The Impact of Meso-Level Factors on SARS-CoV-2 Vaccine Early Hesitancy in the United States
Abstract
:1. Introduction
1.1. Background
1.2. COVID-19 Vaccine Hesitancy
2. Materials and Methods
2.1. The Spatial Model Specification
2.2. Spatial Weight Matrix
2.3. The SARS-CoV-2 Hesitancy Outcome, Covariates Selection, and Data Analysis
2.4. Model Selection
3. Results and Discussion
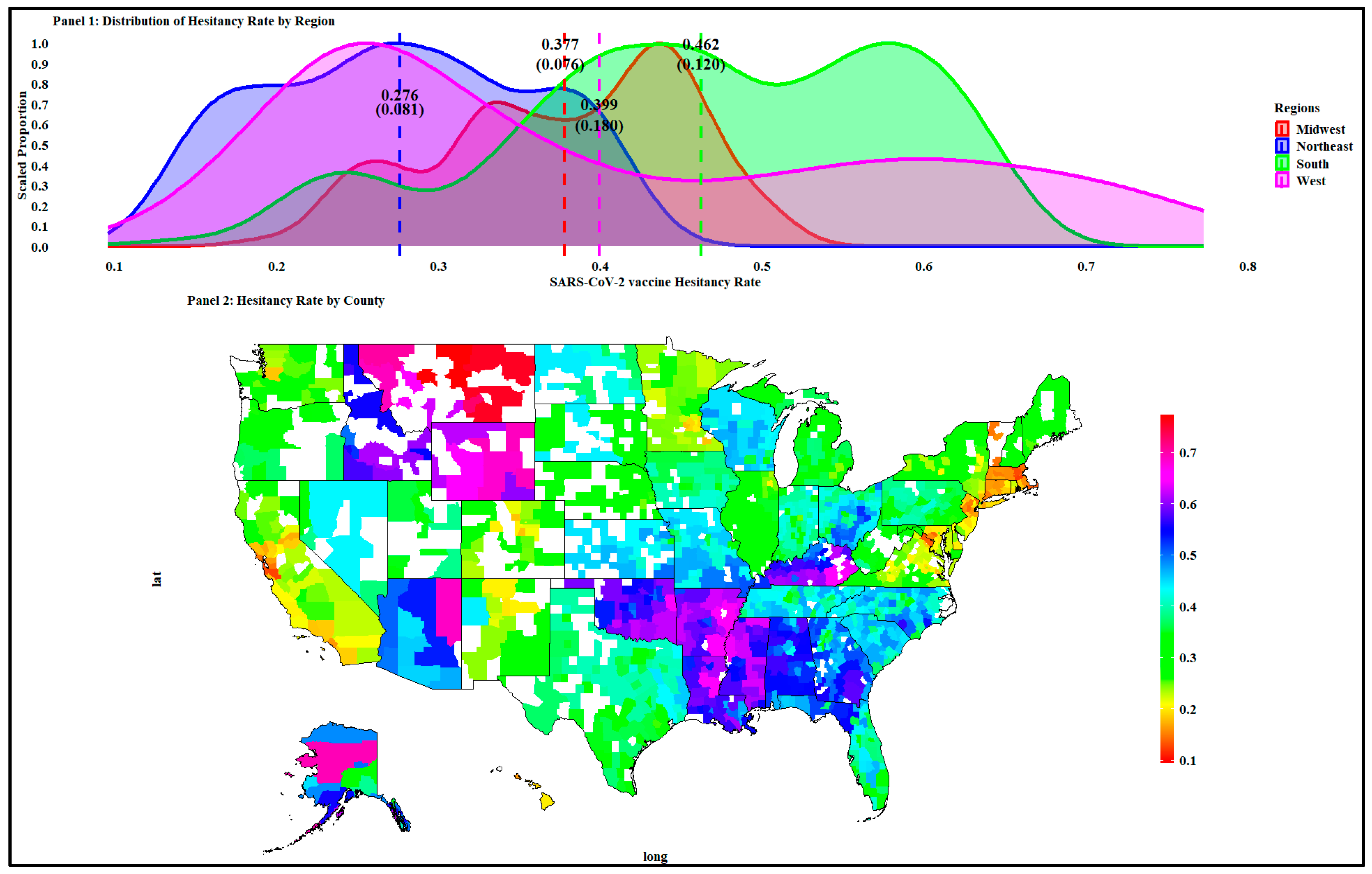
3.1. Descriptive Statistics for the Response and Covariate Variables
3.2. Spatial Regression Results
4. Discussion and Implications
5. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix B
| Variable | Average | Std. Dev. |
|---|---|---|
| Northeast | ||
| Longitude | −75.095 | 2.795 |
| Latitude | 41.825 | 1.429 |
| Population density (people/km2) | 4039.662 | 16,555.057 |
| Metro–urban–rural continuum | ||
| Rural counties (%) | 6.218 | |
| Urban counties (%) | 27.979 | |
| Metropolitan counties (%) | 65.803 | |
| Cook’s political bipartisan index (P.V.I.) | 6.252 | 29.664 |
| Adjusted social vulnerability index (S.V.I.) | 0.390 | 0.213 |
| Socioeconomic status SV subindex | 0.372 | 0.192 |
| Household characteristics S.V. subindex | 0.322 | 0.227 |
| Racial and ethnic minority status S.V. subindex | 0.426 | 0.261 |
| Housing and transportation S.V. subindex | 0.602 | 0.242 |
| Surgo COVID-19 vaccine coverage (C.V.A.C.) index | 0.185 | 0.133 |
| Historic under-vaccination subindex | 0.224 | 0.202 |
| Resource-constrained healthcare system subindex | 0.237 | 0.190 |
| Healthcare accessibility barriers subindex | 0.388 | 0.198 |
| Irregular care-seeking behavior subindex | 0.216 | 0.149 |
| COVID-19 death rate (per 100,000 people) | 184.0 | 83.73 |
| Total adherence rate (per 1000 people) | 418.643 | 110.013 |
| Evangelicals’ rate of adherence | 76.431 | 48.094 |
| Historically black Protestants’ rate of adherence | 9.240 | 10.567 |
| Mainline Protestants’ rate of adherence | 78.446 | 49.346 |
| Catholics’ rate of adherence | 219.085 | 116.490 |
| All other Christian faiths’ rate of adherence | 13.589 | 6.655 |
| All other non-Christian faiths’ rate of adherence | 25.249 | 36.098 |
| Midwest | ||
| Longitude | −91.298 | 5.418 |
| Latitude | 41.618 | 2.840 |
| Population density (people/km2) | 381.487 | 1082.475 |
| Metro–urban–rural continuum | ||
| Rural counties (%) | 33.220 | |
| Urban counties (%) | 33.787 | |
| Metropolitan counties (%) | 32.993 | |
| Cook’s political bipartisan index (P.V.I.) | 34.310 | 23.839 |
| Adjusted social vulnerability index (S.V.I.) | 0.346 | 0.234 |
| Socioeconomic status SV subindex | 0.323 | 0.242 |
| Household characteristics S.V. subindex | 0.397 | 0.251 |
| Racial and ethnic minority status S.V. subindex | 0.322 | 0.218 |
| Housing and transportation S.V. subindex | 0.413 | 0.267 |
| Surgo COVID-19 vaccine coverage (C.V.A.C.) index | 0.356 | 0.245 |
| Historic under-vaccination subindex | 0.442 | 0.331 |
| Resource-constrained healthcare system subindex | 0.464 | 0.260 |
| Healthcare accessibility barriers subindex | 0.355 | 0.250 |
| Irregular care-seeking behavior subindex | 0.370 | 0.218 |
| COVID-19 death rate (per 100,000 people) | 218.0 | 109.90 |
| Total adherence rate (per 1000 people) | 474.859 | 180.632 |
| Evangelicals’ rate of adherence | 182.634 | 105.243 |
| Historically black Protestants’ rate of adherence | 16.569 | 21.989 |
| Mainline Protestants’ rate of adherence | 132.545 | 143.136 |
| Catholics’ rate of adherence | 137.341 | 104.056 |
| All other Christian faiths’ rate of adherence | 14.007 | 11.463 |
| All other non-Christian faiths’ rate of adherence | 3.898 | 11.725 |
| South | ||
| Longitude | −87.404 | 7.084 |
| Latitude | 34.159 | 2.915 |
| Population density (people/km2) | 596.233 | 1749.380 |
| Rural counties (%) | ||
| Urban counties (%) | 24.240 | |
| Metropolitan counties (%) | 32.268 | |
| Cook’s political bipartisan index (P.V.I.) | 32.665 | 32.311 |
| Adjusted social vulnerability index (S.V.I.) | 0.661 | 0.244 |
| Socioeconomic status SV subindex | 0.669 | 0.238 |
| Household characteristics S.V. subindex | 0.621 | 0.261 |
