Examining the Effect of a Parent-to-Parent Intervention for Low-Income Youth with Serious Emotional and Behavioral Challenges
Abstract
:1. Introduction
- Does parent race, caregiver type, child type, or child age predict PSP service completion?
- Are there subpopulation (i.e., parent race, caregiver type, child age, and child type) differences in intervention outcomes (i.e., parents and children) for those who complete PSP services?
- Do parent ratings of treatment acceptability predict intervention effectiveness?
2. Methods
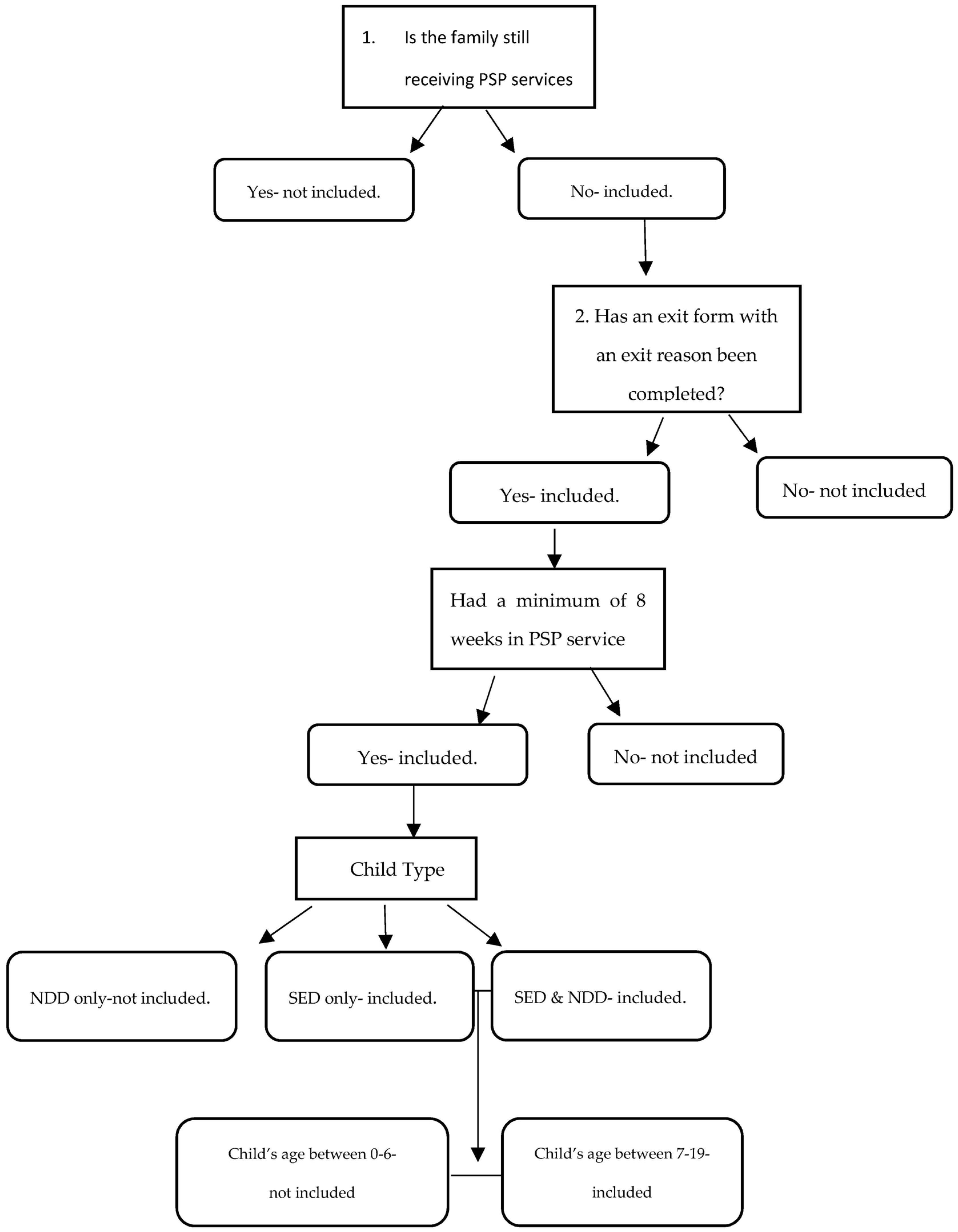
2.1. Participants
2.2. Measures
2.2.1. Attrition
2.2.2. Intervention Effectiveness
2.2.3. Child Functioning
2.2.4. Acceptability
2.3. Procedures
2.4. Data Analytic Plan
3. Results
4. Discussion and Implications
Limitations
5. Conclusions and Future Direction
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shayan, S.J.; Kiwanuka, F.; Nakaye, Z. Barriers associated with evidence-based practice among nurses in low- and middle-income countries: A systematic review. Worldviews Evid.-Based Nurs. 2019, 16, 12–20. [Google Scholar] [CrossRef] [Green Version]
- Mathieson, A.; Grande, G.; Luker, K. Strategies, facilitators and barriers to implementation of evidence-based practice in community nursing: A systematic mixed-studies review and qualitative synthesis. Prim. Health Care Res. Dev. 2018, 20, e6. [Google Scholar] [CrossRef] [Green Version]
- Substance Abuse and Mental Health Services Administration. The Comprehensive Community Health Services for Children with Severe Emotional Disturbance Program. 2017. Available online: https://store.samhsa.gov/system/files/cmhi-2017rtc.pdf (accessed on 28 October 2019).
