DigiHEALTH: Suite of Digital Solutions for Long-Term Healthy and Active Aging
Abstract
1. Introduction
2. Materials and Methods
2.1. Understand Stakeholder Needs
2.2. Define Main Properties of the Digital Suite for Integration in Wider Digital Ecosystems
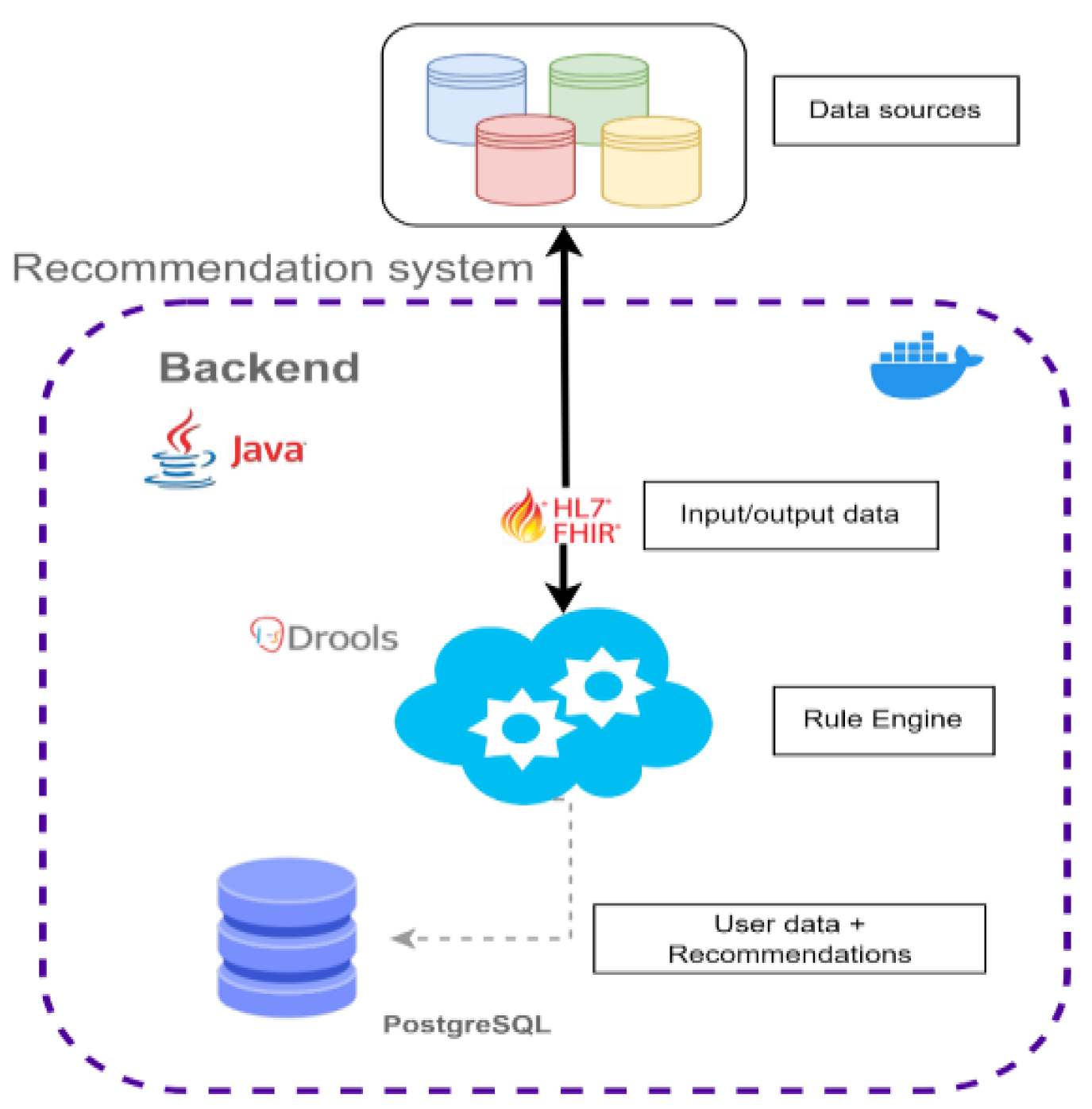
- Adopt standard data models that are aligned with the current necessities of health services. For example, we adopt the Fast Healthcare Interoperability Resources (FHIR) standard that facilitates the exchange of healthcare information in different computing systems regardless of how it is stored. FHIR is a data standard proposed by Health Level 7 (HL7), an organization dedicated to providing a comprehensive framework and related standards for the exchange, integration, sharing, and retrieval of electronic health data (all related information available at http://www.hl7.org/fhir/ (accessed on 1 June 2023)).
- Some specific solutions (especially those focused on alleviating health problems) are aligned with clinical protocols so that their results will articulate similar reasoning processes as traditionally followed by clinical professionals.
- Facilitates the usage of SymbIoTe (symbiosis of smart objects across IoT environments) European project for generating smart networked devices, wearables, sensors, and actuators among various IoT domains (all information available at https://www.symbiote-h2020.eu/ (accessed on 15 June 2023)).
- The digital solutions (DSs) of DigiHEALTH connect with an authentication system based on a single sign-on (SSO) solution for authentication, providing users with a PASETO (Platform-Agnostic Security Tokens) token.
- The different DSs are prepared to be connected with data lakes or other storage layers by RESTful APIs, which would include data curation and aggregation mechanisms as well as the necessary middleware for its integration with different information services.
- Specific tests for the integration of DSs at specific systems have been designed. This allows the traceability of the data towards the conclusions and can be readapted to ad hoc applications for specific services.
- Most of the DSs have been developed using docker technology which facilitates the adaptability and reuse of full or part of the developments. The implementation occurs simultaneously in different parallel environments so that the response to specific requirements from health professionals is fast and scalable at the lowest possible cost.
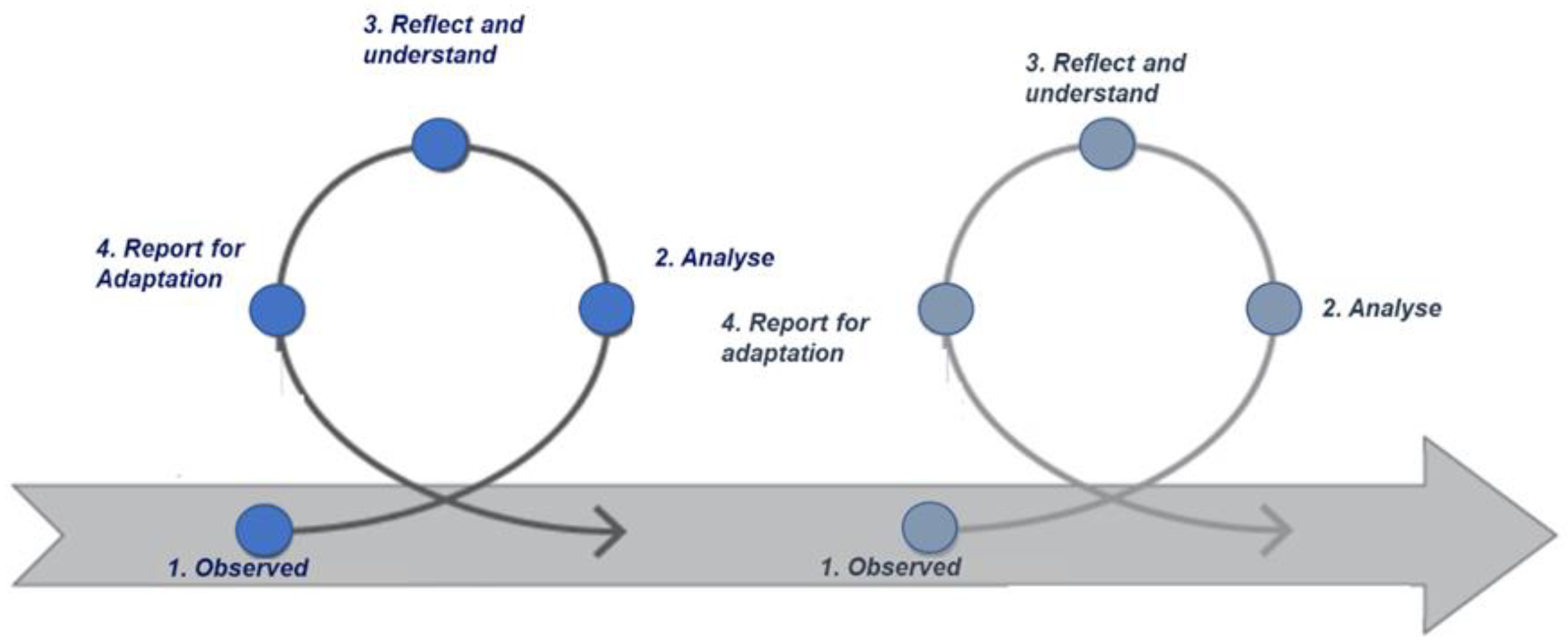
2.3. Codesign of Digital Solutions
- Participation in clusters and networks helps keep the innovative character of the digital suite and understand the main challenges in terms of health promotion, caregiving, etc., but also in terms of interoperability, modularity, standardization, etc. It is also important to share the results with other stakeholders and keep them close to reality.