| Racial and ethnic minority status S.V. subindex | 0.631 | 0.262 |
| Housing and transportation S.V. subindex | 0.575 | 0.274 |
| Surgo COVID-19 vaccine coverage (C.V.A.C.) index | 0.655 | 0.262 |
| Historic under-vaccination subindex | 0.533 | 0.236 |
| Resource-constrained healthcare system subindex | 0.618 | 0.267 |
| Healthcare accessibility barriers subindex | 0.673 | 0.241 |
| Irregular care-seeking behavior subindex | 0.574 | 0.289 |
| COVID-19 death rate (per 100,000 people) | 239.30 | 107.10 |
| Total adherence rate (per 1000 people) | 538.668 | 161.926 |
| Evangelicals’ rate of adherence | 332.754 | 154.279 |
| Historically black Protestants’ rate of adherence | 46.782 | 51.486 |
| Mainline Protestants’ rate of adherence | 65.117 | 41.413 |
| Catholics’ rate of adherence | 87.269 | 119.616 |
| All other Christian faiths’ rate of adherence | 18.235 | 17.949 |
| All other non-Christian faiths’ rate of adherence | 4.830 | 13.209 |
| West | ||
| Longitude | −117.605 | 12.811 |
| Latitude | 42.867 | 7.729 |
| Population density (people/km2) | 550.857 | 2763.194 |
| Metro–urban–rural continuum | ||
| Rural counties (%) | 30.519 | |
| Urban counties (%) | 28.896 | |
| Metropolitan counties (%) | 40.584 | |
| Cook’s political bipartisan index (P.V.I.) | 24.439 | 41.899 |
| Adjusted social vulnerability index (S.V.I.) | 0.543 | 0.280 |
| Socioeconomic status SV subindex | 0.724 | 0.600 |
| Household characteristics S.V. subindex | 0.565 | 0.303 |
| Racial and ethnic minority status S.V. subindex | 1.367 | 2.181 |
| Housing and transportation S.V. subindex | 1.301 | 2.187 |
| Surgo COVID-19 vaccine coverage index (C.V.A.C.) | 0.532 | 0.212 |
| Historic under-vaccination subindex | 1.320 | 2.153 |
| Resource-constrained healthcare system subindex | 0.385 | 0.244 |
| Healthcare accessibility barriers subindex | 1.091 | 2.223 |
| Irregular care-seeking behavior subindex | 1.460 | 2.146 |
| COVID-19 death rate (per 100,000 people) | 140.60 | 115.2 |
| Total adherence rate (per 1000 people) | 413.992 | 157.132 |
| Evangelicals’ rate of adherence | 116.273 | 75.213 |
| Historically black Protestants’ rate of adherence | 5.685 | 5.910 |
| Mainline Protestants’ rate of adherence | 28.555 | 34.091 |
| Catholics’ rate of adherence | 150.689 | 126.528 |
| All other Christian faiths’ rate of adherence | 111.258 | 162.952 |
| All other non-Christian faiths’ rate of adherence | 13.203 | 36.166 |
Appendix C


Appendix D
| Spatial Weighting Matrix | Adjusted R Squared | Probability Values |
|---|---|---|
| (maximum distance threshold = 0) | ||
| (binary) | 0.222 | 0.047 |
| 0.690 | 0.047 | |
| 0.690 | 0.047 | |
| 0.342 | 0.047 | |
| 0.272 | 0.047 | |
| 0.261 | 0.047 | |
| 0.245 | 0.047 | |
| 0.683 | 0.047 | |
| 0.839 | 0.047 | |
| 0.880 | 0.047 | |
| 0.900 | 0.047 | |
| 0.904 | 0.047 | |
| (distance threshold: five neighbors (37.61 km)) | ||
| (binary) | 0.115 | 0.047 |
| 0.719 | 0.047 | |
| 0.719 | 0.047 | |
| 0.393 | 0.047 | |
| 0.282 | 0.047 | |
| 0.228 | 0.047 | |
| 0.216 | 0.047 | |
| 0.597 | 0.047 | |
| 0.814 | 0.047 | |
| 0.867 | 0.047 | |
| 0.895 | 0.047 | |
| 0.900 | 0.047 | |
| (distance threshold: 10 neighbors (38.78)) | ||
| (binary) | 0.079 | 0.016 |
| 0.707 | 0.016 | |
| 0.707 | 0.016 | |
| 0.370 | 0.016 | |
| 0.262 | 0.016 | |
| 0.214 | 0.016 | |
| 0.210 | 0.016 | |
| 0.575 | 0.016 | |
| 0.796 | 0.016 | |
| 0.857 | 0.016 | |
| 0.891 | 0.016 | |
| 0.898 | 0.016 |
Appendix E
| Estimated Model | Metrics | |||
|---|---|---|---|---|
| RMSE | AIC | BIC | ||
| 0.59 | 0.08 | −5761 | −5585 | |
| 0.56 | 0.08 | −5560 | −5460 | |
| 0.54 | 0.09 | −5381 | −5280 | |
| 0.63 | 0.08 | −6035 | −5853 | |
| 0.63 | 0.08 | −6050 | −5867 | |
| 0.63 | 0.08 | −6015 | −5832 | |
| 0.63 | 0.08 | −5909 | −5803 | |
| 0.63 | 0.09 | −5903 | −5797 | |
Appendix F
| Variables | Estimate | Lower Interval | Upper Interval | |
|---|---|---|---|---|
| Intercept | 0.583 | 0.426 | 0.752 | *** |
| Metro dummy variable | −0.012 | −0.019 | −0.004 | *** |
| Cook’s bipartisan political index (P.V.I.) | 0.000 | 0.000 | 0.001 | *** |
| Socioeconomic status vulnerability | 0.041 | 0.020 | 0.062 | *** |