- Williams, N.J.; Scott, L.; Aarons, G.A. Prevalence of serious emotional disturbance among US children: A meta-analysis. Psychiatr. Serv. 2018, 69, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Stagman, S.M.; Cooper, J.L. Children’s Mental Health: What Every Policymaker Should Know; National Center for Children in Poverty: New York, NY, USA, 2010; pp. 1–7. [Google Scholar] [CrossRef]
- Mendenhall, A.N.; Fontanella, C.A.; Hiance, D.L.; Frauenholtz, S. Factors associated with treatment attrition for Medicaid-enrolled youth with serious emotional disturbances. Child. Youth Serv. Rev. 2014, 40, 20–28. [Google Scholar] [CrossRef]
- Merikangas, K.R.; He, J.P.; Burstein, M.; Swendsen, J.; Avenevoli, S.; Case, B.; Georgiades, K.; Heaton, L.; Swanson, S.; Olfson, M. Service utilization for lifetime mental disorders in US adolescents: Results of the National Comorbidity Survey–Adolescent Supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 2011, 50, 32–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aratani, Y.; Cooper, J.L. Racial and ethnic disparities in the continuation of community-based children’s mental health services. J. Behav. Health Serv. Res. 2012, 39, 116–129. [Google Scholar] [CrossRef]
- Warnick, E.M.; Gonzalez, A.; Robin Weersing, V.; Scahill, L.; Woolston, J. Defining dropout from youth psychotherapy: How definitions shape the prevalence and predictors of attrition. Child Adolesc. Ment. Health 2012, 17, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Harpaz-Rotem, I.; Leslie, D.; Rosenheck, R.A. Treatment retention among children entering a new episode of mental health care. Psychiatr. Serv. 2004, 55, 1022–1028. [Google Scholar] [CrossRef]
- Santiago, C.D.; Kaltman, S.; Miranda, J. Poverty and mental health: How do low-income adults and children fare in psychotherapy? J. Clin. Psychol. 2013, 69, 115–126. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. The Ecology of Human Development: Experiments by Nature and Design; Harvard University Press: Cambridge, MA, USA, 1979. [Google Scholar]
- Cavaleri, M.A.; Olin, S.S.; Kim, A.; Hoagwood, K.E.; Burns, B.J. Family support in prevention programs for children at risk for emotional/behavioral problems. Clin. Child Fam. Psychol. Rev. 2011, 14, 399–412. [Google Scholar] [CrossRef]
- Hoagwood, K.E.; Cavaleri, M.A.; Olin, S.S.; Burns, B.J.; Slaton, E.; Gruttadaro, D.; Hughes, R. Family support in children’s mental health: A review and synthesis. Clin. Child Fam. Psychol. Rev. 2010, 13, 1–45. [Google Scholar] [CrossRef]
- Kuhn, E.S.; Laird, R.D. Family support programs and adolescent mental health: Review of evidence. Adolesc. Health Med. Ther. 2014, 5, 127–142. [Google Scholar] [CrossRef] [Green Version]
- Shilling, V.; Morris, C.; Thompson-Coon, J.; Ukoumunne, O.; Rogers, M.; Logan, S. Peer support for parents of children with chronic disabling conditions: A systematic review of quantitative and qualitative studies. Dev. Med. Child Neurol. 2013, 55, 602–609. [Google Scholar] [CrossRef] [PubMed]
- Henderson, R.J.; Johnson, A.; Moodie, S. Parent-to-parent support for parents with children who are deaf or hard of hearing: A conceptual framework. Am. J. Audiol. 2014, 23, 437–448. [Google Scholar] [CrossRef] [Green Version]
- Grape, A.C.; Plum, K.C.; Fielding, S.L. Strain among caregivers of youth designated as seriously emotionally disturbed: Do place of residence and race matter? J. Appl. Soc. Sci. 2015, 9, 83–97. [Google Scholar] [CrossRef]