- Development of projects with direct transferability to an industry that provides the context for the codesign of the solutions, the atmosphere to share the experience of testing, and the methods and tools for the validation of the specific features.
- Collaboration with large consortiums where multiple stakeholders pop up with different interests and necessities. That makes it easier to work with a wide audience of older individuals, test the solutions in different countries that use different languages, and bring forward different cultural assets.
- Peer to peer meetings with professionals of different fields where caregiving to older people is at the center. Indeed, these close spaces provide the atmosphere to share specific details, the experiences of daily caring, the requirements that would make the tools more friendly or attractive, etc.
- Design of validation protocols together with health institutions with real-life cohorts. Indeed, health institutions are crucial stakeholders since they provide the methods for testing and validating the solutions before any of them are put in place.
- Codevelopment spaces where health professionals share common issues of technicians and characteristics of real scenarios. Given certain occasions by innovation projects or in the context of specific actuations or implementations, the communication between health professionals and technicians needs to be fluid.
3. Results
3.1. Digital Solutions for Minimizing Barriers of Digitalization in Older Persons
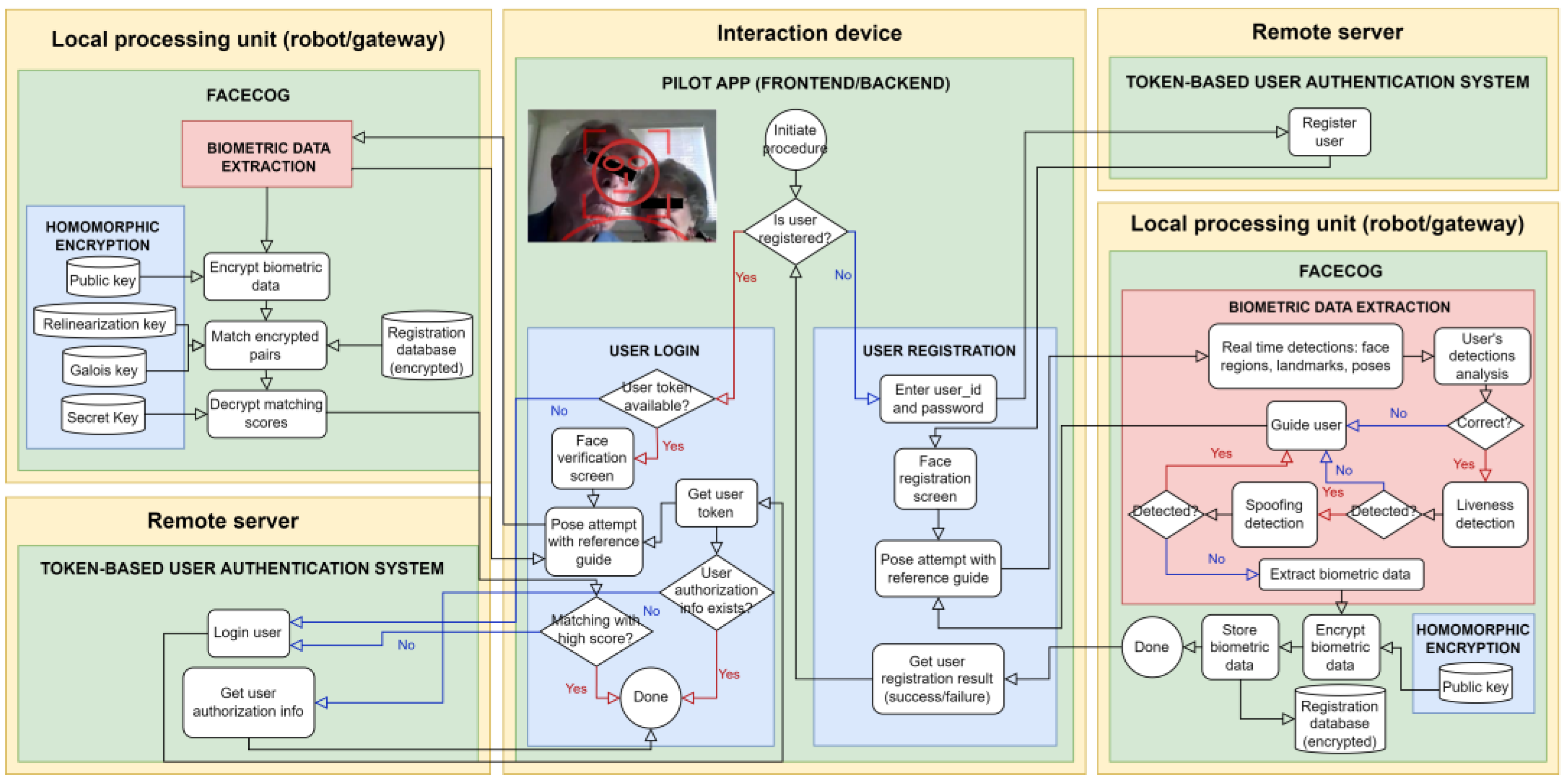
3.1.1. Authentication System for Older Adults—Facecog
- Compatibility: FACECOG is accessible from various devices. This includes ensuring that the technology is compatible with the hardware and software of other devices, as well as ensuring that those have sufficient processing power and memory to run the face recognition algorithms.
- Ease of use: FACECOG provides feedback to obtain correct positioning and tips with clear instructions. It also provides the means to interlink with simple and intuitive interfaces.
- Data privacy and security: FACECOG data privacy and security by guiding end-users on several steps that prevent vulnerable data breaches or identity theft.
3.1.2. Digital Voice Assistant—Adilib
- Agenda: The agenda allows managing the patient’s schedule to keep track of all kinds of events, such as medicine intake or doctor appointments. Caregivers can create and manage calendar events that can then be consulted by the patient at any time (for instance, by saying, “I want to check my medical appointments for today”).
- How-to: the how-to skill guides the patient through a series of—often sequential—processes in order to help them accomplish a task. The caregiver can easily program new tutorials (and even import tutorials from the WikiHow project) that are suitable for the patient, such as “how to make a WhatsApp call” or “how to relax”.
- Questionnaire: This skill allows the caregiver to create and manage questionnaires to be completed by the patients in a conversational way. Caregivers can use the information gathered from customized questionnaires to monitor the patient’s progress and adjust their treatment if needed.
- Reminder: Finally, reminders are a special type of skill that interacts with the agenda, how-to, and questionnaire skills, activating them at a specific date and time defined by the caregiver. Through this skill, patients can be reminded of the events in their calendar, such as medicine intake or medical appointments, or be prompted to perform certain tasks, such as completing daily follow-up questionnaires.
