Epidemiological Determinants of Patient Non-Conveyance to the Hospital in an Emergency Medical Service Environment
Abstract
1. Introduction
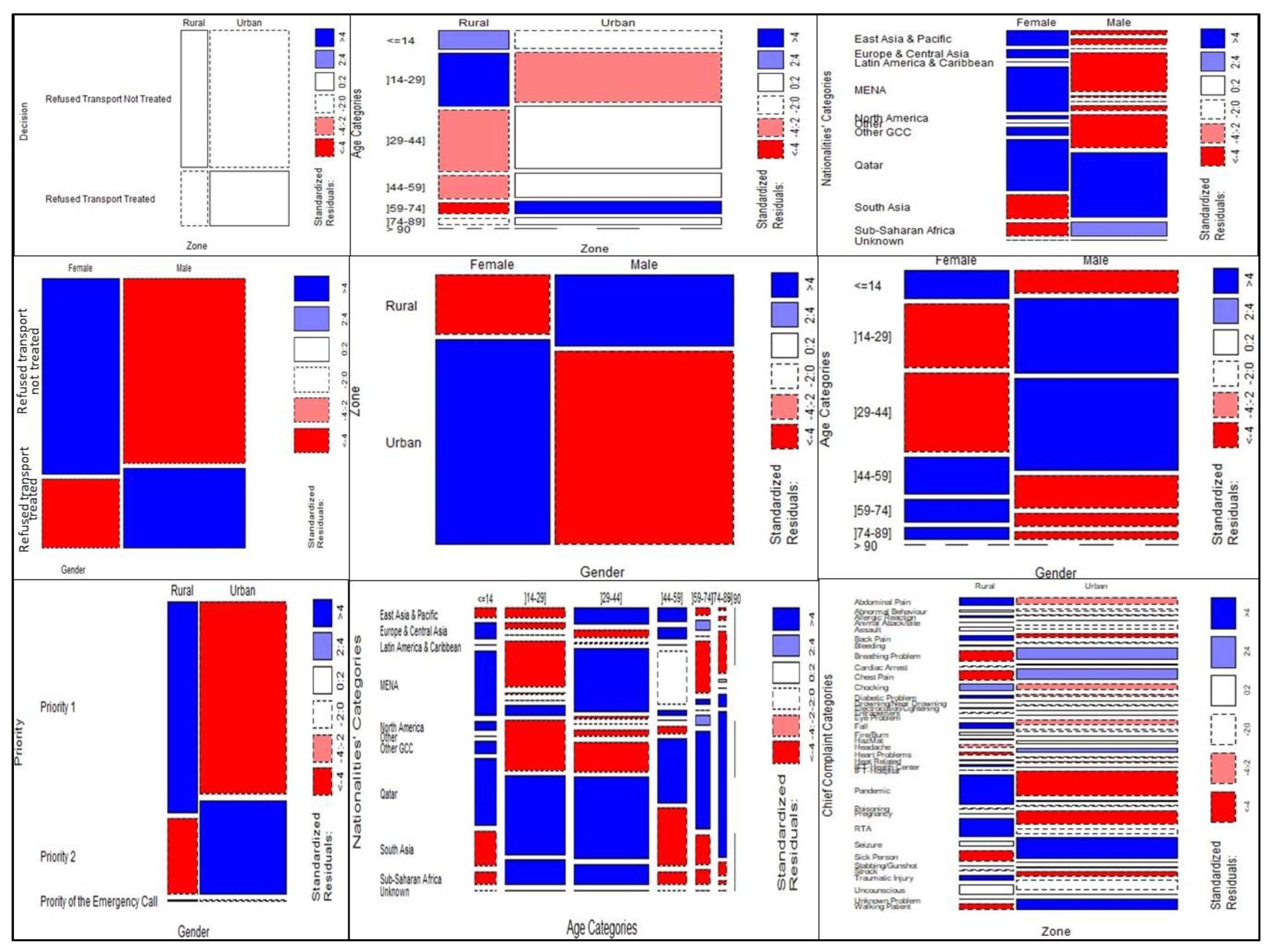
2. Methods
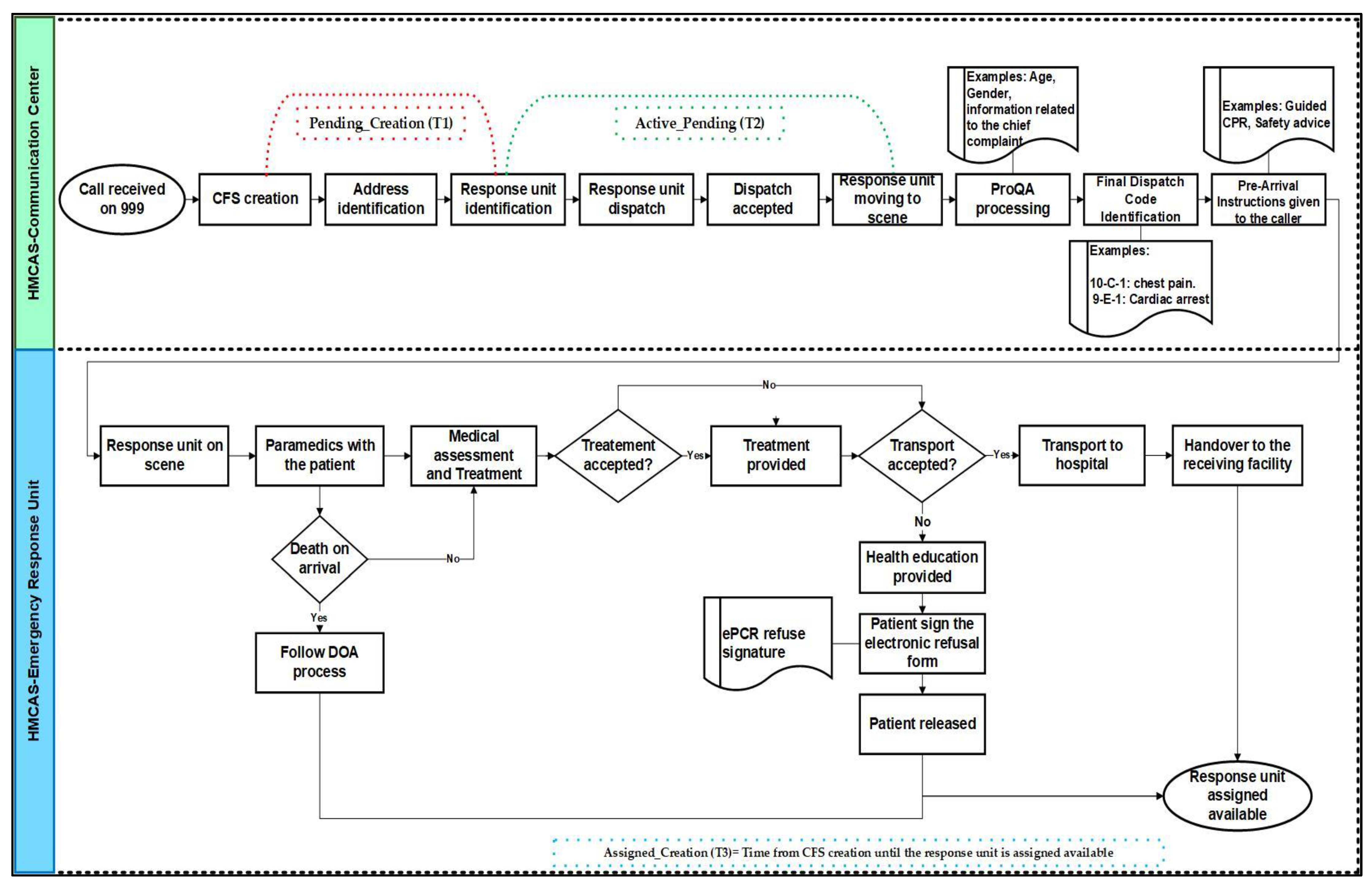
2.1. Study Design and Setting
2.2. Participants and Sampling
- -
- Emergency calls cancelled by the caller before the paramedics’ arrival, or the caller was not found or did not answer the callback, as they result in the EMD engaging with a 999-emergency call processing and providing the ambulance pre-arrival instructions until the ambulance arrived on the scene and was later assigned as available;
- -
- Paramedics arrived at the patient’s side and assessed them, but they refused transport;
- -
- A call was received from an emergency department from another healthcare facility, but the patient refused to be transported to hospital and was released to the community.