- Godoy, L.; Hodgkinson, S.; Robertson, H.A.; Sham, E.; Druskin, L.; Wambach, C.G.; Long, M. Increasing mental health engagement from primary care: The potential role of family navigation. Pediatrics 2019, 143, e20182418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCabe, K.M.; Yeh, M.; Lau, A.; Garland, A.; Hough, R. Racial/ethnic differences in caregiver strain and perceived social support among parents of youth with emotional and behavioral problems. Ment. Health Serv. Res. 2003, 5, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Douma, J.C.H.; Dekker, M.C.; Koot, H.M. Supporting parents of youths with intellectual disabilities and psychopathology. J. Intellect. Disabil. Res. 2006, 50, 570–581. [Google Scholar] [CrossRef]
- Maes, B.; Broekman, T.G.; Došen, A.; Nauts, J. Caregiving burden of families looking after persons with intellectual disability and behavioural or psychiatric problems. J. Intellect. Disabil. Res. 2003, 47, 447–455. [Google Scholar] [CrossRef]
- Kuravackel, G.M.; Ruble, L.A.; Reese, R.J.; Ables, A.P.; Rodgers, A.D.; Toland, M.D. COMPASS for Hope: Evaluating the effectiveness of a parent training and support program for children with ASD. J. Autism Dev. Disord. 2018, 48, 404–416. [Google Scholar] [CrossRef] [PubMed]
- Santelli, B.; Turnbull, A.P.; Marquis, J.; Lerner, E.P. Statewide parent-to-parent programs: Partners in early intervention. Infants Young Child. 2000, 13, 74–88. [Google Scholar] [CrossRef]
- Duppong Hurley, K.L.; January, S.A.A.; Lambert, M.C. Using caregiver strain to predict participation in a peer-support intervention for parents of children with emotional or behavioral needs. J. Emot. Behav. Disord. 2017, 25, 170–177. [Google Scholar] [CrossRef] [Green Version]
- Lammers, E.; Zickafoose, J.; Peterson, G.; Blue, L.; Stewart, K.; Kranker, K. Parent Partners: Evaluation of a novel peer-support intervention for caregivers of children hospitalized for behavioral health conditions. Acad. Pediatr. 2019, 19, 908–916. [Google Scholar] [CrossRef] [PubMed]
- Butler, A.M.; Titus, C. Pilot and feasibility study of a parenting intervention delivered by parent peers. Vulnerable Child. Youth Stud. 2017, 12, 215–225. [Google Scholar] [CrossRef] [Green Version]
- January, S.A.A.; Hurley, K.D.; Stevens, A.L.; Kutash, K.; Duchnowski, A.J.; Pereda, N. Evaluation of a community-based peer-to-peer support program for parents of at-risk youth with emotional and behavioral difficulties. J. Child Fam. Stud. 2016, 25, 836–844. [Google Scholar] [CrossRef]
- Kutash, K.; Duchnowski, A.J.; Green, A.L.; Ferron, J. Supporting parents who have youth with emotional disturbances through a parent-to-parent support program: A proof of concept study using random assignment. Adm. Policy Ment. Health Ment. Health Serv. Res. 2011, 38, 412–427. [Google Scholar] [CrossRef] [PubMed]
- Jamison, J.M.; Fourie, E.; Siper, P.M.; Trelles, M.P.; George-Jones, J.; Buxbaum Grice, A.; Krata, J.; Holl, E.; Shaoul, J.; Hernandez, B.; et al. Examining the efficacy of a family peer advocate model for black and hispanic caregivers of children with autism spectrum disorder. J. Autism Dev. Disord. 2017, 47, 1314–1322. [Google Scholar] [CrossRef]
- Day, C.; Michelson, D.; Thomson, S.; Penney, C.; Draper, L. Evaluation of a peer led parenting intervention for disruptive behaviour problems in children: Community-based randomized controlled trial. Br. Med. J. 2012, 344, e1107. [Google Scholar] [CrossRef] [Green Version]
- Santelli, B.; Turnbull, A.; Marquis, J.; Lerner, E. Parent-to-parent programs: A resource for parents and professionals. J. Early Interv. 1997, 21, 73–83. [Google Scholar] [CrossRef]
- Michigan Department of Health and Human Services. Electronic Medicaid Provider Manual. Available online: https://www.mdch.state.mi.us/dch-medicaid/manuals/MedicaidProviderManual.pdf (accessed on 10 June 2023).