3.2. Digital Solutions for Active and Healthy Aging
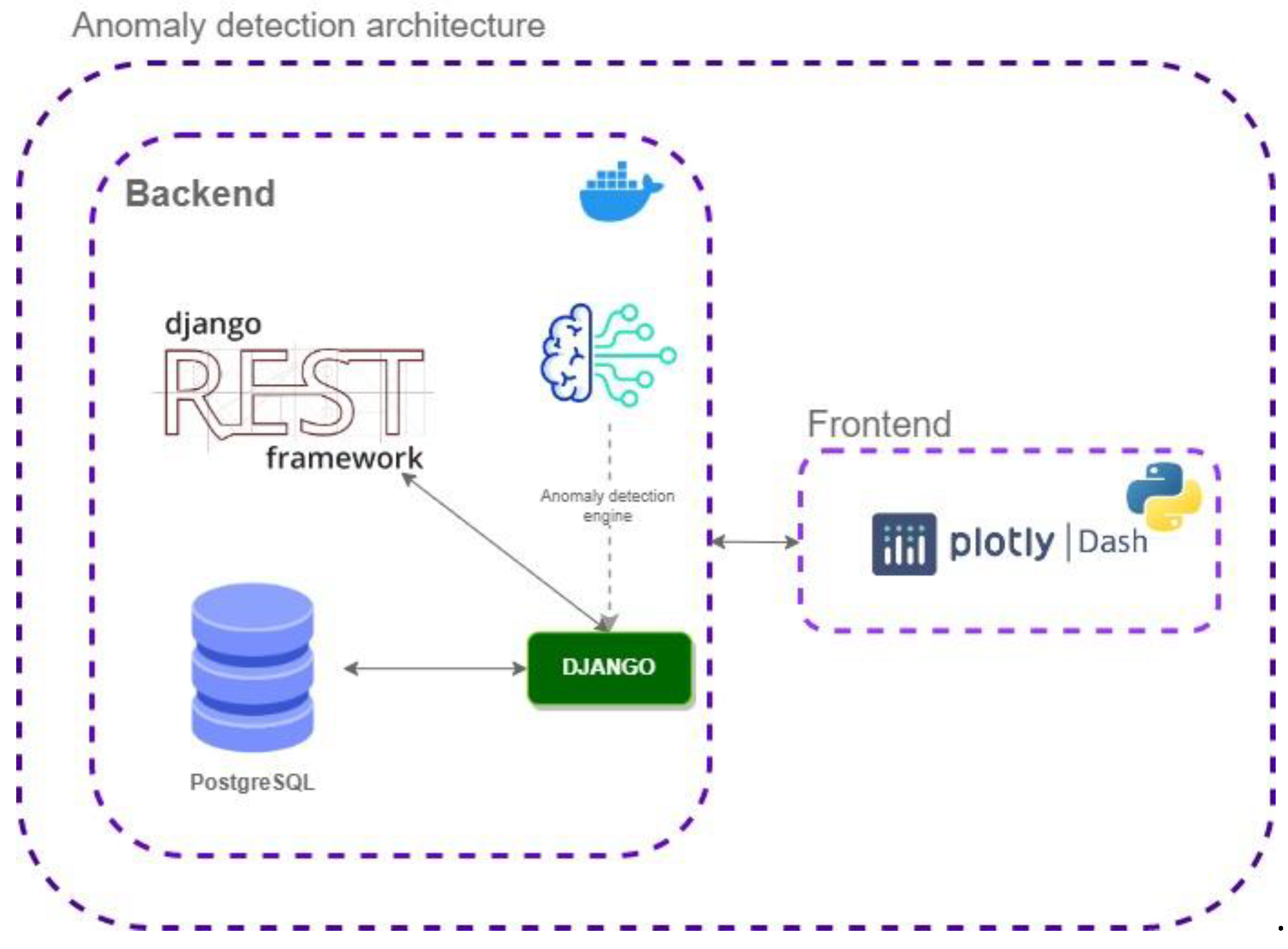
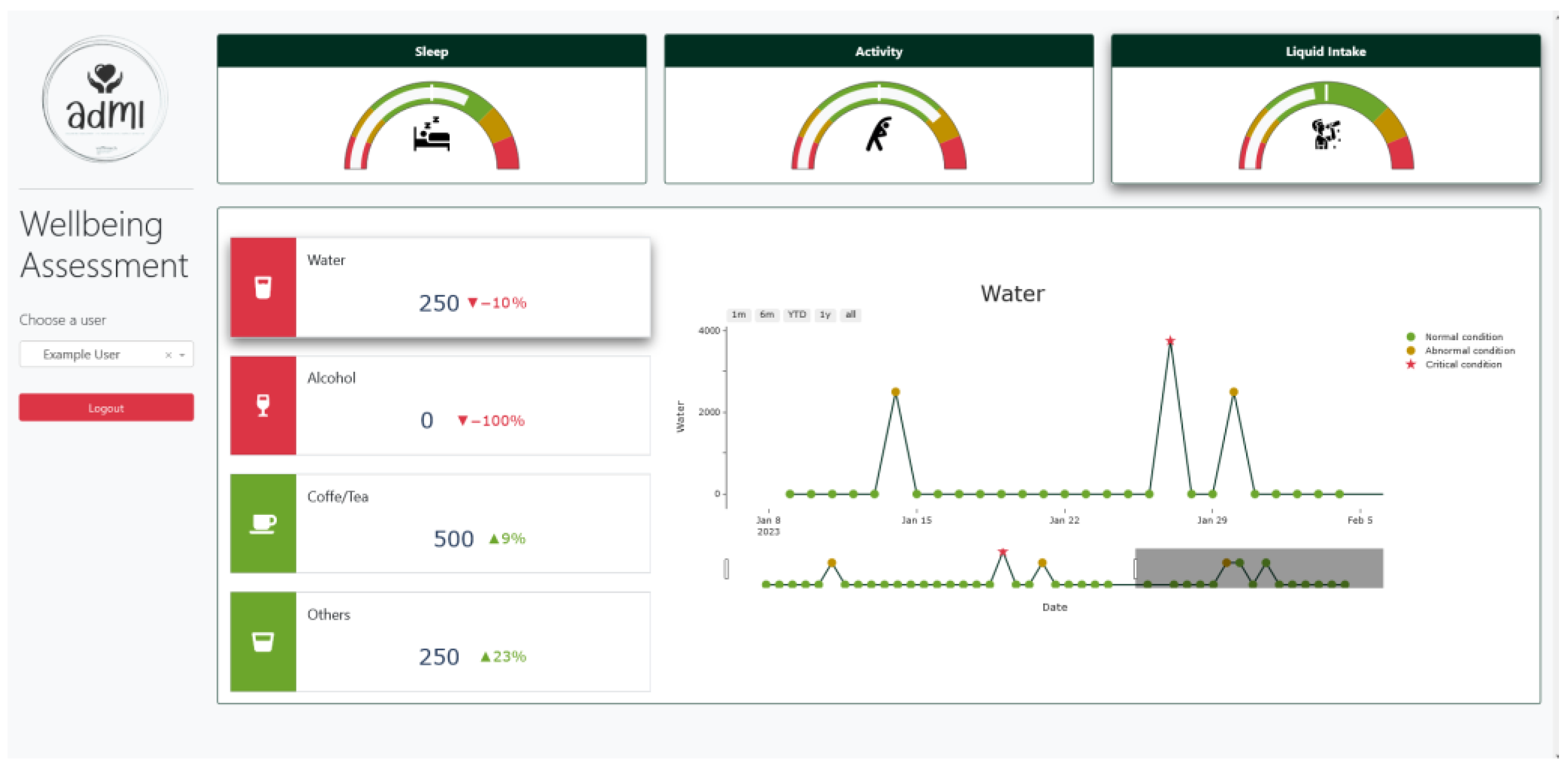
3.2.1. Well-being Assessment
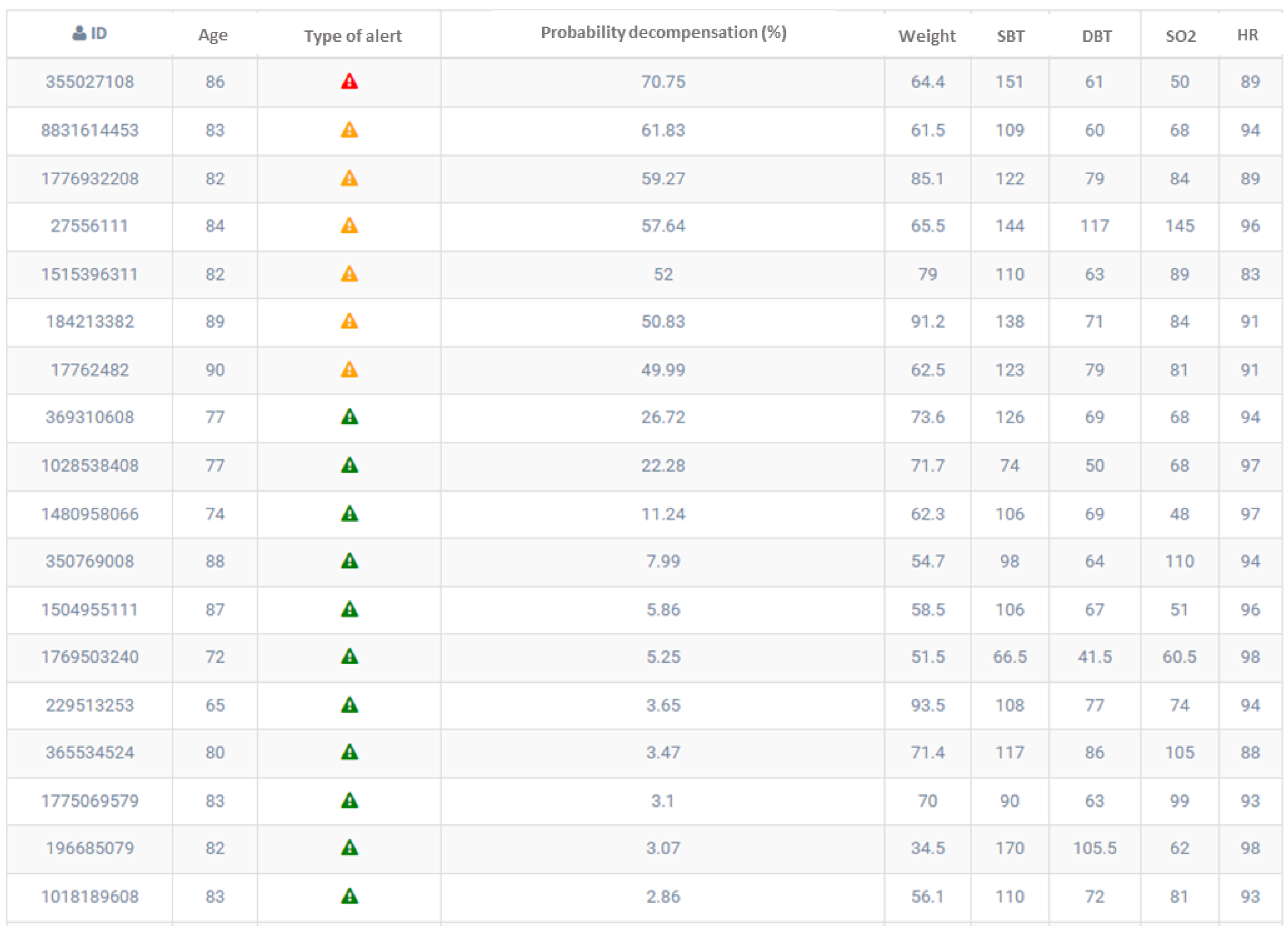
- Giving risk values to each of the individuals to detect health conditions and priorities.