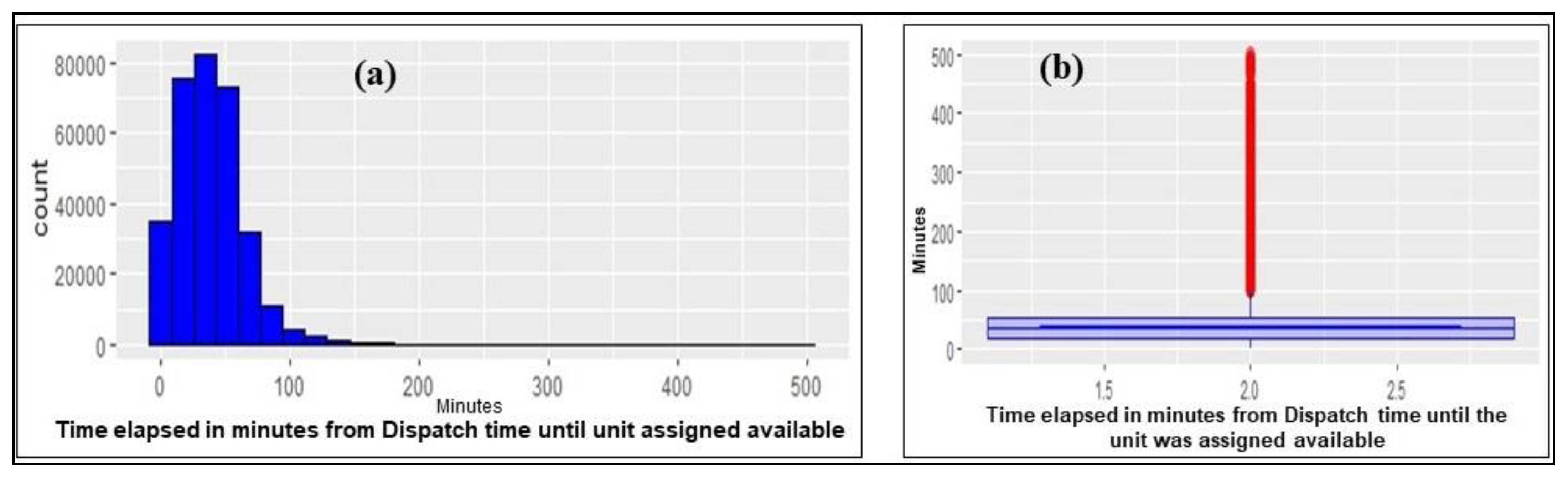
2.3. Quantitative Variables Handling and Measurements
- -
- T1: “Pending_Creation”: From when the EMD receives the emergency call until the closest unit to the emergency is found.
- -
- T2: “Active_Pending”: From when the EMD finds the closest unit to dispatch until that unit accepts the allocation and starts moving to the emergency call location.
- -
- T3: “Assigned_Creation”: From the time the EMD receives the emergency call until the unit dispatched treats the patient and is assigned as being available and ready for the next call.
- -
- Age: Patients were divided into groups according to World Health Organization age categories [16] (≤14 years; (15–29); (30–44); (45–59); (60–74); (75–89) and ≥90).
- -
- Nationalities: 273 nationalities, as recorded in the ePCR system. As the ePCR system has been evolving since it was implemented in the HMCAS in 2016 [27], each nationality was recorded in different ways (e.g.,: US, USA, and American). All recorded nationalities were grouped according to their geographical distribution [28]: Qatar, Gulf Cooperation Council (GCC), Middle East and North Africa (MENA), South Asia, East Asia and Pacific, Europe and Central Asia, Sub-Saharan Africa, North America, Latin America and the Caribbean, others, and unknown.
- -
- Zones: The Ministry of the Municipality in Qatar divides the location into 98 pre-determined zones. They were grouped into urban and rural areas.
- -
- Chief complaints: 1176 ProQA codes determined by the EMDs were grouped into 37 groups according to their chief complaints protocol defined by the International Academy of Emergency Medical Dispatchers [29].
- -
- Response unit: 537 units were dispatched as determined by the MDPS:
- ▪
- ▪
- Ambulances and rapid response cars with ambulance paramedic-credentialed staff from the emergency section (Alpha, Bravo, Delta, Specialized Emergency Management (SEM) and Events units).
- ▪
- Non-emergency section units with ambulance paramedic-credentialled staff (Foxtrot, Tango, COVID and Green bus). These can be dispatched if there is a lack of response units available in the emergency section at peak times, according to HMCAS Standard Operating Procedures.
- -
- Provisional Diagnosis: 158 provisional diagnoses determined by paramedics were grouped into 33 groups as follows: allergic reaction, anaphylaxis, animal bite, burns, cardiac arrest, cardiovascular, respiratory, shock, chronic medical condition (CMC), neurological, gastro-intestinal-gastro-urinary (GIGU), endocrinology, obstetrics and gynecology (OBS GYN), combative patient, diabetic problem, COVID-19 related, febrile illness, heat-related, hazardous material (HazMat), toxicology (other than HazMat exposure), interfacility transport (IFT), minor illness, electrocution, epistaxis, trauma, minor trauma, near-drowning, non-specific-problems (NSP), pain, non-traumatic back-pain, parental concern, sick person, undeniable death (as defined by the HMCAS Clinical Practical Guidelines), and not recorded.