- Michigan Department of Health and Human Services. Parent Support Partner (PSP) Outcome Tool; 2016; unpublished instrument.
- Williams, B.J.; Poole, L.; Esterer, M.; Carlson, J.S.; Batsche-McKenzie, K.; Tate, J.; Shank, J. Investigating the psychometric properties of the Parent Support Partner Outcome Tool. Vulnerable Child. Youth Stud. 2022, 18, 143–148. [Google Scholar] [CrossRef]
- Hodges, K. Child and Adolescent Functional Assessment Scales; Vanderbilt Child Mental Health Services Evaluation Project; Vanderbilt University: Nashville, TN, USA, 1990. [Google Scholar]
- Hodges, K. Child and Adolescent Functional Assessment Scale (CAFAS) Overview of Reliability and Validity. Available online: https://www.fasoutcomes.com/content.aspx?contentid=1084 (accessed on 10 June 2023).
- Hodges, K.; Wong, M.M. Psychometric characteristics of a multidimensional measure to assess impairment: The Child and Adolescent Functional Assessment Scale. J. Child Fam. Stud. 1996, 5, 445–467. [Google Scholar] [CrossRef] [Green Version]
- Hodges, K.; Wong, M.M.; Latessa, M. Use of the Child and Adolescent Functional Assessment Scale (CAFAS) as an outcome measure in clinical settings. J. Behav. Health Serv. Res. 1998, 25, 325–336. [Google Scholar] [CrossRef]
- Michigan Mental Health Act. Mic. Stat. § 330. 1974. Available online: http://www.legislature.mi.gov/(S(jckim1ueldzrdjebpllryckd))/mileg.aspx?page=getObject&objectName=mcl-330-1100d (accessed on 21 April 2022).
- Association for Children’s Mental Health. Parent Support Partner; Association for Children’s Mental Health: Kalamazoo, MI, USA, 2022; Available online: https://www.acmh-mi.org/get-information/acmh-projects/parent-support-partner-project/ (accessed on 13 June 2023).
- Stoltzfus, J.C. Logistic regression: A brief primer. Acad. Emerg. Med. 2011, 18, 1099–1104. [Google Scholar] [CrossRef] [PubMed]
- Ingoldsby, E.M. Review of interventions to improve family engagement and retention in parent and child mental health programs. J. Child Fam. Stud. 2010, 19, 629–645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reardon, T.; Harvey, K.; Baranowska, M.; O’Brien, D.; Smith, L.; Creswell, C. What do parents perceive are the barriers and facilitators to accessing psychological treatment for mental health problems in children and adolescents? A systematic review of qualitative and quantitative studies. Eur. Child Adolesc. Psychiatry 2017, 26, 623–647. [Google Scholar] [CrossRef] [Green Version]
- Hoskote, A.R.; Croce, E.; Johnson, K.E. The evolution of the role of U.S. school nurses in adolescent mental health at the individual, community, and systems level: An integrative review. J. Sch. Nurs. 2023, 39, 51–71. [Google Scholar] [CrossRef] [PubMed]
| Parent-to-Parent Program | Demographic Characteristics Studied Comparable to Current Study | Attrition Rate | Outcome Variables | Measure of Acceptability |
|---|---|---|---|---|
| Parent Support Partner Program (current study) | N = 464 Parent race, child age, caregiver type, and SED type | 56% (n = 263) | Parent change (bridging, collaboration, developing direction, and empowerment) Child functioning | Two questions (helpfulness and recommend to others) |