- Creating alerts for low- and high-risk alterations, detecting irregularities, and limiting or preventing their worsening.
- Comparing a detected alteration with other individual’s attributes in time.
- Analyzing and preventing the development of any complications.
- Dashboard for visual analytics that incorporates filters and other features.
- Well-being questionnaires for validating the detected alterations.
- Preprocessing the data making sure that metrics are relevant in relation to well-being assessment.
- Compare daily metrics with data records of previous days and compute z-score.
- Identify abnormal and critical conditions as those that may represent some health-specific conditions or derive from problems.
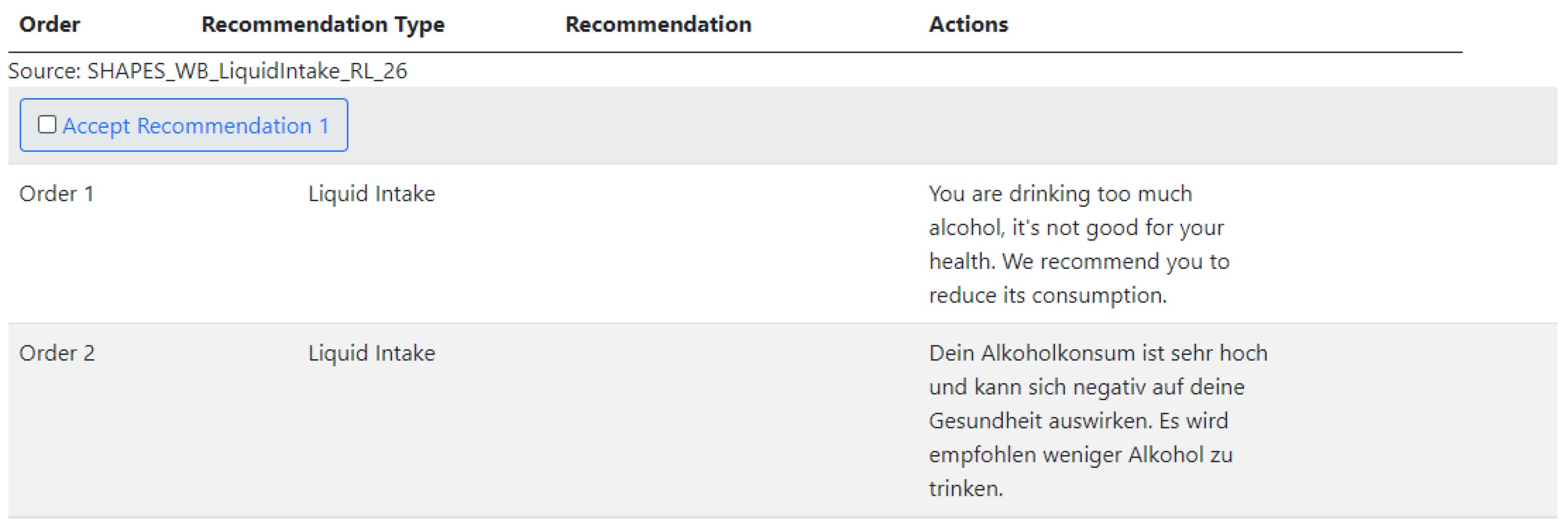
3.2.2. Recommendation System for More Efficient Healthcare
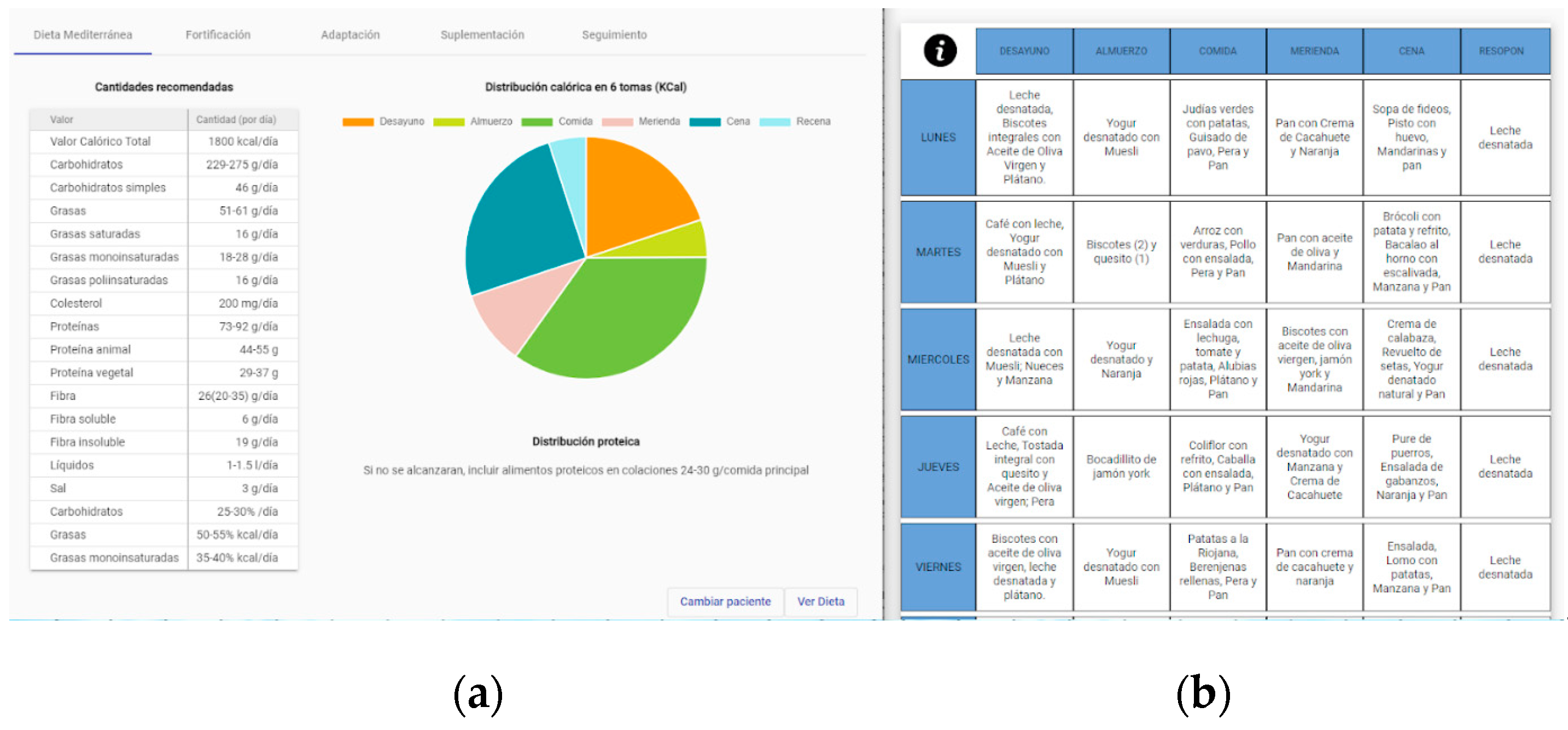
3.2.3. Personalized Nutritional System for Older Adults
Nutritional Recommender System
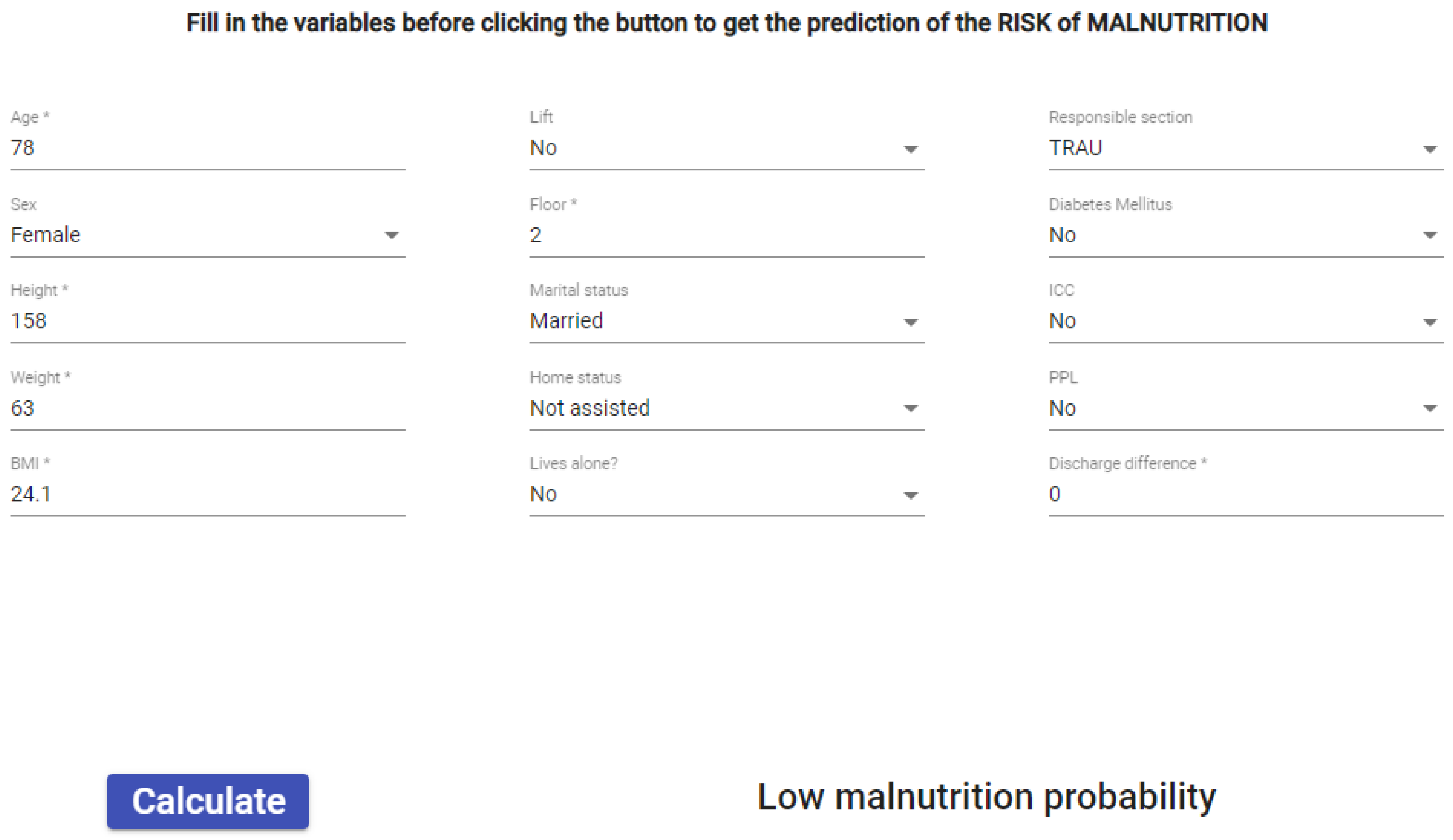
Malnutrition Risk Predictive Model
3.3. Digital Solutions for Specific Impairments
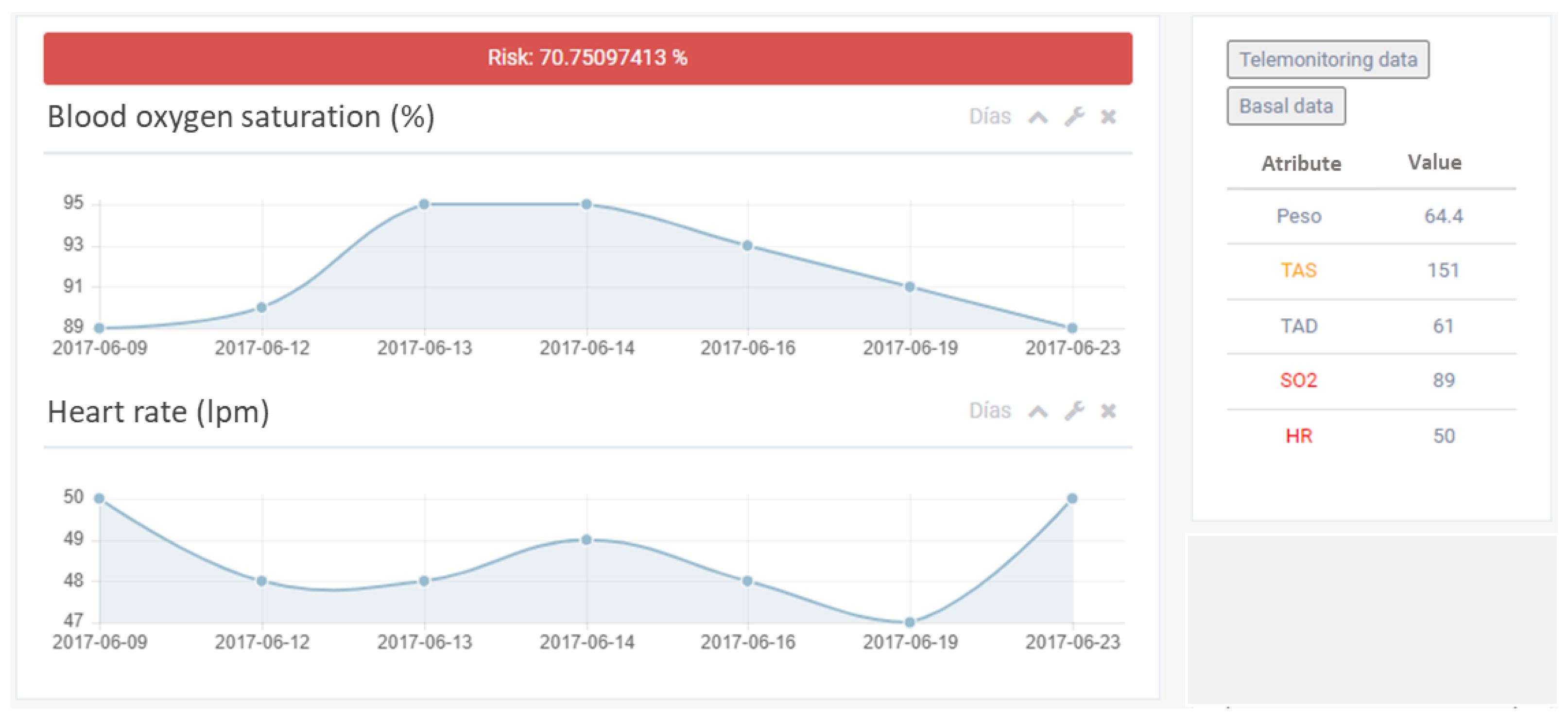
3.3.1. Heart Failure Decompensation Predictive Model