- -
- Response timing duration (T1, T2, and T3).
2.4. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alinier, G.; Wilson, P.; Reimann, T.; Morris, B. Influential factors on urban and rural response times for emergency ambulances in Qatar. Mediterr. J. Emerg. Med. 2018, 26, 8–13. [Google Scholar]
- Clawson, J.; Olola, C.H.O.; Heward, A.; Scott, G.; Patterson, B. Accuracy of emergency medical dispatchers’ subjective ability to identify when higher dispatch levels are warranted over a Medical Priority Dispatch System automated protocol’s recommended coding based on paramedic outcome data. Emerg. Med. J. 2007, 24, 560–563. [Google Scholar] [CrossRef] [PubMed]
- Heinonen, K.; Puolakka, T.; Salmi, H.; Boyd, J.; Laiho, M.; Porthan, K.; Harve-Rytsälä, H.; Kuisma, M. Ambulance crew-initiated non-conveyance in the Helsinki EMS system—A retrospective cohort study. Acta Anaesthesiol. Scand. 2022, 66, 625–633. [Google Scholar] [CrossRef]
- Forsgärde, E.-S.; Elmqvist, C.; Fridlund, B.; Svensson, A.; Andersson, R.; Rööst, M. Patients’ aged ≥65 years dispositions during ambulance assignments, including factors associated with non-conveyance to hospital: A longitudinal and comparative study. BMJ Open 2020, 10, e038885. [Google Scholar] [CrossRef] [PubMed]
- Moafa, H.N.; van Kuijk, S.M.J.; Moukhyer, M.E.; Alqahtani, D.M.; Haak, H.R. Non-Conveyance Due to Patient-Initiated Refusal in Emergency Medical Services: A Retrospective Population-Based Registry Analysis Study in Riyadh Province, Saudi Arabia. Int. J. Environ. Res. Public. Health 2021, 18, 9252. [Google Scholar] [CrossRef]
- Bohm, K.; Kurland, L. The accuracy of medical dispatch—A systematic review. Scand. J. Trauma Resusc. Emerg. Med. 2018, 26, 94. [Google Scholar] [CrossRef]
- Farhat, H.; Alinier, G.; El Aifa, K.; Athemneh, K.; Gangaram, P.; Romero, R.; Khenissi, M.C.; Al Shaikh, L.; Laughton, J. Quality improvement tools to manage emergency callbacks from patients with diabetes in a prehospital setting. BMJ Open Qual. 2023, 12, e002007. [Google Scholar] [CrossRef]
- World Health Organization. Emergency Care Systems for Universal Health Coverage: Ensuring Timely Care for the Acutely Ill and Injured; World Health Organization: Geneva, Switzerland, 2019; Available online: https://apps.who.int/gb/ebwha/pdf_files/WHA72/A72_R16-en.pdf?ua=1 (accessed on 11 February 2023).
- Planning and Statistics Authority. Monthly Figures on Total Population. 2023. Available online: https://www.psa.gov.qa/en/statistics1/StatisticsSite/pages/population.aspx (accessed on 11 February 2023).
- Online Qatar. Qatar Population and Expat Nationalities. 2019. Available online: https://www.onlineqatar.com/visiting/tourist-information/qatar-population-and-expat-nationalities (accessed on 11 February 2023).
- Demir, S.; Tunçbilek, Z.; Alinier, G. Prehospital emergency health services in Qatar. J. Paramed. Pract. 2022, 14, 456–462. [Google Scholar] [CrossRef]
- Campbell, C.B. ECMO retrieval: A case for Critical Care Paramedic integration into the team. Qatar Med. J. 2017. [Google Scholar] [CrossRef]
- Al-Thani, H.; Mekkodathil, A.; Hertelendy, A.J.; Howland, I.; Frazier, T.; El-Menyar, A. Emergency Medical Services (EMS) Transportation of Trauma Patients by Geographic Locations and In-Hospital Outcomes: Experience from Qatar. Int. J. Environ. Res. Public. Health 2021, 18, 4016. [Google Scholar] [CrossRef]
- O’Cathain, A.; Jacques, R.; Stone, T.; Turner, J. Why do ambulance services have different non-transport rates? A national cross sectional study. PLoS ONE 2018, 13, e0204508. [Google Scholar] [CrossRef]
- Hunt, G.J.; Dane, M.A.; Korkola, J.E.; Heiser, L.M.; Gagnon-Bartsch, J.A. Automatic Transformation and Integration to Improve Visualization and Discovery of Latent Effects in Imaging Data. J. Comput. Graph. Stat. 2020, 29, 929–941. [Google Scholar] [CrossRef]
- World Health Organization. Age Group Codelist. In Regional Health Observatory—South East Asia; World Health Organization: Geneva, Switzerland, 2013; Available online: https://apps.who.int/gho/data/node.searo-metadata.AGEGROUP?lang=en (accessed on 22 December 2022).