| Racial and ethnic minority status vulnerability | 0.010 | −0.014 | 0.034 | |
| Housing and transportation vulnerability | 0.005 | −0.010 | 0.022 | |
| Historic under-vaccination | −0.037 | −0.053 | −0.018 | *** |
| Resource-constrained healthcare system | 0.031 | 0.016 | 0.044 | *** |
| Healthcare accessibility barriers | 0.027 | 0.004 | 0.050 | ** |
| Irregular care-seeking behavior | −0.045 | −0.070 | −0.025 | *** |
| COVID-19 death rate (per 1,000,000 people) | 0.023 | 0.005 | 0.039 | *** |
| Evangelicals’ rate of adherence | 0.004 | 0.001 | 0.007 | *** |
| Black Protestants’ rate of adherence | 0.000 | −0.001 | 0.001 | |
| Catholics’ rate of adherence | 0.000 | 0.000 | 0.000 | |
| All other non-Christian faiths’ rate of adherence | −0.016 | −0.034 | 0.004 | |
| Lag. rural dummy variable | −0.460 | −0.649 | −0.287 | *** |
| Lag. Cook’s bipartisan political index (P.V.I.) | 0.004 | 0.001 | 0.007 | *** |
| Lag. socioeconomic status vulnerability | 0.805 | 0.444 | 1.177 | *** |
| Lag. racial and ethnic minority status | −0.446 | −0.643 | −0.250 | *** |
| Lag. housing and transportation vulnerability | −0.466 | −0.802 | −0.115 | *** |
| Lag. historic under-vaccination | −0.195 | −0.410 | 0.001 | ** |
| Lag. resource-constrained healthcare system | −0.870 | −1.070 | −0.693 | *** |
| Lag. healthcare accessibility barriers | 0.227 | −0.122 | 0.545 | |
| Lag. irregular care-seeking behavior | 0.385 | 0.205 | 0.583 | *** |
| Lag. COVID-19 death rate (per 1000,000 people) | 0.100 | −0.101 | 0.288 | |
| Lag. evangelicals’ rate of adherence | −0.130 | −0.173 | −0.084 | *** |
| Lag. black Protestants’ rate of adherence | 0.057 | 0.038 | 0.075 | *** |
| Lag. mainline Protestants’ rate of adherence | −0.001 | −0.001 | 0.000 | *** |
| Lag. Catholics’ rate of adherence | 0.108 | −0.182 | 0.400 | |
| Spatial autocorrelation coefficient () | 0.993 | 0.958 | 0.999 | *** |
| ML residual variance (sigma) | 0.077 | 0.076 | 0.080 |
References
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Bernal, J.L.; Andrews, N.; Gower, C.; Stowe, J.; Robertson, C.; Tessier, E.; Simmons, R.; Cottrell, S.; Roberts, R.; O’Doherty, M.; et al. Early effectiveness of COVID-19 vaccination with BNT162b2 mRNA vaccine and ChAdOx1 adenovirus vector vaccine on symptomatic disease, hospitalizations and mortality in older adults in England. MedRxiv 2021. [Google Scholar] [CrossRef]
- Harris, R.J.; Hall, J.A.; Zaidi, A.; Andrews, N.J.; Dunbar, J.K.; Dabrera, G. Effect of vaccination on household transmission of SARS-COV-2 in England. N. Engl. J. Med. 2021, 385, 759–760. [Google Scholar] [CrossRef] [PubMed]
- Saban, M.; Myers, V.; Ben Shetrit, S.; Wilf-Miron, R. Issues surrounding incentives and penalties for COVID-19 vaccination: The Israeli experience. Prev. Med. 2021, 153, 106763. [Google Scholar] [CrossRef]
- Sallam, M. COVID-19 vaccine hesitancy worldwide: A concise, systematic review of vaccine acceptance rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Enders, A.M.; Uscinski, J.E.; Klofstad, C.; Stoler, J. The different forms of COVID-19 misinformation and their consequences. Harv. Kennedy Sch. Misinformation Rev. 2020. [Google Scholar] [CrossRef]
- Lee, J.J.; Kang, K.-A.; Wang, M.P.; Zhao, S.Z.; Wong, J.Y.; O’Connor, S.; Yang, S.C.; Shin, S. Associations between COVID-19 misinformation exposure and belief with covid-19 knowledge and preventive behaviors: Cross-sectional online study. J. Med. Internet Res. 2020, 22, e22205. [Google Scholar] [CrossRef]
- Pereira, C.; Medeiros, A.; Bertholini, F. Fear of death and polarization: Political consequences of the COVID-19 pandemic. Rev. Adm. Pública 2020, 54, 952–968. [Google Scholar] [CrossRef]
- Kouzy, R.; Jaoude, J.A.; Kraitem, A.; El Alam, M.B.; Karam, B.; Adib, E.; Zarka, J.; Traboulsi, C.; Akl, E.; Baddour, K. Coronavirus goes viral: Quantifying the COVID-19 misinformation epidemic on Twitter. Cureus 2020, 12, 7255. [Google Scholar] [CrossRef] [Green Version]
- Tasnim, S.; Hossain, M.M.; Mazumder, H. Impact of rumors and misinformation on COVID-19 in social media. J. Prev. Med. Public Health 2020, 53, 171–174. [Google Scholar] [CrossRef] [Green Version]