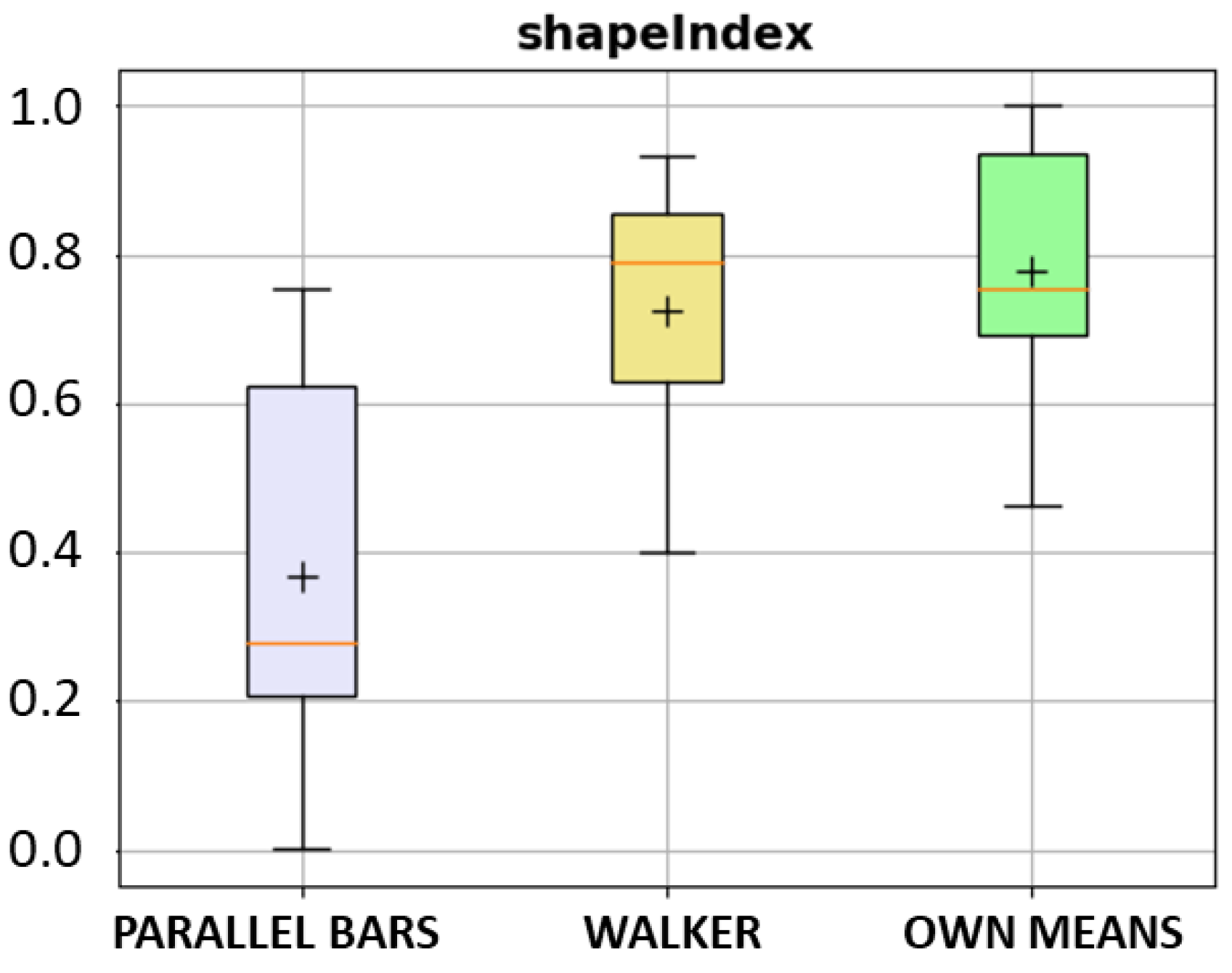
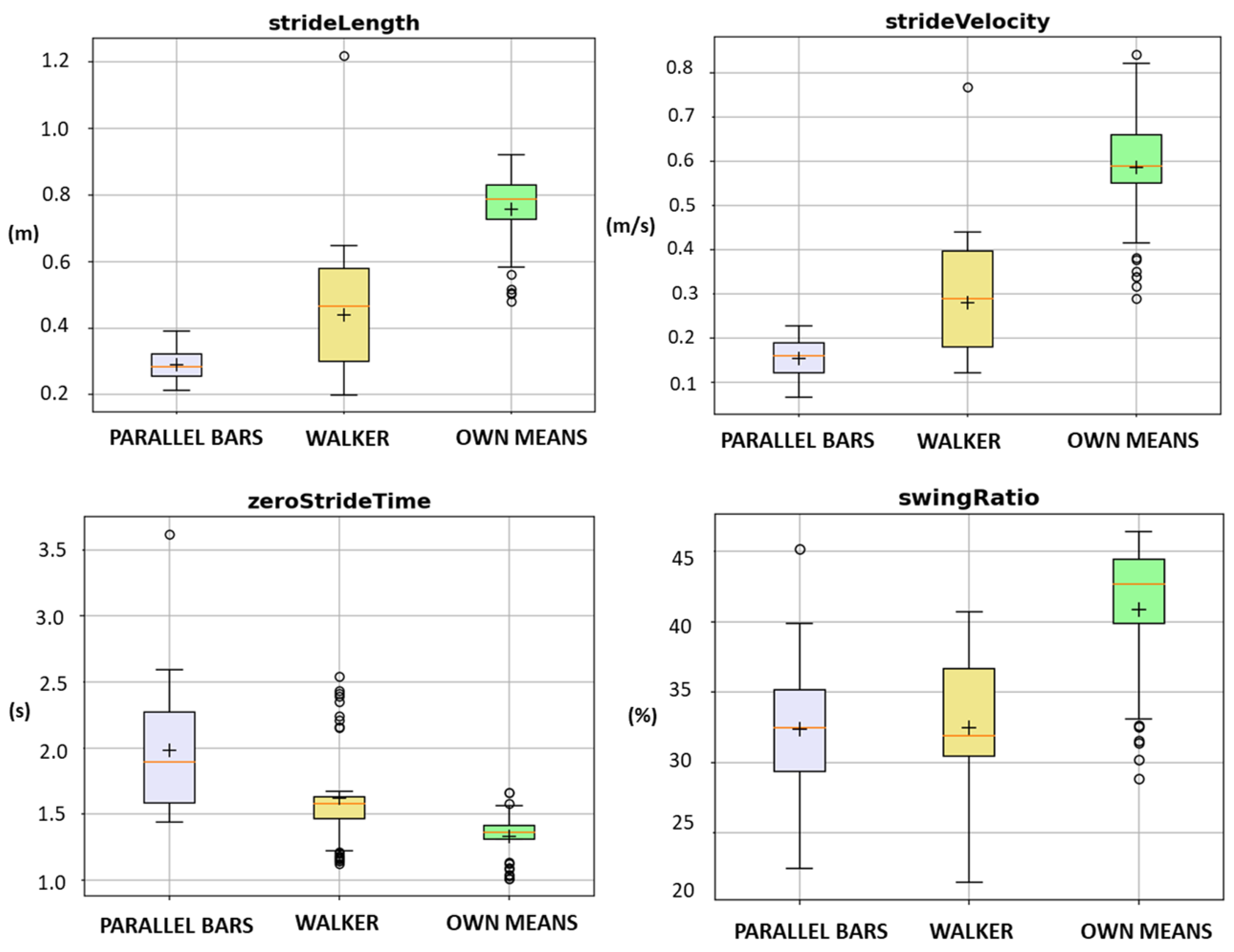
3.3.2. Gait Analysis for Motion Quality Assessment in Older Adults
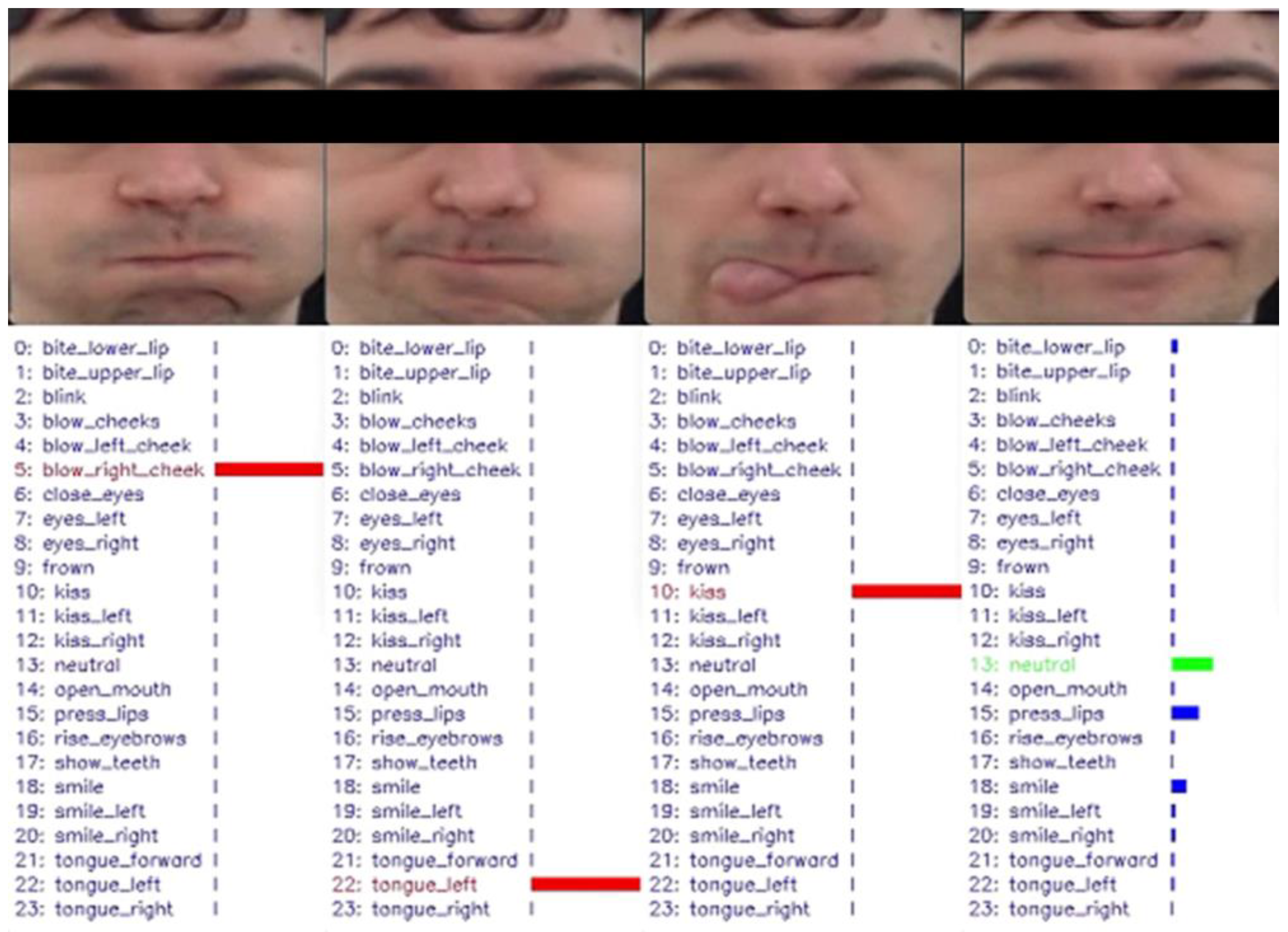
3.3.3. Face Gesture Recognition System for Patients with Degenerative Diseases
- Construct a balanced facial image dataset that includes various facial appearances and features a range of facial gestures commonly used in orofacial rehabilitation, including neutral expressions. This dataset will serve as the reference for measuring the trainee’s progress.