- Bhaganagar, K.; Bhimireddy, S.R. Assessment of the plume dispersion due to chemical attack on April 4, 2017, in Syria. Nat. Hazards 2017, 88, 1893–1901. [Google Scholar] [CrossRef]
- Nemiroff, L.; Marshall, E.G.; Jensen, J.L.; Clarke, B.; Andrew, M.K. Adherence to ‘No Transfer to Hospital’ Advance Directives Among Nursing Home Residents. J. Am. Med. Dir. Assoc. 2019, 20, 1373–1381. [Google Scholar] [CrossRef]
- Cooney, D.R.; Millin, M.G.; Carter, A.; Lawner, B.J.; Nable, J.V.; Wallus, H.J. Ambulance Diversion and Emergency Department Offload Delay: Resource Document for the National Association of EMS Physicians Position Statement. Prehosp. Emerg. Care 2011, 15, 555–561. [Google Scholar] [CrossRef]
- Cone, D.C.; Middleton, P.M.; Pour, S.M. Analysis and impact of delays in ambulance to emergency department handovers. Emerg. Med. Australas. 2012, 24, 525–533. [Google Scholar] [CrossRef]
- Butt, A.A.; Azad, A.M.; Kartha, A.B.; Masoodi, N.A.; Bertollini, R.; Abou-Samra, A.-B. Volume and Acuity of Emergency Department Visits Prior To and After COVID-19. J. Emerg. Med. 2020, 59, 730–734. [Google Scholar] [CrossRef]
- Ivic, R.; Vicente, V.; Kurland, L.; Svensson, J.; Klintemård, R.S.; Castrén, M.; Bohm, K. Pre-hospital emergency nurse specialist’s experiences in caring for patients with non-specific chief complaints in the ambulance—A qualitative interview study. Int. Emerg. Nurs. 2022, 63, 101178. Available online: https://www.sciencedirect.com/science/article/pii/S1755599X22000350 (accessed on 8 July 2022). [CrossRef]
- Beaulieu-Jones, B.K.; Lavage, D.R.; Snyder, J.W.; Moore, J.H.; Pendergrass, S.A.; Bauer, C.R. Characterizing and Managing Missing Structured Data in Electronic Health Records: Data Analysis. JMIR Med. Inform. 2018, 6, e8960. [Google Scholar] [CrossRef]
- Benhar, H.; Idri, A.; Fernández-Alemán, J.L. Data preprocessing for heart disease classification: A systematic literature review. Comput. Methods Programs Biomed. 2020, 195, 105635. [Google Scholar] [CrossRef]
- Zheng, S.; Edwards, J.R.; Dudeck, M.A.; Patel, P.R.; Wattenmaker, L.; Mirza, M.; Tejedor, S.C.; Lemoine, K.; Benin, A.L.; Pollock, D.A. Building an Interactive Geospatial Visualization Application for National Health Care–Associated Infection Surveillance: Development Study. JMIR Public Health Surveill. 2021, 7, e23528. [Google Scholar] [CrossRef] [PubMed]
- McDonald, J.H. Kruskal–Wallis Test—Handbook of Biological Statistics; Sparky House Publishing: Baltimore, MD, USA, 2015; pp. 157–164. Available online: http://www.biostathandbook.com/kruskalwallis.html (accessed on 5 October 2022).
- Hamad Medical Corporation. HMC’s Ambulance Service Records More Than Two Million Patient Encounters Through its Electronic Patient Clinical Record. 2022. Available online: https://www.hamad.qa:443/EN/news/2022/September/Pages/HMC-Ambulance-Service-Records-More-Than-Two-Million-Patient-Encounters-Through-its-Electronic-Patient-Clinical-Record.aspx (accessed on 11 January 2023).
- United Nation Statistics Division. The Online Version of the United Nations Publication ‘Standard Country or Area Codes for Statistical Use’. 2020. Available online: https://unstats.un.org/unsd/methodology/m49/ (accessed on 11 January 2023).
- Clwason, J.J.; Dernocoeur, K.B.; Murray, C. Principles of Emergency Medical Dispatch, 5th ed.; The International Academy of EMD: Salt Lake City, UT, USA, 2014. [Google Scholar]
- Farhat, H.; Laughton, J.; Gangaram, P.; El Aifa, K.; Khenissi, M.C.; Zaghouani, O.; Khadhraoui, M.; Gargouri, I.; Alinier, G. Hazardous material and chemical, biological, radiological, and nuclear incident readiness among prehospital care professionals in the State of Qatar. Glob. Secur. Health Sci. Policy 2022, 7, 24–36. [Google Scholar] [CrossRef]
- Gangaram, P.; Alinier, G.; Menacho, A.M. Crisis Resource Management in emergency medical settings in Qatar. Int. Paramed. Pract. 2017, 7, 18–23. [Google Scholar] [CrossRef]
- Cheema, M.U.; Munir, R.; Su, S. Corporate Governance and Whistleblowing: Corporate Culture and Employee Behaviour; Routledge: Abingdon-on-Thames, UK, 2021. [Google Scholar]
- Artetxe, A.; Beristain, A.; Graña, M. Predictive models for hospital readmission risk: A systematic review of methods. Comput. Methods Programs Biomed. 2018, 164, 49–64. [Google Scholar] [CrossRef]
- Zimmerman, L.P.; Reyfman, P.A.; Smith, A.D.; Zeng, Z.; Kho, A.; Sanchez-Pinto, L.N.; Luo, Y. Early prediction of acute kidney injury following ICU admission using a multivariate panel of physiological measurements. BMC Med. Inform. Decis. Mak. 2019, 19, 16. [Google Scholar] [CrossRef]
- Scott, G. Characterization of Call Prioritization Time in a Medical Priority Dispatch System. Ann. Emerg. Dispatch Response 2016, 4, 27–33. [Google Scholar]
- Thornto, J. Covid-19: A&E visits in England fall by 25% in week after lockdown. BMJ 2020, 369, m1401. [Google Scholar]
- Satty, T.; Ramgopal, S.; Elmer, J.; Mosesso, V.N.; Martin-Gill, C. EMS responses and non-transports during the COVID-19 pandemic. Am. J. Emerg. Med. 2021, 42, 1–8. [Google Scholar] [CrossRef]
- Kurt, N.G.; Gunes, C. How has Covid-19 pandemic affected crowded emergency services? Int. J. Clin. Pract. 2020, 74, e13624. [Google Scholar] [CrossRef]
- Al Kuwari, H.M.; Rahim, H.F.A.; Abu-Raddad, L.J.; Abou-Samra, A.B.; Al Kanaani, Z.; Al Khal, A.; Al Kuwari, E.; Al Marri, S.; Al Masalmani, M.; Al Romaihi, H.E.; et al. Epidemiological investigation of the first 5685 cases of SARS-CoV-2 infection in Qatar, 28 February–18 April 2020. BMJ Open 2020, 10, e040428. [Google Scholar] [CrossRef]
- World Health Organization. Qatar: WHO Coronavirus Disease (COVID-19) Dashboard With Vaccination Data. 2023. Available online: https://covid19.who.int (accessed on 10 February 2023).