- Cuello-Garcia, C.; Pérez-Gaxiola, G.; van Amelsvoort, L. Social media can impact how we manage and investigate the COVID-19 pandemic. J. Clin. Epidemiol. 2020, 127, 198–220. [Google Scholar] [CrossRef]
- Islam, M.S.; Sarkar, T.; Khan, S.H.; Mostofa Kamal, A.-H.; Hasan, S.M.; Kabir, A.; Yeasmin, D.; Islam, M.A.; Amin Chowdhury, K.I.; Anwar, K.S.; et al. COVID-19–related infodemic and its impact on public health: A global social media analysis. Am. J. Trop. Med. Hyg. 2020, 103, 1621–1629. [Google Scholar] [CrossRef]
- Sommariva, S.; Vamos, C.; Mantzarlis, A.; Đào, L.U.-L.; Tyson, D.M. Spreading the (fake) news: Exploring health messages on social media and the implications for health professionals using a case study. Am. J. Health Educ. 2018, 49, 246–255. [Google Scholar] [CrossRef]
- Radu, R. COVID-19: Fighting the ‘Infodemic’: Legal Responses to COVID-19 Disinformation. Soc. Media Soc. 2020, 6, 2056305120948190. [Google Scholar] [CrossRef]
- Alvarez-Risco, A.; Mejia, C.R.; Delgado-Zegarra, J.; Del-Aguila-Arcentales, S.; Arce-Esquivel, A.A.; Valladares-Garrido, M.J.; del Portal, M.R.; Villegas, L.F.; Curioso, W.H.; Sekar, M.C.; et al. The Peru approach against the COVID-19 infodemic: Insights and Strategies. Am. J. Trop. Med. Hyg. 2020, 103, 583–586. [Google Scholar] [CrossRef]
- Hua, J.; Shaw, R. Coronavirus (COVID-19) “Infodemic” and emerging issues through a data lens: The case of china. Int. J. Environ. Res. Public Health 2020, 17, 2309. [Google Scholar] [CrossRef] [Green Version]
- Iyer, G.; Soberman, D.; Villas-Boas, J.M. The targeting of advertising. Mark. Sci. 2005, 24, 461–476. [Google Scholar] [CrossRef] [Green Version]
- Subasinghe, A.K.; Nguyen, M.; Wark, J.D.; Tabrizi, S.N.; Garland, S.M. Targeted Facebook advertising is a novel and effective method of recruiting participants into a human papillomavirus vaccine effectiveness study. JMIR Res. Protoc. 2016, 5, e5679. [Google Scholar] [CrossRef]
- Lee, J.; Huang, Y. COVID-19 Vaccine hesitancy: The role of socioeconomic factors and spatial effects. Vaccines 2022, 10, 352. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.-K.; Wei, W.I.; Tang, A.; Wong, S.Y.; Lee, S.S. Influenza vaccine uptake, COVID-19 vaccination intention, and vaccine hesitancy among nurses: A survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef]
- Daly, M.; Robinson, E. Willingness to vaccinate against COVID-19 in the U.S.: Representative longitudinal evidence from April to October 2020. Am. J. Prev. Med. 2021, 60, 766–773. [Google Scholar] [CrossRef] [PubMed]
- Razai, M.S.; Osama, T.; McKechnie, D.G.; Majeed, A. COVID-19 vaccine hesitancy among ethnic minority groups. BMJ 2021, 372, n513. [Google Scholar] [CrossRef] [PubMed]
- Schwarzinger, M.; Watson, V.; Arwidson, P.; Alla, F.; Luchini, S. COVID-19 vaccine hesitancy in a representative working-age population in France: A survey experiment based on vaccine characteristics. Lancet Public Health 2021, 6, 210–221. [Google Scholar] [CrossRef]
- Willis, D.E.; Andersen, J.A.; Bryant-Moore, K.; Selig, J.P.; Long, C.R.; Felix, H.C.; Curran, G.M.; McElfish, P.A. COVID-19 vaccine hesitancy: Race/ethnicity, Trust, and Fear. Clin. Transl. Sci. 2021, 14, 2200–2207. [Google Scholar] [CrossRef] [PubMed]
- Prati, G.; Pietrantoni, L.; Zani, B. Influenza vaccination: The persuasiveness of messages among people aged 65 years and older. Health Commun. 2012, 27, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Quick, B.L.; LaVoie, N.R.; Reynolds-Tylus, T.; Martinez-Gonzalez, A.; Skurka, C. Examining mechanisms underlying fear-control in the extended parallel process model. Health Commun. 2017, 33, 379–391. [Google Scholar] [CrossRef]
- Vorpahl, M.K.M.; Yang, J.Z. Who is to blame? Framing HPV to influence vaccination intentions among college students. Health Commun. 2017, 33, 620–627. [Google Scholar] [CrossRef]
- Mollalo, A.; Tatar, M. Spatial modeling of COVID-19 vaccine hesitancy in the United States. Int. J. Environ. Res. Public Health 2021, 18, 9488. [Google Scholar] [CrossRef]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef]