- Develop an effective and efficient facial image processing strategy for frame normalization and motion magnification, particularly for micro gestures.
- Design personalized metrics for evaluating facial gesture accomplishment, taking into account each individual’s neutral expression.
- Analyze the visual distinguishability of the required facial gestures in order to train an effective and efficient facial expression classification model.
4. Conclusions
- -
- Minimize digital barriers for older adults: (1) authentication system based on face recognition and (2) digital voice assistant.
- -
- Facilitate active and healthy living: (3) well-being assessment module, (4) recommendation system, and (5) personalized nutritional system.
- -
- Mitigate specific impairments: (6) heart failure decompensation, (7) mobility assessment and correction, and (8) orofacial gesture trainer.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhao, Y.; Ni, Q.; Zhou, R. What Factors Influence the Mobile Health Service Adoption? A Meta-Analysis and the Moderating Role of Age. Int. J. Inf. Manag. 2018, 43, 342–350. [Google Scholar] [CrossRef]
- Shay, L.A.; Lafata, J.E. Understanding Patient Perceptions of Shared Decision Making. Patient Educ. Couns. 2014, 96, 295–301. [Google Scholar] [CrossRef]
- Kriston, L.; Scholl, I.; Hölzel, L.; Simon, D.; Loh, A.; Härter, M. The 9-Item Shared Decision Making Questionnaire (SDM-Q-9). Development and Psychometric Properties in a Primary Care Sample. Patient Educ. Couns. 2010, 80, 94–99. [Google Scholar] [CrossRef]
- Park, M.; Bui, L.K.; Jeong, M.; Choi, E.J.; Lee, N.; Kwak, M.; Kim, J.; Kim, J.; Jung, J.; Giap, T.-T.; et al. ICT-Based Person-Centered Community Care Platform (IPC3P) to Enhance Shared Decision-Making for Integrated Health and Social Care Services. Int. J. Med. Inform. 2021, 156, 104590. [Google Scholar] [CrossRef] [PubMed]
- Research, Z.M. Global Artificial Intelligence (AI) in Healthcare Market Will Reach USD 17.8 Billion by 2025: Zion Market Research. GlobeNewswire News Room. Available online: https://www.globenewswire.com/news-release/2019/03/25/1759846/0/en/Global-Artificial-Intelligence-AI-in-Healthcare-Market-Will-Reach-USD-17-8-Billion-By-2025-Zion-Market-Research.html (accessed on 27 February 2023).
- Artificial Intelligence in Healthcare Market Growth Report—2032; Global Market Insights Inc.: Selbyville, DE, USA, 2023; Available online: https://www.gminsights.com/industry-analysis/healthcare-artificial-intelligence-market (accessed on 27 February 2023).
- Bellucci, N. Disruptive Innovation and Technological Influences on Healthcare. J. Radiol. Nurs. 2022, 41, 98–101. [Google Scholar] [CrossRef]
- Yadav, R.; Giri, A.; Chatterjee, S. Understanding the Users’ Motivation and Barriers in Adopting Healthcare Apps: A Mixed-Method Approach Using Behavioral Reasoning Theory. Technol. Forecast. Soc. Chang. 2022, 183, 121932. [Google Scholar] [CrossRef]
- Hasnan, S.; Aggarwal, S.; Mohammadi, L.; Koczwara, B. Barriers and Enablers of Uptake and Adherence to Digital Health Interventions in Older Patients with Cancer: A Systematic Review. J. Geriatr. Oncol. 2022, 13, 1084–1091. [Google Scholar] [CrossRef]
- Massaro, M. Digital Transformation in the Healthcare Sector through Blockchain Technology. Insights from Academic Research and Business Developments. Technovation 2023, 120, 102386. [Google Scholar] [CrossRef]
- Du, H.; Shi, H.; Zeng, D.; Zhang, X.-P.; Mei, T. The Elements of End-to-End Deep Face Recognition: A Survey of Recent Advances. ACM Comput. Surv. 2022, 54, 1–42. [Google Scholar] [CrossRef]
- Chaparro, J.D.; Ruiz, J.F.-B.; Romero, M.J.S.; Peño, C.B.; Irurtia, L.U.; Perea, M.G.; Garcia, X.D.T.; Molina, F.J.V.; Grigoleit, S.; Lopez, J.C. The SHAPES Smart Mirror Approach for Independent Living, Healthy and Active Ageing. Sensors 2021, 21, 7938. [Google Scholar] [CrossRef] [PubMed]
- Dodd, C.; Athauda, R.; Adam, M. Designing User Interfaces for the Elderly: A Systematic Literature Review. In Proceedings of the 28th Australasian Conference on Information Systems (ACIS2017), Sydney, Australia, 4–6 December 2017. [Google Scholar]
- Wang, J.J.; Fu, Y.; Lou, V.; Tan, S.Y.; Chui, E. A Systematic Review of Factors Influencing Attitudes towards and Intention to Use the Long-Distance Caregiving Technologies for Older Adults. Int. J. Med. Inform. 2021, 153, 104536. [Google Scholar] [CrossRef] [PubMed]
- Stanley, M.; Cheek, J. Well-being and older people: A review of the literature. Can. J. Occup. Ther. 2003, 70, 51–59. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Programme on Mental Health: WHOQOL User Manual; WHO/HIS/HSI Rev.2012.03; World Health Organization: Geneva, Switzerland, 1998; Available online: https://apps.who.int/iris/handle/10665/77932 (accessed on 27 February 2023).
- Kruger, T.B.; Marty-Dugas, J.; Ralph, B.C.W.; Dixon, M.J.; Smilek, D. The Relation between Self-Reported Healthy Living and Attentional Engagement in Everyday Life. Curr. Res. Behav. Sci. 2023, 4, 100086. [Google Scholar] [CrossRef]
- Torres, J.; Artola, G.; Larburu, N.; Agirre, A.; Narbaiza, E.; Berges, I.; Lizaso, A. Personalized Nutritional Guidance System to Prevent Malnutrition in Pluripathological Older Patients. In Proceedings of the 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health, Online, 23–25 April 2022; SCITEPRESS—Science and Technology: Setúbal, Portugal, 2022; pp. 338–343. [Google Scholar] [CrossRef]
- Amilibia, M.Z.; Cortés, C.; Simonetti, Á.B.; Satrustegi, A.; Iturburu, M.; Reina, I.; Finez, J.; Alonso-Arce, M.; Callejo, P. Preliminary Evaluation of an Objective Assessment Approach from Session Data in Exoskeleton-Assisted Gait Rehabilitation after SCI. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Online, 1–5 November 2021; pp. 6019–6024. [Google Scholar] [CrossRef]
- Cortés, C.; de los Reyes-Guzmán, A.; Scorza, D.; Bertelsen, Á.; Carrasco, E.; Gil-Agudo, Á.; Ruiz-Salguero, O.; Flórez, J. Inverse Kinematics for Upper Limb Compound Movement Estimation in Exoskeleton-Assisted Rehabilitation. BioMed Res. Int. 2016, 2016, e2581924. [Google Scholar] [CrossRef] [PubMed]
- Executive Board 146/26. Data and Innovation: Draft Global Strategy on Digital Health; Report by the Director-General, 23 December 2019; World Health Organization: Geneva, Switzerland, 2019; Available online: https://apps.who.int/gb/ebwha/pdf_files/EB146/B146_26-en.pdf (accessed on 28 January 2021).
- Cosgriff, C.; Ebner, D.; Celi, L. Data sharing in the era of COVID-19. Lancet Digit. Health 2020, 2, E224. [Google Scholar] [CrossRef]
- Gardner, L.; Ratcliff, J.; Dong, E.; Katz, A. A need for open public data standards and sharing in light of COVID-19. Lancet Infect. Dis. 2021, 21, E80. [Google Scholar] [CrossRef]
- Shrivastava, U.; Song, J.; Han, B.T.; Dietzman, D. Do data security measures, privacy regulations, and communication standards impact the interoperability of patient health information? A cross-country investigation. Int. J. Med. Inform. 2021, 148, 104401. [Google Scholar] [CrossRef]
- Benfeldt, O. A comprehensive review of data governance literature. AIS Electronic Library (AISeL). 2017, pp. 120–133. Available online: https://core.ac.uk/download/pdf/301373908.pdf (accessed on 21 June 2023).