- Oxford Business Group. The Report: Qatar 2016; Oxford Business Group: London, UK, 2016. [Google Scholar]
- Aboobacker, V.M.; Samiksha, S.V.; Veerasingam, S.; Al-Ansari, E.M.A.S.; Vethamony, P. Role of shamal and easterly winds on the wave characteristics off Qatar, central Arabian Gulf. Ocean Eng. 2021, 236, 109457. [Google Scholar] [CrossRef]
- Irfan, F.B.; Pathan, S.A.; Bhutta, Z.A.; Abbasy, M.E.; Elmoheen, A.; Elsaeidy, A.M.; Tariq, T.; Hugelmeyer, C.D.; Dardouri, H.; Shah, N.B.K.B.; et al. Health System Response and Adaptation to the Largest Sandstorm in the Middle East. Disaster Med. Public Health Prep. 2017, 11, 227–238. [Google Scholar] [CrossRef]
- Vloet, L.; de Kreek, A.; van der Linden, E.; van Spijk, J.J.; Theunissen, V.A.; van Wanrooij, M.; van Grunsven, P.M.; Ebben, R.H. A retrospective comparison between non-conveyed and conveyed patients in ambulance care. Scand. J. Trauma Resusc. Emerg. Med. 2018, 26, 91. [Google Scholar] [CrossRef]
- Ali, M.; Alamin, M.A.; AAli, G.; Alzubaidi, K.; Ali, B.; Ismail, A.; Daghfal, J.; Almaslamani, M.; Hadi, H.A. Microbiological and clinical characteristics of invasive Group B Streptococcal blood stream infections in children and adults from Qatar. BMC Infect. Dis. 2022, 22, 881. [Google Scholar] [CrossRef]
- Mathew, S.; Alansari, K.; Smatti, M.K.; Zaraket, H.; Al Thani, A.A.; Yassine, H.M. Epidemiological, Molecular, and Clinical Features of Norovirus Infections among Pediatric Patients in Qatar. Viruses 2019, 11, 400. [Google Scholar] [CrossRef]
- Abdulnassir FH Aljaziri and Alinier. Access to Emergency Healthcare. In Healthcare Access; IntechOpen: London, UK, 2022; p. 171. [Google Scholar]
- Laffineur, C.; Tavakoli, M.; Fayolle, A.; Amara, N.; Carco, M. Insights from Female Entrepreneurs in MENA Countries: Barriers and Success Factors. In Entrepreneurship Ecosystem in the Middle East and North Africa (MENA): Dynamics in Trends, Policy and Business Environment; Faghih, N., Zali, M.R., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 351–397. [Google Scholar] [CrossRef]
- Assaad, R.; Hendy, R.; Lassassi, M.; Yassin, S. Explaining the MENA Paradox: Rising Educational Attainment, Yet Stagnant Female Labor Force Participation. Demogr. Res. 2020, 43, 817–850. [Google Scholar] [CrossRef]
- Planning and Statistics Authority. Population. 2023. Available online: https://www.psa.gov.qa/en/statistics1/pages/topicslisting.aspx?parent=Population&child=Population (accessed on 11 January 2023).
- Al-Thani, H.; El-Menyar, A.; Consunji, R.; Mekkodathil, A.; Peralta, R.; Allen, K.A.; Hyder, A.A. Epidemiology of occupational injuries by nationality in Qatar: Evidence for focused occupational safety programmes. Injury 2015, 46, 1806–1813. [Google Scholar] [CrossRef]
- Moafa, H.N.; van Kuijk, S.M.J.; Alqahtani, D.M.; Moukhyer, M.E.; Haak, H.R. Disparities between Rural and Urban Areas of the Central Region of Saudi Arabia in the Utilization and Time-Centeredness of Emergency Medical Services. Int. J. Environ. Res. Public. Health 2020, 17, 7944. [Google Scholar] [CrossRef]
- Moafa, H.N.; van Kuijk, S.M.; Moukhyer, M.E.; Alqahtani, D.M.; Haak, H.R. Variation in on-scene time of emergency medical services and the extent of the difference of on-scene time between genders: A retrospective population-based registry study in Riyadh Province, Saudi Arabia. BMJ Open 2022, 12, e052481. [Google Scholar] [CrossRef]
- Shaheen, Y.; Al-Maadid, F.; Soliman, M.; Melikyan, G.; Mesraoua, B.; Deleu, D.; Al Hail, H.J.; Own, A.; El Sotouhy, A.; Mahfoud, Z.; et al. Neurocysticercosis in Qatar (P5.9-032). Neurology 2019, 92. Available online: https://n.neurology.org/content/92/15_Supplement/P5.9-032 (accessed on 11 January 2023).
- Lipson, J.G.; Meleis, A.I. Issues in Health Care of Middle Eastern Patients. West. J. Med. 1983, 139, 854–861. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1011016/ (accessed on 11 January 2023).
- Klautzer, L.; Becker, J.; Mattke, S. The curse of wealth—Middle Eastern countries need to address the rapidly rising burden of diabetes. Int. J. Health Policy Manag. 2014, 2, 109–114. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Magnusson, C. Patient Assessment and Triage in Emergency Medical Services—The Swedish EMS Nurse in a New Role. Ph.D. Thesis, University of Gothenburg, Gothenburg, Sweden, 2021. Available online: https://gupea.ub.gu.se/handle/2077/67134 (accessed on 11 February 2023).
- Alhabdan, N.; Alhusain, F.; Alharbi, A.; Alsadhan, M.; Hakami, M.; Masuadi, E. Exploring emergency department visits: Factors influencing individuals’ decisions, knowledge of triage systems and waiting times, and experiences during visits to a tertiary hospital in Saudi Arabia. Int. J. Emerg. Med. 2019, 12, 35. [Google Scholar] [CrossRef] [PubMed]
- Markun, S.; Holzer, B.M.; Rodak, R.; Kaplan, V.; Wagner, C.C.; Battegay, E.; Zimmerli, L. Therapeutic Conflicts in Emergency Department Patients with Multimorbidity: A Cross-Sectional Study. PLoS ONE 2014, 9, e110309. [Google Scholar] [CrossRef] [PubMed]
- Koenig, K.L. Emergency Ambulance Utilization in Harlem, New York (July 1985). Prehosp. Emerg. Care 2022, 26, W1–W17. [Google Scholar] [CrossRef]
- O’Cathain, A.; Knowles, E.; Bishop-Edwards, L.; Coster, J.; Crum, A.; Jacques, R.; James, C.; Lawson, R.; Marsh, M.; O’Hara, R.; et al. Understanding Variation in Ambulance Service Non-Conveyance Rates: A Mixed Methods Study. 2018. Available online: http://uhra.herts.ac.uk/handle/2299/20208 (accessed on 8 July 2022).
- Patton, A.; O’Donnell, C.; Keane, O.; Henry, K.; Crowley, D.; Collins, A.; Redmond, E.; Glynn, N.; Dunne, M.; Deasy, C. The Alternative Pre-hospital Pathway team: Reducing conveyances to the emergency department through patient centered Community Emergency Medicine. BMC Emerg. Med. 2021, 21, 138. [Google Scholar] [CrossRef]
- Leikkola, P.; Mikkola, R.; Salminen-Tuomaala, M.; Paavilainen, E. Non-Conveyance of Patients: Challenges to Decision-Making in Emergency Care. 2016. Available online: https://trepo.tuni.fi/handle/10024/99964 (accessed on 18 February 2023).