- Soares, P.; Rocha, J.V.; Moniz, M.; Gama, A.; Laires, P.A.; Pedro, A.R.; Dias, S.; Leite, A.; Nunes, C. Factors associated with COVID-19 vaccine hesitancy. Vaccines 2021, 9, 300. [Google Scholar] [CrossRef]
- Anselin, L. Model selection in spatial econometric models. Spat. Econom. Methods Model. 1988, 4, 243–252. [Google Scholar]
- Anselin, L. Model validation in spatial econometrics: A Review and evaluation of alternative approaches. Int. Reg. Sci. Rev. 1988, 11, 279–316. [Google Scholar] [CrossRef]
- Shobande, O.; Ogbeifun, L. A spatial econometric analysis on the impact of COVID-19 on mortality outcome. Econ. Bus. 2020, 34, 179–200. [Google Scholar] [CrossRef]
- Sawatzky, R.; Kwon, J.-Y.; Barclay, R.; Chauhan, C.; Frank, L.; Hout, W.B.V.D.; Nielsen, L.K.; Nolte, S.; Sprangers, M.A.G.; the Response Shift—In Sync Working Group. Implications of response shift for micro-, meso-, and macro-level healthcare decision-making using results of patient-reported outcome measures. Qual. Life Res. 2021, 30, 3343–3357. [Google Scholar] [CrossRef]
- U.S. Department of Agriculture (U.S.D.A.). Rural-Urban Commuting Area Codes. 2019. Available online: https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/ (accessed on 17 February 2023).
- M.I.T. Election Data and Science Lab. County Presidential Election Returns 2000–2020. Available online: https://electionlab.mit.edu/data (accessed on 17 February 2023).
- Surgo U.S. COVID-19 Vaccine Coverage Index. 2021. Available online: https://vaccine.precisionforcovid.org/ (accessed on 30 January 2023).
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef] [Green Version]
- Sunstein, C.; Altieri, E.; Kim, M.; Carrasco, M.A.; Chadborn, T.; Gauri, V.; George, G.; Gordon, R.; Houéto, D.; Kutalek, R.; et al. Behavioral Considerations for Acceptance and Uptake of COVID-19 Vaccines: WHO Technical Advisory Group on Behavioral Insights and Sciences for Health, Meeting Report, October 15, 2020; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Brewer, N.T.; Hall, M.E.; Malo, T.L.; Gilkey, M.B.; Quinn, B.; Lathren, C. Announcements versus conversations to improve HPV vaccination coverage: A randomized trial. Pediatrics 2017, 139, e20161764. [Google Scholar] [CrossRef] [Green Version]
- Manski, C.F. Identification of endogenous social effects: The reflection problem. Rev. Econ. Stud. 1993, 60, 531–542. [Google Scholar] [CrossRef] [Green Version]
- LeSage, J.P. What regional scientists need to know about spatial econometrics. Rev. Reg. Stud. 2014, 44, 13–32. [Google Scholar]
- Bivand, R.; Hauke, J.; Kossowski, T. Computing the jacobian in gaussian spatial autoregressive models: An illustrated comparison of available methods. Geogr. Anal. 2013, 45, 150–179. [Google Scholar] [CrossRef] [Green Version]
- Tobler, W. Spatial interaction patterns. J. Environ. Syst. 1976, 6, 271–301. [Google Scholar] [CrossRef] [Green Version]
- Burkey, M.L. Spatial econometrics and G.I.S. YouTube Playlist. Region 2018, 5, R13–R18. [Google Scholar] [CrossRef]
- Anselin, L. Some robust approaches to testing and estimation in spatial econometrics. Reg. Sci. Urban Econ. 1990, 20, 141–163. [Google Scholar] [CrossRef]
- Fingleton, B.; Le Gallo, J. Estimating spatial models with endogenous variables, a spatial lag, and spatially dependent disturbances: Finite sample properties. Pap. Reg. Sci. 2008, 87, 319–339. [Google Scholar] [CrossRef]
- Grubesic, T.H.; Rosso, A.L. The use of spatially lagged explanatory variables for modeling neighborhood amenities and mobility in older adults. Cityscape 2014, 16, 205–214. [Google Scholar]
- Gleditsch, K.; Ward, M.D. Spatial Regression Models; Sage Publications Inc.: London, UK, 2008; p. 155. [Google Scholar]
- Lee, H.; Ghosh, S.K. Performance of information criteria for spatial models. J. Stat. Comput. Simul. 2009, 79, 93–106. [Google Scholar] [CrossRef] [Green Version]
- United States Census Bureau. Household Pulse Survey Data Tables Phase 3.2: July 21–October 11. 2021. Available online: https://www.census.gov/programs-surveys/household-pulse-survey/data.html (accessed on 18 February 2023).