| Parent Connectors [25,28,29] * | N = 128 caregiver type and child age | 0% | Caregiver strain In-school suspensions | N/A |
| N = 348 (i.e., 180 parent connectors and 168 control parents) Parent race, caregiver type, and child age | 1% (n = 2) | Treatment integrity | Call length, helpfulness, and recommendations to others | |
| N= 115 (i.e., 60 intervention parents and 55 controls) Caregiver type and child age | 26% (n = 14) | Parent engagement and functioning Child impairment Academic assessment | Parent satisfaction | |
| N = 139 parent race and child age | Not Reported | Parent protective factors | N/A | |
| Parent Partners [26] * | N = 2854 parent race, child age, and SED type | Not Reported | Child impairment | N/A |
| Parent Empowerment Program (PEP; [30]) | N = 39 (i.e., 19 parents within the intervention groups and 20 in the control condition control groups) Child age | 15% (n = 6) | Psychoeducation Caregiver strain Family empowermentService utilization | N/A |
| Smart and Secure Intervention [27] * | N = 15 caregiver type, child age, and parent race | 60% (n = 9) | Child problems Parent stress Parent competence | N/A |
| Empowering Families, Empowering Communities [31,32] | N = 73 Child age | 34% (n = 25) | Peer facilitator training Child functioning Parent stress | Peer facilitator acceptability |
| N = 116 (i.e., 59 intervention parents and 57 waitlist parents) parent race, child age, and caregiver type | 8% (n = 5) | Parenting behaviors Parent stress | Treatment acceptability |
| Subpopulation Characteristics for This Study | n |
|---|---|
| Caregiver Type | |
| Biological mothers | 326 (70%) |
| * Nonbiological mothers | 138 (30%) |
| Child Age (7–19) | 464 M = 11.29, SD = 2.98 |
| Parent Race | |
| White/Caucasian | 346 (75%) |
| Black/African American | 84 (18%) |
| ** Other | 34 (7%) |
| SED Type | |
| SED only | 402 (89%) |
| SED and NDD | 45 (11%) |
| Subpopulation Demographics | Completers (n = 201) | Noncompleters (n = 263) | |||||
|---|---|---|---|---|---|---|---|
| Frequency | % | Frequency | % | Wald’s c2 | p | eb | |
| Parent race | |||||||
| White | 155 | 77% | 191 | 73% | 1.926 | 0.165 | 1.705 |
| Black | 35 | 17% | 49 | 18% | 0.756 | 0.384 | 1.461 |
| Other | 11 | 6% | 23 | 9% | |||
| Caregiver type | |||||||
| Biological Mother | 144 | 72% | 182 | 70% | 0.685 | 0.408 | 1.191 |
| Nonbiological Mother | 57 | 28% | 81 | 30% | |||
| Child type (n = 194, 253) | |||||||
| SED Only | 171 | 88% | 231 | 91% | 0.935 | 0.333 | 0.736 |
| SED and NDD | 23 | 12% | 22 | 9% | |||
| Child Age | |||||||
| Early Adolescence (ages < 13) | 156 | 78% | 199 | 76% | 0.042 | 0.838 | 1.048 |
| Late Adolescence (ages 14–19) | 45 | 22% | 64 | 24% | |||
| Constant | 1.365 | 0.24 | 0.539 | ||||
| Subpopulation Demographics | Pre-Test | Post-test | ANOVA | ||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | Effect | F | η2 | |
| Parent race (n = 153) | |||||||
| White (n = 117) | 73.45 | 1.42 | 82.67 | 1.13 | T | 22.73 ** | 0.132 |
| Black (n = 25) | 79.20 | 3.07 | 86.20 | 2.45 | G | 2.39 | 0.031 |
| Other (n = 11) | 76.00 | 4.63 | 89.27 | 3.69 | TxG | 0.552 | 0.007 |
| Caregiver type (n = 153) | |||||||
| Biological Mother (n = 94) | 76.17 | 1.58 | 83.79 | 1.27 | T | 49.40 ** | 0.246 |
| Nonbiological Mother (n = 54) | 72.03 | 2.00 | 83.63 | 1.61 | G | 1.32 | 0.009 |