- Lowing, D.; Chung, S.; Luk, J.; Dingeldein, L. Prehospital Epinephrine Use in Pediatric Anaphylaxis by Emergency Medical Services. Pediatr. Emerg. Care 2022, 38, 367. [Google Scholar] [CrossRef]
- Hana, P.S. Logistic Regression (with Elastic Net Regularization). In Logistic Regression (with Elastic Net Regularization), 2.0. SAP HANA Predictive Analysis Library (PAL); SAP: London, UK, 2017; Available online: https://help.sap.com/docs/SAP_HANA_PLATFORM/2cfbc5cf2bc14f028cfbe2a2bba60a50/46effe560ea74ecbbf43bab011f2acf8.html?version=2.0.01&locale=en-US (accessed on 16 October 2022).
| Description | Sub-Groups | Data after Pre-Processing | |
|---|---|---|---|
| Frequencies | Percentages (%) | ||
| Decision | Refused Transport and Not Treated | 169,552 | 71.28 |
| Refused Transport and Treated | 67,062 | 28.19 | |
| DOA | 1248 | 0.52 | |
| Gender | Male | 145,610 | 61.22 |
| Female | 92,252 | 38.78 | |
| Zone | Urban | 177,424 | 74.59 |
| Rural | 60,438 | 25.41 | |
| Age groups (Years) | ≤14 | 24,769 | 10.41 |
| (15–29) | 68,586 | 28.83 | |
| (30–44) | 84,841 | 35.67 | |
| (45–59) | 33,252 | 13.98 | |
| (60–74) | 16,635 | 6.99 | |
| (75–89) | 8766 | 3.69 | |
| ≥90 | 1013 | 0.43 | |
| Years | 2018 (June to December) | 21,671 | 9.11 |
| 2019 | 43,771 | 18.40 | |
| 2020 | 61,936 | 26.04 | |
| 2021 | 62,964 | 26.47 | |
| 2022 (January to July) | 47,520 | 19.98 | |
| Months | April | 34,325 | 14.43 |
| March | 3558 | 14.11 | |
| January | 33,382 | 14.03 | |
| May | 32,396 | 13.62 | |
| June | 30,208 | 12.70 | |
| February | 27,768 | 11.67 | |
| July | 10,276 | 4.32 | |
| December | 9181 | 3.86 | |
| August | 6901 | 2.90 | |
| November | 6875 | 2.89 | |
| September | 6585 | 2.77 | |
| October | 6407 | 2.69 | |
| Response priorities | Priority 1 | 163,923 | 68.92 |
| Priority 2 | 73,388 | 30.85 | |
| Others (Walking patients, referral, or self-dispatch) | 551 | 0.23 | |
| Region based on Nationality | South Asia | 69,849 | 29.37 |
| MENA | 57,936 | 24.36 | |
| Qatar | 56,558 | 23.78 | |
| Sub-Saharan Africa | 19,302 | 8.12 | |
| East Asia and the Pacific | 12,286 | 5.17 | |
| Europe and Central Asia | 9143 | 3.84 | |
| Other GCC | 8863 | 3.73 | |
| North America | 3212 | 1.35 | |
| Latin America and the Caribbean | 453 | 0.19 | |
| Unknown | 203 | 0.09 | |
| Other (i.e., officials such as United Nations) | 57 | 0.02 | |
| Emergency Response Units | Alpha | 206,338 | 86.75 |
| Bravo | 19,663 | 8.27 | |
| Charlie | 331 | 0.14 | |
| COVID | 111 | 0.05 | |
| Delta | 505 | 0.21 | |
| Event | 2198 | 0.92 | |
| Foxtrot | 368 | 0.16 | |
| Green Bus | 1028 | 0.43 | |
| SEM | 7193 | 3.02 | |
| Tango | 127 | 0.05 | |
| Age Group Categories (Years) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤14 | (15–29) | (30–44) | (45–59) | (60–74) | (75–89) | ≥90 | Total | |||||||||
| % | n | % | n | % | N | % | n | % | n | % | N | % | n | % | N | |
| Pandemic (P 36) | 1.5 | 3622 | 3.7 | 8779 | 6.1 | 14,584 | 2.4 | 5726 | 1.6 | 3793 | 1.1 | 2568 | 0.15 | 375 | 16.58 | 39,447 |
| Sick Person (P 26) | 1.5 | 3600 | 3.1 | 7431 | 3.4 | 8184 | 1.7 | 4119 | 1.1 | 2489 | 0.5 | 1161 | 0.04 | 116 | 11.38 | 27,100 |
| RTA (P 29) | 0.8 | 1788 | 4.2 | 9902 | 3.6 | 8645 | 0.9 | 2141 | 0.1 | 332 | 0 | 52 | 0 | 5 | 9.602 | 22,865 |
| Breathing Problem (P 6) | 0.7 | 1627 | 1.9 | 4569 | 2.3 | 5381 | 1.1 | 2588 | 0.7 | 1733 | 0.6 | 1393 | 0.06 | 163 | 7.33 | 17,454 |
| Chest Pain (P 10) | 0.1 | 292 | 1.1 | 2682 | 2.5 | 5932 | 1.4 | 3221 | 0.7 | 1697 | 0.4 | 888 | 0.02 | 64 | 6.19 | 14,776 |
| Unconscious (P 31) | 0.3 | 751 | 2 | 4860 | 2.3 | 5404 | 0.9 | 2057 | 0.4 | 909 | 0.2 | 433 | 0.02 | 54 | 6.083 | 14,468 |
| Walking Patient | 0.6 | 1530 | 1.8 | 4174 | 1.9 | 4591 | 0.8 | 1927 | 0.4 | 881 | 0.1 | 199 | 0 | 7 | 5.593 | 13,309 |
| Abdominal Pain (P 1) | 0.2 | 463 | 1.5 | 3512 | 1.8 | 4296 | 0.6 | 1432 | 0.3 | 629 | 0.1 | 320 | 0.01 | 27 | 4.5 | 10,679 |
| Choking (P 11) | 0.7 | 1649 | 1.4 | 3224 | 1.4 | 3377 | 0.4 | 837 | 0.1 | 237 | 0 | 33 | 0.01 | 12 | 3.935 | 9369 |
| Fall (P 17) | 1.1 | 2505 | 0.7 | 1713 | 0.8 | 1947 | 0.4 | 1047 | 0.2 | 384 | 0.1 | 161 | 0.01 | 12 | 3.265 | 7769 |
| Seizure (P 12) | 0.3 | 590 | 1.1 | 2597 | 1.1 | 2661 | 0.3 | 672 | 0.1 | 208 | 0 | 75 | 0.01 | 11 | 2.865 | 6814 |
| Traumatic Injury (P 30) | 0.9 | 2057 | 0.9 | 2036 | 0.8 | 1812 | 0.2 | 508 | 0.1 | 168 | 0 | 60 | 0 | 0 | 2.803 | 6641 |