- Snyder, B.F.; Parks, V. Spatial variation in socio-ecological vulnerability to COVID-19 in the contiguous United States. Health Place 2020, 66, 10247. [Google Scholar] [CrossRef]
- Fridman, A.; Gershon, R.; Gneezy, A. COVID-19 and vaccine hesitancy: A longitudinal study. PLoS ONE 2021, 16, e0250123. [Google Scholar] [CrossRef]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope, and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Quinn, S.C.; Jamison, A.M.; An, J.; Hancock, G.R.; Freimuth, V.S. Measuring vaccine hesitancy, confidence, trust, and flu vaccine uptake: Results of a national survey of White and African American adults. Vaccine 2019, 37, 1168–1173. [Google Scholar] [CrossRef]
- Wilson, R.J.; Paterson, P.; Jarrett, C.; Larson, H.J. Understanding factors influencing vaccination acceptance during pregnancy globally: A literature review. Vaccine 2015, 33, 6420–6429. [Google Scholar] [CrossRef] [Green Version]
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl. Trop. Dis. 2020, 14, e0008961. [Google Scholar] [CrossRef]
- King, W.C.; Rubinstein, M.; Reinhart, A.; Mejia, R. COVID-19 vaccine hesitancy January-May among 18–64-year-old U.S. adults by employment and occupation. Prev. Med. Rep. 2021, 24, 101569. [Google Scholar] [CrossRef]
- Flanagan, B.E.; Gregory, E.W.; Hallisey, E.J.; Heitgerd, J.L.; Lewis, B. A social vulnerability index for disaster management. J. Homel. Secur. Emerg. Manag. 2011, 8, 0000102202154773551792. [Google Scholar] [CrossRef]
- Kasstan, B. If a rabbi did say you have to vaccinate, we wouldn’t: Unveiling the secular logic of religious exemption and opposition to vaccination. Soc. Sci. Med. 2021, 280, 114052. [Google Scholar] [CrossRef]
- Brewer, N.T.; Chapman, G.B.; Gibbons, F.X.; Gerrard, M.; McCaul, K.D.; Weinstein, N.D. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychol. 2007, 26, 136–145. [Google Scholar] [CrossRef] [Green Version]
- Davila-Payan, C.; Swann, J.; Wortley, P.M. System factors to explain 2009 pandemic H1N1 state vaccination rates for children and high-risk adults in U.S. emergency response to the pandemic. Vaccine 2014, 32, 246–251. [Google Scholar] [CrossRef] [Green Version]
- Garcia, L.L.; Yap, J.F. The role of religiosity in COVID-19 vaccine hesitancy. J. Public Health 2021, 43, e529–e530. [Google Scholar] [CrossRef]
- Grabenstein, J.D. What the World’s religions teach, applied to vaccines and immune globulins. Vaccine 2013, 31, 2011–2023. [Google Scholar] [CrossRef]
- Karwowski, M.; Kowal, M.; Groyecka, A.; Białek, M.; Lebuda, I.; Sorokowska, A.; Sorokowski, P. When in danger, turn right: Does the COVID-19 threat promote social conservatism and right-wing presidential candidates? Hum. Ethol. 2020, 35, 37–48. [Google Scholar] [CrossRef]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef]
- Murthy, B.P.; Sterrett, N.; Weller, D.; Zell, E.; Reynolds, L.; Toblin, R.L.; Murthy, N.; Kriss, J.; Rose, C.; Cadwell, B.; et al. Disparities in COVID-19 vaccination coverage between urban and rural counties In the U.S. Morb. Mortal. Wkly. Rep. 2021, 70, 759. [Google Scholar] [CrossRef] [PubMed]
- Ruijs, W.L.M.; Hautvast, J.L.A.; Kerrar, S.; van der Velden, K.; Hulscher, M.E.J.L. The role of religious leaders in promoting vaccination acceptance within a minority group: A qualitative study. B.M.C. Public Health 2013, 13, 511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rutjens, B.T.; Sutton, R.M.; van der Lee, R. Not all skepticism is equal: Exploring the ideological antecedents of science acceptance and rejection. Personal. Soc. Psychol. Bull. 2017, 44, 384–405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elhorst, J.P. Applied Spatial Econometrics: Raising the bar. Spat. Econ. Anal. 2010, 5, 9–28. [Google Scholar] [CrossRef]
- Bauman, D.; Drouet, T.; Fortin, M.-J.; Dray, S. Optimizing the choice of a spatial weighting matrix in eigenvector-based methods. Ecology 2018, 99, 2159–2166. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022; Available online: https://www.R-project.org/ (accessed on 18 February 2023).
- Wickham, H.; Averick, M.; Bryan, J.; Chang, W.; McGowan, L.D.; François, R.; Grolemund, G.; Hayes, A.; Henry, L.; Hester, J.; et al. Welcome to the tidyverse. J. Open-Source Softw. 2019, 4, 1686. [Google Scholar] [CrossRef] [Green Version]
- Dray, S.; Bauman, D.; Blanchet, G.; Borcard, D.; Clappe, S.; Guénard, G.; Jombart, T.; Larocque, G.; Legendre, P.; Madi, N.; et al. Adespatial: Multivariate Multiscale Spatial Analysis. R package version 0.3-20. 2022. Available online: https://CRAN.R-project.org/package=adespatial (accessed on 18 February 2023).
- Bivand, R.S.; Wong, D.W.S. Comparing implementations of global and local indicators of spatial association. Test 2018, 27, 716–748. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Wyka, K.; White, T.M.; Picchio, C.A.; Rabin, K.; Ratzan, S.C.; Parsons Leigh, J.; Hu, J.; El-Mohandes, A. Revisiting COVID-19 vaccine hesitancy around the World using data from 23 countries in 2021. Nat. Commun. 2022, 13, 3801. [Google Scholar] [CrossRef]
- Lin, C.; Tu, P.; Beitsch, L.M. Confidence and receptivity for COVID-19 vaccines: A rapid systematic review. Vaccines 2020, 9, 16. [Google Scholar] [CrossRef]
- Ingram, D.D.; Franco, S.J. NCHSurban–Rural Classification Scheme for Counties. Vital Health Stat 2 2012, 154, 1–65. [Google Scholar]
- Public Religion Research Institute. The 2020 Census of American Religion. Available online: https://www.prri.org/research/2020-census-of-american-religion/#page-section-0 (accessed on 18 February 2023).
- Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry/Geospatial Research, Analysis, and Services Program. CDC/ATSDR Social Vulnerability Index2020 Database U.S. Available online: https://www.atsdr.cdc.gov/placeandhealth/svi/ (accessed on 17 February 2023).
- Surgo Ventures. The US COVID-19 Vaccine Coverage Index (C.V.A.C.) Methodology, Version 1. 2021. Available online: http://precisionforcovid.org/cvac (accessed on 17 February 2023).
- Yasmin, F.; Najeeb, H.; Moeed, A.; Naeem, U.; Asghar, M.S.; Chughtai, N.U.; Yousaf, Z.; Seboka, B.T.; Ullah, I.; Lin, C.-Y.; et al. COVID-19 vaccine hesitancy in the United States: A systematic review. Front. Public Health 2021, 9, 770985. [Google Scholar] [CrossRef]
- Alcendor, D.J. Targeting COVID vaccine hesitancy in rural communities in Tennessee: Implications for extending the COVID-19 pandemic in the South. Vaccines 2021, 9, 1279. [Google Scholar] [CrossRef]
- Gopez, J.M.W. Building public trust in COVID-19 vaccines through the Catholic Church in the Philippines. J. Public Health 2021, 43, e330–e331. [Google Scholar] [CrossRef]
- Nagar, S.; Ashaye, T. A shot of faith—Analyzing vaccine hesitancy in certain religious communities in the United States. Am. J. Health Promot. 2022, 36, 765–767. [Google Scholar] [CrossRef]
- Mirpuri, P.; Rovin, R.A. COVID-19 and Historic Influenza Vaccinations in the United States: A Comparative Analysis. Vaccines 2021, 9, 1284. [Google Scholar] [CrossRef]
- Oyekale, A.S. Effect of Health Insurance Uptake on Hesitancy toward COVID-19 Vaccines in Nigeria: A Recursive Bivariate Probit and Decomposition Estimation. Int. J. Environ. Res. Public Health 2023, 20, 2566. [Google Scholar] [CrossRef]
- McFadden, S.M.; Demeke, J.; Dada, D.; Wilton, L.; Wang, M.; Vlahov, D.; Nelson, L.E. Confidence and hesitancy during the early rollout of COVID-19 vaccines among black, Hispanic, and undocumented immigrant communities: A review. J. Urban Health 2022, 99, 3–14. [Google Scholar] [CrossRef]
- Bhochhibhoya, A.; Branscum, P.; Thapaliya, R.; Ghimire, P.S.; Wharton, H. Applying the health belief model for investigating the impact of political affiliation on COVID-19 vaccine uptake. Am. J. Health Educ. 2021, 52, 241–250. [Google Scholar] [CrossRef]
- Nayak, A.; Islam, S.J.; Mehta, A.; Ko, Y.A.; Patel, S.A.; Goyal, A.; Sullivan, S.; Lewis, T.T.; Vaccarino, V.; Morris, A.A.; et al. Impact of social vulnerability on COVID-19 incidence and outcomes in the United States. MedRxiv 2020. [Google Scholar]
- Gatwood, J.; McKnight, M.; Fiscus, M.; Hohmeier, K.C.; Chisholm-Burns, M. Factors influencing the likelihood of COVID-19 vaccination: A survey of Tennessee adults. Am. J. Health-Syst. 2021, 78, 879–889. [Google Scholar] [CrossRef]
- Njoku, A.; Joseph, M.; Felix, R. Changing the narrative: Structural barriers and racial and ethnic inequities in COVID-19 vaccination. Int. J. Environ. Res. Public Health 2021, 18, 9904. [Google Scholar] [CrossRef] [PubMed]


| Type of Comparison | Hypothesis | Test Statistic | Adjusted p-Value |
|---|---|---|---|
| One-way analysis of variance | Equal mean | F value | Pr(>F) |
| Regions ( | 0.4125 | 213.8 | <0.001 *** |
| Levene’s test for homogeneity of variance | Equal variance | F value | Pr(>F) |
| Regions ( | 0.1268 | 135 | <0.001 *** |
| Tukey multiple comparisons of means | Mean difference | t value | Pr(>|t|) |
| Midwest–Northeast | 0.10158 | 11.16 | <0.001 *** |
| South–Northeast | 0.18620 | 21.05 | <0.001 *** |
| West–Northeast | 0.11702 | 11.15 | <0.001 *** |
| South–Midwest | 0.08462 | 16.89 | <0.001 *** |
| West–Midwest | 0.01544 | 2.05 | 0.16 |
| West–South | −0.06919 | −9.57 | <0.001 *** |
| Variable | Average | Std. Dev. |
|---|---|---|
| Longitude | −91.33 | 12.675 |
| Latitude | 38.195 | 5.391 |
| Population density (number/km2) | 769.226 | 483.00 |
| Metro-urban-rural continuum | ||
| Metropolitan counties (%) | 41.3 | |
| Urban counties (%) | 32.07 | |
| Rural counties (%) | 26.63 | |
| Cook’s bipartisan political index (PVI) | 30.338 | 31.792 |
| Adjusted social vulnerability index (SVI) | 0.524 | 0.283 |
| Socioeconomic status vulnerability subindex | 0.54 | 0.347 |
| Household characteristics vulnerability subindex | 0.519 | 0.285 |
| Racial and ethnic minority status vulnerability subindex | 0.6 | 0.84 |
| Housing and transportation vulnerability subindex | 0.608 | 0.831 |
| Surgo COVID-19 vaccine coverage index (CVAC) | 0.508 | 0.291 |
| Historic under-vaccination subindex | 0.573 | 0.829 |
| Resource-constrained healthcare system subindex | 0.512 | 0.282 |
| Healthcare accessibility barriers subindex | 0.596 | 0.825 |