| TxG | 2.12 | 0.014 | |||||
| Child SED type (n = 148) | |||||||
| SED Only (n = 141) | 75.02 | 1.28 | 83.91 | 1.04 | T | 12.92 ** | 0.081 |
| SED and NDD (n = 7) | 64.00 | 5.71 | 78.14 | 4.67 | G | 3.84 | 0.026 |
| TxG | 0.673 | 0.005 | |||||
| Child Age (n = 153) | |||||||
| Early Adolescence (n = 117) | 74.31 | 1.43 | 83.73 | 1.14 | T | 31.42 ** | 0.172 |
| Late Adolescence (n = 36) | 75.44 | 2.58 | 83.72 | 2.06 | G | 0.792 | 0.000 |
| TxG | 0.131 | 0.001 | |||||
| Subpopulation Demographics | Pre-Test | Post-Test | ANOVA | ||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | Effect | F | η2 | |
| Parent race (n = 153) | |||||||
| White (n = 117) | 104.44 | 31.87 | 88.55 | 36.67 | T | 15.58 ** | 0.094 |
| Black (n = 25) | 106.80 | 36.93 | 82.40 | 26.50 | G | 0.172 | 0.002 |
| Other (n = 11) | 105.45 | 25.44 | 96.36 | 43.65 | TxG | 0.977 | 0.013 |
| Caregiver type (n = 153) | |||||||
| Biological Mother (n = 94) | 102.66 | 32.50 | 84.79 | 34.69 | T | 34.92 ** | 0.188 |
| Nonbiological Mother (n = 54) | 108.47 | 31.55 | 93.39 | 36.68 | G | 2.17 | 0.014 |
| TxG | 0.250 | 0.002 | |||||
| SED type (n = 148) | |||||||
| SED Only (n = 141) | 104.33 | 32.63 | 88.72 | 36.29 | T | 10.67 ** | 0.068 |
| SED and NDD (n = 7) | 112.86 | 34.50 | 85.71 | 34.57 | G | 0.056 | 0.000 |
| TxG | 0.778 | 0.005 | |||||
| Child age (n = 153) | |||||||
| Early Adolescence (n = 117) | 99.23 | 29.91 | 81.28 | 30.97 | T | 23.52 ** | 0.135 |
| Late Adolescence (n = 36) | 123.33 | 32.68 | 110.28 | 41.09 | G | 25.85 ** | 0.146 |
| TxG | 0.586 | 0.004 | |||||
| Variable | B | β | t | p |
|---|---|---|---|---|
| Change in PSP scores | ||||
| Constant | −22.62 | −2.22 | 0.031 | |
| Treatment acceptability | 1.68 | 0.263 | 3.16 | * 0.002 |
| Change in CAFAS Scores | ||||
| Constant | −21.31 | −0.87 | 0.386 | |
| Treatment acceptability | 0.22 | 0.015 | 0.17 | 0.866 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poole, L.B.; Carlson, J.S.; Batsche-McKenzie, K.; Tate, J.; Shank, J. Examining the Effect of a Parent-to-Parent Intervention for Low-Income Youth with Serious Emotional and Behavioral Challenges. Int. J. Environ. Res. Public Health 2023, 20, 6435. https://doi.org/10.3390/ijerph20146435
Poole LB, Carlson JS, Batsche-McKenzie K, Tate J, Shank J. Examining the Effect of a Parent-to-Parent Intervention for Low-Income Youth with Serious Emotional and Behavioral Challenges. International Journal of Environmental Research and Public Health. 2023; 20(14):6435. https://doi.org/10.3390/ijerph20146435
Chicago/Turabian StylePoole, Lindsay B., John S. Carlson, Kim Batsche-McKenzie, Justin Tate, and Jane Shank. 2023. "Examining the Effect of a Parent-to-Parent Intervention for Low-Income Youth with Serious Emotional and Behavioral Challenges" International Journal of Environmental Research and Public Health 20, no. 14: 6435. https://doi.org/10.3390/ijerph20146435
APA StylePoole, L. B., Carlson, J. S., Batsche-McKenzie, K., Tate, J., & Shank, J. (2023). Examining the Effect of a Parent-to-Parent Intervention for Low-Income Youth with Serious Emotional and Behavioral Challenges. International Journal of Environmental Research and Public Health, 20(14), 6435. https://doi.org/10.3390/ijerph20146435








