.471 | <0.001 | 1.301 | 0.738 | 0.363 | 0.002 |
| Diabetes | 0.557 | 0.032 | −1.305 | 0.884 | 0.354 | 0.094 |
| Hypertension | 0.328 | 0.058 | −1.409 | 0.774 | 0.443 | 0.003 |
| Heart condition | 0.737 | 0.053 | 9.174 | 0.578 | 0.200 | 0.599 |
| Lung disease | 0.578 | 0.070 | 7.333 | 0.340 | 0.500 | 0.069 |
| Depression | 0.670 | 0.005 | 8.590 | 0.093 | 0.355 | 0.056 |
| Frequency of at Least Moderate Exercise (Times per Week) | Duration of at Least Moderate Exercise in One Day (Minute) | Frequency of Strength Training (Times per Week) | ||||
|---|---|---|---|---|---|---|
| Estimate | p-Value | Estimate | p-Value | Estimate | p-Value | |
| Whole Population | 0.645 | <0.001 | 5.688 | 0.065 | 0.307 | 0.010 |
| Chronic Patients | 0.611 | <0.001 | 11.349 | 0.015 | 0.352 | 0.016 |
| Diabetes | 0.639 | 0.092 | 15.257 | 0.244 | −0.078 | 0.854 |
| Hypertension | 0.727 | 0.004 | 14.148 | 0.039 | 0.629 | 0.007 |
| Heart condition | 1.020 | 0.207 | 24.316 | 0.173 | 0.902 | 0.198 |
| Lung disease | 1.322 | 0.003 | 12.280 | 0.320 | 0.354 | 0.412 |
| Depression | 0.426 | 0.213 | 7.497 | 0.202 | 0.269 | 0.330 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, S.; Chen, Z.; Wu, X. The Impact of Wearable Devices on Physical Activity for Chronic Disease Patients: Findings from the 2019 Health Information National Trends Survey. Int. J. Environ. Res. Public Health 2023, 20, 887. https://doi.org/10.3390/ijerph20010887
Yu S, Chen Z, Wu X. The Impact of Wearable Devices on Physical Activity for Chronic Disease Patients: Findings from the 2019 Health Information National Trends Survey. International Journal of Environmental Research and Public Health. 2023; 20(1):887. https://doi.org/10.3390/ijerph20010887
Chicago/Turabian StyleYu, Shiyuan, Zhifeng Chen, and Xiang Wu. 2023. "The Impact of Wearable Devices on Physical Activity for Chronic Disease Patients: Findings from the 2019 Health Information National Trends Survey" International Journal of Environmental Research and Public Health 20, no. 1: 887. https://doi.org/10.3390/ijerph20010887