| Irregular care-seeking behavior subindex | 0.584 | 0.842 |
| COVID-19 death rate (per 100,000 people) | 217.052 | 111.947 |
| Total adherence rate (per 1000 people) | 494.435 | 171.3149 |
| Evangelicals’ rate of adherence | 239.684 | 157.721 |
| Historically black Protestants’ rate of adherence | 34.787 | 45.827 |
| Mainline Protestants’ rate of adherence | 84.512 | 96.154 |
| Catholics’ rate of adherence | 122.166 | 121.182 |
| All other Christian faiths’ rate of adherence | 27.727 | 65.994 |
| All other non-Christian faiths’ rate of adherence | 6.97 | 20.206 |
| Variable | Estimate | Lower Interval | Upper Interval | |
|---|---|---|---|---|
| Direct | ||||
| Irregular care-seeking behavior | −0.0404 | −0.0618 | −0.0191 | *** |
| Historic under-vaccination | −0.0395 | −0.0556 | −0.0234 | *** |
| Metro dummy variable | −0.0185 | −0.0260 | −0.0109 | *** |
| All other non-Christian faiths’ rate of adherence | −0.0140 | −0.0334 | 0.0055 | |
| Housing and transportation vulnerability | −0.0013 | −0.0181 | 0.0155 | |
| Catholics’ rate of adherence | −0.0001 | −0.0001 | 0.0000 | *** |
| Cook’s bipartisan political index (P.V.I.) | 0.0004 | 0.0002 | 0.0006 | *** |
| Black Protestants’ rate of adherence | 0.0011 | −0.0001 | 0.0023 | * |
| Evangelicals’ rate of adherence | 0.0025 | −0.0005 | 0.0054 | |
| Racial and ethnic minority status vulnerability | 0.0038 | −0.0199 | 0.0274 | |
| Resource-constrained healthcare system | 0.0186 | 0.0032 | 0.0339 | ** |
| COVID-19 death rate (per 1,000,000 people) | 0.0249 | 0.0079 | 0.0419 | *** |
| Healthcare accessibility barriers | 0.0303 | 0.0086 | 0.0520 | *** |
| Socioeconomic status vulnerability | 0.0529 | 0.0325 | 0.0733 | *** |
| Indirect | ||||
| Resource-constrained healthcare system | −20.1111 | −27.8318 | −12.3905 | *** |
| Metro dummy variable | −11.2352 | −16.7978 | −5.6726 | *** |
| Housing and transportation vulnerability | −10.8746 | −20.2472 | −1.5021 | ** |
| Racial and ethnic minority status vulnerability | −10.4776 | −16.3187 | −4.6365 | *** |
| Historic under-vaccination | −5.5636 | −10.8990 | −0.2282 | ** |
| Evangelicals’ rate of adherence | −3.0024 | −4.5244 | −1.4804 | *** |
| Catholics’ rate of adherence | −0.0227 | −0.0374 | −0.0080 | *** |
| Cook’s bipartisan political index (P.V.I.) | 0.1118 | 0.0308 | 0.1928 | *** |
| Black Protestants’ rate of adherence | 1.3705 | 0.7354 | 2.0057 | *** |
| All other non-Christian faiths’ rate of adherence | 2.2432 | −4.8355 | 9.3220 | |
| COVID-19 death rate (per 1,000,000 people) | 2.8096 | −2.4472 | 8.0664 | |
| Healthcare accessibility barriers | 6.0689 | −2.4014 | 14.5393 | |
| Irregular care-seeking behavior | 8.3187 | 3.1648 | 13.4726 | *** |
| Socioeconomic status vulnerability | 20.0416 | 8.2052 | 31.8779 | *** |
| Total | ||||
| Resource-constrained healthcare system | −20.0926 | −27.8134 | −12.3717 | *** |
| Metro dummy variable | −11.2537 | −16.8182 | −5.6892 | *** |
| Housing and transportation vulnerability | −10.8759 | −20.2493 | −1.5025 | ** |
| Racial and ethnic minority status vulnerability | −10.4739 | −16.3089 | −4.6388 | *** |
| Historic under-vaccination | −5.6031 | −10.9311 | −0.2750 | ** |
| Evangelicals’ rate of adherence | −2.9999 | −4.5221 | −1.4778 | *** |
| Catholics’ rate of adherence | −0.0227 | −0.0374 | −0.0081 | *** |
| Cook’s bipartisan political index (P.V.I.) | 0.1122 | 0.0312 | 0.1932 | *** |
| Black Protestants’ rate of adherence | 1.3716 | 0.7362 | 2.0070 | *** |
| All other non-Christian faiths’ rate of adherence | 2.2293 | −4.8477 | 9.3062 | |
| COVID-19 death rate (per 1,000,000 people) | 2.8345 | −2.4210 | 8.0900 | |
| Healthcare accessibility barriers | 6.0993 | −2.3699 | 14.5685 | |
| Irregular care-seeking behavior | 8.2782 | 3.1311 | 13.4254 | *** |
| Socioeconomic status vulnerability | 20.0945 | 8.2558 | 31.9331 | *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaliba, A.R.; Andrews, D.R. The Impact of Meso-Level Factors on SARS-CoV-2 Vaccine Early Hesitancy in the United States. Int. J. Environ. Res. Public Health 2023, 20, 6313. https://doi.org/10.3390/ijerph20136313
Kaliba AR, Andrews DR. The Impact of Meso-Level Factors on SARS-CoV-2 Vaccine Early Hesitancy in the United States. International Journal of Environmental Research and Public Health. 2023; 20(13):6313. https://doi.org/10.3390/ijerph20136313
Chicago/Turabian StyleKaliba, Aloyce R., and Donald R. Andrews. 2023. "The Impact of Meso-Level Factors on SARS-CoV-2 Vaccine Early Hesitancy in the United States" International Journal of Environmental Research and Public Health 20, no. 13: 6313. https://doi.org/10.3390/ijerph20136313