- Fontaine, J.; Zheng, K.; Van De Ven, C.; Li, H.; Hiner, J.; Mitchell, K.; Gendler, S.; Hanauer, D.A. Evaluation of a proximity card authentication system for health care settings. Int. J. Med. Inform. 2016, 92, 1–7. [Google Scholar] [CrossRef]
- Horgan, D.; Hackett, J.; Westphalen, C.B.; Kalra, D.; Richer, E.; Romao, M.; Andreu, A.L.; Lal, J.A.; Bernini, C.; Tumiene, B.; et al. Digitalisation and COVID-19: The perfect storm. Biomed. Hub 2020, 5, 43–65. [Google Scholar] [CrossRef]
- Winter, J.S.; Davidson, E.J. Harmonizing Regulatory Spheres to Overcome Challenges for Governance of Patient-Generated Health Data in the Age of Artificial Intelligence and Big Data. In Proceedings of the 48th Research Conference on Communication, Information and Internet Policy, Online, 17–19 February 2021. [Google Scholar] [CrossRef]
- Jagals, M.; Karger, E. Inter-Organizational Data Governance: A Literature Review. In Proceedings of the 29th European Conference on Information Systems (ECIS 2021), Marrakech, Morocco, 14–16 June 2021. [Google Scholar]
- Bezuidenhout, L.; Shanahan, H. Rethinking the A in FAIR data: Issues of data access and accessibility in research. Front. Res. Metr. Anal. 2022, 7, 912456. [Google Scholar] [CrossRef]
- Golubnitschaja, O.; Kinkorova, J.; Costigliola, V. Predictive, preventive and personalized medicine as the hardcore of ‘Horizon 2020’: Epma position paper. EPMA J. 2014, 5, 1–29. [Google Scholar] [CrossRef]
- Maher, M.; Khan, I.; Prikshat, V. Monetisation of digital health data through a GDPR-compliant and blockchain enabled digital health datamarketplace: A proposal to enhance patient’s engagement with health data repositories. Int. J. Inf. Manag. Data Insights 2023, 3, 100159. [Google Scholar] [CrossRef]
- HealthSuite. Available online: https://health-suite.net/acerca-Health-Suite (accessed on 25 April 2023).
- HealthCare. Available online: https://www.philips.es/healthcare/innovation/about-health-suite (accessed on 25 April 2023).
- Healthineers’ Digital Marketplace. Available online: https://www.siemens-healthineers.com/digital-health-solutions/digital-marketplace (accessed on 25 April 2023).
- MyChart-EPIC Health. Available online: https://www.epic.com/software (accessed on 25 April 2023).
- Navify Marketplace. Available online: https://marketplace.roche.com/products (accessed on 25 April 2023).
- IQVIA API Marketplace. Available online: https://www.iqvia.com/solutions/technologies/developer/api-marketplace (accessed on 25 April 2023).
- Bodenheimer, T.; Sinsky, C. From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider. Ann. Fam. Med. 2014, 12, 573–576. [Google Scholar] [CrossRef] [PubMed]
- Värmland County Administrative Board, A Quadruple Helix Guide for Innovations, 2018, Sweden. Available online: https://northsearegion.eu/media/5326/quadruple-helix-guide-version-20180612.pdf (accessed on 21 June 2023).
- Shah, S.W.; Kanhere, S.S. Recent Trends in User Authentication—A Survey. IEEE Access 2019, 7, 112505–112519. [Google Scholar] [CrossRef]
- Elordi, U.; Lunerti, C.; Unzueta, L.; Goenetxea, J.; Aranjuelo, N.; Bertelsen, Á.; Arganda-Carreras, I. Designing Automated Deployment Strategies of Face Recognition Solutions in Heterogeneous IoT Platforms. Information 2021, 12, 532. [Google Scholar] [CrossRef]
- Naresh Boddeti, V. Secure Face Matching Using Fully Homomorphic Encryption. In Proceedings of the 2018 IEEE 9th International Conference on Biometrics Theory, Applications and Systems (BTAS), IEEE, Redondo Beach, CA, USA, 22–25 October 2018; pp. 1–10. [Google Scholar] [CrossRef]
- Papp, D.; Zombor, M.; Buttyán, L. TEE-Based Protection of Cryptographic Keys on Embedded IoT Devices. In Annales Mathematicae et Informaticae AMI; Eszterházy Károly Egyetem Líceum Kiadó: Eger, Hungary, 2021; Volume 53, pp. 245–256. [Google Scholar] [CrossRef]
- Dratsiou, I.; Varella, A.; Romanopoulou, E.; Villacañas, O.; Cooper, S.; Isaris, P.; Serras, M.; Unzueta, L.; Silva, T.; Zurkuhlen, A.; et al. Assistive Technologies for Supporting the Wellbeing of Older Adults. Technologies 2022, 10, 8. [Google Scholar] [CrossRef]
- Cooper, S.; Di Fava, A.; Villacañas, Ó.; Silva, T.; Fernandez-Carbajales, V.; Unzueta, L.; Serras, M.; Marchionni, L.; Ferro, F. Social Robotic Application to Support Active and Healthy Ageing. In Proceedings of the 30th IEEE International Conference on Robot & Human Interactive Communication (RO-MAN), Vancouver, BC, Canada, 8–12 August 2021; pp. 1074–1080. [Google Scholar] [CrossRef]
- Këpuska, V.; Breitfeller, J. Wake-up-Word Speech Recognition Application for First Responder Communication Enhancement. In Sensors, and Command, Control, Communications, and Intelligence (C3I); SPIE: Bellingham, WA, USA, 2006; Volume 6201, p. 62011E. [Google Scholar] [CrossRef]
- Artola, G.; Carrasco, E.; Rebescher, K.M.; Larburu, N.; Berges, I. Behavioral anomaly detection system for the wellbeing assessment and lifestyle support of older people at home. Procedia Comput. Sci. 2021, 192, 2047–2057. [Google Scholar] [CrossRef]
- Torres, J.; Artola, G.; Muro, N. A Domain-Independent Semantically Validated Authoring Tool for Formalizing Clinical Practice Guidelines. Stud. Health Technol. Inform. 2020, 270, 517–521. [Google Scholar] [CrossRef] [PubMed]
- Larburu, N.; Artola, G.; Kerexeta, J.; Caballero, M.; Ollo, B.; Lando, C.M. Key Factors and AI-Based Risk Prediction of Malnutrition in Hospitalized Older Women. Geriatrics 2022, 7, 105. [Google Scholar] [CrossRef]
- Kerexeta, J.; Larburu, N.; Escolar, V.; Lozano-Bahamonde, A.; Macía, I.; Iraola, A.B.; Graña, M. Prediction and Analysis of Heart Failure Decompensation Events Based on Telemonitored Data and Artificial Intelligence Methods. J. Cardiovasc. Dev. Dis. 2023, 10, 48. [Google Scholar] [CrossRef]
- Larburu, N.; Artetxe, A.; Escolar, V.; Lozano, A.; Kerexeta, J. Artificial Intelligence to Prevent Mobile Heart Failure Patients Decompensation in Real Time: Monitoring-Based Predictive Model. Mob. Inf. Syst. 2018, 2018, e1546210. [Google Scholar] [CrossRef]
- Williams, M.; Evans, P.L.; Abu-Serriah, M. Modern Maxillofacial Rehabilitation. In Atlas of Extreme Facial Cancer: Challenges and Solutions; Burton, I., Klaassen, M.F., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 381–420. [Google Scholar] [CrossRef]
- López-Fernández, J.; Unzueta, L.; Garcia, M.; Aguirre, M.; Méndez, A.; del Pozo, A. Knowledge-Driven Dialogue and Visual Perception for Smart Orofacial Rehabilitation. In EAI PervasiveHealth 2022—16th EAI International Conference on Pervasive Computing Technologies for Healthcare, Thessaloniki, Greece, 12–14 December 2022; Springer Nature: Cham, Switzerland, 2022. [Google Scholar]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martin, C.; Amaya, I.; Torres, J.; Artola, G.; García, M.; García-Navarro, T.; De Ramos, V.; Cortés, C.; Kerexeta, J.; Aguirre, M.; et al. DigiHEALTH: Suite of Digital Solutions for Long-Term Healthy and Active Aging. Int. J. Environ. Res. Public Health 2023, 20, 6200. https://doi.org/10.3390/ijerph20136200
Martin C, Amaya I, Torres J, Artola G, García M, García-Navarro T, De Ramos V, Cortés C, Kerexeta J, Aguirre M, et al. DigiHEALTH: Suite of Digital Solutions for Long-Term Healthy and Active Aging. International Journal of Environmental Research and Public Health. 2023; 20(13):6200. https://doi.org/10.3390/ijerph20136200
Chicago/Turabian StyleMartin, Cristina, Isabel Amaya, Jordi Torres, Garazi Artola, Meritxell García, Teresa García-Navarro, Verónica De Ramos, Camilo Cortés, Jon Kerexeta, Maia Aguirre, and et al. 2023. "DigiHEALTH: Suite of Digital Solutions for Long-Term Healthy and Active Aging" International Journal of Environmental Research and Public Health 20, no. 13: 6200. https://doi.org/10.3390/ijerph20136200
APA StyleMartin, C., Amaya, I., Torres, J., Artola, G., García, M., García-Navarro, T., De Ramos, V., Cortés, C., Kerexeta, J., Aguirre, M., Méndez, A., Unzueta, L., Del Pozo, A., Larburu, N., & Macía, I. (2023). DigiHEALTH: Suite of Digital Solutions for Long-Term Healthy and Active Aging. International Journal of Environmental Research and Public Health, 20(13), 6200. https://doi.org/10.3390/ijerph20136200