| Non-traumatic Back Pain (P5) | 0 | 53 | 0.6 | 1463 | 1.2 | 2912 | 0.6 | 1333 | 0.2 | 396 | 0.1 | 132 | 0 | 5 | 2.652 | 6294 |
| Assault (P 4) | 0.1 | 180 | 1.1 | 2492 | 1.2 | 2803 | 0.2 | 545 | 0 | 42 | 0 | 11 | 0 | 2 | 2.571 | 6075 |
| Heart Problems (P 19) | 0.1 | 285 | 0.5 | 1293 | 0.9 | 2241 | 0.4 | 943 | 0.2 | 512 | 0.1 | 183 | 0.01 | 29 | 2.31 | 5486 |
| Age Group Categories (Years) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤14 | (15–29) | (30–44) | (45–59) | (60–74) | (75–89) | ≥90 | Total | |||||||||
| % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | |
| NSP | 3.06 | 7268 | 6.14 | 14,600 | 7.49 | 17,822 | 2.83 | 6727 | 1.55 | 3690 | 0.77 | 1841 | 0.1 | 203 | 21.9 | 52,151 |
| Pain | 0.46 | 1102 | 4.15 | 9859 | 6.88 | 14,480 | 2.7 | 6425 | 1.18 | 2816 | 0.5 | 1194 | 0.04 | 99 | 15.9 | 35,975 |
| Minor Trauma | 2.05 | 4869 | 5.67 | 13,488 | 4.5 | 11,876 | 1.21 | 2876 | 0.35 | 838 | 0.11 | 258 | 0.01 | 30 | 13.9 | 34,235 |
| Neurological | 0.25 | 587 | 2.58 | 6138 | 2.99 | 7102 | 1.19 | 2826 | 0.44 | 1036 | 0.18 | 419 | 0.01 | 30 | 7.64 | 18,138 |
| GIGU | 0.5 | 1199 | 2.25 | 5340 | 2.95 | 7013 | 1.04 | 2480 | 0.46 | 1095 | 0.25 | 598 | 0.02 | 47 | 7.47 | 17,772 |
| Minor Illness | 0.71 | 1687 | 1.36 | 3240 | 1.86 | 4427 | 0.83 | 1976 | 0.53 | 1253 | 0.35 | 827 | 0.04 | 103 | 5.68 | 13,513 |
| Respiratory | 0.63 | 1497 | 1.39 | 3305 | 1.83 | 4356 | 0.79 | 1886 | 0.38 | 907 | 0.37 | 868 | 0.05 | 108 | 5.44 | 12,927 |
| Trauma | 0.55 | 1311 | 1.6 | 3810 | 1.58 | 3762 | 0.43 | 1026 | 0.1 | 247 | 0.03 | 59 | 0 | 1 | 4.29 | 10,216 |
| Febrile Illness | 0.86 | 2056 | 1.04 | 2470 | 1.4 | 3305 | 0.47 | 1108 | 0.28 | 665 | 0.18 | 417 | 0.03 | 78 | 4.26 | 10,099 |
| COVID-19 Related | 0.48 | 1134 | 0.81 | 1920 | 1.8 | 4183 | 0.7 | 1667 | 0.3 | 720 | 0.12 | 289 | 0.01 | 33 | 4.22 | 9946 |
| Diabetic Problem | 0.04 | 89 | 0.22 | 524 | 0.42 | 987 | 0.4 | 939 | 0.41 | 968 | 0.23 | 550 | 0.01 | 23 | 1.73 | 4080 |
| CMC | 0.04 | 86 | 0.13 | 312 | 0.3 | 703 | 0.33 | 783 | 0.47 | 1112 | 0.38 | 894 | 0.1 | 152 | 1.75 | 4042 |
| Cardiovascular | 0.01 | 30 | 0.16 | 378 | 0.47 | 1112 | 0.49 | 1166 | 0.33 | 787 | 0.15 | 361 | 0.01 | 32 | 1.62 | 3866 |
| Burns | 0.18 | 433 | 0.36 | 860 | 0.04 | 917 | 0.14 | 325 | 0.04 | 93 | 0.01 | 16 | 0 | 0 | 0.77 | 2644 |
| Allergic Reaction | 0.16 | 830 | 0.2 | 483 | 0.22 | 537 | 0.09 | 205 | 0.03 | 73 | 0.01 | 16 | 0 | 3 | 0.71 | 2147 |
| Part I: Chi-Square Test of Patient Non-Conveyance Decisions Groups and Other Groups of Variables: | ||||
|---|---|---|---|---|
| Variables | Subgroups | Patient Non-conveyance decisions | Chi-square | |
| Refused Transport and Not Treated | Refused Transport and Treated | |||
| observed (expected) | observed (expected) | |||
| Zone | Rural | 43,058 (43,047.61) | 17,016 (17,039.68) | X2 = 0.01, df = 1, p-value = 0.91 |
| Urban | 126,494 (126,504.39) | 50,046 (50,035.61) | ||
| Gender | Male | 101,361 (103,793.24) | 43,214 (41,052.79) | X2 = 438.34, df = 1, p-value < 2.2 × 10−16 |
| Female | 68,191 (65,758.76) | 23,848 (26,009.21) | ||
| Year | 2018 (June to December) | 15,578 (15,447.45) | 5955 (6109.84) | X2 = 74.93, df = 4, p-value = 2.06 × 10−15 |
| 2019 | 31,054 (31,200.70) | 12,492 (12,340.64) | ||
| 2020 | 44,747 (44,149.01) | 16,907 (17,462.02) | ||
| 2021 | 44,158 (44,881.79) | 18,455 (17,751.85) | ||
| 2022 (January to July) | 34,015 (33,873.05) | 13,253 (13,397.62) | ||
| Response priorities | Priority 1 | 122,323 (116,847.04) | 40,441 (46,215.89) | X2 = 3157.8, df = 2, p-value = 2.2 × 10−16 |
| Priority 2 | 46,830 (52,312.19) | 26,469 (20,690.76) | ||
| Other response priorities | 399 (392.76) | 152 (155.34) | ||
| Part II: The Mann-Whitney U Test (Wilcoxon Rank Sum Test) for the Non-Conveyance: | ||||
| W-values | p-values | |||
| Patient non-conveyance decisions | Months | 5,562,400,046 | <2.2 × 10−16 | |
| Nationalities Categories | 5,419,676,164 | 2.2 × 10−8 | ||
| Provisional diagnoses categories | 5,182,154,299 | <2.2 × 10−16 | ||
| Response units categories | 6,102,256,789 | <2.2 × 10−16 | ||
| Age categories | 5,580,476,590 | 3.59 × 10−13 | ||
| Duration from CFS creation to assigned available | 5,647,879,250 | 0.01 | ||
| Duration from CFS creation to pending dispatch | 6,196,555,806 | <2.2 × 10−16 | ||
| Duration from CFS pending to active dispatch | 5,950,198,517 | <2.2 × 10−16 | ||
| Part (I) Variables with Positive Coefficients in the Backward Model | |||||||
|---|---|---|---|---|---|---|---|
| Variables | Sub-categories | Coefficients | OR | p-value | 95% CI | ||
| Gender | Male | 0.11 | 1.11 | <0.001 | 0.09, 0.13 | ||
| Years | 2019 | 0.15 | 1.17 | <0.001 | 0.11, 0.20 | ||
| 2020 | 0.40 | 1.50 | <0.001 | 0.35, 0.46 | |||
| 2021 | 0.56 | 1.75 | <0.001 | 0.51, 0.61 | |||
| 2022 | 0.48 | 1.62 | <0.001 | 0.43, 0.54 | |||
| Months | August | 0.21 | 1.23 | <0.001 | 0.14, 0.28 | ||
| December | 0.26 | 1.30 | <0.001 | 0.20, 0.32 | |||
| July | 0.12 | 1.13 | <0.001 | 0.06, 0.17 | |||
| June | 0.08 | 1.08 | <0.001 | 0.04, 0.12 | |||
| May | 0.08 | 1.08 | <0.001 | 0.04, 0.12 | |||
| November | 0.31 | 1.36 | <0.001 | 0.24, 0.38 | |||
| October | 0.21 | 1.23 | <0.001 | 0.14, 0.28 | |||
| September | 0.31 | 1.36 | <0.001 | 0.24, 0.38 | |||
| Nationalities categories | Other GCC | 0.15 | 1.16 | <0.001 | 0.08, 0.22 | ||
| Qatar | 0.18 | 1.19 | <0.001 | 0.13, 0.23 | |||
| South Asia | 0.25 | 1.28 | <0.001 | 0.20, 0.30 | |||
| Sub-Saharan Africa | 0.24 | 1.27 | <0.001 | 0.19, 0.30 | |||
| Chief complaints (Call-taking protocols) | Back Pain (Protocol 5) | 0.21 | 1.23 | <0.001 | 0.14, 0.27 | ||
| Units’ categories | Bravo | 1.3 | 3.72 | <0.001 | 1.3, 1.4 | ||
| Event | 0.24 | 1.27 | <0.001 | 0.14, 0.34 | |||
| Provisional diagnoses categories | Anaphylaxis | 1.3 | 3.61 | <0.001 | 0.86, 1.7 | ||
| Burns | 1.0 | 2.82 | <0.001 | 0.86, 1.2 | |||
| Cardiovascular | 0.27 | 1.31 | 0.002 | 0.10, 0.44 | |||
| CMC | 0.48 | 1.62 | <0.001 | 0.32, 0.65 | |||
| Diabetic Problem | 0.93 | 2.54 | <0.001 | 0.76, 1.1 | |||
| Epistaxis | 0.68 | 1.98 | <0.001 | 0.48, 0.89 | |||
| Febrile Illness | 0.94 | 2.57 | <0.001 | 0.79, 1.1 | |||
| GIGU | 0.91 | 2.49 | <0.001 | 0.76, 1.1 | |||
| HazMat | 0.41 | 1.51 | <0.001 | 0.19, 0.63 | |||
| Heat-Related | 1.4 | 3.93 | <0.001 | 1.2, 1.6 | |||
| Minor Trauma | 1.3 | 3.79 | <0.001 | 1.2, 1.5 | |||
| Neurological | 0.78 | 2.19 | <0.001 | 0.63, 0.94 | |||
| Not Recorded | 1.9 | 6.67 | <0.001 | 0.98, 2.8 | |||
| Pain | 0.98 | 2.66 | <0.001 | 0.83, 1.1 | |||
| Respiratory | 0.80 | 2.23 | <0.001 | 0.65, 0.96 | |||
| Shock | 2.0 | 7.56 | <0.001 | 1.6, 2.5 | |||
| Sick Person | 0.75 | 2.11 | 0.004 | 0.24, 1.2 | |||
| Trauma | 1.1 | 3.14 | <0.001 | 0.98, 1.3 | |||
| Response time durations | T1 (“Pending_Creation”) | 3.06 × 10−3 | 1.00 | 0.003 | 0.00, 0.01 | ||
| Part (II) Regression Analysis Models’ Comparison | |||||||
| Resid. Df | Resid. Dev | Df | DV | Cp | AIC | Pr (>Chi) | |
| Model 1 | 236,498 | 249,941 | 0 | −1.71 | 250,173 | 250,200 | 0.63 |
| Model 2 | 236,501 | 249,943 | 0 | 0 | 250,173 | 250,169 | |
| Deviance Residuals: | Min | 1Q | Median | 3Q | Max | ||
| Model 1 | −1.944 | −0.861 | −0.5248 | 1.0219 | 2.8513 | ||
| Model 2 | −1.945 | −0.861 | −0.5246 | 1.0217 | 2.8508 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Farhat, H.; Abid, C.; El Aifa, K.; Gangaram, P.; Jones, A.; Khenissi, M.C.; Khadhraoui, M.; Gargouri, I.; Al-Shaikh, L.; Laughton, J.; et al. Epidemiological Determinants of Patient Non-Conveyance to the Hospital in an Emergency Medical Service Environment. Int. J. Environ. Res. Public Health 2023, 20, 6404. https://doi.org/10.3390/ijerph20146404
Farhat H, Abid C, El Aifa K, Gangaram P, Jones A, Khenissi MC, Khadhraoui M, Gargouri I, Al-Shaikh L, Laughton J, et al. Epidemiological Determinants of Patient Non-Conveyance to the Hospital in an Emergency Medical Service Environment. International Journal of Environmental Research and Public Health. 2023; 20(14):6404. https://doi.org/10.3390/ijerph20146404
Chicago/Turabian StyleFarhat, Hassan, Cyrine Abid, Kawther El Aifa, Padarath Gangaram, Andre Jones, Mohamed Chaker Khenissi, Moncef Khadhraoui, Imed Gargouri, Loua Al-Shaikh, James Laughton, and et al. 2023. "Epidemiological Determinants of Patient Non-Conveyance to the Hospital in an Emergency Medical Service Environment" International Journal of Environmental Research and Public Health 20, no. 14: 6404. https://doi.org/10.3390/ijerph20146404
APA StyleFarhat, H., Abid, C., El Aifa, K., Gangaram, P., Jones, A., Khenissi, M. C., Khadhraoui, M., Gargouri, I., Al-Shaikh, L., Laughton, J., & Alinier, G. (2023). Epidemiological Determinants of Patient Non-Conveyance to the Hospital in an Emergency Medical Service Environment. International Journal of Environmental Research and Public Health, 20(14), 6404. https://doi.org/10.3390/ijerph20146404






